Abstract
Background
There is increasing evidence showing beneficial effects of mindfulness and mindfulness training on various indicators of mental and physical health.
Purpose
This paper reports the 6-month follow-up effects of a mindfulness stress reduction training program among patients treated for cancer on perceived stress, depression, anxiety, post-traumatic stress symptoms, positive states of mind, coping self-efficacy, and mindfulness.
Methods
Patients with a previous cancer diagnosis were recruited and randomized into an intervention group or a waiting-list control group. The intervention consisted of an 8-week mindfulness-training course.
Results
Compared to participants in the control group, the intervention group showed a larger increase in mindfulness at 6-month follow-up. However, there were no differences on any of the other outcomes between the intervention and control groups. Continued meditation practice was associated with a significant reduction in post traumatic stress symptoms of avoidance.
Conclusions
The study draws attention to the need to better understand the mechanisms behind the effect of mindfulness training, and to potential modification of mindfulness interventions to promote sustained benefits over time.
Keywords: Mindfulness, Meditation, Stress reduction, Cancer, Depression, Perceived stress
INTRODUCTION
Receiving a cancer diagnosis is stressful. In addition to the excessive physiological stress caused by the disease and its treatment, many patients experience psychological stress regarding worries about diagnosis and prognosis, demanding treatments, treatment decisions, and disruption of ordinary life functions and roles [1]. A recent US study of long-term cancer survivors reported an increased prevalence of serious psychological distress in cancer survivors even among those who had been disease free for 5 years or more as compared to the general population [2].
The mindfulness-based stress reduction (MBSR) program developed by Jon Kabat-Zinn [3] and his colleagues at the Stress Reduction and Relaxation Clinic, Massachusetts Medical Center has been widely used in medical settings and has been shown to have potential to decrease stress and depression [4–8]. It has shown positive effects on quality of life and decreased stress symptoms in patients with varying cancer diagnoses [9–11]. Studies have also shown promising results of MBSR programs on sleep disturbances among cancer patients [7, 12]. A meta-analysis of the effects of MBSR on different patient groups gives support for the use of MBSR in reducing stress and enhancing quality of life, even though more well-designed studies are needed [7, 13]. The longer-term effect of mindfulness interventions for cancer patients has not been extensively studied. However, a few non-randomized studies have shown initial support for the longer-term effect of mindfulness training [9, 14]. Most of the published studies of the effects of mindfulness meditation with cancer patients have been conducted in North America, used short follow-ups, and only a few studies have used a randomized controlled design [13]. The current study was conducted in Northern Europe and used a randomized controlled study design to extend findings regarding the effects of mindfulness training to a different cultural setting.
The aim of the current paper was to examine the effects of a mindfulness training program for patients treated for cancer delivered in group sessions, using a modified version of the original MBSR-program developed at the Massachusetts Medical Center, six months post-randomization. In a previous report from this study, we found that mindfulness training was associated with significantly decreased perceived stress and post traumatic stress symptoms, and increased mindfulness and positive states of mind at 3-months post-randomization [15]. In this study, we examined the continued effects of mindfulness training on perceived stress, depression, anxiety, post-traumatic stress symptoms, positive states of mind, mindfulness and coping self-efficacy.
METHOD
Study sample and recruitment
Study participants were recruited between April 2007 and March 2008 by advertisement and e-mail list announcements through cancer patient organizations. The study was open to patients with varying cancer diagnoses, who were not undergoing current radiation or chemotherapy treatment. Individuals interested in participation phoned the study coordinator and received more information. If eligible, the participant was randomized to either the intervention group or the waiting-list control group. Random selection of participants to either the intervention or control group was done consecutively using a random sequence of numbers indicating group assignment. Once a participant was recruited to the study, he/she was assigned a study number and was assigned to intervention or control group according to the sequence of numbers. The sequence was produced through SPSS software’s random selection procedure [16]. Questionnaires were sent to the participants by mail directly after randomization, and at three and six months after randomization, together with prepaid return envelopes. The waiting-list participants were scheduled to participate in the intervention program after approximately 6 months. A power calculation was conducted to decide the adequate number of participants. The calculation was based on a similar study of patients treated for cancer by Speca et al. showing an intervention effect with an effect size of 0.6 (Cohen’s d) on symptoms of stress [10]. With an alpha at 0.05 and 80% power we estimated a need to include 40 individuals in each study group. The study was approved by the Ethics Committee of the Karolinska Institute (No. 2007/48-31/2).
Intervention – mindfulness training program
The intervention involved eight two-hour weekly sessions and consisted of experiential and group exercises. The program was a modified version of the program developed by Jon Kabat-Zinn [3] and his colleagues at the Stress Reduction and Relaxation Clinic, Massachusetts Medical Center. The modified program has been described in greater detail in a previous publication [15].
Measures
In addition to information regarding age, gender, education, income, type of cancer diagnosis, time of diagnosis, and current medication, a number of psychosocial measures and a question regarding meditation practice were used at all assessments.
Perceived Stress Scale (PSS)
The PSS is a ten-item scale measuring perception of stressful experiences during the past month [17]. The PSS has previously been used in several different populations. In the current study the internal consistency was 0.83.
Hospital Anxiety and Depression Scale (HADS)
The HADS is a 14-item scale measuring anxiety and depression in non-psychiatric populations and it has been frequently used within the health care setting [18]. It consists of two separate subscales measuring depression and anxiety over the past week. In the current study the internal consistency was 0.86 for the anxiety scale and 0.79 for the depression scale.
Impact of Event Scale Revised (IES-R)
The IES-R is a 22-item scale measuring common post-traumatic stress symptoms and the impact of stressful life events over the past week [19]. It is a revision of the original Impact of Event Scale consisting of two subscales measuring intrusive and avoidant symptoms [20]. The revised version has three subscales measuring: intrusive thinking related to the traumatic event (IES-intrusion), avoidant behavior (IES-avoidance), and emotional arousal (IES-hyperarousal). In the current study the respondents were instructed to relate to their cancer diagnosis as their stressful event and the internal consistency was 0.88 for IES-intrusion, 0.85 for IES-avoidance, and 0.80 for IES-hyperarousal.
Positive States of Minds (PSOM)
The PSOM is a six-item scale measuring different positive emotional and cognitive experiences [21, 22]. It assesses experiences of focused attention, productivity, responsible caretaking, restful repose, sharing, and sensuous nonsexual pleasure. In the current study the internal consistency for the PSOM was 0.77.
Coping Self-Efficacy Scale (CSES)
The CSES is a 26-item measure of people’s confidence in performing coping behaviors when faced with life challenges. The scale was designed for and is especially suitable for intervention research when changes in coping are assumed [23]. The internal consistency for the CSES in this sample was 0.91.
Five Facet Mindfulness Questionnaire (FFMQ)
The FFMQ is a self-report measure of mindfulness developed by Baer and colleges [24]. A recent study of the construct validity of the FFMQ supports the possibility to assess mindfulness by means of self-report, and showed a positive relationship between mindfulness and meditation experience [25]. The Swedish version of the scale has demonstrated adequate psychometric properties in a recent cross-sectional study [26]. In the current study the Cronbach’s alpha coefficients for the total mindfulness score was 0.93. The internal consistencies of the subscales were; observing 0.83, describing 0.95, acting with awareness 0.90, non-judging of inner experience 0.89, and non-reactivity to inner experience 0.83.
Meditation practice
The frequency of meditation practice before and during the study period was assessed with one question. The respondents were to indicate the frequency of meditation practice during the past three months with one of five response alternatives (never, at a few occasions, about once a month, about once a week, several times a week). The question was used to categorize the respondents into three groups, those who meditate regularly (several times a week), moderately (about once a week), and infrequently (once a month or less often).
Statistical analysis
Baseline characteristics of the sample, stratified by experimental group, were examined to ensure that key variables were evenly distributed by randomization. An initial intention-to-treat analysis was conducted with missing data at follow-up imputed according to last-observation-carried-forward strategy. Additionally, a per-protocol analysis was conducted using the data for those who successfully completed both baseline and the 6-month follow-up assessments. Missing data across questionnaire items ranged from 1.4% to 2.8%, and scale means were computed using the mean of available items for each participant. The intervention effect was analyzed using multivariate repeated measures analyses of covariance (MANCOVAs). Two analyses were performed, one with the psychological outcome variables (perceived stress, depression, anxiety, post-traumatic stress symptoms, positive states of mind, and coping self-efficacy) as dependent variables, and one with mindfulness subscales (observing, describing, acting with awareness, non-judging of inner experience, and non-reactivity to inner experience) as dependent variables. Time, group (intervention vs. control) and education were entered as factors in the analyses and age was entered as a covariate. Age and education were entered into the equation as previous research has shown that these factors are important predictors of long-term psychological distress in patients treated for cancer [2]. Spearman’s Rho correlation statistics was used to calculate correlations between frequency of meditation practice and outcome variables.
RESULTS
Study flow and intervention participation
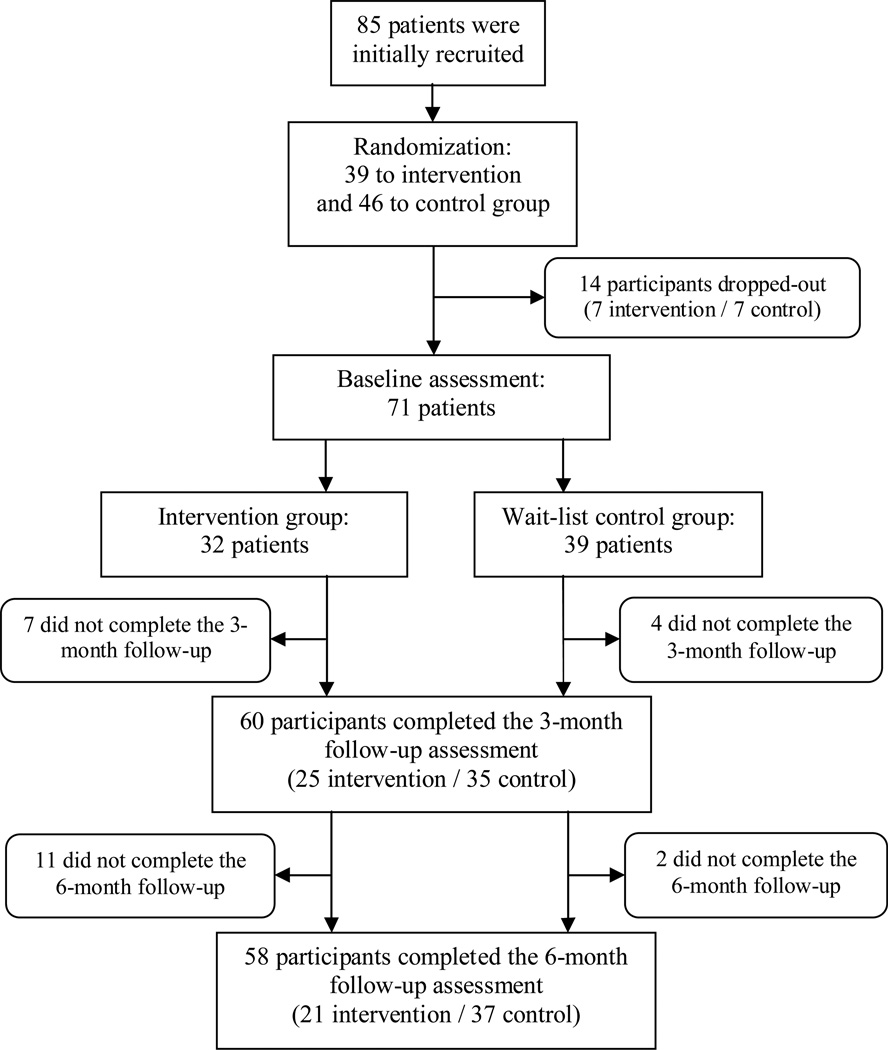
Eighty-five participants agreed to take part in the study and were randomized to either mindfulness training or a waiting-list control group. All participants except one were women. The man was randomized to the control group. Fourteen participants dropped out of the study before returning the baseline assessment, 7 individuals randomized to the intervention group and 7 individuals randomized to the control group, see study flow chart Figure 1. Reasons for dropout were: change of mind before first questionnaire was sent or problems finding a suitable time to participate in the intervention group. Among the remaining participants in the intervention group, eight (25.0%) completed all eight group sessions, seven (21.9%) individuals participated in seven sessions, eight (25.0%) in six sessions, two (6.2%) in five sessions, two (6.2%) in four sessions, three (9.4%) in three sessions, and two (6.2%) participants did not attend any of the sessions. Home practice of meditation during the program was assessed with a question included in the follow-up questionnaire regarding frequency of meditation practice during the program period. Sixty percent of the participants reported regular meditation practice during the intervention period, 28% reported a moderate amount of meditation, and 12% reported infrequent meditation practice. Seven of the 32 participants (21.9%) in the intervention group and four participants in the control group (10.3%) did not return the 3-month follow-up questionnaire, and eleven of the 32 participants (34.4%) in the intervention group and two participants in the control group (5.1%) did not return the 6-month follow-up questionnaire. There were no significant differences between dropouts and the rest of the sample regarding age, education, or income, and no differences in outcome measures at baseline (p>0.10).
Figure 1.
Flow shart describing study recruitment and drop-out.
The current study is based on an intention-to-treat analysis of the results collected among the 71 participants recruited to the study (32 individuals in the intervention group and 39 individuals in the control group) that were randomized and also successfully filled out and returned the baseline questionnaire, and an additional per-protocol analysis of the 58 participants (21 individuals in the intervention group and 37 individuals in the control group) that were randomized and also successfully filled out and returned both baseline and 6-month follow-up questionnaires. In the sample of 71 participants, 54 had been treated for breast cancer, 10 for gynecological cancer, 5 for lymphatic cancer, 1 for pancreatic cancer, and 1 had been treated for cancer in the neck. Ten participants had received their diagnosis within the last year, 39 participants between 1 and 2 years ago, and 22 participants had been diagnosed with cancer more than 2 years ago. The mean age was 51.8 years (SD=9.86; range: 30–65), 39 of the participants (54.9%) had at least a bachelor degree, 30 participants (42.3%) had full or part-time employment, and 44 (62.0%) had a household income of 30 000 Swedish kronor (SEK) or more. Twenty-three participants (32.4%) used antidepressants. The analysis in this paper used the baseline and six-month follow-up measurements. There were no adverse events or side effects reported.
Change in psychological distress, positive states of mind, and coping self-efficacy
The MANCOVA analysis with baseline and follow-up at 6 months on psychological outcomes: perceived stress, depression, anxiety, post traumatic stress symptoms (IES-intrusion, IES-avoidance, and IES-hyperarousal), positive states of mind (reversely coded), and coping self-efficacy (reversely coded) did not show a significant time × group (intervention vs. control) interaction (F8, 59=1.42, p=0.21, partial η2=0.16), indicating no overall significant differences between the intervention group and the control group. There was no significant main effect of time or group, and none of the potential confounding variables showed significant effects. Results from the univariate tests as well as mean values, change scores, and effect size for the differences in change between intervention and control group on the psychological outcome variables are presented in table 1. Although not significant at alpha level 0.05, there were noteworthy trends of greater reduction in perceived stress (p=0.06) and anxiety (p=0.09) in the intervention group as compared to the control group. The subsequent per-protocol analysis with the 58 participants that filled-out and returned both the baseline and the 6-month follow-up questionnaires, gave similar results and did not show a significant time × group (intervention vs. control) interaction (F8,46=1.79, p=0.10, partial η2=0.24).
Table 1.
Means and standard deviations of psychological outcome variables at baseline and 6-month follow-up for the intervention (n=32) and control group (n=39).
| Mindfulness intervention | Waiting-list control | ||||||
|---|---|---|---|---|---|---|---|
| Baseline | 6-month follow-up |
Baseline | 6-month follow-up |
Intervention effect |
Effect size |
||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | F (1, 66) | P | ddiffa | |
| Perceived stress | 22.56 (6.20) | 17.22 (6.61) | 20.74 (5.45) | 17.85 (6.43) | 3.54 | 0.06 | 0.40 |
| Depression | 6.41 (4.46) | 4.85 (4.20) | 7.18 (3.55) | 6.57 (4.04) | 2.30 | 0.13 | 0.24 |
| Anxiety | 10.53 (4.70) | 8.32 (4.40) | 10.44 (4.59) | 9.54 (5.10) | 2.90 | 0.09 | 0.28 |
| Post-traumatic stress symptoms (Intrusion of Event Scale [IES]): | |||||||
| IES-Intrusion | 13.28 (7.07) | 11.81 (6.36) | 15.05 (6.72) | 13.05 (6.67) | 0.10 | 0.76 | 0.08 |
| IES-Avoidance | 10.55 (6.79) | 7.88 (7.65) | 11.77 (7.51) | 10.54 (7.23) | 2.05 | 0.16 | 0.20 |
| IES-Hyperarousal | 9.50 (5.51) | 7.22 (5.24) | 10.85 (5.52) | 8.90 (5.13) | 0.12 | 0.73 | 0.06 |
| Positive states of mind | 18.97 (3.68) | 21.22 (4.34) | 18.90 (3.70) | 19.94 (4.40) | 2.46 | 0.12 | 0.31 |
| Coping self-efficacy | 139.31 (47.25) | 160.90 (42.33) | 142.97 (31.40) | 149.88 (37.97) | 1.14 | 0.29 | 0.38 |
The effect size was calculated based on the difference between the group means on baseline and 6-month follow-up change scores, and the denominator was based on the pooled SD at baseline and 6-month follow-up adjusted for different sample sizes between groups.
Change in mindfulness
The MANCOVA analysis with baseline and follow-up at 6 months on mindfulness subscales – observing, describing, acting with awareness, non-judging of inner experience, and non-reactivity to inner experience – showed a significant effect for the time × group (intervention vs. control) interaction (F5, 62=3.63, p<0.01, partial η2=0.23), indicating that the intervention group reported a larger increase in mindfulness subscales than the control group. There was no significant main effect of time and none of the potential confounding variables showed significant effects. There was a significant main effect of group (F5, 62=2.70, p<0.05, partial η2=0.18) indicating higher scores in the intervention group. Results from the univariate tests as well as mean values, change scores, and effect size for the differences in change between intervention and control group on the mindfulness subscales are presented in table 2. The univariate tests showed that there were significant group-by-time interactions for four of the five mindfulness subscales: observing (F1, 66=9.26, p<0.01, partial η2=0.12), describing (F1, 66=10.40, p<0.01, partial η2=0.12), acting with awareness (F1, 66=8.71, p<0.01, partial η2=0.12), and non-reactivity to inner experience (F1, 66=7.85, p<0.01, partial η2=0.11). The intervention group experienced a larger increase on these subscales.
Table 2.
Means and standard deviations of the five subscales of mindfulness at baseline and 6-month follow-up for the intervention (n=32) and control group (n=39).
| Mindfulness intervention | Waiting-list control | ||||||
|---|---|---|---|---|---|---|---|
| Baseline | 6-month follow-up |
Baseline | 6-month follow-up |
Intervention effect |
Effect size |
||
| Mindfulness subscales: | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | F (1,66) | p | ddiffa |
| Observing | 28.92 (6.14) | 31.54 (5.14) | 27.23 (5.92) | 26.62 (5.84) | 9.26 | <0.01 | 0.57 |
| Describing | 27.93 (7.44) | 29.91 (6.48) | 28.06 (7.70) | 27.13 (8.64) | 10.40 | <0.01 | 0.39 |
| Acting with awareness | 24.03 (6.44) | 28.69 (6.50) | 20.67 (6.64) | 21.72 (6.04) | 8.71 | <0.01 | 0.58 |
| Non-judging of inner experiences |
24.78 (7.77) | 28.72 (7.04) | 23.97 (7.58) | 26.03 (7.38) | 2.14 | 0.15 | 0.26 |
| Non-reactivity to inner experiences |
17.79 (4.95) | 21.31 (3.86) | 17.72 (4.85) | 19.03 (4.67) | 7.85 | <0.01 | 0.49 |
The effect size was calculated based on the difference between the group means on baseline and 6-month follow-up change scores, and the denominator was based on the pooled SD at baseline and 6-month follow-up adjusted for different sample sizes between groups.
The subsequent per-protocol analysis with the 58 participants that filled-out and returned both baseline and follow-up assessments also showed a significant effect for the time × group (intervention vs. control) interaction (F5, 49=3.86, p<0.01) with a slightly larger effect size (partial η2=0.28). The univariate tests again showed significant group-by-time interactions for observing (F1,66=7.50, p<0.01, partial η2=0.12), describing (F1,66=6.98, p<0.05, partial η2=0.12), acting with awareness (F1,66=10.86, p<0.01, partial η2=0.17), and non-reactivity to inner experience (F1,66=9.64, p<0.01, partial η2=0.15).
Meditation practice post-intervention
According to responses given in the 6-month follow-up questionnaire, 38% of the participants in the intervention group continued to meditate regularly, 14% reported a moderate amount of meditation, and 48% reported infrequent meditation practice. To examine if post-intervention meditation practice influenced psychological outcomes, change scores from baseline to 6-month follow-up were subsequently analyzed for the subset of the intervention group that meditated regularly compared with the control group. Those in the intervention group who continued to meditate regularly after the intervention period had a significant reduction in post-traumatic avoidance symptoms at 6-month follow-up (t=2.50, p<0.05). No other significant intervention effect on psychological outcomes was found among those who continued meditating.
The correlation between frequency of meditation practice and change score in mindfulness and psychological outcome varibles from baseline to 6-month follow-up for the intervention group is presented in Table 3. There was no significant correlation between frequency of meditation practice and change in mindfulness or psychological outcome between baseline and 6-month follow-up.
Table 3.
Bivariate correlation between frequency of meditation practice and change score in mindfulness and psychological outcome variables from baseline to 6-month follow-up for the intervention group.
| Frequency of meditation practice | ||
|---|---|---|
| ρ | Sig. | |
| Mindfulness subscales: | ||
| Observing | 0.04 | P=0.87 |
| Describing | −0.16 | P=0.50 |
| Acting with awareness | −0.07 | P=0.78 |
| Non-judging of inner experiences | 0.18 | P=0.44 |
| Non-reactivity to inner experiences | 0.27 | P=0.24 |
| Perceived stress | 0.22 | P=0.34 |
| Depression | 0.28 | P=0.22 |
| Anxiety | 0.16 | P=0.48 |
| Post-traumatic stress symptoms (Intrusion of Event Scale [IES]): | ||
| IES-Intrusion | 0.07 | P=0.75 |
| IES-Avoidance | −0.30 | P=0.18 |
| IES-Hyperarousal | −0.01 | P=0.98 |
| Positive states of mind | −0.27 | P=0.24 |
| Coping self-efficacy | 0.07 | P=0.78 |
DISCUSSION
Mindfulness-based treatments and stress reduction techniques hold great promise and seem to positively affect stress symptoms and psychological wellbeing. Short-term reduction of psychological distress and stress symptoms as a result of mindfulness interventions for patients treated for cancer have been reported previously in a few randomized studies [10, 11], and some non-randomized studies [5, 6, 9, 27, 28]. But the way in which increased mindfulness leads to positive outcomes is not well understood and the longer-term effect of mindfulness practice is more unclear. Results from this study have been presented in a previous publication reporting on the positive short-term intervention effects at 3-month follow-up [15]. In this study, we report on the longer-term effect of the mindfulness program and found positive longer-term effect of the mindfulness training on mindfulness as measured by the FFMQ, but no significant differences between intervention and control group on psychological outcomes. The previous study showed that increases in mindfulness mediated the effect of the intervention on psychological outcomes at 3-months post-randomization but in these 6 month post randomization data we found an effect on mindfulness only. The differences between intervention and control group on psychological outcomes were diminished and no longer significant. However, there were noteworthy trends of greater reduction in perceived stress and anxiety in the intervention group as compared to the control group.
Although this study showed no clear longer-term effect of the intervention over the control group, there are several possible explanations. A reason why the initial positive effect of the mindfulness intervention was not sustained could be the low rate of post-intervention meditation practice among the participants. Just over a third of the participants continued to meditate regularly. Previous studies have shown that the amount of meditation practice is related to the beneficial effect and future studies should examine the potential of using additional intervention strategies to encourage and facilitate continued practice [25, 29]. It is notable that participants in the intervention group reported continued higher scores on most of the mindfulness subscales. This indicated that being “mindful” might not be enough to reduce stress and increase wellbeing. It might be that regular meditation practice is also required, as suggested by the significant intervention effect on post-traumatic avoidance symptoms among the subgroup of respondents that continued to practice meditation after the end of the program. Another possibility is that the initial benefits of the program may have been the result of group support. The 3-month follow-up assessment was finished shortly after completion of the program and it is possible that the following reduction of effect as measured at 6 months was a result of losing the group support. Finally, the lack of significant effect at 6-month follow-up might be due to the fairly high degree of dropout of the study, and our study may have been underpowered to detect main effects. At 6-month follow-up only 21 of those 32 (66%) initially randomized to the intervention returned the assessment questionnaire.
The findings from this study have some important clinical implications. The lack of clear longer-term effects of the mindfulness training suggests that booster sessions or other tools for increasing post-intervention continuation of training might be considered in future interventions to promote sustained positive results. Modification of the program would also be possible with a larger emphasis on the integration of training into daily life. Some studies of mindfulness training for patients treated for cancer have found preliminary support for longer-term effects [9, 14]. Theoretically, the ability to be more aware in the present moment as a result of the training should work as a buffer against the negative effect of life stress. A study of dispositional mindfulness also showed that increased dispositional level of mindfulness moderated the influence of stress on both depression and perceived health, so that the associations of perceived stress with depression and perceived health were diminished for those with higher levels of mindfulness [26]. However, it is possible that an ability such as being mindful in everyday life needs sustained practice over a longer period of time than eight weeks.
While this study shows very promising results, there are several limitations. First, the fact that we study a specific population limits the possibility to generalize the findings to different illness groups or others experiencing stress. The group recruited is presumably also a highly motivated group of individuals that were self selected to participate in a study that required a great deal of time commitment. The recruitment of a limited sample of participants with experience of varying cancer diagnoses does not enable the examination of differential effect of the intervention on patients treated for specific cancer diagnoses. Information regarding specific treatments and side effects from treatments were not systematically collected, and thus, we could not adjust for these factors in our analysis nor examine the specific effects of these factors. Another potential limitation is the wait-list control design. It is unclear what part of the intervention is actually influencing outcomes and a study design using an active placebo intervention would give stronger support for the specific effects of the mindfulness intervention. A further limitation was that there was no systematic collection of information regarding program fidelity and only limited retrospective self-report assessment of meditation practice among participants. A single item question was used to measure frequency of meditation practice and this strategy may have been too narrow to represent true differences. Measures of both frequency and duration would have been more informative of actual ‘dose’ of meditation and might better have differentiated those that benefitted the most by the intervention. Further, no differentiation was made between formal (taking time to meditate for an extended period of time) and informal (bringing mindfulness to an activity) practices as meditation. Both types of practice are encouraged during the intervention program and systematic measurement of this information would have been of value. Future research should focus on understanding which specific elements of the mindfulness training influence particular psychological outcomes and differentiate the group support and the mindfulness practice components. The short-term positive effect of mindfulness training calls for studies among patients at particular times after diagnosis that might clarify when and for whom mindfulness interventions are the most efficient. Future studies should examine the potential of additional intervention tools to encourage and facilitate prolonged post-intervention meditation practice and the effects of continued practice. Better measurement of daily home practice of both formal and informal mindfulness activities using diaries should be used in future studies to enable a better understanding of the importance of continued meditation and the effect of different amount and type of practice.
ACKNOWLEDGEMENTS
This research was funded by a research grant from the Osher Center for Integrative Medicine at the Karolinska Institute, Sweden. Richard Bränström is funded by research grants from the Swedish Council for Working Life and Social Research (Nr: 2006-1264 and 2006-0069), Center for Health Care Science at the Karolinska Institute, Sweden (Nr: 2008-4737), the Swedish Cancer Society, and Cancer- och Trafikskadades Riksförbund, Sweden.
REFERENCES
- 1.McGregor BA, Antoni MH. Psychological intervention and health outcomes among women treated for breast cancer: a review of stress pathways and biological mediators. Brain Behav Immun. 2009;23(2):159–166. doi: 10.1016/j.bbi.2008.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoffman KE, et al. Psychological distress in long-term survivors of adult-onset cancer: results from a national survey. Arch Intern Med. 2009;169(14):1274–1281. doi: 10.1001/archinternmed.2009.179. [DOI] [PubMed] [Google Scholar]
- 3.Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain and illness. New York: Delacourt; 1990. [Google Scholar]
- 4.Bishop SR. What do we really know about mindfulness-based stress reduction? Psychosom Med. 2002;64(1):71–83. doi: 10.1097/00006842-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Carlson LE, Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med. 2005;12(4):278–285. doi: 10.1207/s15327558ijbm1204_9. [DOI] [PubMed] [Google Scholar]
- 6.Carlson LE, et al. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med. 2003;65(4):571–581. doi: 10.1097/01.psy.0000074003.35911.41. [DOI] [PubMed] [Google Scholar]
- 7.Grossman P, et al. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 8.Smith JE, et al. Mindfulness-Based Stress Reduction as supportive therapy in cancer care: systematic review. J Adv Nurs. 2005;52(3):315–327. doi: 10.1111/j.1365-2648.2005.03592.x. [DOI] [PubMed] [Google Scholar]
- 9.Carlson LE, et al. The effects of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients-6-month follow-up. Support Care Cancer. 2001;9(2):112–123. doi: 10.1007/s005200000206. [DOI] [PubMed] [Google Scholar]
- 10.Speca M, et al. A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med. 2000;62(5):613–622. doi: 10.1097/00006842-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Lengacher CA, et al. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psychooncology. 2009 doi: 10.1002/pon.1529. [DOI] [PubMed] [Google Scholar]
- 12.Shapiro SL, et al. The efficacy of mindfulness-based stress reduction in the treatment of sleep disturbance in women with breast cancer: an exploratory study. J Psychosom Res. 2003;54(1):85–91. doi: 10.1016/s0022-3999(02)00546-9. [DOI] [PubMed] [Google Scholar]
- 13.Ledesma D, Kumano H. Mindfulness-based stress reduction and cancer: a meta-analysis. Psychooncology. 2009;18(6):571–579. doi: 10.1002/pon.1400. [DOI] [PubMed] [Google Scholar]
- 14.Carlson LE, et al. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. 2007;21(8):1038–1049. doi: 10.1016/j.bbi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 15.Bränström R, et al. Self-report Mindfulness as a Mediator of Psychological Wellbeing in a Stress Reduction Intervention for Cancer Patients - a randomized study. Annals Behavioral Medicine. 2010;39(2):151–161. doi: 10.1007/s12160-010-9168-6. [DOI] [PubMed] [Google Scholar]
- 16.SPSS Inc. SPSS 15.0 for Windows. Chicago: SPSS Inc.; 1999. [Google Scholar]
- 17.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 18.Bjelland I, et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 19.Weiss D, Marmar C. The Impact of Event Scale - Revised. In: Wilson J, Keane T, editors. Assessing psychological trauma and PTSD. Guilford: New York; 1996. pp. 399–411. [Google Scholar]
- 20.Horowitz M, Wilner N, Alvarex W. Impact of Event Scale: A Measure of Subjective Stress. Psychosomatic Medicine. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Adler NE, et al. Additional validation of a scale to assess positive states of mind. Psychosom Med. 1998;60(1):26–32. doi: 10.1097/00006842-199801000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Horowitz M, Adler N, Kegeles S. A scale for measuring the occurrence of positive states of mind: a preliminary report. Psychosom Med. 1988;50(5):477–483. doi: 10.1097/00006842-198809000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Chesney MA, et al. A validity and reliability study of the coping self-efficacy scale. Br J Health Psychol. 2006;11(3):421–437. doi: 10.1348/135910705X53155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baer RA, et al. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- 25.Baer RA, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- 26.Bränström R, Duncan L, Moskowitz JT. The association between dispositional mindfulness, psychological well-being and perceived health in a Swedish population-based sample. British Journal of Health Psychology. 2010;(16):300–316. doi: 10.1348/135910710X501683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carlson LE, et al. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29(4):448–474. doi: 10.1016/s0306-4530(03)00054-4. [DOI] [PubMed] [Google Scholar]
- 28.Witek-Janusek L, et al. Effect of mindfulness based stress reduction on immune function, quality of life and coping in women newly diagnosed with early stage breast cancer. Brain Behav Immun. 2008;22(6):969–981. doi: 10.1016/j.bbi.2008.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. 2008;31(1):23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]