Abstract
Pulmonary hypertension is characterized by elevated pulmonary arterial pressure and secondary right ventricular failure. A thromboembolic occlusion of the proximal or distal pulmonary vasculature results in chronic thromboembolic pulmonary hypertension. We report an uncommon case that presented to our hospital with symptoms of dyspnea on exertion over 2 years. The patient had been treated for profound pulmonary thrombosis and right ventricular failure with adequate anticoagulation and sildenafil. Our echocardiography disclosed a large atrial septal defect with severe pulmonary hypertension and right ventricular failure. A diagnosis of Eisenmenger syndrome with pulmonary artery thrombosis was made. Although Eisenmenger syndrome with pulmonary thrombosis is well described in western societies, a huge pulmonary thrombosis is seldom reported in eastern countries. Profound pulmonary thrombosis may obfuscate the actual diagnosis of pulmonary artery hypertension with underlying congenital heart disease. A physical examination and echocardiography are essential in patients with pulmonary hypertension.
Keywords: Pulmonary embolism, Eisenmenger syndrome
Introduction
Pulmonary hypertension is characterized by elevated pulmonary arterial pressure and possible subsequent secondary right ventricular failure. Patients with pulmonary hypertension may initially complain of dyspnea upon exertion, lethargy, and fatigue. As the disease progresses, right ventricular failure develops, and exertional chest pain, syncope, and edema may occur. Chronic thromboembolic pulmonary hypertension, recognized as a thromboembolic occlusion of the proximal or distal pulmonary vasculature, can be diagnosed accurately by computed tomography or a pulmonary perfusion scan. However, pulmonary thrombosis can be secondary to other conditions such as primary pulmonary hypertension,1) hypercoagulation status, deep venous thrombosis, or Eisenmenger syndrome. We report an uncommon case of a secundum type of atrial septal defect (ASD) with Eisenmenger syndrome that presented with pulmonary hypertension, profound pulmonary thrombosis, and right ventricular failure. Eisenmenger syndrome with pulmonary thrombosis is well described in western countries.2-5) However, a huge pulmonary thrombosis is seldom reported in eastern countries. The mechanisms contributing to thrombus formation are poorly understood. Profound pulmonary thrombosis may conceal the actual diagnosis of pulmonary artery hypertension resulting from underlying congenital heart disease.
Case
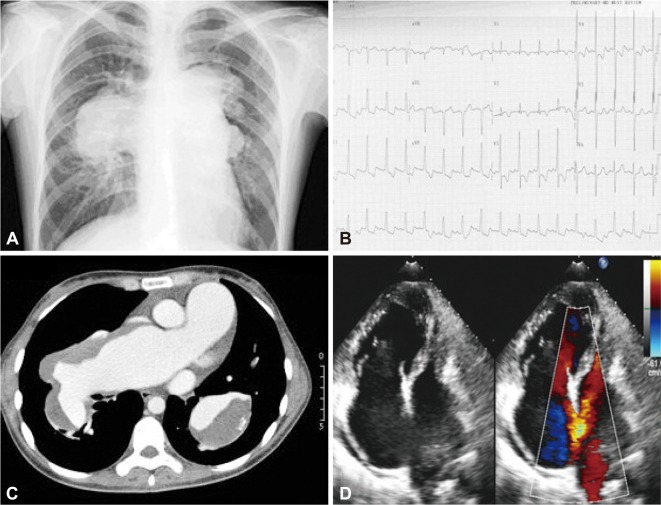
A 39-year-old woman presented to our outpatient department with a 2 year history of palpitation, shortness of breath, and dyspnea on exertion. For 1 year, she had been told that she had pulmonary artery hypertension without knowing the leading cause. During the period, she had received anticoagulation therapy and sildenafil. The symptoms persisted and progressed. Tracing her medical history, she denied smoking, previous hormone therapy, pregnancy, childbearing, or any other systemic illnesses. On admission, her oxygen saturation was 90% under room air. A physical examination revealed grade III systolic murmurs over the left lower sternal border and a wide fixed splitting S2. Grade I pre-tibia pitting edema was also noted. Laboratory examinations showed normal blood cell counts, with a target international ratio of 2.0, and a mildly elevated D-dimer level (2.0 mg/L; reference, <0.5 mg/L). Chest radiography revealed marked enlargement and a lobulated contour to the hilar shadows of bilateral lungs (Fig. 1A). An electrocardiogram revealed a right axis deviation and bi-ventricular hypertrophy with a strain pattern (Fig. 1B). A thoracic computed tomography scan showed a huge thrombus in the aneurysmal dilatation of the proximal pulmonary arteries (Fig. 1C). Lower-limb Doppler sonography disclosed no deep venous thrombosis. We also surveyed possible causes of her pro-coagulant status, including hepatitis serum marker, anti-human immunodeficiency virus antibody, the Venereal Disease Research Laboratory test, anti-double stranded deoxyribonucleic acid antibodies, anti-phospholipid IgG/IgM, anti-beta 2 glycoprotein IgG/IgM, anti-nuclear antibody, lupus anticoagulant, protein C, protein S, anti-thrombin III, and homocysteine level without positive findings. An underlying malignancy was ruled out by careful examination. Transthoracic echocardiography revealed profound pulmonary hypertension with right ventricular hypertrophy and dysfunction. The estimated pulmonary arterial systolic pressure was 207 mm Hg. Transesophageal echocardiography showed a large secundum type ASD with a bi-directional shunt and a pulmonary-to-systemic flow ratio (Qp/Qs) of 3.0 (Fig. 1D). A right heart catheter was also done. Pulmonary thrombosis with an ASD and Eisenmenger syndrome was thus diagnosed. A thrombectomy with aneurysm repair requiring a bypass would have been an extremely high risk operation and is reserved for acute deterioration. Thus, a heart-lung transplantation was arranged for her.
Fig. 1.
Pulmonary arterial thrombosis in atrial septal defect with Eisenmenger syndrome. A: chest radiography revealed marked enlargement and lobulated contour of the hilar shadows of bilateral pulmonary arteries. B: electrocardiogram revealed right axis deviation and bi-ventricular hypertrophy with strain pattern. C: thoracic computed tomographic (CT) scan showed thrombus in the aneurysmal dilatation of proximal pulmonary arteries. D: the transthoracic echocardiography showed a large secundum type atrial septal defect (ASD).
Discussion
Pulmonary hypertension with profound pulmonary thrombosis can be due to many reasons such as emboli from other sites, hypercoagulation disease, primary pulmonary hypertension, or Eisenmenger syndrome. In situ thrombus formation was suspected in this patient in the absence of hereditary thrombophilia disease or other thrombogenic foci. Chronic thromboembolic pulmonary hypertension is defined as mean pulmonary artery pressure >25 mm Hg that persists 6 months after a pulmonary embolism has been diagnosed.6) No obvious acute deteriorating episodes occurred in this patient. Insidious and prolonged symptoms may imply the slowly progressive nature of the disease. Although primary pulmonary hypertension increases the risk for thrombogenesis, it seldom results in massive hemodynamically significant pulmonary arterial thrombosis.7) After a careful physical examination and compact echocardiography, ASD with Eisenmenger syndrome and a huge pulmonary thrombosis were diagnosed.
Eisenmenger syndrome is the clinical phenotype of an extreme form of pulmonary arterial hypertension associated with congenital heart disease. Chronic increasing pulmonary blood flow eventually reverses the original left-to-right shunts to right-to-left or bidirectional shunts through the original lesions. Patients with Eisenmenger syndrome have a substantial risk for pulmonary artery thrombus formation of 21-29%.2),3) Several studies have found women and patients with lower oxygen saturation,2) low pulmonary artery velocity,3) and biventricular dysfunction, who are at the highest risk for developing a thrombosis.3) The mechanisms of thrombus formation are poorly understood. Previous studies have failed to identify significant hypercoagulation status or thrombus formation outside the pulmonary trunk in this group of patients. Platelet function is consistently abnormal in patients with Eisenmenger syndrome but no differences are observed between thrombosis and non-thrombosis groups.2) In situ thrombosis formation is a well-accepted concept.2) Large aneurysmal dilatations of the pulmonary artery with heavy calcification are commonly seen in these patients. Chronic endothelial damage can be caused by increasing shear stress on the vessel walls, increasing blood volume, viscosity, and chronic hypoxemia.8),9) These observations imply that structural and functional damage to the pulmonary artery endothelium may play a critical role during the development of pulmonary thrombosis.10) Although a previous study failed to show evidence of systemic inflammation in those with a thrombus, as gauged by C-reactive protein levels, a more specific endothelium functional assay is lacking in such a group of patients.2)
Patients with primary pulmonary hypertension aggravated by an intravascular thrombosis are routinely anticoagulated to improve survival.11),12) However, Eisenmenger syndrome poses a medical dilemma because it includes both bleeding and clotting tendencies. Hemoptysis is observed in 20% of patients with Eisenmenger syndrome. Anticoagulative therapy can aggravate this condition.5) Cyanotic patients have labile international normalized ratios under anticoagulative therapy. Hence, the role of anticoagulation treatment needs further investigation.2-5) Surgical intervention experience including a thrombectomy and aneurysmal repair in this group of patients is limited. In our case, we preferred reserving the operation for acute hemodynamic deterioration. Medical treatment including endothelin receptor antagonists, phosphodiesterase type-5 inhibitors, prostacyclin, and prostacyclin analogs have proven beneficial in patients with Eisenmenger syndrome.13) A combination of anticoagulation and selective phosphodiesterase type 5 inhibitors were administered to our patient.
In conclusion, we report an uncommon case that presented with huge pulmonary thrombi accompanied by pulmonary hypertension and right-side heart failure. Primary pulmonary hypertension with secondary thrombus formation was diagnosed at first.
However, after a thorough examination, an ASD with Eisenmenger syndrome combined with pulmonary artery thrombosis was diagnosed. Profound pulmonary thrombosis may obfuscate the actual diagnosis of pulmonary artery hypertension with underlying congenital heart disease. This report reminds us of the importance of suspecting pulmonary arterial hypertension associated with Eisenmenger syndrome when we see patients with proximal thrombi in pulmonary arteries.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Hassell KL. Altered hemostasis in pulmonary hypertension. Blood Coagul Fibrinolysis. 1998;9:107–117. doi: 10.1097/00001721-199803000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Broberg CS, Ujita M, Prasad S, et al. Pulmonary arterial thrombosis in Eeisenmenger syndrome is associated with biventricular dysfunction and decreased pulmonary flow velocity. J Am Coll Cardiol. 2007;50:634–642. doi: 10.1016/j.jacc.2007.04.056. [DOI] [PubMed] [Google Scholar]
- 3.Silversides CK, Granton JT, Konen E, Hart MA, Webb GD, Therrien J. Pulmonary thrombosis in adults with Eisenmenger syndrome. J Am Coll Cardiol. 2003;42:1982–1987. doi: 10.1016/j.jacc.2003.07.022. [DOI] [PubMed] [Google Scholar]
- 4.Jensen AS, Iversen K, Vejlstrup NG, Sondergaard L. Images in cardiovascular medicine: pulmonary artery thrombosis and hemoptysis in Eisenmenger syndrome. Circulation. 2007;115:e632–e634. doi: 10.1161/CIRCULATIONAHA.107.695312. [DOI] [PubMed] [Google Scholar]
- 5.Broberg C, Ujita M, Babu-Narayan S, et al. Massive pulmonary artery thrombosis with haemoptysis in adults with Eisenmenger's syndrome: a clinical dilemma. Heart. 2004;90:e63. doi: 10.1136/hrt.2004.039198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piazza G, Goldhaber SZ. Chronic thromboembolic pulmonary hypertension. N Engl J Med. 2011;364:351–360. doi: 10.1056/NEJMra0910203. [DOI] [PubMed] [Google Scholar]
- 7.Moser KM, Fedullo PF, Finkbeiner WE, Golden J. Do patients with primary pulmonary hypertension develop extensive central thrombi? Circulation. 1995;91:741–745. doi: 10.1161/01.cir.91.3.741. [DOI] [PubMed] [Google Scholar]
- 8.Niwa K, Perloff JK, Kaplan S, Child JS, Miner PD. Eisenmenger syndrome in adults: ventricular septal defect, truncus arteriosus, univentricular heart. J Am Coll Cardiol. 1999;34:223–232. doi: 10.1016/s0735-1097(99)00153-9. [DOI] [PubMed] [Google Scholar]
- 9.Niwa K, Perloff JK, Bhuta SM, et al. Structural abnormalities of great arterial walls in congenital heart disease: light and electron microscopic analyses. Circulation. 2001;103:393–400. doi: 10.1161/01.cir.103.3.393. [DOI] [PubMed] [Google Scholar]
- 10.Lopes AA, Caramurú LH, Maeda NY. Endothelial dysfunction associated with chronic intravascular coagulation in secondary pulmonary hypertension. Clin Appl Thromb Hemost. 2002;8:353–358. doi: 10.1177/107602960200800407. [DOI] [PubMed] [Google Scholar]
- 11.Fuster V, Steele PM, Edwards WD, Gersh BJ, McGoon MD, Frye RL. Primary pulmonary hypertension: natural history and the importance of thrombosis. Circulation. 1984;70:580–587. doi: 10.1161/01.cir.70.4.580. [DOI] [PubMed] [Google Scholar]
- 12.Rich S, Kaufmann E, Levy PS. The effect of high doses of calcium channel blockers on survival in primary pulmonary hypertension. N Engl J Med. 1992;327:76–81. doi: 10.1056/NEJM199207093270203. [DOI] [PubMed] [Google Scholar]
- 13.Beghetti M, Gallè N. Eisenmenger syndrome a clinical perspective in a new therapeutic era of pulmonary arterial hypertension. J Am Coll Cardiol. 2009;53:733–740. doi: 10.1016/j.jacc.2008.11.025. [DOI] [PubMed] [Google Scholar]