Abstract
The role of individual versus community level social connections in promoting health is an important factor to consider when addressing Latino health. This analysis examines the relationships between social support, social cohesion, and health in a sample of Latinos in the United States. Using data from the National Latino and Asian American Study, the analysis uses ordered logistic regression to explore the relationships of family support, friend support, family cultural conflict, and neighborhood social cohesion with self-rated physical and mental health, taking into account language proficiency and use, nativity, and sociodemographic variables. Family support, friend support, and neighborhood social cohesion were positively related to self-rated physical and mental health, and family cultural conflict was negatively related when controlled only for sex and age. After controlling for education, income, and other demographic measures, only family support was found to have a weak association with self-rated physical health; however, the relationship seemed to be mediated by language. In contrast, family support and family cultural conflict were strongly associated with self-rated mental health, after controlling for language, education, income, and other demographic measures. The study did not find neighborhood social cohesion to be significantly related to either self-rated physical or mental health, after accounting for the effects of the other social connection variables. Language of interview did not explain the highly significant effects of language proficiency and use. Social connections are important for health and mental health, but language and other sociodemographic factors seem to be related to how Latinos establish these social linkages. Further investigation into the role of language in the development and maintenance of social connections may help unravel the mechanisms by which they promote or decrease health.
Keywords: USA, social cohesion, social support, Latino, self-rated health, self-rated mental health
Introduction
An extensive literature supports a relationship between community level social connection (e.g., social cohesion) and health, both in terms of its relationship to mortality at the community level (Lochner, Kawachi, Brennan, & Buka, 2003) and to self-rated health on an individual level (Browning & Cagney, 2002). Common indicators of community-level connection include participation in civic activities and willingness to help neighbors (Macinko & Starfield, 2001). A wide social epidemiology literature (Kawachi & Berkman, 2000) similarly examines the healthful effects of qualitative social support from social networks, including friends and family. However, there is little empirical work comparing different types of social connections to health, particularly how individual and community level supports differentially affect health (Wen, Cagney, & Christakis, 2005).
A related area of interest explores how mechanisms of social connection operate in relationship to physical and mental health for United States residents from Latino cultures. Individual level social support factors have been cited as mediating variables for both better health (Finch & Vega, 2003) and mental health (Galea, Vlahov, Tracy, Hoover, Resnick, & Kilpatrick, 2004) for low-income, immigrant Latinos. Recent critiques have identified conceptual concerns with the ways that the relationships between health and social factors for Latinos are defined and analyzed, particularly how measures of acculturation are applied in these analyses (Hunt, Schneider, & Comer, 2004). These authors note that acculturation measures vary widely across studies and the role of sociodemographic factors such as language and education in facilitating access to structural health benefits (e.g., health information) and positive health outcomes is not adequately explored (Borrayo & Jenkins, 2003).
The focus of this paper is to examine relationships between three domains of social connection and self-rated physical and mental health in a sample of Latinos across three domains of social connection, considering the role of socioeconomic status (SES) and language in facilitating these connections. At the individual level, we look at two domains: family connections (both family support and family conflict) and friend support. At the community level, we look at neighborhood social cohesion. We include measures of education, income and Spanish language proficiency and language used when thinking in our analyses to strengthen our understanding of these mechanisms in the context of social connection.
Background
Physical and Mental Health for Latinos
Overall, Latinos have lower mortality rates compared to other ethnic groups with the same socioeconomic status (SES) (Abraido-Lanza, Chao, & Florez, 2005; Franzini, Ribble, & Keddie, 2001). However, for many specific disorders, low education and income have inverse relationships with health among Latinos (Hunninghake, Weiss, & Celedon, 2006; Reynolds, 2004). In mental health, no consistent patterns have been identified. Lower-income immigrant Latinos have been found to be at lower risk for psychiatric disorders than those who are more acculturated (Alegría, Canino, Stinson, & Grant, 2006; Vega, Sribney, Aguilar-Gaxiola, & Kolody, 2004) and lower risk compared to non-Latino whites (Breslau, Aguilar-Gaxiola, Kendler, Su, Williams, & Kessler, 2006). However, other studies have found that Latinos have higher rates of depressive symptoms than non-Latino whites (Perreira, Deeb-Sossa, Mullan Harris, & Bollen, 2005), and that lower income, Latino immigrants have higher depressive symptomatology compared to more acculturated Latinos (Gonzalez, Haan, & Hinton, 2001). These patterns suggest a complicated relationship among sociodemographic factors, social connections and health for Latinos.
Social Connections for Latinos
The variability in findings regarding Latinos and health suggests that even within the same sociodemographic category, social connections that seem to be related to health may not be uniform for Latinos (Weinick, Jacobs, Stone, Ortega, & Burstin, 2004).
Family support and conflict
A frequent explanation for what appears to be better health for Latinos has been a higher degree of family support among Latino families. Studies have found positive mental and physical health benefits of family support for Latinos (Bird, Canino, Davies, Zhang, Ramirez, & Lahey, 2001; Page, 2004). In understanding family support, an important distinction is between functional support (e.g., emotional assistance) and structural support, (e.g., size of these supports) (Thoits, 1995). Some have hypothesized that the informal support of extended family is a critical structural factor in healthier outcomes for poor Latino infants (McGlade, Saha, & Dahlstrom, 2004), while others stress the quality of relationships; for example, in Latino families with a family member with mental illness, the presence of warmth was protective of relapse (Lopez, Nelson, Polo, Jenkins, Karno, Vaughn et al., 2004).
However, maintaining strong connections with extended family does not necessarily mean better outcomes. The nature of these connections within the family may also be a strong factor in health. Some studies have found that for Latinos, family conflict was related to increased emotional distress and other health risk behaviors (McQueen, Getz, & Bray, 2003; Tschann, Flores, Marin, Pasch, Baisch, & Wibbelsman, 2002). Others have argued that changes in the structure of the Latino family across generations may increase stress thus negatively affecting Latinos' mental health (Alegría, Mulvaney-Day, Torres, Polo, Cao, & Canino, in press). It is important to consider the ways in which both family conflict and family support may vary depending upon how extended families navigate the transition from first to second generation and beyond.
Friend Support
Studies within ethnic enclaves have alternately found both positive and negative associations between dense relationships with friends and access to economic opportunity (Portes, 1998). Immersion in close networks of friends from the same background can lead to increased economic opportunities for recent immigrants and others still living in ethnic enclaves (Nee, Sanders, & Sernau, 1994; Portes, 1987). Alternately, dependence on interpersonal connections inside impoverished crime-ridden immigrant communities can lead to a dearth of opportunities for economic advancement (Stack, 1974; Sullivan, 1989).
The social support of unrelated, close friends is considered to exert a positive impact on physical and mental health (Kawachi & Berkman, 2000), and has been found in some studies to have a more significant impact on mental health for Latinos than family support (Rodriguez, Mira, Myers, Morris, & Cardoza, 2003; Vega, Kolody, & Valle, 1987). However, social connectedness with friends may also have a negative impact on mental health in low-income or rural communities, where survival may depend upon conformity to oppressive community norms (Caughy, O'Campo, & Mutaner, 2003; Wakefield & Poland, 2005). Higher levels of community social network density have been found to be associated with increased mortality in a sample of elderly, and are more common in communities characterized by higher rates of crime and lower levels of SES (Wen, Cagney, & Christakis, 2005). Similar to family support, the relationship between friend support and health may be particularly vulnerable to the socioeconomic characteristics of the community.
Neighborhood social cohesion
With neighborhood social cohesion, the external environment is the source of healthful effects, beyond the qualitative support provided by individual relationships with family and friends. This type of social connection is characterized by the presence of trusting relationships among individuals who may not have close emotional ties. The locus of support provided by neighborhood social cohesion theoretically lies in the community. Living in a community where there is trust has been hypothesized to support “loose” interpersonal connections that have many positive structural benefits (Putnam, 2000), including better access to social and health services (Hendryx & Ahern, 2001; Rosenheck, 2001). Alternately, those who live in neighborhoods with low trust may not have the opportunity to share information with others (e.g., in neighborhood playgrounds) and may miss an important source of community level support.
How these community-level variables operate for Latinos specifically is an understudied area, and particularly complex given the broad experiences of community influences for this diverse group. For example, for recent immigrants, help-seeking and health care patterns may be primarily influenced by experiences in their country of origin and not their current social context (Portes, Kyle, & Eaton, 1992). The presence of loose ties in the neighborhood, and how this might facilitate knowledge about and access to health care for Latinos, is complicated as the Spanish/English language capacity of both the individual and the dominant language in the surrounding community may impact these relationships. One recent study found that ethnic minorities living in homogeneous neighborhoods were more likely to use health care services than those living in heterogeneous communities (Haas, Phillips, Sonneborn, McCulloch, Baker, Kaplan et al., 2004).
Sociodemographic Mechanisms
Both SES and language may facilitate or impede the process of developing and maintaining social connections and may create pathways for social connections that have profound influences on health.
Socioeconomic status
Although in general higher socioeconomic status facilitates social connections and health (Adler & Newman, 2002), in immigrant communities, the potentially healthful effects of social connections may compete with a process of acculturation that promises increased access to education and income, but also increased exposure to discrimination and other social stresses that might negatively impact health (Finch & Vega, 2003). Recent work has found that lower education may be protective against psychiatric disorder for some minorities (Breslau, Aguilar-Gaxiola, Kendler et al., 2006). Family conflict may increase as generations become more educated and move further from home (Pasch, Deardorff, Tschann, Flores, Penilla, & Pantoja, 2006), thus increasing stress and potentially the risk of mental health disorders.
Language
English language ability increases access to information and access to health services (Reynolds, 2004; Stuart, Minas, Klimidis, & O'Connell, 1996). However, maintaining Spanish in the process of assimilating into the U.S. culture may also be a mechanism whereby the positive effects of social connection are maintained. Fluent bilingualism has been found to be associated with better family relations and psychosocial adjustment in second generation immigrants from multiple backgrounds, compared to both monolingualism and limited bilinguals (Portes & Hao, 2002). To our knowledge, however, the relationship between Spanish/English bilingualism and physical health outcomes has not been studied in U.S. Latinos. For mental health, we would expect that maintaining Spanish is indicative of closer relationships with one's extended family across generations. One study found that both English proficiency and Spanish language use had a positive effect on the presence of loose social ties in a school setting (Stanton-Salazar & Dornbusch, 1995). These studies suggest that the healthful effects of maintaining Spanish may depend upon how well the Spanish-speaker also speaks English, but that English-speaking alone may not indicate the greatest access to healthful connections and resources.
Objectives of this study
The goal for this analysis is to examine the association of perceptions of neighborhood social cohesion, family support, friend support, and family cultural conflict with self-rated physical and mental health for Latinos, in relation to SES and language. We observe the broad influences of these social connection variables on self-rated mental health, rather than isolating a single psychiatric disorder (Aneshensel, Rutter, & Lachenbruch, 1991). The process of immigration and of assimilation into a new culture can be stressful (Vega & Amaro, 1994), and the way social connections either exacerbate or mitigate this stress for Latinos is complex. Given that the health effects of stress are likely related not to a single physical or mental health disorder but rather will manifest themselves according to non-specific health effects, we use self-rated physical and mental health to capture these broad relationships. Self-rated physical health has construct and criterion validity and predicts mortality and morbidity (Idler & Benyamini, 1997). Among racial and ethnic minorities, it has been found to be a valid predictor of morbidity (Chandola & Jenkinson, 2000), and of mortality for more acculturated Latinos (Finch, Hummer, Reindl, & Vega, 2002). Although the validity of self-rated mental health is less explored (Rohrer, 2004), other studies have used self-rated mental health with Latinos (Albizu-García, Alegría, Freeman, & Vera, 2001).
We hypothesize that the relationships between the social connection variables and self-rated health will be similar across the two outcomes. For physical health, we hypothesize that social cohesion will have a positive relationship with self-rated physical health given that neighborhood social cohesion has a negative relationship with mortality (Lochner, Kawachi, Brennan et al., 2003) and neighborhood violence (Sampson, Raudenbush, & Earls, 1997). Based on theories that community level social cohesion should be strongly associated with mental health (Kawachi & Berkman, 2000; Sartorius, 2003), we also hypothesize that neighborhood social cohesion will be positively associated with self rated mental health. We further hypothesize that the family and friend support variables will be positively related to self-rated mental health, and that family conflict will be negatively related. Since theories indicate that social cohesion will facilitate access to health information and services, which will be positively associated with mental and physical health, we expect that neighborhood social cohesion will capture a different quality of relationship than family and friend support. Hence, we hypothesize that neighborhood social cohesion will have an independent effect on self-rated health and mental health, beyond the support of family or friends. Finally, given the previous discussion, we expect that the language variables, after controlling for the effects of education, income, and family and friend support, will be related to self-rated mental and physical health; in particular, for this exploratory analysis, those who indicate mastery in both Spanish and English will have better physical and mental health than those who think and speak primarily in one language.
Data and Methods
Description of the sample
The data set for this analysis is from the National Latino and Asian American Study (NLAAS), a nationally representative household survey of Latinos and Asians based on a stratified area probability sample design (Alegría, Takeuchi, Canino, Duan, Shrout, Meng et al., 2004; Heeringa, Wagner, Torres, Duan, Adams, & Berglund, 2004). Data collection was conducted by the University of Michigan's Institute for Social Research (ISR) between May 2002 and November 2003. The analytic sample consists of 2554 Latinos from four distinct subgroups: 577 Cuban; 495 Puerto Rican; 868 Mexican; and 614 Other Latino. All respondents who wanted to be interviewed in Spanish were accommodated. The final weighted response rate for the Latino sample was 75.5%.
Measures
Dependent variables for analysis were self-rated physical and mental health. The physical health question asks, “How would you rate your overall physical health – excellent, very good, good, fair or poor.” Self-rated mental health was measured using a parallel question. We maintained the ordinal structure of these measures, including all five categories in the analyses.
Analyses were controlled for sex, age, marital status, nativity, and subethnicity (Puerto Rican, Cuban, Mexican, or Other Latino). Independent variables for the analyses were education, income, and language. We created a measure of language proficiency and use consisting of six categories from two questions that asked how well the respondent spoke Spanish and whether the respondent used Spanish or English when thinking. Those who reported speaking Spanish either “excellent” or “good” were separated into three categories – using Spanish all or most of the time when thinking, using Spanish and English equally, or using English all or most of the time when thinking. Those who reported speaking Spanish either “fair” or “poor” were separated into the same three categories of language used when thinking. We also included language of interview in our analysis. In NLAAS, language of interview was determined by respondent self-selection with one exception. A portion of those who reported proficiency in both English and Spanish (13.5% of the total weighted sample) were randomly assigned to either the English or Spanish interview.
The social connection variables were measured using four scales. All scales were simple additive scores of equal items with higher scores indicating higher levels of the construct being measured. The Social Cohesion scale (mean= 12.0, SD = 2.9, range = 4–16) asks whether people in the neighborhood can be trusted and whether they get along with each other (Sampson, Raudenbush, & Earls, 1997), whether the respondents have neighbors who could help in an emergency (National Institute of Mental Health, 1994) and whether the respondent thinks people in the neighborhood look out for one another (Bearman, Jones, & Udry, 1997) (Cronbach's α = 0.81 for English interview and 0.81 for the Spanish interview).
Family and friend support measure the degree of support provided in these two domains (Kessler, Berglund, Demler, Jin, Koretz, Merikangas et al., 2003). Family support (mean = 11.6, SD = 2.7, range = 5–15) was measured by three items to assess the respondent's ability to rely on extended family for emotional support (α = 0.71 English, 0.72 Spanish). The questions ask how often the respondent talks on the phone or gets together with relatives, how much the respondent can rely on relatives for help with a serious problem and how much the respondent can open up to family and talk about worries. The friend support scale (mean = 10.3, SD = 2.9, range = 5–15) consists of three parallel items that assess the respondent's ability to rely on friends for emotional support (α = 0.75 English, 0.78 Spanish).
The family cultural conflict scale (mean = 6.3, SD = 1.9, range = 5–15) measures cultural conflict between the respondents and their families (α = 0.90 English, 0.96 Spanish). Drawn from a subscale of the Hispanic Stress Inventory (HSI), the scale demonstrates good psychometric properties for Latinos (Cervantes, Padilla, & Salgado de Snyder, 1991). The five items ask whether the respondent has ever felt being close to family interfered with goals, felt isolated due to lack of family unity, felt family relations were becoming less important, had family conflict due to different customs, or had family conflict due to personal goals.
Since these scales did not have normative or other scaling based on prior studies, we normalized them to have zero mean and a standard deviation of one in the full NLAAS Latino sample population.
Statistical analyses
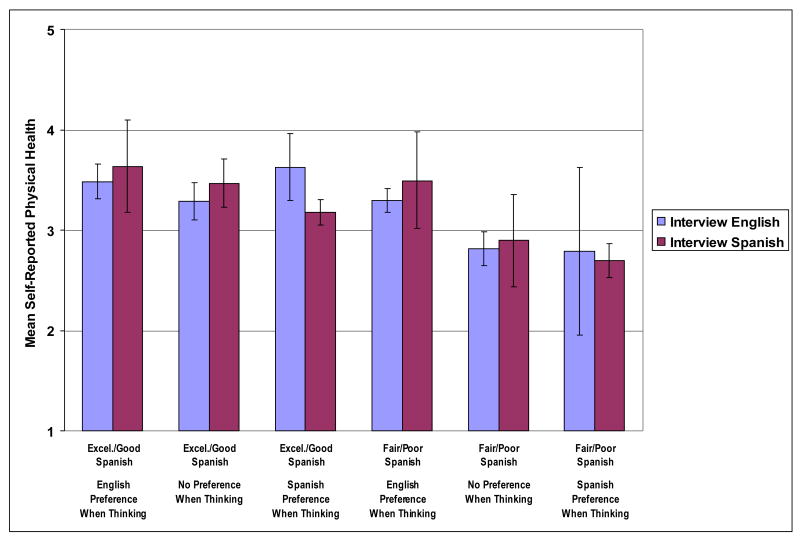
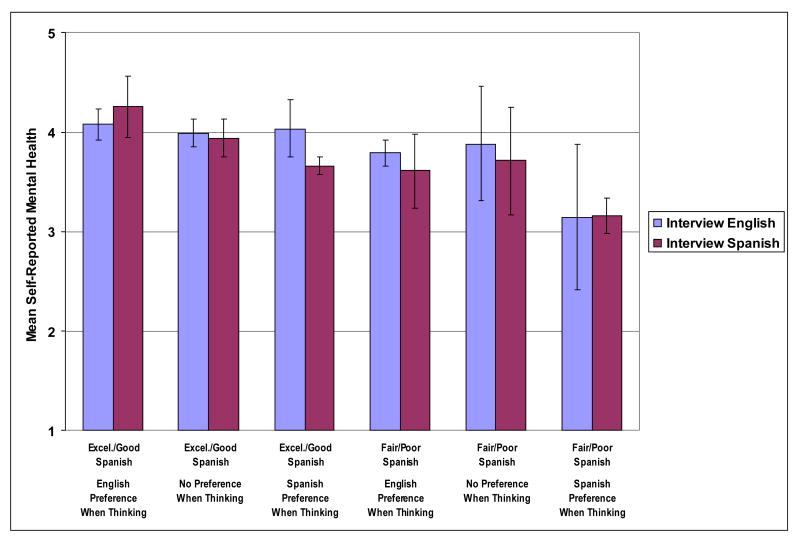
Table 1 shows weighted estimates of proportions. Table 2 gives mean scores of the social connection scales by categories of self-rated physical and mental health, education, income, and language variables. Weights were adjusted by sex and age within each category to remove any effect of sex–age differences. In Tables 3 and 4, weighted ordered logistic regressions (McCullagh & Nelder, 1989) were fit to model the two ordinal outcome variables, self-rated physical and mental health. Initial models included all social connection scales. Since scales were highly collinear, one scale could potentially mask the effect of another scale; hence, non-significant scales were removed from final models shown in the tables. Figures 1 and 2 used weighted linear regressions with the same variables as the final models shown in Tables 3 and 4, except that the six language categories were interacted by language of interview. Figures show adjusted means for each of the resulting 12 language categories with error bars corresponding to 95% confidence intervals. Standard error estimates for all analyses were adjusted for the sampling design through a first-order Taylor series approximation. In Tables 2–4, design-based Wald tests (Korn & Graubard, 1990) were conducted to test the joint effects of each domain. Significance tests for weighted correlations among the scales were conducted using a jackknife procedure (Rust & Rao, 1996). All analyses were conducted using Stata version 8.2 (StataCorp, 2004).
Table 1.
Sociodemographic Characteristics and Self-rated Physical and Mental Health1 of U.S. Latinos in the National Latino and Asian American Study.
| % | |||
|---|---|---|---|
| Female | 48.5 | ||
| Male | 51.5 | ||
| Age (y) | |||
| 18–24 | 20.7 | ||
| 25–34 | 28.4 | ||
| 35–49 | 30.1 | ||
| 50–64 | 13.4 | ||
| ≥65 | 7.5 | ||
| Marital status | |||
| Married | 51.9 | ||
| Divorced/separated/widowed | 18.4 | ||
| Never married | 29.7 | ||
| Education (y) | |||
| No high school (<9) | 25.1 | ||
| Some high school (<12) | 19.4 | ||
| High school graduate (12) | 24.5 | ||
| Some college (13–15) | 20.8 | ||
| College degree or greater (≥16) | 10.2 | ||
| Household income ($) | |||
| <15,000 | 27.5 | ||
| 15,000–34,999 | 28.7 | ||
| 35,000–74,999 | 27.7 | ||
| ≥75,000 | 16.1 | ||
| Nativity | |||
| Foreign born | 58.5 | ||
| U.S. born | 41.5 | ||
| Subethnicity | |||
| Puerto Rican2 | 10.0 | ||
| Cuban | 4.6 | ||
| Mexican | 56.6 | ||
| Other Latino | 28.7 | ||
| Language of interview | |||
| Spanish | 54.3 | ||
| English | 45.7 | ||
| Language used when thinking | |||
| Spanish all or most of the time | 53.8 | ||
| Spanish and English equally | 16.3 | ||
| English all or most of the time | 30.0 | ||
| Spanish language proficiency | |||
| Excellent or good | 71.2 | ||
| Fair or poor | 28.8 | ||
| Spanish proficiency/Language used when thinking | |||
| Spanish excellent/good, English all or most of the time when thinking | 15.6 | ||
| Spanish excellent or good, English and Spanish when thinking | 13.1 | ||
| Spanish excellent or good, Spanish all or most of the time when thinking | 42.3 | ||
| Spanish fair or poor, English all or most of the time when thinking | 14.4 | ||
| Spanish fair or poor, English and Spanish when thinking | 3.2 | ||
| Spanish fair or poor, Spanish all or most of the time when thinking | 11.4 | ||
| Self-rated physical health | |||
| Excellent | 15.5 | ||
| Very good | 24.7 | ||
| Good | 31.4 | ||
| Fair | 24.9 | ||
| Poor | 3.5 | ||
| Self-rated mental health | |||
| Excellent | 30.4 | ||
| Very good | 27.8 | ||
| Good | 30.0 | ||
| Fair | 11.0 | ||
| Poor | 0.7 | ||
All data are reported as weighted estimates of population percentages.
Persons born in Puerto Rico are U.S. citizens; “foreign born” and “US born” refer to island birthplace and mainland birthplace, respectively.
Table 2.
Mean1 Social Connection Scale Values by Self-rated Physical and Mental Health, Education, Income, and Language of U.S. Latinos.
| Social cohesion | Family support | Family cultural conflict | Friend support | |
|---|---|---|---|---|
| Self-rated physical health | ||||
| Excellent | 0.03 (0.07) | 0.07 (0.06) | 0.03 (0.06) | 0.01 (0.05) |
| Very good | 0.11 (0.05) | 0.12 (0.06) | −0.11 (0.04) | 0.16 (0.05) |
| Good | 0.07 (0.05) | 0.04 (0.04) | −0.03 (0.04) | 0.01 (0.05) |
| Fair | −0.20 (0.05) | −0.15 (0.05) | 0.03 (0.05) | −0.20 (0.05) |
| Poor | −0.21 (0.12) | −0.06 (0.12) | 0.12 (0.12) | −0.04 (0.14) |
| *** | * | * | *** | |
| Self-rated mental health | ||||
| Excellent | 0.09 (0.04) | 0.14 (0.06) | −0.07 (0.05) | 0.10 (0.04) |
| Very good | 0.04 (0.06) | −0.03 (0.05) | −0.07 (0.04) | 0.14 (0.04) |
| Good | −0.03 (0.06) | 0.00 (0.04) | 0.00 (0.06) | −0.13 (0.05) |
| Fair | −0.23 (0.07) | −0.36 (0.07) | 0.37 (0.10) | −0.28 (0.08) |
| Poor | −0.09 (0.30) | −0.57 (0.29) | 0.81 (0.47) | −0.74 (0.29) |
| ** | *** | ** | *** | |
| Education (y) | ||||
| No high school (<9) | −0.22 (0.08) | −0.26 (0.05) | −0.01 (0.09) | −0.35 (0.07) |
| Some high school (<12) | 0.02 (0.06) | −0.04 (0.05) | 0.07 (0.08) | −0.12 (0.07) |
| High school graduate (12) | 0.09 (0.06) | 0.06 (0.05) | 0.01 (0.05) | 0.09 (0.05) |
| Some college (13–15) | 0.06 (0.06) | 0.12 (0.08) | −0.01 (0.07) | 0.23 (0.04) |
| College degree or greater (≥16) | 0.14 (0.09) | 0.13 (0.10) | −0.04 (0.08) | 0.41 (0.10) |
| NS | *** | NS | *** | |
| Household income ($) | ||||
| <15,000 | −0.16 (0.05) | −0.05 (0.07) | 0.08 (0.04) | −0.13 (0.05) |
| 15,000–34,999 | −0.08 (0.06) | −0.07 (0.05) | −0.01 (0.04) | −0.12 (0.04) |
| 35,000–74,999 | 0.11 (0.04) | 0.13 (0.04) | −0.08 (0.04) | 0.08 (0.05) |
| ≥75,000 | 0.27 (0.05) | 0.01 (0.07) | 0.00 (0.05) | 0.28 (0.06) |
| *** | ** | NS | *** | |
| Language used when thinking | ||||
| Spanish all or most of the time | −0.14 (0.04) | −0.07 (0.04) | −0.13 (0.05) | −0.21 (0.03) |
| Spanish and English equally | 0.07 (0.05) | −0.08 (0.07) | 0.20 (0.06) | 0.01 (0.07) |
| English all or most of the time | 0.16 (0.07) | 0.03 (0.07) | 0.14 (0.04) | 0.21 (0.04) |
| ** | NS | *** | *** | |
| Spanish language proficiency | ||||
| Excellent or good | 0.00 (0.03) | 0.03 (0.03) | −0.01 (0.04) | −0.02 (0.03) |
| Fair or poor | −0.06 (0.06) | −0.17 (0.04) | 0.06 (0.04) | −0.06 (0.04) |
| NS | *** | NS | NS | |
| Spanish proficiency/Language used when thinking | ||||
| Spanish excellent/good, English all or most of the time when thinking | 0.17 (0.08) | 0.08 (0.09) | 0.20 (0.06) | 0.26 (0.06) |
| Spanish excellent or good, English and Spanish when thinking | 0.10 (0.04) | −0.04 (0.10) | 0.13 (0.08) | −0.04 (0.07) |
| Spanish excellent or good, Spanish all or most of the time when thinking | −0.09 (0.05) | 0.01 (0.04) | −0.13 (0.06) | −0.16 (0.04) |
| Spanish fair or poor, English all or most of the time when thinking | 0.14 (0.08) | −0.02 (0.08) | 0.09 (0.07) | 0.15 (0.06) |
| Spanish fair or poor, English and Spanish when thinking | −0.09 (0.20) | −0.33 (0.09) | 0.50 (0.17) | 0.06 (0.14) |
| Spanish fair or poor, Spanish all or most of the time when thinking | −0.27 (0.07) | −0.38 (0.09) | −0.15 (0.08) | −0.40 (0.08) |
| *** | *** | *** | *** |
Means adjusted for sex and age. SE shown in parentheses.
NS = non-significant,
p < 0.05,
p < 0.01,
p < 0.001, for significance of association of domain with scale.
Table 3.
Ordered Logistic Regression Models (Coefficients with 95% Confidence Intervals) for Self-rated Physical Health of U.S. Latinos.
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Social connection scales | |||
| Family support | 0.12 [0.01, 0.23]* | 0.12 [0.02, 0.21]* | 0.09 [0.00, 0.19] |
| Friend support | 0.12 [0.02, 0.21]* | NS | NS |
| *** | * | NS | |
| Female | −0.43 [−0.59, −0.26]*** | −0.39 [−0.55, −0.23]*** | –0.39 [−0.55, −0.23]*** |
| Age (y) | |||
| 18–24 | 0 | 0 | 0 |
| 25–34 | −0.08 [−0.28, 0.12] | −0.18 [−0.40, 0.04] | −0.22 [−0.46, 0.02] |
| 35–49 | −0.77 [−1.17, −0.37]*** | −0.35 [−0.64, −0.05]* | −0.38 [−0.70, −0.05]* |
| 50–64 | −1.36 [−1.93, −0.79]*** | −0.74 [−1.14, −0.34]*** | −0.82 [−1.20, −0.44]*** |
| ≥65 | −1.36 [−1.93, −0.79]*** | −1.03 [−1.55, −0.51]*** | −1.04 [−1.65, −0.43]** |
| *** | *** | *** | |
| Marital status | |||
| Married | 0 | 0 | 0 |
| Divorced/separated/widowed | −0.32 [−0.58, −0.05]* | −0.22 [−0.46, 0.02] | −0.17 [−0.44, 0.10] |
| Never married | −0.19 [−0.35, −0.04]* | −0.08 [−0.22, 0.06] | −0.07 [−0.20, 0.06] |
| * | NS | NS | |
| Foreign born | −0.08 [−0.31, 0.15] | 0.12 [−0.07, 0.31] | 0.22 [−0.04, 0.48] |
| Subethnicity | |||
| Puerto Rican | −0.14 [−0.44, 0.17] | −0.12 [−0.41, 0.17] | −0.19 [−0.48, 0.10] |
| Cuban | 0.33 [0.06, 0.61]* | 0.21 [−0.05, 0.46] | 0.21 [−0.04, 0.46] |
| Mexican | −0.52 [−0.82, −0.22]** | −0.33 [−0.62, −0.04]* | −0.30 [−0.60, −0.01]* |
| Other Latino | 0 | 0 | 0 |
| *** | * | * | |
| Education (y) | |||
| No high school (<9) | 0 | 0 | |
| Some high school (<12) | 0.44 [0.12, 0.77]** | 0.30 [−0.05, 0.64] | |
| High school graduate (12) | 0.61 [0.35, 0.88]*** | 0.39 [0.09, 0.69]* | |
| Some college (13–15) | 0.77 [0.52, 1.02]*** | 0.54 [0.30, 0.78]*** | |
| College degree or greater (≥16) | 1.12 [0.81, 1.42]*** | 0.78 [0.42, 1.15]*** | |
| *** | *** | ||
| Household income ($) | |||
| <15,000 | 0 | 0 | |
| 15,000–34,999 | 0.25 [0.02, 0.49]* | 0.24 [0.00, 0.47] | |
| 35,000–74,999 | 0.26 [0.04, 0.47]* | 0.26 [0.04, 0.47]* | |
| ≥75,000 | 0.50 [0.30, 0.70]*** | 0.51 [0.24, 0.78]*** | |
| *** | ** | ||
| Language of interview | |||
| Spanish | −0.04 [−0.32, 0.23] | ||
| Spanish proficiency/Language used when thinking | |||
| Spanish excellent/good, English all or most of the time when thinking | 0.28 [0.01, 0.55]* | ||
| Spanish excellent or good, English and Spanish when thinking | 0.13 [−0.13, 0.38] | ||
| Spanish excellent or good, Spanish all or most of the time when thinking | 0.05 [−0.35, 0.46] | ||
| Spanish fair or poor, English all or most of the time when thinking | 0 | ||
| Spanish fair or poor, English and Spanish when thinking | −0.61 [−1.09, −0.12]* | ||
| Spanish fair or poor, Spanish all or most of the time when thinking | −0.74 [–1.26, −0.22]** | ||
| *** | |||
NS = non-significant,
p < 0.05,
p < 0.01,
p < 0.001. Significance of domain indicated below domain variables.
Table 4.
Ordered Logistic Regression Models (Coefficients with 95% Confidence Intervals) of Self-rated Mental Health of U.S. Latinos.
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| Demographics Model | Demographics and SES Model | Demographics, SES, and Language Model | ||||
| Social connection scales | ||||||
| Family support | 0.13 [0.02, 0.24]* | 0.12 [0.02, 0.23]* | 0.15 [0.06, 0.24]** | |||
| Family cultural conflict | −0.17 [−0.31, −0.04]* | −0.18 [−0.32, −0.04]* | −0.21 [−0.34, −0.08]** | |||
| Friend support | 0.19 [0.10, 0.27]*** | 0.11 [0.04, 0.18]** | NS | |||
| *** | *** | *** | ||||
| Female | −0.25 [−0.41, −0.09]** | −0.22 [−0.39, −0.05]* | −0.20 [−0.36, −0.03]* | |||
| Age (y) | ||||||
| 18–24 | 0 | 0 | 0 | |||
| 25–34 | 0.09 [−0.12, 0.30] | −0.02 [−0.26, 0.21] | 0.02 [−0.26, 0.30] | |||
| 35–49 | −0.07 [−0.33, 0.20] | −0.17 [−0.47, 0.12] | −0.11 [−0.46, 0.23] | |||
| 50–64 | −0.28 [−0.68, 0.12] | −0.31 [−0.77, 0.14] | −0.28 [−0.68, 0.12] | |||
| ≥65 | −0.33 [−0.88, 0.22] | −0.07 [−0.61, 0.46] | 0.01 [−0.55, 0.56] | |||
| * | NS | NS | ||||
| Marital status | ||||||
| Married | 0 | 0 | 0 | |||
| Divorced/separated/widowed | −0.26 [−0.59, 0.07] | −0.17 [−0.50, 0.17] | −0.11 [−0.47, 0.25] | |||
| Never married | −0.32 [−0.58, −0.06]* | −0.27 [−0.52, −0.03]* | −0.20 [−0.41, 0.02] | |||
| NS | NS | NS | ||||
| Foreign born | −0.22 [−0.38, −0.07]** | 0.01 [−0.13, 0.15] | 0.30 [0.10, 0.50]** | |||
| Subethnicity | ||||||
| Puerto Rican | −0.16 [−0.48, 0.15] | −0.14 [−0.45, 0.17] | −0.22 [−0.54, 0.09] | |||
| Cuban | −0.09 [−0.37, 0.20] | −0.22 [−0.50, 0.05] | −0.27 [−0.54, 0.01] | |||
| Mexican | −0.46 [−0.76, −0.16]** | −0.28 [−0.56, 0.01] | −0.32 [−0.60, −0.04]* | |||
| Other Latino | 0 | 0 | 0 | |||
| * | NS | NS | ||||
| Education (y) | ||||||
| No high school (<9) | 0 | 0 | ||||
| Some high school (<12) | 0.29 [−0.01, 0.58] | 0.09 [−0.23, 0.40] | ||||
| High school graduate (12) | 0.63 [0.27, 0.98]*** | 0.45 [0.11, 0.78]* | ||||
| Some college (13–15) | 0.95 [0.63, 1.27] *** | 0.71 [0.40, 1.03] *** | ||||
| College degree or greater (≥16) | 1.08 [0.65, 1.52]*** | 0.82 [0.40, 1.25]*** | ||||
| *** | *** | |||||
| Household income ($) | ||||||
| <15,000 | 0 | 0 | ||||
| 15,000–34,999 | 0.22 [−0.05, 0.49] | 0.21 [−0.05, 0.48] | ||||
| 35,000–74,999 | 0.11 [−0.21, 0.43] | 0.07 [−0.25, 0.40] | ||||
| ≥75,000 | 0.37 [0.00, 0.75] | 0.30 [−0.11, 0.70] | ||||
| * | NS | |||||
| Language of interview | ||||||
| Spanish | −0.30 [−0.59, −0.01]* | |||||
| Spanish proficiency/Language used when thinking | ||||||
| Spanish excellent/good, English all or most of the time when thinking | 0.57 [0.25, 0.90]** | |||||
| Spanish excellent or good, English and Spanish when thinking | 0.46 [0.17, 0.75]** | |||||
| Spanish excellent or good, Spanish all or most of the time when thinking | 0.11 [−0.34, 0.57] | |||||
| Spanish fair or poor, English all or most of the time when thinking | 0 | |||||
| Spanish fair or poor, English and Spanish when thinking | 0.45 [−0.32, 1.21] | |||||
| Spanish fair or poor, Spanish all or most of the time when thinking | −0.70 [−1.14, −0.25]** | |||||
| *** | ||||||
NS = non-significant,
p < 0.05,
p < 0.01,
p < 0.001. Significance of domain indicated below domain variables.
Figure 1.
Mean Self-rated Physical Health by Spanish Proficiency, Language Used When Thinking, and Language of Interview, Adjusted for Sociodemographic Variables.
Figure 2.
Mean Self-rated Mental Health by Spanish Proficiency, Language Used When Thinking, and Language of Interview, Adjusted for Sociodemographic Variables.
Results
Descriptive results
The weighted sample population included almost equal numbers of males and females with about half younger than 35 years of age (Table 1). A quarter of the population had less than nine years of education, with only 10% reporting a college degree or more. The population was also predominantly low to middle income with 56% making less than $35,000 per year. The majority were foreign born (59%), with 57% identifying their ethnicity as Mexican. Over half (54%) of the weighted sample interviewed in Spanish, and a similar percentage (54%) reported using Spanish when thinking all or most of the time, whereas about 70% reported excellent or good Spanish proficiency. Table 1 also shows the cross-tabulation of Spanish proficiency and language used when thinking. Given that the majority of the population were immigrants, it was not surprising that the largest cell (42%) was persons with excellent or good Spanish and thinking in Spanish all or most of the time. More surprising was that 11% of the population reported fair or poor Spanish but thinking in Spanish all or most of the time. For self-rated physical health and mental health, 28% rated themselves in poor or fair physical health and 12% rated themselves as having poor or fair mental health.
Table 2 shows mean values of the neighborhood social cohesion, family support, family cultural conflict, and friend support scales (adjusted by sex and age) by categories of self-rated physical and mental health, education, income, and language variables. Self-rated physical health had highly significant (p < 0.001) associations with both the social cohesion and friend support scale; persons with lower scale scores tended to report worse physical health. Associations with the other scales were also significant, but much less so. Self-rated mental health had highly significant (p < 0.01) associations with all four scales, with the strongest associations for family and friend support. Education was significantly related only to family and friend support. Household income was significantly associated with all scales except family cultural conflict.
The association with language is best examined by looking at the 6 category combination of Spanish proficiency and language used when thinking. This combined language measure was strongly associated (p < 0.001) with each of the scales. Persons who described their Spanish as fair or poor and yet thought in Spanish all or most of the time (11% of the population; see Table 1) reported the lowest scores on the social cohesion, family support, and friend support scales. Persons who described their Spanish as fair or poor and thought in English and Spanish reported the highest levels of family cultural conflict. This group was mostly comprised of U.S. born (60%) and immigrants who arrived in the U.S. before age 18 (31%), likely representing individuals raised in a family where Spanish was mostly or exclusively spoken who simultaneously experience a high degree of acculturation to U.S. society outside the home.
As expected, there were strong correlations among most of the social connection variables: social cohesion was significantly correlated (p < 0.001) with family support (r = 0.18), family cultural conflict (r = −0.17), and friend support (r = 0.19). Family support was significantly correlated (p < 0.001) with family cultural conflict (r = −0.19) and friend support (r = 0.28). The only non-significant correlation was between family cultural conflict and friend support (r = −0.01), which may indicate that friend support occurs across all levels of family conflict, in some cases exacerbating or resulting from family conflict and in others concomitant with family cultural values
Regression results
Tables 3 and 4 each present three order logistic regressions models, one for self-rated physical health and the other for mental health. In each table, the first model includes the social connection variables and demographic variables (sex, age, marital status, nativity, and subethnicity); the second adds education and income; and the third includes language variables. Because of the high correlations among social connection scales, we dropped non-significant scales from the models.
Self-rated physical health
In the first model in Table 3, only family and friend support scales have a significant association with self-rated physical health, after controlling for demographic characteristics. Although the social cohesion scale is significant in the first model without the other scales, it is non-significant after the inclusion of family and friend support scales. This finding indicates that the association of self-rated physical health and social cohesion is likely due to the association between social cohesion and family and friend support (or an association with an unmeasured common factor). When family cultural conflict is put in the model without the other scales, it is marginally non-significant (p = 0.06).
When education and income are added in Model 2 (both significant at p < 0.001), the friend support scale becomes non-significant. The apparent effect of friend support in Model 1 was likely due to its strong association with education and income (see Table 2). Again, social cohesion, if entered in Model 2 without family support, is significant.
Once the language variables are entered in Model 3, however, the family support scale becomes marginally non-significant (p = 0.06). Similarly, social cohesion becomes non-significant with the addition of the language variables when it is the only scale in the model. In Table 2, we saw all scales (controlled only for sex and age) significantly associated with self-rated physical health. But in the final model of Table 3, the scales are neither singly nor jointly significant. In this dataset, the strongest associations of self-rated physical health are with education, income, and language (as well as sex and age), and associations with social connection scales were only manifest when these variables were not fully controlled for.
For self-rated physical health, language of interview is not significant. However, those with poor or fair Spanish proficiency who thought mostly in Spanish or in English and Spanish equally had significant negative associations with self-rated physical health. Jointly, the Spanish proficiency and language of thinking terms are highly related to self-rated physical health (p < 0.001). Interestingly, the coefficient estimates for the sociodemographic variables change very little from Models 2 and 3, suggesting that the effects of language are independent of other predictors, notably education and income.
Self-rated mental health
In the models for self-rated mental health in Table 4, family support and family cultural conflict are significant in all three models. Friend support becomes nonsignificant in Model 3 when family support and family cultural conflict scales are included, despite being highly significant in Models 1 and 2. The spurious association between friend support and mental health seen in Models 1 and 2 (and Table 2) is likely due to friend support being strongly associated with the stronger predictors of education and language. Social cohesion is not significant in any of the three models when the other scales are included. When social cohesion is included without any other scales, it is highly significant in Model 1 (p = 0.004), significant (p = 0.02) in Model 2, and nonsignificant in Model 3.
Spanish language of interview is negative and marginally significant (p = 0.04) in Model 3 of Table 4. As with physical health, the joint test of the Spanish proficiency and language of thinking terms are highly significant (p < 0.001). Those who think in Spanish and rate themselves as poor or fair Spanish speakers are associated with poorer self-rated mental health (p < 0.01). In contrast, those who have excellent or good Spanish proficiency and think in English or in English and Spanish equally are associated with better self-rated mental health (p < 0.01). In contrast to physical health, we see here that sex has a weaker, but still significant association; age is not significant; nativity is highly significant; and income is not significant. The nativity term shifts directionality across the models, from negative in Model 1, near zero in Model 2 and positive in Model 3.
Tests of interactions
Interactions between nativity and the social connection scale variables were analyzed in other models and found to be non-significant (data not shown). Interactions between the language proficiency and language of thinking variables and the scales were also analyzed and found to be non-significant. Hence, there was no evidence to suggest that the scales affected the outcomes differentially in the U.S. born than the foreign born or among the different language groups.
Language of interview
Since language of interview is highly collinear with the language proficiency and language of thinking variables, language of interview may interact with the other language terms in Tables 3 and 4, explaining some of the effects seen. Hence, models were fit with language of interview fully interacted by the other language terms. Since results are best seen graphically, linear regressions were used so that adjusted means could be plotted (results were statistically no different from ordered logistic regressions that were also run). Figure 1 for self-rated physical health corresponds to Model 3 of Table 3, and Figure 2 for self-rated mental health corresponds to Model 3 of Table 4. Figures 1 and 2 show that within each of the six categories, language of interview makes little difference to the level of self-rated physical or mental health. Figures 1 and 2 are consistent with the statistical results reported in Tables 3 and 4: language of interview was non-significant for physical health and marginally significant for mental health, whereas Spanish proficiency and language of thinking categories were highly significant (p < 0.001). In this dataset, the strong language associations seen were not primarily due to the language of interview.
Discussion
Although all social connection scales have a significant relationship with self-rated physical and mental health in bivariate relationships (Table 2), we find no support for our hypothesis that neighborhood social cohesion has an association with self-rated physical and mental health, independent of the other types of social connection, after accounting for sociodemographic characteristics. It appears that for both self-rated physical and mental health, the healthful effects of social connection are primarily experienced through individual-level (e.g., family and friend support) rather than community-level social connections, according to the results of this analysis. These findings suggest caution when using community level variables to explain patterns of health and social connection for Latinos (Portes, 1998), and suggest that individual-level connections may more accurately represent the vehicles through which Latinos experience health benefits.
Self-rated physical health
Overall rates of poor or fair physical health are similar to other studies of self-rated physical health among Latinos, who tend to rate their health poorer than whites (Browning, Cagney, & Wen, 2003). All social connection scales are significantly associated with self-rated physical health in the bivariate relationships, although only family support and friend support are significant in the multivariate model (Table 3, Model 1). However, these relationships disappear once both SES and language variables are entered into the model. For physical health, not only is there no independent relationship between neighborhood social cohesion and health, but the SES and language variables appear to mediate the relationship between family and friend support and self-rated physical health.
Given the strength of the associations of the language variables in the bivariate relatonships, and the fact that once the language variables are added into the regression model, none of the social connection variables are significant, it seems that the social connections related to physical health for Latinos are also closely tied to language capabilities. Despite much emphasis on the health producing effects of family connections for Latino families, we find a marginally non-significant effect of family support once we consider language. The complex Spanish proficiency construct included in this analysis appears to be a proxy for a particular pattern of connection that facilitates general physical health. Including language of thinking as part of the measure of language proficiency seems to capture a deeper level of how these respondents make sense of the world, one that also seems to be strongly related to health. Of particular interest are those who speak Spanish well and use English all or most of the time when thinking. This bilingual group reports better self-rated health, suggesting that bilingualism may play a role in positive health, perhaps through facilitating access to services and other resources.
The subset of the sample who rate themselves as poor or fair Spanish speakers but think in Spanish or think in English and Spanish equally are far more likely to report poor or fair physical health than other language groups. Possible explanations include an interview distortion effect across all the rating scales whereby this group is more likely to answer poor/fair across all scales (the self-rated health scales and the language rating scales). Self-rated health measures tend to be rated lower by non-English speaking, immigrant Latinos compared to more acculturated Latinos (Finch & Vega, 2003; Franzini & Fernandez-Esquer, 2004). According to the interview distortion hypothesis, these low rates may have less to do with how this group views their health and more with how they respond to Likert-scaled questions in general. The fact that there were no significant differences in self-rated health across language of interview implies that this possible effect is independent of the language in which the question is asked, suggesting this pattern of response is also not due to differences in how the question was translated from English to Spanish.
Alternately, this group may represent socially impaired Latinos who do not function well within either predominately Latino or other mixed communities. Self-rated health measures may express “social” health for Latinos and thus could be picking up perceived social standing in the community (Franzini & Fernandez-Esquer, 2004). Previous analyses of the self-rated health measure support this theory, as the measure better captures overall health than disease specific medical status (Idler & Benyamini, 1997). Poor or fair Spanish speakers who think mostly in Spanish or in Spanish and English may represent Latino immigrants from indigenous backgrounds who have a language other than English or Spanish as a first language, individuals who suffer from cognitive impairments or other learning disabilities, or individuals who are socially marginalized. They may have low health literacy and consequently have difficulty accessing services and thus lower self-rated health (Sarfaty, Turner, & Damotta, 2005). It is a limitation of the NLAAS survey that data were not collected on other languages spoken, and thus we cannot explore further whether these individuals speak another first language. It would be important to look closely at this group in future analyses to better understand the links between health, language and social connections.
Self-rated mental health
As expected, the family variables are significantly associated with self-rated mental health. Family support shows statistical significance across all three models shown in Table 4, suggesting that the relationship between family support and self-rated mental health is robust. Further, our analyses suggest a strong protective effect of family support regardless of SES or language status.
Interestingly, although friend support is associated with self-rated mental health in the first two models, it looses its significance after adding the language variables. Language ability appears to influence the social connections through which one acquires positive health and mental health benefits. Similar to the physical health model, the language variables expose a vulnerable group of Latinos who rate themselves as poor or fair Spanish speakers and have a negative association with self-rated mental health. These variables may be capturing the negative effects of insular relationships in poor isolated communities. Alternately, they could be proxies for stressful experiences, such as employment vulnerability and fear of deportation (Hovey & Magana, 2002; Sullivan & Rehm, 2005) or overt discrimination, sometimes even experienced in immigrants' country of origin before arriving in the United States (McGuire & Georges, 2003).
For the mental health model, we also observe two groups with good or excellent Spanish speaking abilities who think all or some of the time in English that have a strong and positive relationship with self-rated mental health. There appears to be something protective for broad mental health about maintaining Spanish language capacity, possibly indicative of wider social connections. A small study found that children who preferred to speak both English and Spanish had higher rates of familism than those who spoke Spanish only (Romero, Robinson, Haydel, Mendoza, & Killen, 2004). The positive mental health effect for those who think in English but maintain strong Spanish speaking capabilities requires further research.
Despite positive correlations of other social connection variables with self-rated mental health, neighborhood social cohesion is not significantly related. These findings are consistent with a recent study which also found no association between social cohesion and self-rated mental health (Harpham, Grant, & Rodriguez, 2004). The strength of the association of income and education with self-rated physical health, and of education with self-rated mental health, suggests that greater attention should be paid to how structural factors determine access to health. Recent work looking at the link between SES and health for minorities finds that neighborhood resources via more affluent neighbors has a strong, positive effect on health status for minorities (Browning, Cagney, & Wen, 2003).
Conclusion
With the exception of the association between mental health and both family support and family conflict, language and other sociodemographic factors appear to be strongly associated with how Latinos establish social linkages. The fact that neighborhood social cohesion did not play a role in facilitating physical or mental health could be due to the individual level measurement of this variable. More objective measures of social cohesion might find a unique community level effect for self-rated physical and mental health. However, our results are consistent with another recent study that included objective measures of social cohesion and found no relationship with mortality levels (Wen, Cagney, & Christakis, 2005). It is important to note that the social connection scales measure perceptions of support, and the dependent variables of interest are also based on the respondents' subjective perceptions. Those who perceive themselves to have higher levels of social connection may also simply perceive themselves to be in good physical or mental health. Our findings are limited by the cross-sectional design of the study. The direction of causality cannot be inferred by associations, and those who are healthier may simply be more able to develop positive social connections.
The language categories included in this study also do not represent simple proxies of high, medium and low acculturation. For example, it is not clear whether someone who speaks Spanish well and thinks in Spanish and English would be more or less “acculturated” than someone who speaks fair or poor Spanish and uses Spanish and English equally when thinking. The significance of the relationship of language to self-rated physical and mental health in this exploratory analysis suggests that understanding these relationships will require a more refined investigation of the role of language as a marker for acculturation and as a mechanism for accessing health resources. Further, it would be important to expand analyses of these language groups to consider the characteristics of those within these groups. Qualitative work could distinguish potential artifactual explanations from actual levels of health impairment for poor or fair Spanish speakers.
Acknowledgments
The NLAAS data used in this analysis were provided by the Center for Multicultural Mental Health Research at the Cambridge Health Alliance. The project was supported by NIH Research Grant # U01 MH62209 funded by the National Institute of Mental Health and SAMHSA/CMHS and OBSSR. We would like to thank four anonymous reviewers for very helpful comments. We also thank Antonio Polo for helpful comments in the interpretation of the analysis, and Vanessa Oddo for her assistance with manuscript preparation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Margarita Alegria, Cambridge Health Alliance, Harvard Medical School, Somerville, MA UNITED STATES malegria@charesearch.org
William Sribney, Third Way Statistics, Somerville, MA UNITED STATES bill@thirdwaystat.com
Dr. Norah E. Mulvaney-Day, Cambridge Health Alliance, Harvard Medical School Somerville, MA UNITED STATES, nmulvaney-day@charesearch.org
References
- Abraido-Lanza A, Chao M, Florez K. Do healthy behaviors decline with great acculturation?: Implications for the Latino mortality paradox. Social Science & Medicine. 2005;61:1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler N, Newman K. Socioeconomic Disparities in Health : Pathways and Policies. Health Affairs. 2002;21(2):60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- Albizu-García C, Alegría M, Freeman D, Vera M. Gender and Health Service Use for Mental Health Problems. Social Science & Medicine. 2001;53:863–878. doi: 10.1016/s0277-9536(00)00380-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Takeuchi D, Canino G, Duan N, Shrout P, Meng X, Vega W, Zane N, Vila D, Woo M, Vera M, Guarnaccia P, Aguilar-Gaxiola S, Sue S, Escobar J, Lin K, Gong F. Considering Context, Place and Culture: the National Latino and Asian American Study. International Journal of Methods in Psychiatric Research. 2004;13(4):208–220. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Stinson F, Grant B. Nativity and DSM-IV psychiatric disorders among Puerto Ricans, Cuban Americans and non-Latino Whites in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67(1):56–65. doi: 10.4088/jcp.v67n0109. [DOI] [PubMed] [Google Scholar]
- Alegría M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of Psychiatric Disorders Across Latino Subgroups in the United States. American Journal of Public Health. doi: 10.2105/AJPH.2006.087205. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aneshensel C, Rutter C, Lachenbruch P. Social structure, stress, and mental health: Competing conceptual and analytic models. American Sociological Review. 1991;56:166–178. [Google Scholar]
- Bearman J, Jones J, Udry R. The national longitudinal study of adolescent health. Chapel Hill, NC: Carolina Population Center; 1997. [Google Scholar]
- Bird H, Canino G, Davies M, Zhang H, Ramirez R, Lahey B. Prevalence and correlates of antisocial behaviors among three ethnic groups. Journal of Abnormal Child Psychology. 2001;29(6):465–478. doi: 10.1023/a:1012279707372. [DOI] [PubMed] [Google Scholar]
- Borrayo E, Jenkins S. Feeling Frugal: Socioeconomic Status, Acculturation, and Cultural Health Beliefs Among Women of Mexican Descent. Cultural Diversity and Ethnic Minority Psychology. 2003;9(2):197–206. doi: 10.1037/1099-9809.9.2.197. [DOI] [PubMed] [Google Scholar]
- Breslau J, Aguilar-Gaxiola S, Kendler K, Su M, Williams D, Kessler R. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychological Medicine. 2006;35:1–12. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning C, Cagney K. Neighborhood structural disadvantage, collective efficacy, and self-rated physical health in an urban setting. Journal of Health & Social Behavior. 2002;43(4):383–399. [PubMed] [Google Scholar]
- Browning C, Cagney K, Wen M. Explaining Variation in Health Status Across Space and Time: Implications for Racial and Ethnic Disparities in Self-Rated Health. Social Science & Medicine. 2003;57:1221–1235. doi: 10.1016/s0277-9536(02)00502-6. [DOI] [PubMed] [Google Scholar]
- Caughy M, O'Campo P, Mutaner C. When being alone might be better: neighborhood poverty, social capital, and child mental health. Social Science & Medicine. 2003;57:227–237. doi: 10.1016/s0277-9536(02)00342-8. [DOI] [PubMed] [Google Scholar]
- Cervantes R, Padilla A, Salgado de Snyder W. The Hispanic Stress Inventory: A culturally relevant approach to psychological assessment. Psychological Assessment. 1991;3:438–447. [Google Scholar]
- Chandola T, Jenkinson C. Validating self-rated health in different ethnic groups. Ethnicity and Health. 2000;5(2):151–159. doi: 10.1080/713667451. [DOI] [PubMed] [Google Scholar]
- Finch B, Hummer R, Reindl M, Vega W. Validity of self-rated health among Latino(a)s. American Journal of Epidemiology. 2002;155(8):755–759. doi: 10.1093/aje/155.8.755. [DOI] [PubMed] [Google Scholar]
- Finch B, Vega W. Acculturation stress, social support, and self-rated health among Latinos in California. Journal of Immigrant Health. 2003;5(3):109–117. doi: 10.1023/a:1023987717921. [DOI] [PubMed] [Google Scholar]
- Franzini L, Ribble J, Keddie A. Understanding the Hispanic paradox. Ethnicity and Disease. 2001;11(3):496–518. [PubMed] [Google Scholar]
- Franzini L, Fernandez-Esquer M. Socioeconomic, cultural, and personal influences on health outcomes in low income Mexican-origin individuals in Texas. Social Science & Medicine. 2004;59(8):1629–1646. doi: 10.1016/j.socscimed.2004.02.014. [DOI] [PubMed] [Google Scholar]
- Galea S, Vlahov D, Tracy M, Hoover D, Resnick H, Kilpatrick D. Hispanic ethnicity and post-traumatic stress disorder after a disaster: evidence from a general population survey after September 11, 2001. Annals of Epidemiology. 2004;14(8):520–531. doi: 10.1016/j.annepidem.2004.01.006. [DOI] [PubMed] [Google Scholar]
- Gonzalez H, Haan M, Hinton L. Acculturation and the Prevalence of Depression in Older Mexican Americans: Baseline Results of the Sacramento Area Latino Study on Aging. J Am Geriatr Soc. 2001;49:948–953. doi: 10.1046/j.1532-5415.2001.49186.x. [DOI] [PubMed] [Google Scholar]
- Haas J, Phillips K, Sonneborn D, McCulloch C, Baker L, Kaplan C, Perez-Stable E, Liang S. Variation in Access to Health Care for Different Racial/Ethnic Groups by the Racial/Ethnic Composition of an Individual's County of Residence. Medical Care. 2004;42(7):707–714. doi: 10.1097/01.mlr.0000129906.95881.83. [DOI] [PubMed] [Google Scholar]
- Hagan J, MacMillan R, Wheaton B. New Kid in Town: Social Capital and the Life Course Effects of Family Migration on Children. American Sociological Review. 1996;61(June):368–385. [Google Scholar]
- Harpham T, Grant E, Rodriguez C. Mental health and social capital in Cali, Colombia. Social Science & Medicine. 2004;58(11):2267–2277. doi: 10.1016/j.socscimed.2003.08.013. [DOI] [PubMed] [Google Scholar]
- Hendryx M, Ahern M. Access to mental health services and health sector social capital. Administration and Policy in Mental Health. 2001;28(3):205–218. doi: 10.1023/a:1007860002137. [DOI] [PubMed] [Google Scholar]
- Heeringa S, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) International Journal of Methods in Psychiatric Research. 2004;13(4):221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovey J, Magana C. Cognitive, Affective, and Physiological Expressions of Anxiety Symptomatology Among Mexican Migrant Farmworkers: Predictors and Generational Differences. Community Mental Health Journal. 2002;38(3):223–237. doi: 10.1023/a:1015215723786. [DOI] [PubMed] [Google Scholar]
- Hunninghake G, Weiss S, Celedon J. Asthma in Hispanics. American Journal of Respiratory and Critical Care Medicine. 2006;173(2):143–163. doi: 10.1164/rccm.200508-1232SO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt L, Schneider S, Comer B. Should “acculturation” be a variable in health research? A critical review of research on US Hispanics. Social Science & Medicine. 2004;59:973–986. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- Idler E, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health & Social Behavior. 1997;38(1):21–37. [PubMed] [Google Scholar]
- Kawachi I, Berkman L. Social Cohesion, Social Capital, and Health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. Oxford University Press; 2000. pp. 174–190. [Google Scholar]
- Kessler R, Berglund P, Demler O, Jin R, Koretz D, Merikangas K, Rush J, Walters E, Wang P. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) Journal of the American Medical Association. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Korn E, Graubard B. Simultaneous Testing of Regression Coefficients with Complex Survey Data: Use of Bonferroni t Statistics. American Statistician. 1990;44(4):270–276. [Google Scholar]
- Lochner K, Kawachi I, Brennan R, Buka S. Social capital and neighborhood mortality rates in Chicago. Social Science & Medicine. 2003;56:1797–1805. doi: 10.1016/s0277-9536(02)00177-6. [DOI] [PubMed] [Google Scholar]
- Lopez S, Nelson H, Polo A, Jenkins J, Karno M, Vaughn C, Snyder K. Ethnicity, expressed emotion, attributions, and course of schizophrenia: family warmth matters. Journal of Abnormal Psychology. 2004;113(3):428–439. doi: 10.1037/0021-843X.113.3.428. [DOI] [PubMed] [Google Scholar]
- Macinko J, Starfield B. The utility of social capital in research on health determinants. Milbank Quarterly. 2001;79(3):387–427. doi: 10.1111/1468-0009.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullagh P, Nelder J. Generalized Linear Models. London: Chapman and Hall; 1989. [Google Scholar]
- McGlade M, Saha S, Dahlstrom M. The Latina Paradox: An Opportunity for Restructuring Prenatal Care Delivery. American Journal of Public Health. 2004;94(12):2062–2065. doi: 10.2105/ajph.94.12.2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire S, Georges J. Undocumentedness and Liminality as Health Variables. Advances in Nursing Science. 2003;26(3):185–195. doi: 10.1097/00012272-200307000-00004. [DOI] [PubMed] [Google Scholar]
- McQueen A, Getz J, Bray J. Acculturation, Substance Use, and Deviant Behavior: Examining Separation and Family Conflict as Mediators. Child Development. 2003;74(6):1737–1750. doi: 10.1046/j.1467-8624.2003.00635.x. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. Cooperative Agreement for a Multi-Site Study of Mental Health Service Use, Need, Outcomes, and Costs in Child and Adolescent Populations (UNO-CAP) In: G.S. Administration, editor. Catalog of Federal Domestic Assistance 93.242-Request for Applications. Rockville, MD: 1994. [Google Scholar]
- Nee V, Sanders J, Sernau S. Job transitions in an immigrant metropolis: ethnic boundries and the mixed economy. American Sociological Review. 1994;59:849–872. [Google Scholar]
- Page R. Positive Pregnancy Outcomes in Mexican Immigrants: What Can We Learn? Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2004;33(6):783–790. doi: 10.1177/0884217504270595. [DOI] [PubMed] [Google Scholar]
- Pasch L, Deardorff J, Tschann J, Flores E, Penilla C, Pantoja P. Acculturation, parent-adolescent conflict, and adolescent adjustment in Mexican American families. Family Process. 2006;45(1):75–86. doi: 10.1111/j.1545-5300.2006.00081.x. [DOI] [PubMed] [Google Scholar]
- Perreira K, Deeb-Sossa N, Mullan Harris K, Bollen K. What are we measuring? And evaluation of the CES-D Across Race/Ethnicity and Immigrant Generation. Social Forces. 2005;83(4):1567–1602. [Google Scholar]
- Portes A. The social origins of the Cuban enclave economy of Miami. Sociological Perspective. 1987;30:340–372. [Google Scholar]
- Portes A, Kyle D, Eaton WW. Mental illness and help-seeking behavior among Mariel Cuban and Haitian refugees in South Florida. Journal of Health & Social Behavior. 1992;33(4):283–298. [PubMed] [Google Scholar]
- Portes A. Social Capital: Its Origins and Applications in Modern Sociology. Annual Review of Sociology. 1998;24:1–24. [Google Scholar]
- Portes A, Hao L. Working paper. Center for Migration and Development, Princeton University; 2002. The price of uniformity: Language, family, and personality adjustment in the immigrant second generation. [Google Scholar]
- Putnam R. Bowling Alone. The Collapse and Revival of American Community. New York: Touchstone; 2000. [Google Scholar]
- Reynolds D. Cervical cancer in Hispanic/Latino women. Clinical Journal of Oncology Nursing. 2004;8(2):146–150. doi: 10.1188/04.CJON.146-150. [DOI] [PubMed] [Google Scholar]
- Rodriguez N, Mira C, Myers H, Morris J, Cardoza D. Family or friends: who plays a greater supportive role for Latino college students? Cultural Diversity & Ethnic Minority Psychology. 2003;9(3):236–250. doi: 10.1037/1099-9809.9.3.236. [DOI] [PubMed] [Google Scholar]
- Rohrer J. Medical care usage and self-rated mental health. BMC Public Health. 2004;4(3) doi: 10.1186/1471-2458-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romero A, Robinson T, Haydel K, Mendoza F, Killen J. Associations Among Familism, Language Preference, and Education in Mexican-American Mothers and Their Children. Developmental and Behavioral Pediatrics. 2004;25(1):34–39. doi: 10.1097/00004703-200402000-00006. [DOI] [PubMed] [Google Scholar]
- Rosenheck R. Organizational process: A missing link between research and practice. Psychiatric Services. 2001;52(12):1607–1612. doi: 10.1176/appi.ps.52.12.1607. [DOI] [PubMed] [Google Scholar]
- Rust K, Rao J. Variance estimation for complex surveys using replication techniques. Statistical Methods in Medical Research. 1996;5(3):283–310. doi: 10.1177/096228029600500305. [DOI] [PubMed] [Google Scholar]
- Sampson R, Raudenbush S, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Sarfaty M, Turner C, Damotta E. Use of a Patient Assistant to Facilitate Medical Visits For Latino Patients with Low Health Literacy. Journal of Community Health. 2005;30(4):299–307. doi: 10.1007/s10900-005-3707-2. [DOI] [PubMed] [Google Scholar]
- Sartorius N. Social capital and mental health. Current Opinion in Psychiatry. 2003;16(S2):S101–S105. [Google Scholar]
- Stack C. All Our Kin. New York: Harper & Row; 1974. [Google Scholar]
- Stanton-Salazar R, Dornbusch S. Social Capital and the Reproduction of Inequality : Information Networks among Mexican -origin High School Students. Sociology of Education. 1995;68(April):116–135. [Google Scholar]
- Stata Statistical Software Release 8.2. StataCorp; College Station, TX: Stata Corporation; 2004. [Google Scholar]
- Stuart G, Minas I, Klimidis S, O'Connell S. English language ability and mental health service utilization : a census. Australian & New Zealand Journal of Psychiatry. 1996;30(2):270–277. doi: 10.3109/00048679609076105. [DOI] [PubMed] [Google Scholar]
- Sullivan M. Getting Paid: Youth Crime and Work in the Inner City. Ithaca, NY: Cornell University Press; 1989. [Google Scholar]
- Sullivan M, Rehm R. Mental Health of Undocumented Mexican Immigrants. Advances in Nursing Science. 2005;28(3):240–251. doi: 10.1097/00012272-200507000-00006. [DOI] [PubMed] [Google Scholar]
- Thoits P. Stress, Coping, and Social Support Processes: Where Are We? What Next? Journal of Health & Social Behavior. 1995;35(Extra Issue: Forty Years of Medical Sociology: The State of the Art and Directions for the Future):53–79. [PubMed] [Google Scholar]
- Tschann J, Flores E, Marin B, Pasch L, Baisch EM, Wibbelsman C. Interparental Conflict and Risk Behaviors Among Mexican American Adolescents: A Cognitive-Emotional Model. Journal of Abnormal Child Psychology. 2002;30(4):373–385. doi: 10.1023/a:1015718008205. [DOI] [PubMed] [Google Scholar]
- Vega W, Kolody B, Valle J. Migration and mental health: an empirical test of depression risk factors among immigrant Mexican women. International Migration Review. 1987;21:512–530. [PubMed] [Google Scholar]
- Vega W, Amaro H. Latino outlook: Good health, uncertain prognosis. Annual Review of Public Health. 1994;15:39–67. doi: 10.1146/annurev.pu.15.050194.000351. [DOI] [PubMed] [Google Scholar]
- Vega W, Sribney W, Aguilar-Gaxiola S, Kolody B. 12-month prevalence of DSM-III-R psychiatric disorders among Mexican Americans: nativity, social assimilation, and age determinants. Journal of Nervous and Mental Disorders. 2004;192(8):532–541. doi: 10.1097/01.nmd.0000135477.57357.b2. [DOI] [PubMed] [Google Scholar]
- Wakefield S, Poland B. Family, friend or foe? Critical reflections on the relevance and role of social capital in health promotion and community devlopment. Social Science & Medicine. 2005;60(12):2819–2832. doi: 10.1016/j.socscimed.2004.11.012. [DOI] [PubMed] [Google Scholar]
- Weinick R, Jacobs E, Stone L, Ortega A, Burstin H. Hispanic healthcare disparities: challenging the myth of a monolithic Hispanic population. Medical Care. 2004;42(4):313–320. doi: 10.1097/01.mlr.0000118705.27241.7c. [DOI] [PubMed] [Google Scholar]
- Wen M, Cagney K, Christakis N. Effect of specific aspects of community social environment on the morality of individuals diagnosed with serious illness. Social Science & Medicine. 2005;61(6):1119–1134. doi: 10.1016/j.socscimed.2005.01.026. [DOI] [PubMed] [Google Scholar]