Abstract
Cyclooxygenase (COX) inhibitors reduce colorectal adenoma recurrence by up to 45% and selenium supplementation may prevent colorectal cancer. Following colonoscopic adenoma resection, 1,600 men and women aged 40-80 years were randomized to celecoxib (400 mg daily), a selective COX-2 inhibitor, and/or selenium (200 μg daily as selenized yeast), or double placebo. The trial was initiated in November, 2001. The primary trial endpoint is adenoma recurrence in each intervention group compared to placebo, as determined by surveillance colonoscopy performed 3-5 years after baseline. Randomization was stratified by use of low-dose aspirin (81 mg) and clinic site. Following reports of cardiovascular toxicity associated with COX-2 inhibitors, the celecoxib arm was discontinued in December, 2004 when 824 participants had been randomized. Accrual continued with randomization to selenium alone or placebo. Randomization of the originally planned cohort (n=1,621) was completed in November, 2008. A further 200 patients with 1+ advanced adenomas (denoting increased risk for colorectal cancer) were accrued to enhance statistical power for determining intervention efficacy in this higher-risk subgroup. Accrual of the total cohort (n=1,824) was completed in January, 2011. Baseline cohort characteristics include: mean age 62.9 years; 65% male; BMI 29.1 ±5.1; 47% taking low-dose aspirin while on trial; 20% with 3+ adenomas; and 38% with advanced adenomas. Intervention effects on adenoma recurrence will be determined, and their modification by genetic background and baseline selenium level. The effect of selenium supplementation on risk for type 2 diabetes will also be reported (Funded by the National Cancer Institute; ClinicalTrials.gov number, NCT00078897.)
Keywords: colorectal adenoma, celecoxib, selenium, randomized trial
Introduction
Approximately 143,000 new cases and 52,000 deaths from colorectal cancer are expected in 2012 in the United States, a cancer morbidity and mortality that is second only to that of lung cancer (1). Implementation of screening is considered an important factor in the decline of incidence and mortality from colorectal cancer over recent decades. However, the proportion of colorectal cancer deaths that can be prevented by screening is unclear with estimated mortality reductions ranging from approximately 20% to more than 50% (2-5). Among screening modalities, colonoscopy has yielded the largest mortality reductions. However, a limitation of colonoscopic screening is that it may be less effective for reducing risk (6) and mortality (7, 8) of right-sided than left-sided colorectal cancers. Incomplete compliance with guidelines, regardless of the modality, may also limit what can be achieved by screening alone; prevalence of colorectal cancer screening in U.S. adults combined, African Americans, Hispanics and uninsured individuals, respectively, was reported recently as 53.2%, 48.9%, 37.2% and 19.5% (9). Thus, to optimize reductions in colorectal cancer incidence and mortality, additional effective interventions that are safe, easy to use and inexpensive are needed to complement screening.
Chemoprevention has been advocated as a potential adjunct to screening for reducing colorectal cancer morbidity and mortality (10). In randomized chemoprevention trials, calcium supplementation (11) and the non-steroidal anti-inflammatory drug (NSAID) aspirin (12, 13) were shown to reduce colorectal adenoma risk by 15-35%; aspirin yielded a greater 41% reduction in risk (12) for adenomas with advanced pathology, which are associated with a high risk of subsequent neoplasia (14-16). Recently, in a meta-analysis of cardiovascular prevention trials, aspirin reduced colon cancer risk and mortality, respectively, by 24% and 35% (17) and colorectal cancer risk was reduced by 44% in Lynch syndrome patients receiving aspirin for a mean of 56 months (18).
The anti-neoplastic actions of aspirin are attributed at least in part to inhibition of cyclooxygenase (COX) (19) but the level of gastrointestinal toxicity caused by aspirin and other NSAIDS (20) has restrained enthusiasm for their use as cancer preventive agents. Because inhibition of the COX-1 isoform is thought to be responsible for NSAID-related gastrointestinal toxicity, immense effort was directed to the development of selective COX-2 inhibitors (coxibs), such as celecoxib and rofecoxib, that would, hypothetically, conserve the beneficial effects of NSAIDs and minimize their toxicity. Although in randomized trials celecoxib and rofecoxib reduced colorectal adenoma risk by 24 – 45% (14, 16, 21), an associated increased risk of serious cardiovascular events with both agents prohibited the subsequent clinical use of coxibs for chemoprevention.
Selenium is an essential micronutrient with antioxidant activity and chemopreventive potential (22-24). It is incorporated into specialized selenocysteine-containing selenoproteins (25) that mediate redox-dependent and other cellular functions (24, 26, 27). Evidence that selenium might help to prevent colorectal cancer came from the Nutritional Prevention of Cancer (NPC) Trial, a randomized controlled trial of selenium 200 μg daily as selenized yeast for the prevention of skin cancer (28). Although the intervention had no effect on the incidence of basal or squamous cell cancers, in planned secondary analyses there was a significant reduction of colorectal cancer incidence, which attenuated over time (29). In a subsequent pooled analysis of data from three colorectal adenoma recurrence trials, participants’ baseline blood selenium levels were inversely related to risk for developing metachronous (recurrent) colorectal adenomas (30). Selenium interventions were of significant benefit in four trials included in a Cochrane review of randomized controlled trials of antioxidant supplements administered for colorectal cancer prevention (31); there was some evidence that benefits of selenium were sustained in a later follow-up report (32). While finding the methodologies of these four trials suboptimal, the Cochrane review authors considered the evidence for a potential effect of selenium in preventing colorectal cancer sufficient to warrant randomized trials of this agent.
At the time the current study was designed, the majority of randomized trials for the chemoprevention of colorectal adenomas compared a single intervention to placebo. We hypothesized that combining relatively modest doses of two agents, each targeting a separate carcinogenesis pathway, would optimize efficacy while minimizing toxicity. The interventions we selected were celecoxib in a single daily dose of 400 mg and selenium as selenized yeast in a single daily dose of 200 μg. The 2×2 factorial design included each intervention alone, the combined interventions, and placebo. We report here the study design and baseline data of the complete trial cohort and an unavoidable modification to the study design—withdrawal of the celecoxib intervention—when the Federal Drug Administration terminated all coxib colorectal adenoma prevention trials because of unanticipated cardiotoxicity (33, 34). After the withdrawal of celecoxib, accrual to the trial was completed with randomization to selenium or placebo only. In this report we focus on methodological adjustments that enabled us to complete trial accrual. We believe that this experience may be helpful for the design of future cancer prevention trials and that dissemination of this experience need not be delayed until the trial results are reported after unblinding in late 2013.
Materials and Methods
Trial design
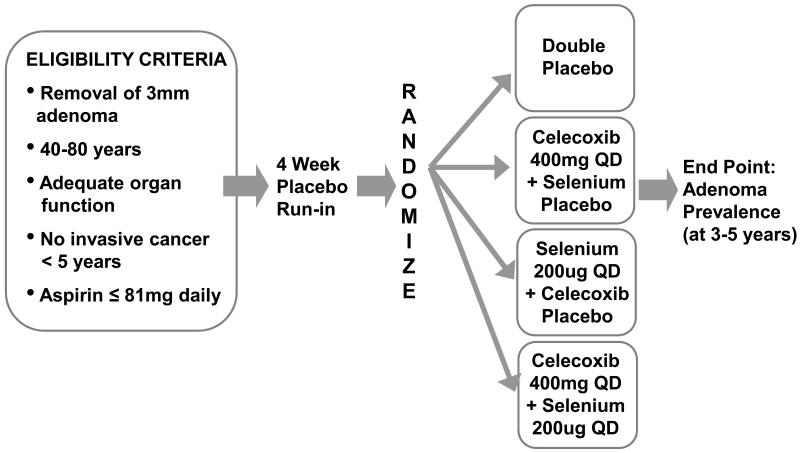
Originally, this was a phase III randomized, parallel, 2×2 factorial design trial of celecoxib (active versus placebo) crossed with a selenium supplement (active versus placebo) for prevention of metachronous (recurrent) colorectal adenomas (Figure 1). The CONSORT 2010 guidelines for reporting randomized controlled trials (35) have been followed in the following description of completed accrual of the trial cohort.
Figure 1. Original study schema—Celecoxib/Selenium Trial.
Eligibility
Healthy male and female patients between the ages of 40 and 80 years who had undergone total colonoscopy and complete removal of one or more colorectal adenomas with a diameter of 3 mm or more within the six months prior to registration were eligible. Adenomas were categorized as non-advanced or advanced; the latter defined as adenomas with a diameter of 1+ cm, or any adenoma with villous features or high-grade dysplasia. Patients with 1 or more advanced adenomas or ≥3 non-advanced adenomas were classified in a “high-risk adenoma” category. Patients with a family history of familial adenomatous polyposis or Lynch syndrome and those diagnosed with invasive cancer within the previous five years were among those excluded. Patients taking low-dose aspirin, defined as a maximum dose of 81 mg daily, were eligible.
Study sites
Participants were recruited through clinical centers in Arizona, Colorado, Texas and New York (Table 1) following ambulatory colonoscopies performed at local high-volume endoscopy facilities. All study data and biospecimens are collected, managed and archived at the University of Arizona Cancer Center (Tucson, AZ). The University of Arizona Institutional Review Board (IRB) approved and oversaw the study protocol and conduct of the trial was in accordance with requirements of the local IRB at each study site.
Table 1. Baseline Participant Characteristics.
| Full Factorial Cohort1 (n=824) |
Selenium Cohort2 (n=797) |
Advanced Adenoma Cohort3 (n=203) |
Total (n=1824) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Clinic | |||||||||
| Baylor | 2 | (0.2) | 100 | (12.5) | 21 | (10.3) | 123 | (6.7) | |
| Colorado | 183 | (22.2) | 100 | (12.5) | 40 | (19.7) | 323 | (17.7) | |
| Mayo | 6 | (0.7) | 49 | (6.1) | 9 | (4.4) | 64 | (3.5) | |
| Phoenix | 461 | (55.9) | 457 | (57.3) | 86 | (42.4) | 1004 | (55.0) | |
| Tucson | 172 | (20.9) | 91 | (11.4) | 16 | (7.9) | 279 | (15.3) | |
| Western New York | 0 | (0.0) | 0 | (0.0) | 31 | (15.3) | 31 | (1.7) | |
| Mean age ± SD | 62.9 | ± 9.3 | 63.5 | ± 8.6 | 60.5 | ± 8.7 | 62.9 | ± 9.0 | |
| Age Group | |||||||||
| <50 y | 55 | (6.7) | 28 | (3.5) | 16 | (7.9) | 99 | (5.4) | |
| 50-59 y | 234 | (28.4) | 249 | (31.2) | 77 | (37.9) | 560 | (30.7) | |
| 60-69 y | 323 | (39.2) | 298 | (37.4) | 71 | (35.0) | 692 | (37.9) | |
| ≥ 70 y | 212 | (25.7) | 222 | (27.9) | 39 | (19.2) | 473 | (25.9) | |
| Sex | |||||||||
| Male | 559 | (67.8) | 497 | (62.4) | 123 | (60.6) | 1179 | (64.6) | |
| Female | 265 | (32.2) | 300 | (37.6) | 80 | (39.4) | 645 | (35.4) | |
| Race4 | |||||||||
| White | 778 | (94.6) | 742 | (93.2) | 188 | (93.1) | 1708 | (93.8) | |
| Black/African | 16 | (1.9) | 32 | (4.0) | 7 | (3.5) | 55 | (3.0) | |
| Asian | 12 | (1.5) | 4 | (0.5) | 3 | (1.5) | 19 | (1.0) | |
| American Indian/Alaskan | 4 | (0.5) | 4 | (0.5) | 1 | (0.5) | 9 | (0.5) | |
| Other/Mixed | 12 | (1.5) | 14 | (1.8) | 3 | (1.5) | 29 | (1.6) | |
| Unknown | 2 | 1 | 1 | 4 | |||||
| Hispanic/Latino | |||||||||
| Yes | 42 | (5.1) | 41 | (5.2) | 7 | (3.5) | 90 | (4.9) | |
| No | 782 | (94.9) | 754 | (94.8) | 195 | (96.5) | 1731 | (95.1) | |
| Unknown | 0 | 2 | 1 | 3 | |||||
| Education | |||||||||
| < High School | 18 | (2.2) | 14 | (1.8) | 3 | (1.5) | 35 | (1.9) | |
| High School or GED | 156 | (18.9) | 154 | (19.4) | 43 | (21.2) | 353 | (19.4) | |
| Some college | 253 | (30.7) | 242 | (30.4) | 46 | (22.7) | 541 | (29.7) | |
| Bachelor's Degree | 168 | (20.4) | 158 | (19.9) | 55 | (27.1) | 381 | (20.9) | |
| Graduate/Professional | 229 | (27.8) | 227 | (28.6) | 56 | (27.6) | 512 | (28.1) | |
| Unknown | 0 | 2 | 0 | 2 | |||||
| Mean BMI5 ± SD | 29.1 | ± 4.9 | 29.0 | ± 5.3 | 29.2 | ± 5.2 | 29.1 | ± 5.1 | |
| BMI unknown | 0 | 2 | 0 | 2 | |||||
| Cigarette smoking status | |||||||||
| Ever6 | 484 | (60.1) | 440 | (57.1) | 108 | (57.1) | 1032 | (58.5) | |
| Current | 79 | (9.8) | 66 | (8.6) | 26 | (13.8) | 171 | (9.7) | |
| Previous | 405 | (50.3) | 374 | (48.6) | 82 | (43.4) | 861 | (48.8) | |
| Never | 321 | (39.9) | 330 | (42.9) | 81 | (42.9) | 732 | (41.5) | |
| Unknown | 19 | 27 | 14 | 60 | |||||
| History of colorectal polyps7 | |||||||||
| Yes | 233 | (28.8) | 271 | (34.5) | 78 | (39.6) | 582 | (32.5) | |
| No | 575 | (71.2) | 514 | (65.5) | 119 | (60.4) | 1208 | (67.5) | |
| Unknown | 16 | 12 | 6 | 34 | |||||
| Family History of CRC8 | |||||||||
| Yes | 160 | (20.6) | 140 | (18.3) | 37 | (19.1) | 337 | (19.4) | |
| No | 617 | (79.4) | 623 | (81.7) | 157 | (80.9) | 1397 | (80.6) | |
| Unknown | 47 | 34 | 9 | 90 | |||||
| Diabetes | |||||||||
| Yes | 61 | (7.4) | 88 | (11.1) | 23 | (11.3) | 172 | (9.4) | |
| No | 763 | (92.6) | 708 | (88.9) | 180 | (88.7) | 1651 | (90.6) | |
| Unknown | 0 | 1 | 0 | 1 | |||||
| Personal history of cancer9 | |||||||||
| Yes | 49 | (5.9) | 47 | (5.9) | 9 | (4.4) | 105 | (5.8) | |
| No | 775 | (94.1) | 749 | (94.1) | 194 | (95.6) | 1718 | (94.2) | |
| Unknown | 0 | 1 | 0 | 1 | |||||
| Personal history of skin cancer10 | |||||||||
| Yes | 117 | (14.2) | 141 | (17.7) | 28 | (13.8) | 286 | (15.7) | |
| No | 707 | (85.8) | 655 | (82.3) | 175 | (86.2) | 1537 | (84.3) | |
| Unknown | 0 | 1 | 0 | 1 | |||||
| Aspirin use in the past 20 years11 | |||||||||
| < 1 year | 481 | (58.4) | 411 | (51.8) | 122 | (60.1) | 1014 | (55.7) | |
| 1 to <5 years | 174 | (21.1) | 170 | (21.4) | 36 | (17.7) | 380 | (20.9) | |
| 5 to <10 years | 73 | (8.9) | 90 | (11.3) | 14 | (6.9) | 177 | (9.7) | |
| ≥ 10 years | 96 | (11.7) | 123 | (15.5) | 31 | (15.3) | 250 | (13.7) | |
| Unknown | 0 | 3 | 0 | 3 | |||||
| Aspirin use at randomization | |||||||||
| 0 mg/d | 423 | (51.3) | 426 | (53.5) | 126 | (62.1) | 975 | (53.5) | |
| 1-81 mg/d | 401 | (48.7) | 371 | (46.5) | 77 | (37.9) | 849 | (46.5) | |
| NSAID use in the past 20 years12 | |||||||||
| < 1 year | 739 | (89.7) | 699 | (88.0) | 180 | (88.7) | 1618 | (88.9) | |
| 1 to <5 years | 53 | (6.4) | 58 | (7.3) | 13 | (6.4) | 124 | (6.8) | |
| 5 to <10 years | 16 | (1.9) | 17 | (2.1) | 3 | (1.5) | 36 | (2.0) | |
| ≥ 10 years | 16 | (1.9) | 20 | (2.5) | 7 | (3.4) | 43 | (2.4) | |
| Unknown | 0 | 3 | 0 | 3 | |||||
| Supplement User | |||||||||
| Yes | 537 | (68.4) | 521 | (69.7) | 123 | (63.7) | 1181 | (68.4) | |
| No | 248 | (31.6) | 227 | (30.3) | 70 | (36.3) | 545 | (31.6) | |
| Unknown | 39 | 49 | 10 | 98 | |||||
Note: Counts and percentages for categorical variables; mean ± standard deviation for continuous variables. Percentages are calculated from non-missing data.
Full Factorial Cohort: Celecoxib vs Selenium vs Combination vs Placebo, 11/27/2001-12/16/2004
Selenium Cohort: Selenium vs Placebo, 02/02/2005-11/26/2008
Advanced Adenoma Cohort: Selenium vs Placebo among participants selected for advanced adenoma at qualification, 07/30/2008-01/19/2011
25 participants marked more than one race, including 22 who selected a race they identified with primarily (and classified accordingly), and 3 who were unable to identify with one group (classified as Mixed).
Body Mass Index, calculated as 703*(weight in pounds)/(height in inches)2.
Ever smoker defined as 100 or more cigarettes.
History of colorectal polyp(s) on prior occasion to baseline colonoscopy with polypectomy that determined study eligibility
Family history of colorectal cancer in a first degree relative
Excluding non-melanoma skin cancer
Including basal cell, squamous cell, and skin cancer of unknown type
Number of years in total within the past twenty years taking aspirin or aspirin containing products at least twice a week for at least six consecutive months.
Number of years in total within the past twenty years taking a non-steroidal anti-inflammatory drug (NSAID), excluding aspirin, either over-the-counter or prescription at least twice a week for at least six consecutive months.
Interventions
Celecoxib (Celebrex®) 200 mg capsules and matching placebo were provided by Pfizer (New York, NY). The active intervention was celecoxib 400 mg taken as a single daily dose of two 200 mg capsules. The drug was stored at room temperature in a locked storage facility. Celecoxib content of the stored drug was assayed annually by high performance liquid chromatography in the University of Arizona Cancer Center Analytical Core Laboratory (36). The range of celecoxib content in these assays was 189 – 204 mg per capsule. Selenium as SelenoExcell High Selenium Yeast capsules (selenium 200 μg/capsule) and matching placebo are provided by Cypress Systems (Fresno, CA). The active intervention is selenium 200 μg as a single daily dose. The selenium content of stored intervention tablets as measured semi-annually by atomic absorption spectrophotometry in the University of Arizona Cancer Center Analytical Core Laboratory is within the range of 196 – 201 μg. Selenium plasma levels are measured at baseline and annually by atomic absorption spectrophotometry in all participants while on study.
Outcomes
The primary study outcome is colorectal adenoma recurrence. Recurrence rates are determined as the percentage of participants with metachronous adenomas diagnosed in each randomization group at surveillance colonoscopies, which are timed according to usual practice guidelines (37). The pre-specified primary outcome measures are recurrence rates with any (non-advanced or advanced) adenoma in participants taking celecoxib alone, selenium alone, celecoxib + selenium, or placebo. Additional planned analyses include the number, location and non-advanced/advanced/high-risk status of metachronous adenomas. A further pre-specified primary aim is to measure the type and incidence of adverse events occurring during prolonged treatment with celecoxib and selenium, given alone or in combination, with or without concomitant low-dose aspirin therapy in patients with colorectal adenomas.
Secondary outcome measures include: modification of the effects of the celecoxib or selenium interventions on colorectal adenoma risk by concomitant low-dose aspirin; modification of the effects of the selenium intervention by baseline blood selenium level; and modification of the effects of the selenium intervention by sequence variations of candidate selenoprotein genes.
Participant safety and outcomes are monitored by an External Data and Safety Monitoring Committee (EDSMC), which convenes semi-annually or more frequently if necessary. At each meeting, the EDSMC reviews unblinded safety and efficacy data in the context of newly reported information from other trials and studies as the basis for a recommendation on whether or not the trial should be continued, with or without modification.
Randomization
Potentially eligible patients were identified through screening of colonoscopy and pathology reports by study coordinators from the respective clinical sites. After implementation of the Health Insurance Portability and Accountability Act (HIPAA) in 2003, those patients who were screened for possible eligibility gave written permission (“caregivers’ consent”) before their colonoscopy for: their records to be reviewed for this purpose by research staff after the procedure; and, if potentially eligible, for study staff then to contact them concerning possible participation in the study.
Patients who fulfilled all trial eligibility criteria were asked to provide written informed consent for participation, which included consent for isolation of their DNA to be used for analyses of sequence variations in selenoprotein genes. Those who consented to participate began a 4-week run-in assessment period of taking placebo medication for assessment of future compliance with taking study medication; they were blinded to the placebo nature of the run-in medication. The study intervention manager was notified of potential participants at the time a patient started run-in medication. Those who returned for clinic visits as scheduled and had taken at least 75% of the placebo medication doses were randomized into one of four groups, i.e. celecoxib + placebo, selenium + placebo, celecoxib + selenium, or double placebo (Figure 1).
Randomization was performed using a Structured Query Language function that first checked for previous randomization and a valid clinic identification number. Randomization was stratified by clinical center and for use of low-dose aspirin (≤81 mg/day). A block size of 4 was used for the factorial design.
After the randomization group was assigned, the information was sent to the Intervention Manager at the central study pharmacy, which dispatches study medication for all participants to their respective clinical centers. Only the intervention manager and designated backup and statistical center personnel responsible for randomization and preparation of unblinded reports for the EDSMC have access to the unblinded list of participant study identification numbers, treatment codes, and intervention identity.
Design changes after commencement
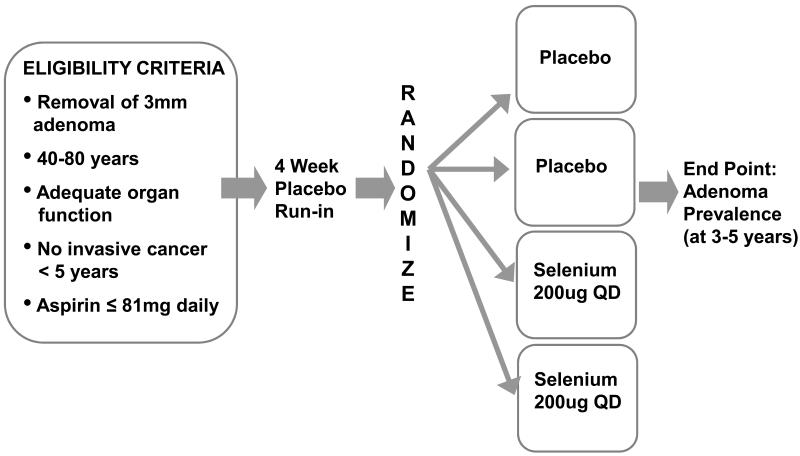
On September 30, 2004, Merck (Whitehouse Station, NJ) announced the world-wide withdrawal of rofecoxib (VIOXX®), like celecoxib a coxib-class selective COX-2 inhibitor, because of an increased relative risk of adverse cardiovascular events in patients taking rofecoxib compared to placebo in a colorectal adenoma prevention trial. On December 17, 2004, the National Institutes of Health announced that it had suspended a second selective COX-2 inhibitor colorectal adenoma prevention trial because of an increased risk of cardiotoxicity associated with the drug: celecoxib was the agent in this trial. The EDSMC recommended permanent suspension of the celecoxib arm of our trial on December 20, 2004. On December 23, 2004, the Food and Drug Administration (FDA) placed the trial on clinical hold. However, when informed that the celecoxib arm of the trial had already been permanently suspended by the EDSMC, the same day the FDA authorized uninterrupted continuation of the selenium arm of the trial. With the withdrawal of celecoxib, the study was modified to a randomized parallel two-group design, comparing selenium to placebo. Participants previously randomized to celecoxib with or without placebo were retained in the appropriate selenium or placebo arm (Figure 2).
Figure 2. Revised study schema—Selenium Trial.
As noted, adenomas with advanced pathology are those at greatest risk for progression to colorectal cancer (38). It was apparent as accrual of the originally planned cohort of 1,600 individuals approached completion that 25-30% of randomized participants had one or more advanced adenomas at baseline. To enhance study power for demonstrating intervention effects in this higher risk subpopulation, recruitment of an additional 200 participants with one or more advanced adenomas was undertaken after recruitment of the original 1,600 participant cohort was completed. Because surveillance colonoscopy is indicated after three years in patients with an advanced adenoma rather than the five year interval for patients with non-advanced adenomas, this modification did not lengthen the total duration of the trial. EDSMC and National Cancer Institute approval was obtained for the change in design, which was implemented without any modification to the trial’s original primary aims.
Sample size
The sample size selected for the factorial design was 400 participants per cell, thus requiring randomization of a total of 1,600 participants. The sample size justification assumed a separate test of each intervention (celecoxib or selenium) without adjustment for multiple comparisons. The power calculations were based on a Poisson regression analysis, with an estimated adenoma recurrence rate of 0.25 polyps per year. This estimate was originally based on results from the National Polyp Study (39) and our own Wheat Bran Fiber (WBF) Study (40). Based on the level of compliance in the WBF study, we assumed at least 90% compliance with obtaining the endpoint colonoscopy, resulting in a sample size of 360 per group. Our statistical power was 99% to detect a 25% reduction in the recurrence rate due to celecoxib and 95% to detect a 20% reduction in the recurrence rate due to selenium, assuming no negative interaction between celecoxib and selenium (two-sided 0.05 level of significance). Even with a negative interaction of up to 20%, estimated power for detecting effects of celecoxib and selenium, respectively, was 96% and 78%.
Withdrawal of the celecoxib intervention did not alter the total sample size required. The statistical power was reassessed in light of data from our Ursodeoxycholic Acid (UDCA) colorectal adenoma prevention trial (41). Forty two percent of participants had a recurrent adenoma during the three-year follow-up period of the UDCA trial; this implied an annual hazard of recurrence of 0.182. Based on results of other studies, we were interested in the power to detect a 25% reduction in adenoma recurrence rate due to selenium. Given new guidelines that patients with non-advanced adenomas should undergo colonoscopic surveillance after 5 rather than 3 years (37), we assumed an average follow-up of 4 years. This resulted in 94% statistical power to detect a 25% reduction due to selenium, based on a two-group test of proportions at a 2-sided 0.05 level of significance.
Results from the UDCA trial (41) showed a 49% recurrence of non-advanced or advanced adenomas for those who had an advanced adenoma at baseline. The statistical power would have been 73% to detect a 33% reduction in the recurrence rate in those with advanced adenomas at baseline with the originally planned sample size. One hundred additional participants per group with one or more advanced adenomas were therefore added so that the statistical power increased to approximately 87%. This subset analysis was planned without regard to outcome data in the original 1,600 participants and so is not subject to the limitations of a data derived subset analysis.
Results and Discussion
Screening for eligibility and recruitment processes
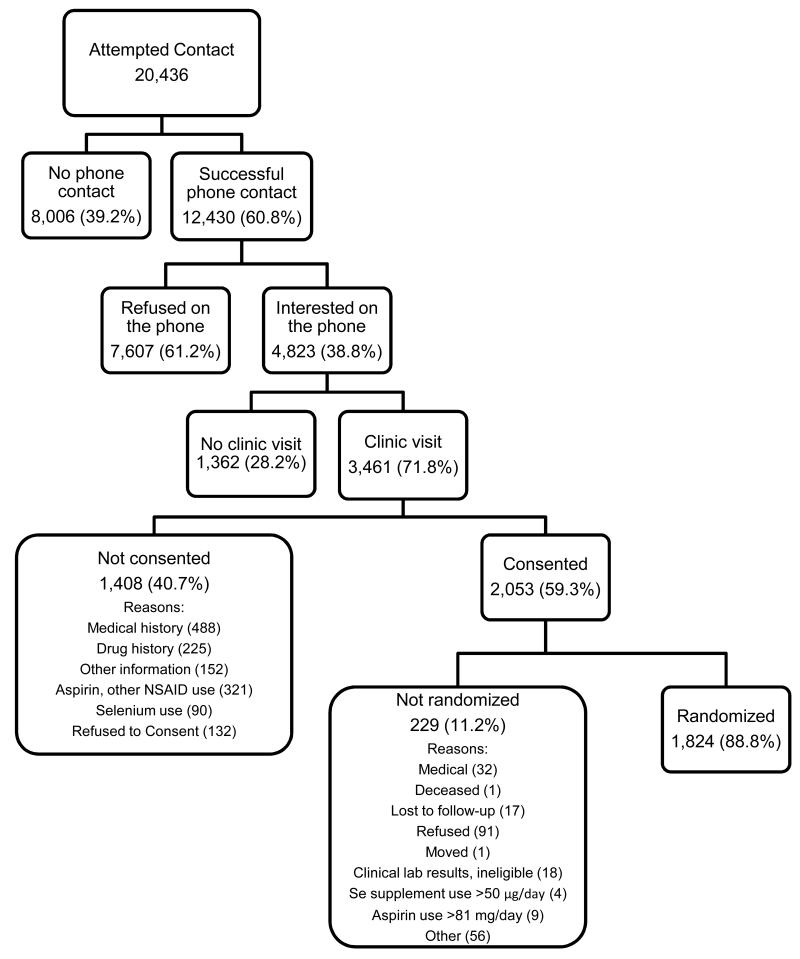
Study coordinators attempted to contact a total of 20,436 patients who had recently undergone colonoscopic polypectomy for a preliminary assessment of potential study eligibility (Figure 3). Successful phone contact was made with 12,430 patients, of whom 3,461 came for a clinic visit and 1,824 were randomized.
Figure 3. Flow diagram of patient enrollment, consenting and randomization.
Accrual phases
The first participant to the “Full Factorial Cohort” (Table 1; celecoxib vs. selenium vs. celecoxib + selenium vs. placebo) was randomized on November 27, 2001. A total of 824 participants were randomized to the Full Factorial Cohort, including 414 to celecoxib, before the EDSMC recommended termination of the celecoxib intervention on December 20, 2004; the last participant in the Full Factorial Cohort was randomized on December 16, 2004. The 414 participants receiving celecoxib took the agent for a median of 14.0 (25th percentile, 4.9; 75th percentile, 22.8) months.
Adverse event data from the 824 participants randomized to either celecoxib or placebo were contributed to a pooled analysis of adjudicated data for cardiovascular risk (the combination of cardiovascular death, myocardial infarction, stroke, heart failure, or thromboembolic event) in 7,950 participants from six placebo-controlled trials comparing celecoxib with placebo for conditions other than arthritis (42). Of note, the risk was lowest (hazard ratio, 1.1; 95% CI, 0.6 to 2.0) for the 400-mg-daily dose of celecoxib, which was the dose used in our trial.
Participants in the Full Factorial Cohort continued active participation after the withdrawal of celecoxib, taking selenium or placebo, until their endpoint colonoscopy. Timing of the latter was not altered by termination of the trial’s celecoxib arm. The effect of celecoxib on adenoma recurrence will be analyzed as originally planned, albeit with less statistical power than originally estimated. In secondary analyses, the length of time for which celecoxib was taken, the duration of any celecoxib effect after the intervention’s termination, and modification of any selenium effects by celecoxib will be considered.
After withdrawal of celecoxib, a further 797 participants with non-advanced or advanced adenomas were randomized to selenium or placebo (Table 1, “Selenium Cohort”) for a total of 1,621 participants in the originally planned cohort. The last of these 1,621 participants was randomized on November 26, 2008. Following completion of the original 1,621-participant cohort, an additional 203 participants with one or more advanced adenomas (Table 1, “Advanced Adenoma Cohort”) were randomized to selenium or placebo, the last of them on January 19, 2011.
Participant characteristics at baseline
Baseline characteristics of the participants in the respective cohorts differed in some respects (Table 1). Mean age of the Full Factorial Cohort (62.9 years) was older than the Advanced Adenoma Cohort (60.5 years). The percentage of female participants increased from 32.2 in the Full Factorial Cohort to 37.6 and 39.4, respectively, in the Selenium and Advanced Adenoma Cohorts. The percentages of participants on regular low-dose aspirin (≤81 mg daily) in the Full Factorial, Selenium and Advanced Adenoma Cohorts, respectively, were 48.7, 46.5 and 37.9. The percentages of participants with a prior history of colorectal polyps in the Full Factorial, Selenium and Advanced Adenoma Cohorts, respectively, were 28.8, 34.5 and 39.6. Overall, an almost 60% majority of participants reported having ever smoked cigarettes.
Adenoma characteristics
Characteristics of participants’ colorectal adenomas at baseline, including anatomic location, size and histological category, are shown in Table 2. Overall, 675 participants (37.9%) had one or more advanced adenomas and 366 (20.1%) had more than two adenomas. Adenomas from 202 of 203 participants in the Advanced Adenoma Cohort were ≥1 cm in size; the remaining participant qualified for the Advanced Adenoma Cohort by having an adenoma with villous histology. Of the 366 participants with more than two adenomas, 199 had at least one advanced adenoma and 164 did not. Thus, a total of 842 participants (47.2%) were in a high risk category by virtue of having one or two advanced adenomas (n=476) (37), or three or more non-advanced adenomas (n=167) (43), or three or more adenomas of which at least one was an advanced adenoma (n=199); the 167 participants with three or more non-advanced adenomas includes three in whom it is unknown whether the adenomas were advanced or non-advanced.
Table 2. Baseline Adenoma Characteristics.
| Full Factorial Cohort1 (n=824) |
Selenium Cohort2 (n=797) |
Advanced Adenoma Cohort3 (n=203) |
Total (n=1824) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Number of adenomas | |||||||||
| 1 | 499 | (60.6) | 471 | (59.1) | 83 | (40.9) | 1053 | (57.7) | |
| 2 | 182 | (22.1) | 170 | (21.3) | 53 | (26.1) | 405 | (22.2) | |
| 3+ | 143 | (17.4) | 156 | (19.6) | 67 | (33.0) | 366 | (20.1) | |
| Proximal adenoma | |||||||||
| No | 294 | (38.5) | 250 | (32.1) | 61 | (30.5) | 605 | (34.7) | |
| Yes | 470 | (61.5) | 528 | (67.9) | 139 | (69.5) | 1137 | (65.3) | |
| Unknown | 60 | 19 | 3 | 82 | |||||
| Distal/Rectal adenoma | |||||||||
| No | 323 | (42.3) | 360 | (46.3) | 80 | (40.0) | 763 | (43.8) | |
| Yes | 441 | (57.7) | 418 | (53.7) | 120 | (60.0) | 979 | (56.2) | |
| Unknown | 60 | 19 | 3 | 82 | |||||
| Largest adenoma | |||||||||
| <1cm | 569 | (71.8) | 590 | (75.7) | 1 | (0.5) | 1160 | (65.4) | |
| ≥1cm | 224 | (28.3) | 189 | (24.3) | 202 | (99.5) | 615 | (34.6) | |
| Unknown | 31 | 18 | 0 | 49 | |||||
| Histology (most severe) | |||||||||
| Tubular, or Adenoma, NOS | 717 | (87.0) | 709 | (89.0) | 156 | (76.8) | 1582 | (86.7) | |
| Tubulovillous or Villous | 107 | (13.0) | 87 | (10.9) | 47 | (23.2) | 241 | (13.2) | |
| Invasive Cancer4 | 0 | (0.0) | 1 | (0.1) | 0 | (0.0) | 1 | (0.1) | |
| High Grade Dysplasia | |||||||||
| No | 808 | (98.1) | 785 | (98.5) | 196 | (96.6) | 1789 | (98.1) | |
| Yes | 16 | (1.9) | 12 | (1.5) | 7 | (3.4) | 35 | (1.9) | |
| Advanced Adenoma5 | |||||||||
| No | 540 | (67.7) | 567 | (72.6) | 0 | (0.0) | 1107 | (62.1) | |
| Yes | 258 | (32.3) | 214 | (27.4) | 203 | (100.0) | 675 | (37.9) | |
| Unknown due to unknown size | 26 | 16 | 0 | 42 | |||||
| High Risk6 | |||||||||
| No | 477 | (59.6) | 466 | (59.6) | 0 | (0.0) | 943 | (52.8) | |
| Yes | 323 | (40.4) | 316 | (40.4) | 203 | (100.0) | 842 | (47.2) | |
| Unknown due to unknown size | 24 | 15 | 0 | 39 | |||||
Note: Counts and percentages of non-missing data.
Full Factorial Cohort: Celebrex vs Selenium vs Combination vs Placebo, 11/27/2001-12/16/2004
Selenium Cohort: Selenium vs Placebo, 02/02/2005-11/26/2008
Advanced Adenoma Cohort: Selenium vs Placebo among participants selected for advanced adenoma at qualification, 07/30/2008-01/19/2011
One participant was diagnosed with CRC less than 6 months after randomization. This is classified as a baseline event (i.e. not endpoint).
Advanced adenoma defined as having one or more of the following features: adenoma ≥1cm, with tubulovillous or villous histology, and/or with high grade dysplasia.
High risk defined as having an advanced adenoma or ≥3 adenomas.
Concomitant low-dose aspirin
Approaching 50% of participants continued low-dose aspirin during the trial. As described, our sample size provides 94% statistical power to detect a 25% reduction due to the selenium intervention averaged across non-aspirin and low-dose aspirin users. As a secondary endpoint, we will also have adequate power to assess whether low-dose aspirin modifies the effect of selenium. The power calculation for the latter analysis assumes an adenoma recurrence rate of 49%, a marginal OR of 0.6 due to selenium (a 25% reduction in the recurrence rate), and a marginal OR for low-dose aspirin of 0.8 (a 10% reduction in the recurrence rate). We will have >80% power to detect an interaction odds ratio of ≤0.5 (a combined 33% reduction in the adenoma recurrence rate from selenium + low-dose aspirin).
Selenium plasma levels
Median baseline plasma selenium levels (interquartile range) in the Full Factorial, Selenium and Advanced Adenoma Cohorts, respectively, were 134.3 (120.4 – 149.8), 137.6 (122.0 – 157.7) and 133.4 (121.9 – 147.8) ng/ml (Table 3). In the Nutritional Prevention of Cancer (NPC) trial of selenized yeast, reductions in overall cancer risk with the selenium intervention were confined to participants whose baseline selenium levels were in the lowest two tertiles (<121.6 ng/ml) (28). Chemoprevention trials in which nutritional supplements, including selenium (44), have been administered to already-replete study populations have been criticized because supplementation of a given intervention above a certain preexisting threshold may confer no additional protection against the neoplastic condition in question (45). The median baseline plasma selenium level of the study population in the current trial was in the replete range. As noted, modification of the effects of the selenium intervention by baseline plasma selenium level will be analyzed.
Table 3. Baseline Selenium Intake and Plasma levels.
| Full Factorial Cohort1 (n=824) |
Selenium Cohort2 (n=797) |
Advanced Adenoma Cohort3 (n=203) |
Total (n=1824) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Selenium supplement use at recruitment |
|||||||||
| 0 μg | 366 | (44.4) | 383 | (48.1) | 103 | (50.7) | 852 | (46.7) | |
| 1-50 μg | 356 | (43.2) | 329 | (41.3) | 43 | (21.2) | 728 | (39.9) | |
| 51-199 μg | 68 | (8.3) | 62 | (7.8) | 50 | (24.6) | 180 | (9.9) | |
| ≥200 μg | 34 | (4.1) | 23 | (2.9) | 7 | (3.4) | 64 | (3.5) | |
| Selenium supplement use at randomization |
|||||||||
| 0 μg | 283 | (42.2) | 410 | (51.4) | 117 | (57.6) | 810 | (48.5) | |
| 1-50 μg | 387 | (57.8) | 387 | (48.6) | 86 | (42.4) | 860 | (51.5) | |
| Missing4 | 154 | 0 | 0 | 154 | |||||
| Selenium Intake from food (μg), median (IQR) |
94.5 (70.5-127.6) | 92.8 (68.7-123.5) | 91.0 (67.9-129.8) | 93.4 (69.1-125.7) | |||||
| Missing5 | 39 | 49 | 10 | 98 | |||||
| Selenium (ng/ml) measured in plasma, median (IQR) | 134.3 (120.4-149.8) | 137.6 (122.0-157.7) | 133.4 (121.9-147.8) | 135.3 (121.3-152.7) | |||||
| Missing6 | 7 | 5 | 2 | 14 | |||||
Note: Counts and percentages of non-missing data unless otherwise noted. IQR=Interquartile Range
Full Factorial Cohort: Celebrex vs Selenium vs Combination vs Placebo, 11/27/2001-12/16/2004
Selenium Cohort: Selenium vs Placebo, 02/02/2005-11/26/2008
Advanced Adenoma Cohort: Selenium vs Placebo among participants selected for advanced adenoma at qualification, 07/30/2008-01/19/2011
Missing data in the original cohort because the first version of the form omitted this question.
Some participants refused to fill out the food frequency questionnaire.
Selenium sample not obtained due to blood draw difficulties
Accrual period
Recruitment of the originally planned 1,600 participants extended over seven years from November, 2001 until November, 2008. The length of the recruitment period, which was much longer than was required in our earlier WBF (40) and UDCA (41) colorectal adenoma prevention trials, was unanticipated. Several factors contributed. Prior to the Health Insurance Portability and Accountability Act (HIPAA), potential participants could be identified and contacted concerning possible participation simply from perusal of endoscopy unit and pathology department logs. The introduction of HIPAA in April, 2003 necessitated developing lengthier processes with additional steps protecting patient confidentiality before study staff could directly contact potential participants. The modified recruitment practices had to be tailored to each study site. Just as post-HIPAA modifications to recruitment strategies were taking effect and recruitment was gathering pace again, adverse events associated with rofecoxib (VIOXX) were announced in graphic terms in the national media. This slowed recruitment to a trial that included celecoxib, an agent from the same class—the coxibs—as rofecoxib, even before the FDA compulsorily withdrew celecoxib and all other coxibs in December, 2004.
Causes for consideration of early termination
Results from two other selenium chemoprevention trials that were published during accrual to the current trial compelled us to consider early termination. The first was a report that supplementation with selenized yeast was associated with increased risk for type 2 diabetes (T2D) (46) and the second was the early termination, for lack of any effect, of the SELECT Trial of selenium and vitamin E for prostate cancer prevention (47).
In a secondary analysis of the NPC trial (28) that was published in 2007, a positive association was reported between selenium supplementation and self-reported diagnoses of T2D during the blinded phase of the trial (46). Participants were followed for an average of 7.7 years and the hazard ratio for development of T2D in those randomized to selenized yeast compared to placebo was 1.55 (95% CI, 1.03 to 2.33). Reports of diabetes came from three sources: self-report at clinic visits, reported use of drugs for diabetes, and reports in medical record documents. Medical record requests were then sent to the primary physicians for every patient with a report of diabetes.
In our ongoing selenium trial, fasting blood specimens for plasma glucose and other measurements are drawn from all participants at baseline and annually thereafter during the blinded phase of the trial. The EDSMC conducted an unblinded analysis of fasting plasma glucose data in our trial after the report of selenium-related increased risk for T2D in NPC trial participants; the investigators remained blinded. After this analysis, the Principal Investigator was instructed by the EDSMC to continue the trial without modification. The fasting blood specimens available for the complete trial cohort will provide a unique opportunity to compare the incidence of T2D in the selenium and placebo groups based on plasma glucose levels and other analyses that are planned.
As noted, the SELECT Trial of the effects of selenium (200 μg daily as selenomethionine) and vitamin E (400 IU daily), alone or in combination, on the risk of prostate cancer in 35,533 men (48) was terminated in October, 2009 before completion. The reason for early termination was the result of a planned interim analysis by an independent data and safety monitoring committee. This showed that neither selenium nor vitamin E had any effect on prostate cancer incidence (47). In light of the early termination of SELECT, the EDSMC for our selenium trial requested a futility analysis in November, 2009. The committee recommended continuation of the trial without modification on the basis of the results of this analysis.
There are several important respects in which our ongoing selenium colorectal adenoma prevention trial differs from the SELECT trial and could, therefore, have a positive outcome. First, selenium may have tissue-specific effects and the target organ for our trial is the colorectum, not the prostate. Second, the endpoint in our trial is adenoma recurrence as opposed to invasive cancer in SELECT, and it is possible that selenium may prevent or reverse premalignant earlier adenoma stages of colorectal carcinogenesis. Finally, selenized yeast, the intervention in our trial, contains additional selenium compounds (49) to selenomethionine and one or more of these compounds may have additional actions with chemopreventive potential to those of the selenomethionine-only intervention used in SELECT.
In summary, while accrual to our trial took longer than expected and administration of the celecoxib intervention was necessarily abbreviated, we are on schedule to unblind trial results for the full study cohort of 1,824 participants in 2013. Close involvement of a vigilant EDSMC enabled us to sustain the trial without compromising patient safety when first celecoxib was withdrawn and then the possibility that selenium supplementation may be associated with increased T2D risk arose. An interactive trial infrastructure involving study physicians, biostatisticians and other key investigators, EDSMC and the funding agency enabled us to enhance accrual of a high-risk group—patients with advanced adenomas—without delaying completion of the trial. Most importantly, the study will answer in the setting of a randomized trial the previously unanswered question of whether a selenized yeast intervention prevents the development of premalignant colorectal adenomas. We will add to the existing body of information on coxib colorectal adenoma chemoprevention. Finally, we will provide detailed novel data of high public health significance on the potential adverse effects of selenium supplementation on glucoregulatory function and risk for T2D.
Acknowledgements
We recognize with much gratitude the research nurses and clinic staff: Mildred Arnold, Patricia Blair, Darlene Bunpian, Amy Carrier, Marita Clifford, Ann Dejong-Ruhnau, Theresa Dunn, Pat Graham, Dianne Parish, Eugenia M. Schleski and Christina Yang-Hellewell. We are most grateful to staff of the study high-throughput laboratory at the University of Arizona Cancer Center: Carole Kepler Christina Preece and Manuel Snyder.
We thank the members of the trial External Data and Safety Monitoring Committee for their continuing and unstinting efforts: Ross Prentice, Ph.D., Chair (Fred Hutchinson Cancer Research Center, Seattle, WA), Jeffrey Borer, M.D. (State University of New York, Downstate Medical Center, Brooklyn, NY), Edward Giovannucci, M.D., Sc.D. (Harvard School of Public Health, Boston, MA), Linda Hicks (Tucson, AZ) and David Ransohoff, M.D. (University of North Carolina at Chapel Hill, NC).
Grant support: National Cancer Institute P01 CA041108 (M.P. Lance), R01 CA151708 (M.P. Lance and P. Thompson-Carino) P30 CA23074 (D.S. Alberts)
Grant Support
Supported by grants P01 CA041108, R01 CA151708 and P30 CA23074 from the National Cancer Institute/National Institutes of Health, Bethesda, MD.
Footnotes
Conflicts of interest: None of the authors of this manuscript has had any scientific, commercial and/or financial relationships that might be perceived as a real or potential conflict of interest.
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012 Jan-Feb;62(1):10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Mandel JS, Church TR, Ederer F, Bond JH. Colorectal cancer mortality: effectiveness of biennial screening for fecal occult blood. J Natl Cancer Inst. 1999;91:434–7. doi: 10.1093/jnci/91.5.434. [DOI] [PubMed] [Google Scholar]
- 3.Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N Engl J Med. 1993 May 13;328(19):1365–71. doi: 10.1056/NEJM199305133281901. [DOI] [PubMed] [Google Scholar]
- 4.Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JM, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010 May 8;375(9726):1624–33. doi: 10.1016/S0140-6736(10)60551-X. [DOI] [PubMed] [Google Scholar]
- 5.Zauber AG, Winawer SJ, O’Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012 Feb 23;366(8):687–96. doi: 10.1056/NEJMoa1100370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M. Protection From Colorectal Cancer After Colonoscopy. Ann Intern Med. 2011 Jan 4;154(1):22–30. doi: 10.7326/0003-4819-154-1-201101040-00004. 2011. [DOI] [PubMed] [Google Scholar]
- 7.Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009 Jan 6;150(1):1–8. doi: 10.7326/0003-4819-150-1-200901060-00306. [DOI] [PubMed] [Google Scholar]
- 8.Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010 Oct;139(4):1128–37. doi: 10.1053/j.gastro.2010.06.052. [DOI] [PubMed] [Google Scholar]
- 9.Smith RA, Cokkinides V, Brooks D, Saslow D, Shah M, Brawley OW. Cancer screening in the United States, 2011: A review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer J Clin. 2011 Jan-Feb;61(1):8–30. doi: 10.3322/caac.20096. [DOI] [PubMed] [Google Scholar]
- 10.Lance P. Chemoprevention for colorectal cancer: some progress but a long way to go. Gastroenterology. 2008 Jan;134(1):341–3. doi: 10.1053/j.gastro.2007.11.024. [DOI] [PubMed] [Google Scholar]
- 11.Baron JA, Beach M, Mandel JS, van Stolk RU, Haile RW, Sandler RS, et al. Calcium Polyp Prevention Study Group Calcium supplements for the prevention of colorectal adenomas. N Engl J Med. 1999 Jan 14;340(2):101–7. doi: 10.1056/NEJM199901143400204. [DOI] [PubMed] [Google Scholar]
- 12.Baron JA, Cole BF, Sandler RS, Haile RW, Ahnen D, Bresalier R, et al. A randomized trial of aspirin to prevent colorectal adenomas. N Engl J Med. 2003 Mar 6;348(10):891–9. doi: 10.1056/NEJMoa021735. [DOI] [PubMed] [Google Scholar]
- 13.Sandler RS, Halabi S, Baron JA, Budinger S, Paskett E, Keresztes R, et al. A randomized trial of aspirin to prevent colorectal adenomas in patients with previous colorectal cancer. N Engl J Med. 2003;348:883–90. doi: 10.1056/NEJMoa021633. [DOI] [PubMed] [Google Scholar]
- 14.Arber N, Eagle CJ, Spicak J, Racz I, Dite P, Hajer J, et al. Celecoxib for the prevention of colorectal adenomatous polyps. N Engl J Med. 2006 Aug 31;355(9):885–95. doi: 10.1056/NEJMoa061652. [DOI] [PubMed] [Google Scholar]
- 15.Cole BF, Logan RF, Halabi S, Benamouzig R, Sandler RS, Grainge MJ, et al. Aspirin for the chemoprevention of colorectal adenomas: meta-analysis of the randomized trials. J Natl Cancer Inst. 2009 Feb 18;101(4):256–66. doi: 10.1093/jnci/djn485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baron JA, Sandler RS, Bresalier RS, Quan H, Riddell R, Lanas A, et al. A randomized trial of rofecoxib for the chemoprevention of colorectal adenomas. Gastroenterology. 2006 Dec;131(6):1674–82. doi: 10.1053/j.gastro.2006.08.079. [DOI] [PubMed] [Google Scholar]
- 17.Rothwell PM, Wilson M, Elwin CE, Norrving B, Algra A, Warlow CP, et al. Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet. 2010 Nov 20;376(9754):1741–50. doi: 10.1016/S0140-6736(10)61543-7. [DOI] [PubMed] [Google Scholar]
- 18.Burn J, Gerdes AM, Macrae F, Mecklin JP, Moeslein G, Olschwang S, et al. Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. Lancet. 2011 Dec 17;378(9809):2081–7. doi: 10.1016/S0140-6736(11)61049-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dannenberg AJ, Altorki NK, Boyle JO, Dang C, Howe LR, Weksler BB, et al. Cyclo-oxygenase 2: a pharmacological target for the prevention of cancer. Lancet Oncol. 2001 Sep;2(9):544–51. doi: 10.1016/S1470-2045(01)00488-0. [DOI] [PubMed] [Google Scholar]
- 20.Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nonsteroidal antiinflammatory drugs. N Engl J Med. 1999;340:1888–99. doi: 10.1056/NEJM199906173402407. [DOI] [PubMed] [Google Scholar]
- 21.Bertagnolli MM, Eagle CJ, Zauber AG, Redston M, Solomon SD, Kim K, et al. Celecoxib for the prevention of sporadic colorectal adenomas. N Engl J Med. 2006 Aug 31;355(9):873–84. doi: 10.1056/NEJMoa061355. [DOI] [PubMed] [Google Scholar]
- 22.Willett WC, Polk BF, Morris JS, Stampfer MJ, Pressel S, Rosner B, et al. Prediagnostic serum selenium and risk of cancer. Lancet. 1983 Jul 16;2(8342):130–4. doi: 10.1016/s0140-6736(83)90116-2. [DOI] [PubMed] [Google Scholar]
- 23.Comstock GW, Bush TL, Helzlsouer K. Serum retinol, beta-carotene, vitamin E, and selenium as related to subsequent cancer of specific sites. Am J Epidemiol. 1992 Jan 15;135(2):115–21. doi: 10.1093/oxfordjournals.aje.a116264. [DOI] [PubMed] [Google Scholar]
- 24.Combs GF, Jr., Gray WP. Chemopreventive agents: selenium. Pharmacol Ther. 1998 Sep;79(3):179–92. doi: 10.1016/s0163-7258(98)00014-x. [DOI] [PubMed] [Google Scholar]
- 25.Kryukov GV, Castellano S, Novoselov SV, Lobanov AV, Zehtab O, Guigo R, et al. Characterization of mammalian selenoproteomes. Science. 2003 May 30;300(5624):1439–43. doi: 10.1126/science.1083516. [DOI] [PubMed] [Google Scholar]
- 26.Samaha HS, Hamid R, el-Bayoumy K, Rao CV, Reddy BS. The role of apoptosis in the modulation of colon carcinogenesis by dietary fat and by the organoselenium compound 1,4-phenylenebis(methylene)selenocyanate. Cancer Epidemiol Biomarkers Prev. 1997 Sep;6(9):699–704. [PubMed] [Google Scholar]
- 27.McKenzie RC, Rafferty TS, Beckett GJ. Selenium: an essential element for immune function. Immunol Today. 1998 Aug;19(8):342–5. doi: 10.1016/s0167-5699(98)01294-8. [DOI] [PubMed] [Google Scholar]
- 28.Clark L, Combs J, J F, Turnbull BW, Slate EH, Chalker DK, Chow J, et al. Effects of selenium supplementation for cancer prevention in patient with carcinomas of the skin. JAMA. 1996;276:1957–63. [PubMed] [Google Scholar]
- 29.Duffield-Lillico AJ, Reid ME, Turnbull BW, Combs GF, Jr., Slate EH, Fischbach LA, et al. Baseline characteristics and the effect of selenium supplementation on cancer incidence in a randomized clinical trial: a summary report of the Nutritional Prevention of Cancer Trial. Cancer Epidemiol Biomarkers Prev. 2002 Jul;11(7):630–9. [PubMed] [Google Scholar]
- 30.Jacobs ET, Jiang R, Alberts DS, Greenberg ER, Gunter E, Karagas MR, et al. Selenium and colorectal adenoma: results of a pooled analysis. J Natl Cancer Inst. 2004 Nov 17;96(22):1669–75. doi: 10.1093/jnci/djh310. [DOI] [PubMed] [Google Scholar]
- 31.Bjelakovic G, Nikolova D, Simonetti RG, Gluud C. Antioxidant supplements for prevention of gastrointestinal cancers: a systematic review and meta-analysis. Lancet. 2004 Oct 2;364(9441):1219–28. doi: 10.1016/S0140-6736(04)17138-9. [DOI] [PubMed] [Google Scholar]
- 32.Bjelakovic G, Nikolova D, Simonetti RG, Gluud C. Systematic review: primary and secondary prevention of gastrointestinal cancers with antioxidant supplements. Aliment Pharmacol Ther. 2008 Sep 15;28(6):689–703. doi: 10.1111/j.1365-2036.2008.03785.x. [DOI] [PubMed] [Google Scholar]
- 33.Bresalier RS, Sandler RS, Quan H, Bolognese JA, Oxenius B, Horgan K, et al. Cardiovascular events associated with rofecoxib in a colorectal adenoma chemoprevention trial. N Engl J Med. 2005 Mar 17;352(11):1092–102. doi: 10.1056/NEJMoa050493. [DOI] [PubMed] [Google Scholar]
- 34.Solomon SD, McMurray JJ, Pfeffer MA, Wittes J, Fowler R, Finn P, et al. Cardiovascular risk associated with celecoxib in a clinical trial for colorectal adenoma prevention. N Engl J Med. 2005 Mar 17;352(11):1071–80. doi: 10.1056/NEJMoa050405. [DOI] [PubMed] [Google Scholar]
- 35.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010 Jun 1;152(11):726–32. doi: 10.7326/0003-4819-152-11-201006010-00232. [DOI] [PubMed] [Google Scholar]
- 36.Chow HH, Anavy N, Salazar D, Frank DH, Alberts DS. Determination of celecoxib in human plasma using solid-phase extraction and high-performance liquid chromatography. J Pharm Biomed Anal. 2004 Jan 27;34(1):167–74. doi: 10.1016/j.japna.2003.08.018. [DOI] [PubMed] [Google Scholar]
- 37.Winawer SJ, Zauber AG, Fletcher RH, Stillman JS, O’Brien MJ, Levin B, et al. Guidelines for colonoscopy surveillance after polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. CA Cancer J Clin. 2006 May-Jun;56(3):143–59. doi: 10.3322/canjclin.56.3.143. quiz 84-5. [DOI] [PubMed] [Google Scholar]
- 38.Itzkowitz SH, Potack J. Colonic Polyps and Polyposis Syndromes. In: Feldman M, Friedman LS, Brandt LJ, editors. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. 9th ed Saunders; Philadelphia: 2010. pp. 2155–89. [Google Scholar]
- 39.Winawer SJ, Zauber AG, Ho MN, O’Brien MJ, Gottlieb LS, Sternberg SS, et al. Prevention of colorectal cancer by colonoscopic polypectomy. N Engl J Med. 1993;329:1977–81. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 40.Alberts DS, Martínez ME, Roe DJ, Guillén-Rodríguez J, Marshall JR, van Leeuwen B, et al. Lack of effect of a high-fiber cereal supplement on the recurrence of colorectal adenomas. N Engl J Med. 2000;342:1156–62. doi: 10.1056/NEJM200004203421602. [DOI] [PubMed] [Google Scholar]
- 41.Alberts DS, Martinez ME, Hess LM, Einspahr JG, Green SB, Bhattacharyya AK, et al. Phase III trial of ursodeoxycholic acid to prevent colorectal adenoma recurrence. J Natl Cancer Inst. 2005 Jun 1;97(11):846–53. doi: 10.1093/jnci/dji144. [DOI] [PubMed] [Google Scholar]
- 42.Solomon SD, Wittes J, Finn PV, Fowler R, Viner J, Bertagnolli MM, et al. Cardiovascular risk of celecoxib in 6 randomized placebo-controlled trials: the cross trial safety analysis. Circulation. 2008 Apr 22;117(16):2104–13. doi: 10.1161/CIRCULATIONAHA.108.764530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martinez ME, Baron JA, Lieberman DA, Schatzkin A, Lanza E, Winawer SJ, et al. A pooled analysis of advanced colorectal neoplasia diagnoses after colonoscopic polypectomy. Gastroenterology. 2009 Mar;136(3):832–41. doi: 10.1053/j.gastro.2008.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bleys J, Navas-Acien A, Guallar E. Selenium and diabetes: more bad news for supplements. Ann Intern Med. 2007 Aug 21;147(4):271–2. doi: 10.7326/0003-4819-147-4-200708210-00177. [DOI] [PubMed] [Google Scholar]
- 45.Martinez ME, Marshall JR, Giovannucci E. Diet and cancer prevention: the roles of observation and experimentation. Nat Rev Cancer. 2008 Aug 7; doi: 10.1038/nrc2441. [DOI] [PubMed] [Google Scholar]
- 46.Stranges S, Marshall JR, Natarajan R, Donahue RP, Trevisan M, Combs GF, et al. Effects of long-term selenium supplementation on the incidence of type 2 diabetes: a randomized trial. Ann Intern Med. 2007 Aug 21;147(4):217–23. doi: 10.7326/0003-4819-147-4-200708210-00175. [DOI] [PubMed] [Google Scholar]
- 47.Lippman SM, Klein EA, Goodman PJ, Lucia MS, Thompson IM, Ford LG, et al. Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the Selenium and Vitamin E Cancer Prevention Trial (SELECT) JAMA. 2009 Jan 7;301(1):39–51. doi: 10.1001/jama.2008.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lippman SM, Goodman PJ, Klein EA, Parnes HL, Thompson IM, Jr., Kristal AR, et al. Designing the Selenium and Vitamin E Cancer Prevention Trial (SELECT) J Natl Cancer Inst. 2005 Jan 19;97(2):94–102. doi: 10.1093/jnci/dji009. [DOI] [PubMed] [Google Scholar]
- 49.Block E, Glass RS, Jacobsen NE, Johnson S, Kahakachchi C, Kaminski R, et al. Identification and synthesis of a novel selenium-sulfur amino acid found in selenized yeast: Rapid indirect detection NMR methods for characterizing low-level organoselenium compounds in complex matrices. J Agric Food Chem. 2004 Jun 16;52(12):3761–71. doi: 10.1021/jf049887z. [DOI] [PubMed] [Google Scholar]