Abstract
Digital clubbing is an ancient and important clinical signs in medicine. Although clubbed fingers are mostly asymptomatic, it often predicts the presence of some dreaded underlying diseases. Its exact pathogenesis is not known, but platelet-derived growth factor and vascular endothelial growth factor are recently incriminated in its causation. The association of digital clubbing with various disease processes and its clinical implications are discussed in this review.
KEY WORDS: Cancer, digital clubbing, hypertrophic osteoarthropathy, megakaryocytes, vascular endothelial growth factor
INTRODUCTION
Digital clubbing is characterized by a focal bulbous enlargement of the terminal segments of the fingers and/or toes due to proliferation of connective tissue between nail matrix and the distal phalanx. It results in increase in both anteroposterior and lateral diameter of the nails.[1] Clubbed fingers are also known as watch-glass nails, drumstick fingers, and Hippocratic fingers/nails. It was first described by Hippocrates[2] nearly 2500 years ago in a patient with empyema. Because of this, it is often described as Hippocratic finger and is regarded to be the oldest sign in clinical medicine.[3] Later on, it was found to be associated with a variety of clinical conditions including bronchiectasis, lung cancer, cirrhosis of liver, cyanotic congenital heart disease, etc. Although clubbed fingers are mostly asymptomatic, it often reflects the presence of dreadful internal illness like lung cancer, idiopathic pulmonary fibrosis, or underlying suppurative conditions. Digital clubbing may occur as isolated finding or is often part of the syndrome of hypertrophic osteoarthropathy (HOA) which is characterized by periostosis of the long bones and occasional painful joint enlargement. It was initially known as hypertrophic pulmonary osteoarthropathy (HPOA) based on the fact that majority of cases of HOA are due to malignant thoracic tumors. The term “pulmonary” was later abandoned as it was realized that the skeletal syndrome may occur in several non-pulmonary diseases and even may occur without any underlying illness. In the later condition, it is known as primary hypertrophic osteoarthropathy (PHO) or pachydermoperiostotis.[4]
PHO or pachydermoperiostosis is a rare hereditary disorder inherited in an autosomal dominant pattern or recessive pattern. It is characterized by digital clubbing, subperiosteal new bone formation, mainly from the ends of long bones, acro-osteolysis, hypertrophy of soft tissues and glands, particularyly in the face and scalp resulting in wrinkling of skin on the face and scalp.[5,6] Skin involvement differentiates it from the secondary form.[7] Secondary form is the more common one and is associated with variety of clinical conditions. A majority of cases of secondary HOA (>90%) are associated with malignancies or chronic suppurative pulmonary diseases and can even predate the diagnosis of an underlying disease.[8,9] Pulmonary malignancies including primary, metastatic lung cancer, and intrathoracic lymphoma account for 80% cases of secondary HOA.[10] Adenocarcinoma lung is the most frequent histopathological type of lung cancer associated with HOA, whereas small cell carcinoma is the least frequently occurred lung cancer.[11] HOA is present in 10-20% cases of digital clubbing.[12]
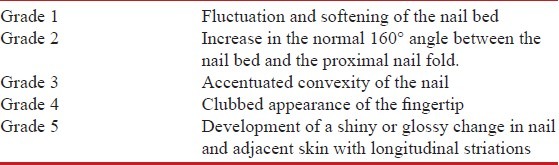
DIFFERENT STAGES OF CLUBBING
Clubbing has been described to occur in different stage [Table 1].[13] In the initial stage, there occurs peri-ungual erythema and softening of nail bed. On palpation, it gives a spongy sensation. In the next stage, increase in the normal 160° angle between the nail bed and the proximal nail fold occurs, resulting in convexity as the nails grow. Eventually, the depth of distal phalanx increases and distal inter-phalangeal joint may become hyper-extensible. At this stage, finger develops a clubbed appearance. Finally, the nail and peri-ungual skin appear shiny and nail develops longitudinal ridging. This whole process usually takes years but in certain conditions, clubbing may develop sub-acutely (e.g. lung abscess, empyema thorasis). Although different grading of clubbing has been described, it has no clinical significance.
Table 1.
Grading of clubbing
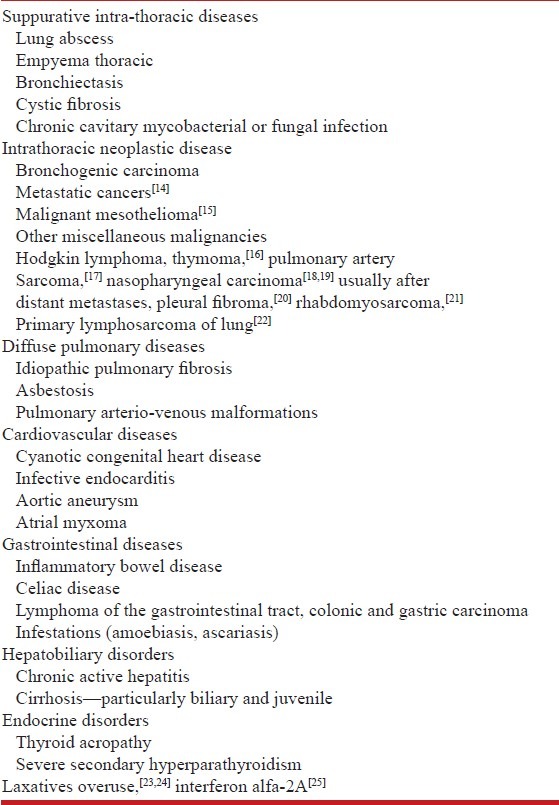
Clubbing may be associated with various clinical conditions [Table 2]; however, lung diseases are most commonly associated with clubbing and neoplastic lung disease is the most common pulmonary cause of clubbing. Other lung diseases that can be associated with clubbing are bronchiectasis, lung abscess, interstitial lung disease, fibrous pleural tumors, mesothelioma, etc. Other diseases are cardiac conditions (namely, cyanotic heart diseases, infective endocarditis) and gastrointestinal diseases (namely, inflammatory bowel disease, coeliac disease, cirrhosis mostly primary biliary cirrhosis). There are also cases of congenital and idiopathic clubbing, and pseudo-clubbing.
Table 2.
Showing different conditions associated with clubbing
LUNG CANCER
In adults, malignant neoplasm of the lung is the predominant pulmonary cause of clubbing, contributing to nearly 90% of cases.[26] Among the different types of thoracic malignancy, lung cancer is responsible for 80% cases of clubbing, whereas pleural tumors and other intrathoracic and mediastinal growth contribute to 10% and 5% cases, respectively.[27] On the other hand, the prevalence of clubbing in lung cancer patient ranges from 5% to 15%.[26] Clubbing in lung cancer is a paraneoplastic manifestation and is also the most common paraneoplastic syndrome in lung cancer patients.[28] A majority of clubbing in lung cancer patient involves non-small cell variety.[26] Clubbing is relatively uncommon in small cell lung carcinoma because of its aggressive course and poor prognosis, thereby leading to early death. However, contrary to this classical view, Findik and Baughman et al.'s[29] series reported similar incidence of clubbing in both SCLC and NSCLC patients. Most studies did notice a male predominance of clubbing in lung cancer patients[26] except Sridhar et al.[30] who found a female predominance of clubbing in lung cancer patients. The megakaryocyte/platelet hypothesis appears quite reliable in explaining digital clubbing in lung cancer patients. Hirakata et al.[31] also reported increased serum transforming growth factor (TGF ß1) level in primary lung cancer patients with clubbing. Therefore, large megakaryocyte or platelet clumps may release TGF ß1 level locally which may increase local accumulation of extra cellular matrix protein. There are few case reports of digital clubbing occurrence in malignant mesothelioma, pleural fibroma, and metastatic osteogenic sarcoma.[32] McGavin et al.[33] noticed finger clubbing based on abnormal fluctuation of nail bed in 30% of the mesothelioma and 14% of benign asbestos pleural disease, respectively. The incidence of clubbing in malignant pleural mesothelioma is high enough to be included in the list of digital clubbing. Solitary fibrous tumor of pleura is less common than malignant mesothelioma. Moreover, they are mesenchymal in origin unlike mesothelial origin of mesothelioma. They often develop characteristic paraneoplastic syndrome of clubbing, HOA, and hypoglycemia, not typically seen with mesothelioma.[34] Inflammatory pseudo-tumor is a rare benign lung tumor of uncertain etiology, occurring more commonly in younger patients. Vandemergel et al.[35] reported the first association of inflammatory pseudo tumor with digital clubbing in an adult patient. Pulmonary metastases from extrathoracic neoplasms are rare cause of clubbing and HPOA. Most of the reported cases have been sarcomas, mainly of bone and soft tissues; among the rest are tumors of the nasopharynx and uterus and cervix and renal cell carcinoma.[36,37] Renal cell carcinoma has been usually associated clubbing in the presence of pulmonary metastases.[36,38] However, in the Vandemergel et al. series renal cell carcinoma patient with digital clubbing did not have evidence of lung metastasis.[35] Hodgkin's lymphoma is rarely associated with digital clubbing. Characteristically, clubbing is mainly seen in the presence of intrathoracic involvement and in children and adolescents. In patients of Hodgkin's lymphoma, the presence of clubbing requires searching for an underlying intrathoracic neoplasm.[39]
INTERSTITIAL LUNG DISEASE
Interstitial lung disease is frequently associated with digital clubbing.[40] Among different ILDs, digital clubbing is most commonly noted in idiopathic pulmonary fibrosis (IPF)[40] which is also the most common pulmonary cause of digital clubbing in developed country. Kanematsu et al. reported clubbing in 67% of the 55 patients of idiopathic pulmonary fibrosis.[41] Surprisingly, the author reported correlation between clubbing of the digits with extent of smooth muscle proliferation in pulmonary fibrotic changes on histopathological examination; however, the significance of this finding is not known. It is more commonly noted among male patients. Ryu et al. from Mayo clinic reported digital clubbing in 45% of IPF patients younger than 50 years.[42] Rarely, patients may develop features of HOA associated with severe pain in the distal extremities.[43] Clubbing rarely occurs in sarcoidosis and is usually seen in advanced fibrotic stage. Asbestosis is another ILD where clubbing is commonly seen. Coutts et al. noted finger clubbing in 43% of asbestosis patients and is usually seen in patients with more severe form of disease.[44]
GASTRO-INTESTINAL DISORDER
Digital clubbing, complicating inflammatory bowel disease has been frequently reported in the Western country. However, its association with secondary HOA has been very rarely found.[45] Digital clubbing is more commonly noted in Crohn's disease than in ulcerative colitis . Kittis et al. reported digital clubbing incidence of 38% and 15% in patients with Crohn's disease and ulcerative colitis, respectively .[46] Megakaryocytes or platelet or their derivatives may play a role in the pathogenesis of clubbing in inflammatory bowel disease. Collins et al.[47] have detected increased circulating platelets aggregates as well as an increase number of platelets in patients with Crohn's disease. Normally, P-selectin (a surface marker of platelet activation) expression is greater in finger tip capillary blood than in venous blood; this difference is further increased in Crohn's disease. So platelets are more susceptible to activation in the micro-circulation in Crohn's disease which could result in increased release of PDGF.[48] Finger clubbing is more significantly associated with active disease than inactive disease in patients with IBD. Patients with Crohn's disease have shown regression of clubbing after resection of macroscopic disease. There is also a possibility that mucosal inflammatory changes and fibrosis in the gut may act as focal stimuli for vagus nerve and possibly other autonomic nerve, acting as the afferent arc of a finger clubbing reflex.[49] Behcets disease[50] and hepato-pulmonary syndrome[51] are rare causes of clubbing. Vasculitis of digital vasculature by impairing endothelial functions promote platelet aggregation and may cause clubbing. Digital clubbing is mainly reported in biliary cirrhosis[52] but has also been described in other liver diseases,[53] such as portal cirrhosis,[54] secondary hepatic amyloidosis, alcoholic cirrhosis, and biliary atresia.[55]
Clubbing in endocrine disease
Clubbing has been reported in few endocrine conditions: Thyroid acropachy, hyperparathyroidism.[56] Thyroid acropachy is an extra-thyroidal manifestation of autoimmune thyroid disease and is frequently associated with dermopathy and ophthalmopathy. It is characterized by clubbing and swelling of the fingers and toes, with or without periosteal reaction of the distal bones.[57] Thyroid function tests revealed hyperthyroidism in 88% but it can also occur with euthyroid and hypothyroid state.[57,58]
The typical features of clubbing and periostitis seen in thyroid acropachy are often different from other causes of clubbing:
In acropachy, periosteal reaction can be asymmetric but in pulmonary osteoarthropathy, periosteal reaction usually is symmetric.[57]
In thyroid acropachy, radiographs show a characteristic subperiosteal spiculated, frothy, or lacy appearance, whereas in classic pulmonary osteoarthropathy, there is laminal periosteal proliferation.[59,60]
Autoimmune phenomena, increased glycosaminoglycan and fibroblast proliferation explain the pathological changes of clubbing in thyroid acropachy[61,62]
Thyroid acropachy less commonly involve proximal long bones and periarticular areas, which occurs in rheumatoid arthritis and metabolic disorders including hyperthyroidism[57]
HUMAN IMMUNODEFICIENCY VIRUS AND CLUBBING
Human immunodeficiency virus (HIV) and clubbing is an interesting topic but studies are weak. Only few case reports are there linking HIV infection and clubbing. However, direct linking of HIV to clubbing is still a matter of controversy. In an observational study, Dever et al.[63] reported 36% incidence of clubbing in HIV infected outpatients. Patients with digital clubbing are slightly younger in age and had history of longer duration of HIV infection. Clubbing in HIV-infected patients has generally been attributed to concomitant pulmonary infection. Ddungu et al.[64] assert that clubbing is more often present in patients with prior tuberculosis (TB).
MECHANISMS OF CLUBBING IN HIV PATIENTS
Underlying pulmonary disease including lymphocytic interstitial pneumonia
HIV infection per se
It may be a part of HIV-associated rheumatologic manifestation like HPOA
CARDIOVASCULAR DISEASE
Infective endocarditis usually causes a milder form of clubbing, whereas in congenital cyanotic heart disease, gross, drumstick appearance may be seen.[65] Although digital clubbing is common in patients with cyanotic congenital heart disease (CCHD), HOA is rarely reported in this condition. However, one Mexican study reported a higher frequency of HOA of 31% in congenital cyanotic heart disease.[66]
PULMONARY TUBERCULOSIS
Although TB has not been reported as a cause of clubbing in major textbooks of medicine, there are several case reports of its occurrence in TB patients. Studies from endemic areas of TB have shown a 30% frequency of clubbing amongst smear-positive TB patients.[67,68] One Indian study also reported a very high frequency of digital clubbing (82%).[69] MacFarlane et al.[70] in an earlier study in Nigeria reported associations of clubbing with severity of disease, cavitary TB, and hypoalbuminemia, indicative of chronic disease. Henry et al. could not find significant association between clubbing and duration of illness, frequency of cavitation, early versus late HIV disease, and hypoalbuminemia, but it was more common among patients with a lower Karnofsky performance scale score or with prior TB.[68]
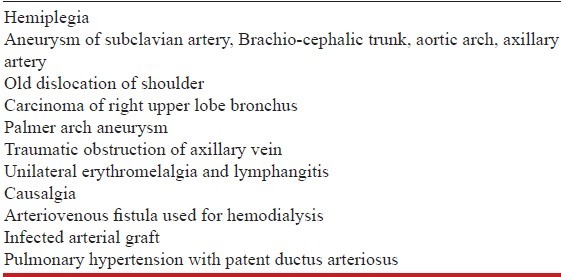
UNILATERAL CLUBBING
Clubbing is generally bilateral, but in some conditions it may occur unilaterally [Table 3]. Unilateral clubbing is usually associated with local vascular lesions of the arm, axilla, and thoracic outlet and with hemiplegia.[71] Vascular aneurysm, particularly of the subclavian artery, is commonly reported in the literature in causing unilateral clubbing although aorta and innominate artery aneurysm have also been reported.[72] Several unilateral phenomena occur in the hemiplegic arm, including unilateral clubbing, sparing of arthritis, unilateral eczema, minimal erythema dose for UV light, and feeling of coldness in the hemiplegic arm.[71] In a group of 87 hemiplegics patients, Alvarez et al. reported a 14% incidence of unilateral clubbing.[73] However, Siragusa et al.[74] reported a lower incidence of 2% only. It may be explained by the different methods use to elicit clubbing. Incidence of clubbing increases with the duration of stroke and Siragusa noticed development of clubbing 60-120 months after the stroke.[74] The pathogenesis of clubbing in hemiplegia is not clear. Hypertrophy and edema of the soft tissues may be responsible for the obliteration of the nail angle in hemiplegic patients.[75] Autonomic nervous system may also play a role in this nail pathology.[7] In vascular graft sepsis, clubbing involves digits distal to the graft. Several theories have been put forward to explain it.[75]
Table 3.
A vasoactive compound, endotoxin, or some other substance produced by bacteria adherent or adjacent to the graft
Chronic infection of the arterial graft may also lead to formation of platelet clumps within vessels with secondary release of PDGF into the circulation leading to clubbing formation
Neurogenic theory
Clubbing may also involve single digit only in case of digital mucoid cyst, osteoid osteoma, myxochondroma, and enchondromas. Occasionally, clubbing may occur selectively in lower limbs, sparing the upper limbs. This is known as differential clubbing. Differential clubbing may occur in patient with patent ductus arteriosus associated with pulmonary artery hypertension and right to left shunt. In this condition, deoxygenated blood from the right ventricle enters aorta distal to the origin of left subclavian artery, thereby sparing the upper extremities. It may also occur in infected abdominal aortic aneurysm.
Chronic obstructive pulmonary disease (COPD) per se does not cause clubbing, but if clubbing is present in COPD, underlying lung cancer and bronchiectasis must be ruled out.
ASSESSMENT OF CLUBBING
Clubbing can be assessed by physical examination. However, it is subjective and often unreliable, particularly in mild cases.[79] There are several objective criteria developed in the past century to quantify clubbing. It was objectively measured by material brass templates[80] with arcs of various sizes, plethysmography,[81] digital casts,[82] and shadowgraph[83] technique. All these methods are relatively crude and cannot be accepted as standard as they do not provide easy quantification. Recently, digital cameras and computerized analysis[1] have been used to objectively assess clubbing. It is an easy, rapid and relatively inexpensive method to study finger clubbing.
Different signs of clubbing are the followings
Profile sign or Lovibond's angle
It was proposed by Lovibond[84] in the year 1939 and is also popularly known as Lovibond's angle. It is defined by the angle made by nail as it exists from the proximal nail fold. In normal subjects, profile angle is usually less than 180°. Profile angle of greater than 180° can be used to differentiate true clubbing from simple nail curving and paronychia, which often produce an angle closer to 160°.
Hyponychial angle
It is constructed by drawing a line from distal digital crease to the cuticle and another line from the cuticle to hyponychium which is the thickened stratum corneum of epidermis lying under the free edge of the nail.[85] Normal hyponychial angle is less than 192°.[86] Hyponychial angle is a preferred objective criterion for clubbing because it is independent of age, sex, height, and weight of the patient[69] and it differentiates normal and clubbed fingers without any overlap. It also correlates strikingly with the subjective assessment of clubbing.[85] Figure 1 shows the profile angle and hyponychial angle in normal and clubbed fingers.
Figure 1.
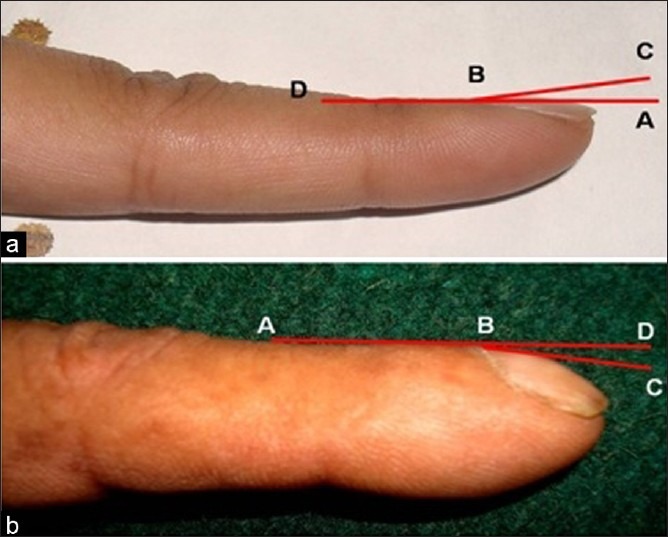
(a-b) Depicting profile and hyponychial angle in normal and clubbed fingers. DBC and DBA are the normal profile and hyponychial angle and ABD and ABC are the increased profile and hyponychial angle in clubbed fingers
Phalangeal depth ratio
It is defined by the ratio of digit's depth measured at the junction between skin and nail (nail bed) and at the distal interphalangeal joint. Normally, the depth at distal interphalangeal joint is more than the depth at nail bed. In clubbing fingers, connective tissue deposition expands the pulp in the terminal phalanx and the ratio becomes reversed. This ratio is also independent of age, sex, and ethnicity of population.[87,88] A Phalangeal depth ratio of over 1 is indicative of clubbing.[86] It can be measured by a caliper or a digital photograph.[86]
While performing this measurement with calipers, it should be ensured that the calipers must not compress the tissues during measurement. It is usually measured at the index finger. The phalangeal depth ratio is shown in Figure 2.
Figure 2.
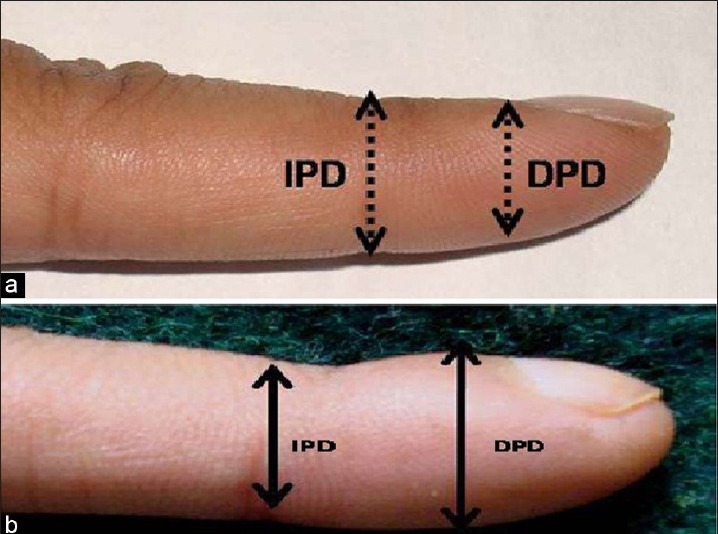
Showing phalangeal depth ratio In normal finger (a), interphalangeal depth (IPD) is more than distal phalangeal depth (DPD) which is altered in clubbed digits (b)
Digital index
It is the sum of phalangeal depth ratio for all 10 fingers. A digital index of 10.2 or higher is indicative of clubbing. Although a phalangeal depth ratio of 1.0 or greater in any finger is suggestive of clubbing, digital index is more specific for clubbing.
Schamroth sign
This sign is named after Dr. Schamroth, a South African physician who not only had described this sign but was himself the patient. This sign is elicited by placing the dorsal surfaces of terminal phalanges of corresponding right and left fingers together. Normal fingers create a diamond-shaped window when the dorsal surfaces of terminal phalanges of similar fingers are opposed to each other [Figure 3]. In patients with clubbing, this diamond-shaped window gets obliterated. Precision and accuracy of this sign is not known.
Figure 3.
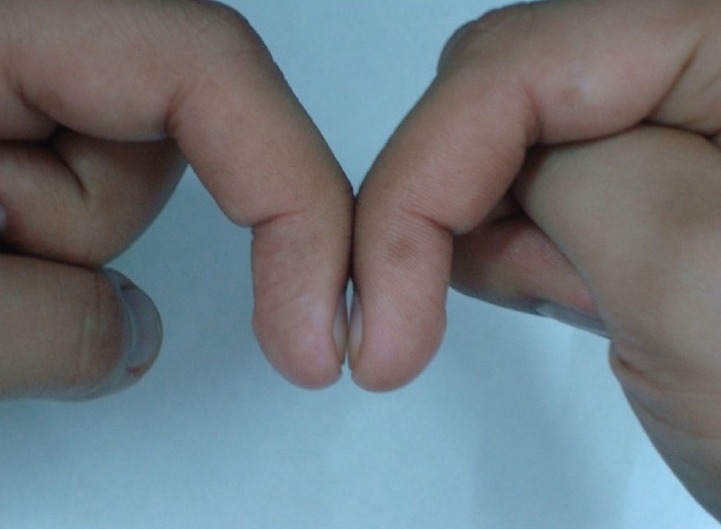
Showing normal diamond shaped space
PATHOGENESIS OF CLUBBING
Various hypotheses have been proposed over the years to explain the pathophysiology of digital clubbing. In patients with lung carcinoma and clubbing, Gosney et al.[89] found significantly higher plasma growth hormone levels than patients without clubbing. However, a subsequent study found no such relationship in patients with lung cancer.[90] Brouwers et al.[91] hypothesized that clubbed digits resemble the human embryonic fingers and toes, and may represent the return of the embryonic claw that we have lost during evolution. Pathologic condition by altering hormone levels in the blood, activates the “dormant” genes and resulting in the development of clubbing. They suggest that these hormones may actually be cytokines, but its exact nature is not known. The most promising hypothesis in digital clubbing is that proposed by Dickinson and Martin in 1987.[92] According to them, megakaryocyte or platelet clusters, lodged in the peripheral vasculature of the digits, release platelet-derived growth factor (PDGF) and lead to the increased vascularity, permeability, and connective tissue changes that are the hallmark of clubbing. Although Dickinson and Martin considered PDGF as the most likely candidate, Fox et al.[93] also found a role of vascular endothelial growth factor (VEGF) in inducing the pathological changes in digital clubbing. They noted dilated vessels, often containing platelets clusters within it in clubbed fingers. They also noted significant increase in VEGF, PDGF, and hypoxia inducible factor expression in clubbed digits compared with controls.
Therefore, release of VEGF and PDGF occurred after platelet impaction and is enhanced by hypoxia. VEGF along with PDGF induces the pathological changes of digital clubbing. Another support for the role of VEGF is beneficial effects of octreotide, a potent VEGF inhibitor in HOA.[94] However, there are several points against this theory of clubbing. Other features of platelets activation e.g., B-thromboglobulin are normal in patients with clubbing.[95] Secondly, clubbing has not been reported in association with arterial thrombosis, where platelets activation and clumping occur. An experimental study in rats has shown no feature of clubbing on intermittent intravenous infusion of PDGF.[96]
Congenital clubbing
Congenital nail clubbing is usually symmetrical and bilateral, but different fingers and toes may be involved to varying degrees. Some fingers or toes may be spared, but the thumbs are almost always involved. Tariq et al.[97] in a genome-wide analysis of 11 affected individuals having congenital nail clubbing in a Pakistani consanguineous family reported a homozygous missense mutation in the human HPGD gene located at 4q33-q34. HPGD gene encodes the NADP-dependent 15-hydroxyprostaglandin dehydrogenase (15-PGDH) enzyme. 15-PGDH is involved in the catabolism of prostaglandin E2 (PGE2). Uppal et al.[98] also found mutation in 15-PGDH, the main enzyme of prostaglandin degradation. Chronically elevated prostaglandin E2 levels may be responsible for various clinical manifestations of clubbing. PGE2 stimulates the activity of both osteoblasts and osteoclasts, thereby causing both bone deposition (periostosis) and resorption (acro-osteolysis),[99] the typical skeletal feature of PHO. 15-PGDH is found in most of the mammalian tissues and the highest activities are located within lung, kidney, and placenta.[100] Failure to metabolize PGE2 by 15-PGDH in the lungs and subsequent incomplete clearance by the diseased lung may underlie clubbing secondary to pulmonary disease (or cyanotic heart disease with right-to-left shunt).[98] Raised PGE2 may explain the prolonged local vasodilatation consistent with finger clubbing.[101] Patients with unexplained clubbing, genetic testing for HPGD mutation, and measurements of PGE2 may become an important diagnostic tool.[102] One Japanese study has also suggested a possible role of auto-immune factors in the causation of clubbing.[103] Figure 4 shows the pathogenesis of clubbing.
Figure 4.
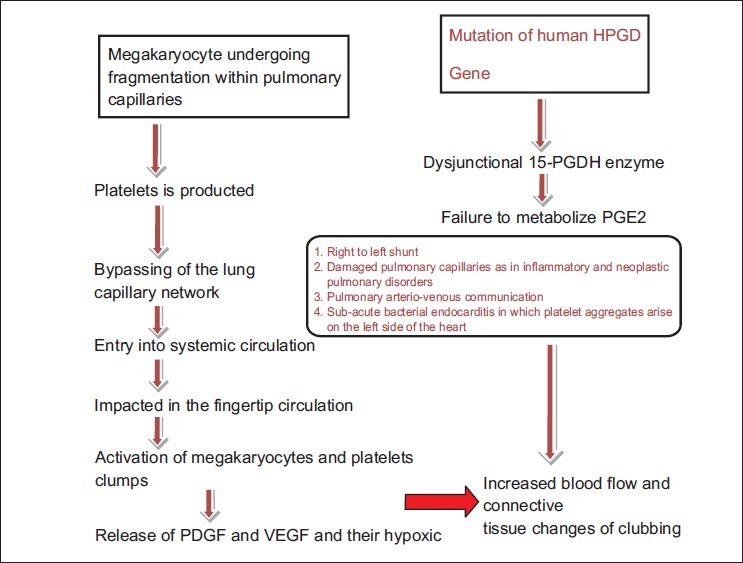
Showing the pathogenesis of digital clubbing
Pathology of clubbed fingers
Increased soft tissue in the fingertips of clubbed fingers
Local vascular neogenesis
Increase width of nail-fold capillary[104]
Clubbed fingers can be differentiated from non-clubbed fingers by measurement of nail bed thickness, using plain radiograph. Moreira et al.[105] reported significantly higher mean nail bed thickness of 3.88 ± 0.55 mm in patients with clubbing compared to 2.38 ± 0.27 mm in the normal subjects (P<0.001).
PSEUDOCLUBBING
Pseudoclubbing (PC) is an atypical presentation of clubbing, characterized clinically by asymmetrical involvement of the fingers, and radiographically by resorption of the terminal tufts (acro-osteolysis). It has been described in chronic renal failure,[106] subungal hemangioma,[107] acrometastases,[108] systemic sclerosis,[109] etc. Exact mechanism is not known, but it could be the result of soft-tissue collapse due to distal phalangeal osteolysis.
Mittermayer et al.[110] suggested the following features that may help in differentiating PC from clubbing. In PC, profile sign is usually normal and there is usually asymmetrical nails involvement. Acro-osteolysis is classically present instead of soft tissue swelling of nail bed in clubbing. Acro-osteolysis may also be present in HOA, but unlike HOA, there are no signs of periostitis or synovial effusion.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Hanssen-flaschen J, Nordberg J. Clubbing and hypertrophic osteoarthropathy. Clin Chest Med. 1987;8:287–98. [PubMed] [Google Scholar]
- 2.Hippocrates . Hippocrates. 1st ed. Vol. 2. London: Loeb Classical Library, No. 148, William Heinemann ltd; 1923. Prognostic; pp. 7–55. Available from: http://www.archive.org/details/hippocrates02hippuoft . [Google Scholar]
- 3.Martinez-Lavin M. Exploring the cause of the most ancient clinical sign of medicine: Finger clubbing. Semin Arthritis Rheum. 2007;36:380–5. doi: 10.1016/j.semarthrit.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 4.Touraine G, Solente A, Golé L. Pachidermoperiostitis. Presse Med. 1935;43:1820. 1935. [Google Scholar]
- 5.Jajic I, Jajic Z, Grazio S. Minor but important symptoms and signs in primary hypertrophic osteoarthropathy. Clin Exp Rheumatol. 2001;19:357–8. [PubMed] [Google Scholar]
- 6.Loredo R, Pathria MN, Salonen D, Resnick D. Magnetic resonance imaging in pachydermoperiostosis. Clin Imaging. 1996;20:212–8. doi: 10.1016/0899-7071(95)00006-2. [DOI] [PubMed] [Google Scholar]
- 7.Vandemergel X, Blocklet D, Decaux G. Possible association between deep infection and hypertrophic osteoarthropathy.Report of three cases and review of literature. Acta Clin Belg. 2003;58:290–5. doi: 10.1179/acb.2003.58.5.004. [DOI] [PubMed] [Google Scholar]
- 8.Jajic Z, Jajic I, Nemcic T. Primary hypertrophic osteoarthropathy: Clinical, radiologic, and scintigraphic characteristics. Arch Med Res. 2001;32:136–42. doi: 10.1016/s0188-4409(01)00251-x. [DOI] [PubMed] [Google Scholar]
- 9.Armstrong DJ, McCausland EM, Wright GD. Hypertrophic pulmonary osteoarthropathy (HPOA) (Pierre Marie-Bamberger syndrome): Two cases presenting as acute inflammatory arthritis. Description and review of the literature. Rheumatol Int. 2007;27:399–402. doi: 10.1007/s00296-006-0224-2. [DOI] [PubMed] [Google Scholar]
- 10.Yao Q, Altman RD, Brahn E. Periostitis and hypertrophic pulmonary osteoarthropathy: Report of 2 cases and review of the literature. Semin Arthritis Rheum. 2009;38:458–66. doi: 10.1016/j.semarthrit.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Michalakis K, Moutzouris DA. Hypertrophic osteoarthropathy and digital clubbing in lung adenocarcinoma. Foot Ankle. 2009;2:1–3. [Google Scholar]
- 12.Benedek TG. Paraneoplastic digital clubbing and hypertrophic osteoarthropathy. Clin Dermatol. 1993;11:53–9. doi: 10.1016/0738-081x(93)90082-n. [DOI] [PubMed] [Google Scholar]
- 13.Altman RD, Tenenbaum J. Hypertrophic osteoarthropathy. In: Kelly WN, Harris ED, Ruddy S, editors. Textbook of Rheumatology. 5th ed. Philadelphia: WB Saunders Company; 1997. pp. 1514–20. [Google Scholar]
- 14.Aufses AH, Aufses BH. Hypertrophic osteoarthropathy in association with pulmonary metastases from extrathoracic malignancies. Dis Chest. 1960;38:399–40. doi: 10.1378/chest.38.4.399. [DOI] [PubMed] [Google Scholar]
- 15.Mcgavin C., Hughes P. Short Report Finger clubbing in malignant Mesothelioma and benign asbestos pleural disease. Respiratory Medicine. 1998;92:691–2. doi: 10.1016/s0954-6111(98)90519-4. [DOI] [PubMed] [Google Scholar]
- 16.Kim SJ, Seo JH, Choi CW, Lee ES, Seo BK, Kim JS. Unusual presentation of thymic carcinoma: Hypertrophic osteoarthropathy. Korean J Intern Med. 2003;18:125–8. doi: 10.3904/kjim.2003.18.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loredo JS, Fedullo PF, Piovella F, Moser KM. Digital clubbing associated with pulmonary artery sarcoma. Chest. 1996;109:1651–3. doi: 10.1378/chest.109.6.1651. [DOI] [PubMed] [Google Scholar]
- 18.Ali N, Abbasi AN, Karsan F, Hashmi R, Badar QA, Sheikh AJ. A case of finger clubbing associated with nasopharyngeal carcinoma in a young girl, and review of pathophysiology. J Pak Med Assoc. 2009;59:253–4. [PubMed] [Google Scholar]
- 19.Biswal BM, Kareem A, Ahmed NM. Hypertrophic osteoarthropathy: An unusual manifestation in nasopharyngeal cancer. Australas Radiol. 2001;45:71–3. doi: 10.1046/j.1440-1673.2001.00883.x. [DOI] [PubMed] [Google Scholar]
- 20.Urschel JD, Anderson TM, Whooley BP. Finger clubbing and a lung mass. Chest. 1999;115:1735–7. doi: 10.1378/chest.115.6.1735. [DOI] [PubMed] [Google Scholar]
- 21.Garganese MC, De Sio L, Serra A, De Ioris MA, Bock C, Donfrancesco A, et al. Rhabdomyosarcoma associated hypertrophic osteoarthropathy in a child: Detection by bone scintigraphy. Clin Nucl Med. 2009;34:155–7. doi: 10.1097/RLU.0b013e3181966dfb. [DOI] [PubMed] [Google Scholar]
- 22.Benfield GF. Primary lymphosarcoma of lung associated with hypertrophic pulmonary osteoarthropathy. Thorax. 1979;34:279–80. doi: 10.1136/thx.34.2.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Silk DB, Gibson JA, Murray CR. Reversible finger clubbing in a case of purgative abuse. Gastroenterology. 1975;68:790. [PubMed] [Google Scholar]
- 24.Malmquist J, Ericsson B, Hultén-Nosslin MB, Jeppsson JO, Ljungberg O. Finger clubbing and aspartylglucosamine excretion in a laxative-abusing patient. Postgrad Med J. 1980;56:862–4. doi: 10.1136/pgmj.56.662.862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alam MT, Sheikh SS, Aziz S, Masroor M. An unusual side effect of interferon alfa 2A: Digital clubbing. J Ayub Med Coll Abbottabad. 2008;20:165–6. [PubMed] [Google Scholar]
- 26.Erkan ML, Findik S, Kandemir B, Atici AG, Talisöz H. The prevalence of clubbing in different types of lung cancer. Ann Saudi Med. 2002;22:295–6. doi: 10.5144/0256-4947.2002.295. [DOI] [PubMed] [Google Scholar]
- 27.Coury L. Hippocratic fingers and hypertrophic osteoarthropathy study of 350 cases. Br J dis chest. 1960;54:202–9. doi: 10.1016/s0007-0971(60)80001-0. [DOI] [PubMed] [Google Scholar]
- 28.Macedo AG, Fusari VC, Almeida JR. Digital clubbing as the initial diagnosis of bronchogenic cancer. An bras Dermatol. 2004;79:457–62. [Google Scholar]
- 29.Baughman RP, Gunther KL, Buchsbaum JA, Lower EE. Prevalence of digital clubbing in bronchogenic carcinoma by a new digital index. Clin Exp Rheumatol. 1998;16:21–6. [PubMed] [Google Scholar]
- 30.Sridhar Kasi S, Lobo Christopher F, Altman Roy D. Digital clubbing and lung cancer. Chest. 1998;114:1535–7. doi: 10.1378/chest.114.6.1535. [DOI] [PubMed] [Google Scholar]
- 31.Hirakata Y, Kitamura S. Elevated serum transforming growth factor ß1 level in primary lung cancer patients with finger clubbing. Eur J Clin Invest. 1996;26:820–3. doi: 10.1046/j.1365-2362.1996.2260560.x. [DOI] [PubMed] [Google Scholar]
- 32.Myers KA, Farquhar DR. The rational clinical examination. Does this patient have clubbing? JAMA. 2001;286:341–7. doi: 10.1001/jama.286.3.341. [DOI] [PubMed] [Google Scholar]
- 33.McGavin C, Hughes P. Short report finger clubbing in malignant mesothelioma and benign asbestos pleural disease. Respir Med. 1998;92:691–2. doi: 10.1016/s0954-6111(98)90519-4. [DOI] [PubMed] [Google Scholar]
- 34.Briselli M, Mark EJ, Dickersin GR. Solitary fibrous tumors of the pleura: Eight new cases and review of 360 cases in the literature. Cancer. 1981;47:2678–89. doi: 10.1002/1097-0142(19810601)47:11<2678::aid-cncr2820471126>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 35.Vandemergel X, Renneboog B. Prevalence, etiology and significance of clubbing in a Department of General Internal Medicine. Euro J Internal Med. 2008;19:325–9. doi: 10.1016/j.ejim.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 36.Firooznia H, Seliger G, Genieser NB, Barasch E. Hypertrophic Pulmonary osteoarthropathy in pulmonary metastases. Radiology. 1975;115:269–74. doi: 10.1148/115.2.269. [DOI] [PubMed] [Google Scholar]
- 37.Yacoub MH, Simon G, Ohnsorge J. Hypertrophic pulmonary osteoarthropathy in association with pulmonary metastases from extrathoracic tumours. Thorax. 1967;22:226. doi: 10.1136/thx.22.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arora VK, Bedi RS, Sharma S. Clubbing in association with pulmonary metastases from renal carcinoma-a case report. Lung India. 1989;1:50–2. [Google Scholar]
- 39.Goodyer MJ, Cronin M, Ketsitlile DG, O’Reilly SP, Moylan EJ. Hodgkin's lymphoma with digital clubbing. J Clin oncolo. 2009;27:e95–6. doi: 10.1200/JCO.2008.21.7323. [DOI] [PubMed] [Google Scholar]
- 40.Schwarz Ml, King TE, Cherniack RM. General principles and diagnostic approach to the interstitial lung diseases. In: Murray JF, Nadel JA, editors. Textbook of respiratory medicine. 2nd ed. Philadelphia: WB Saunders; 1994. pp. 1803–14. [Google Scholar]
- 41.Kanematsu T, Kitaichi M, Nishimura K, Nagai S, Izumi T. Clubbing of the fingers and smooth-muscle proliferation in fibrotic changes in the lung in patients with idiopathic pulmonary fibrosis. Chest. 1994;105:339–42. doi: 10.1378/chest.105.2.339. [DOI] [PubMed] [Google Scholar]
- 42.Nadrous HF, Myers JL, Decker PA, Ryu JH. Idiopathic pulmonary fibrosis in patients younger than 50 years. Mayo Clin Proc. 2005;80:37–40. doi: 10.1016/S0025-6196(11)62955-8. [DOI] [PubMed] [Google Scholar]
- 43.Galko B, Grossman RF, Day A, Tenenbaum J, Kirsh J, Rebuck AS. Hypertrophic pulmonary osteodystrophy in four patients with interstitial pulmonary disease. Chest. 1985;88:94–7. doi: 10.1378/chest.88.1.94. [DOI] [PubMed] [Google Scholar]
- 44.Coutts II, Gilson JC, Kerr IH, Parkes WR, Turner-warwick M. Significance of finger clubbing in asbestosis. Thorax. 1987;42:117–9. doi: 10.1136/thx.42.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Makiyama K, Ishida K, Zea-Iriarte W, Itsuno M, Yamakawa M, Mori N. Case report: Hippocratic digital and Crohn's disease. J Gastroenterol Hepatol. 1996;11:692–5. doi: 10.1111/j.1440-1746.1996.tb00316.x. [DOI] [PubMed] [Google Scholar]
- 46.Kitis G, Thompson H, Allan RN. Finger clubbing in inflammatory bowel disease: Its prevalence and pathogenesis. Br Med J. 1979;2:825–8. doi: 10.1136/bmj.2.6194.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Collins CE, Rampton DS. Inflammatory bowel disease. Gut. 1995;36:5–8. doi: 10.1136/gut.36.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tschoepe D, Schwippert B, Schumacher B, Strauss K, Jackson A, Niedrau C. Increased P-selectin (CD62) expression on platelets from capillary whole blood of patients with Crohn's disease. Gastroenterology. 1993;104:A1680. [Google Scholar]
- 49.Tosti A, Iorizzo M, Piraccini BM, Starace M. The nail in systemic diseases. Dermatol Clin. 2006;24:341–7. doi: 10.1016/j.det.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 50.Benekli M, Güllü IH. Hippocratic fingers in Behçet's disease. Postgrad Med J. 1997;73:575–6. doi: 10.1136/pgmj.73.863.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ede K, McCurdy D, Garcia-Lloret M. Hypertrophic osteoarthropathy in the hepatopulmonary syndrome. J Clin Rheumatol. 2008;14:230–3. doi: 10.1097/RHU.0b013e31817de06c. [DOI] [PubMed] [Google Scholar]
- 52.Mendlowitz M. Clubbing and hypertrophic osteoarthropathy. Medicine (Baltimore) 1942;21:269–306. [Google Scholar]
- 53.Epstein O, Dick R, Sherlock S. Prospective study of periostitis and finger clubbing in primary biliary cirrhosis and other forms of chronic liver disease. Gut. 1981;22:203–6. doi: 10.1136/gut.22.3.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Buchan DJ, Mitchell DM. Hypertrophic osteoarthropathy in portal cirrhosis. Ann Intern Med. 1967;66:130–5. doi: 10.7326/0003-4819-66-1-130. [DOI] [PubMed] [Google Scholar]
- 55.Rothberg AD, Boal DK. Hypertrophic osteoarthropathy in biliary atresia. Pediatr Radiol. 1983;13:44–6. doi: 10.1007/BF00975667. [DOI] [PubMed] [Google Scholar]
- 56.Grekas D, Avdelidou A. Digital clubbing as an unusual complication associated with severe secondary hyperparathyroidism: Report of two cases. Hemodial Int. 2007;11:193–7. doi: 10.1111/j.1542-4758.2007.00168.x. [DOI] [PubMed] [Google Scholar]
- 57.Fatourechi V, Ahmed DD, Schwartz KM. Thyroid acropachy: Report of 40 patients treated at a single institution in a 26-year period. J Clin Endocrinol Metab. 2002;87:5435–41. doi: 10.1210/jc.2002-020746. [DOI] [PubMed] [Google Scholar]
- 58.Fatourechi V, Pajouhi M, Fransway AF. Dermopathy of Graves’ disease (pretibial myxedema): Review of 150 cases. Medicine (Baltimore) 1994;73:1–7. doi: 10.1097/00005792-199401000-00001. [DOI] [PubMed] [Google Scholar]
- 59.Winkler A, Wilson D. Thyroid acropachy: Case report and literature review. Mo Med. 1985;82:756–61. [PubMed] [Google Scholar]
- 60.Kinsella RA, Jr, Back DK. Thyroid acropachy. Med Clin North Am. 1968;52:393–8. [PubMed] [Google Scholar]
- 61.Smith TJ, Bahn RS, Gorman CA, Cheavens M. Stimulation of glycosaminoglycan accumulation by interferon -gamma in cultured human retroocular fibroblasts. J Clin Endocrinol Metab. 1991;72:1169–71. doi: 10.1210/jcem-72-5-1169. [DOI] [PubMed] [Google Scholar]
- 62.Heufelder AE, Dutton CM, Sarkar G, Donovan KA, Bahn RS. Detection of TSH receptor RNA in cultured fibroblasts from patients with Graves’ ophthalmopathy and pretibial dermopathy. Thyroid. 1993;3:297–300. doi: 10.1089/thy.1993.3.297. [DOI] [PubMed] [Google Scholar]
- 63.Dever LL, Matta JS. Digital clubbing in HIV-infected patients: An observational study. AIDS Patient Care STDS. 2009;23:19–22. doi: 10.1089/apc.2008.0102. [DOI] [PubMed] [Google Scholar]
- 64.Ddungu H, Johnson JL, Smieja M, Mayanja-Kizza H. Digital clubbing in tuberculosis – relationship to HIV infection, extent of disease and hypoalbuminemia. BMC Infect Dis. 2006;6:45. doi: 10.1186/1471-2334-6-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chan LH. Cutaneous manifestations of cardiovascular diseases. Singapore Med J. 1990;31:480–5. [PubMed] [Google Scholar]
- 66.Martínez-Lavín M, Bobadilla M, Casanova J, Attié F, Martínez M. Hypertrophic osteoarthropathy in cyanotic congenital heart disease: Its prevalence and relationship to bypass of the lung. Arthritis Rheum. 1982;25:1186–93. doi: 10.1002/art.1780251007. [DOI] [PubMed] [Google Scholar]
- 67.Reeve PA, Harries AD, Nkhoma WA, Nyangulu DS, Wirima JJ. Clubbing in African patients with pulmonary tuberculosis. Thorax. 1987;42:986–7. doi: 10.1136/thx.42.12.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ddungu H, Johnson JL, Smieja M, Mayanja-Kizza H. Digital clubbing in tuberculosis – relationship to HIV infection, extent of disease and hypoalbuminemia. BMC Infectious Diseases. 2006;6:45–51. doi: 10.1186/1471-2334-6-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Khanna BK, Khare KS. Clubbing in pulmonary tuberculosis. Ind J Tub. 1986;33:11. [Google Scholar]
- 70.Macfarlane JT, Ibrahim M, Tor-Agbidye S. The importance of finger clubbing in pulmonary tuberculosis. Tubercle. 1979;60:45–8. doi: 10.1016/0041-3879(79)90055-2. [DOI] [PubMed] [Google Scholar]
- 71.Wanklyn P, Forster A, Young J, Mulley G. Prevalence and associated features of the cold hemiplegic arm. Stroke. 1995;26:1867–70. doi: 10.1161/01.str.26.10.1867. [DOI] [PubMed] [Google Scholar]
- 72.Rodgers RE. Unilateral clubbing of the fingers. With a Summary of the Literature. Br Med J. 1941;27(2):439–40. doi: 10.1136/bmj.2.4212.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Alveraz AS, McNair D, Wildman J, Hewson JW. Unilateral clubbing of the fingernails in patients with hemiplegia. Gerontol Clin. 1975;17:7–2. doi: 10.1159/000245547. [DOI] [PubMed] [Google Scholar]
- 74.Siragusa M, Schepis C, Cosentino FI, Spada RS, Toscano G, Ferri R. Nail pathology in patients with hemiplegia. Br J Dermatol. 2001;144:557–60. doi: 10.1046/j.1365-2133.2001.04083.x. [DOI] [PubMed] [Google Scholar]
- 75.Denham MJ, Hodkinson HM, Wright BM. Unilateral clubbing in hemiplegia. Gerontol Clin (Basel) 1975;17:7–12. doi: 10.1159/000245548. [DOI] [PubMed] [Google Scholar]
- 76.Kaditis AG, Nelson AM, Driscoll DJ. Takayasu's arteritis presenting with unilateral digital clubbing. J Rheumatol. 1995;22:2346–8. [PubMed] [Google Scholar]
- 77.Orient JM, Sapira JD. Sapira's art and science of bedside diagnosis. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2005. pp. 127–63. [Google Scholar]
- 78.Leb DE, Sharma JK. Clubbing secondary to an arteriovenous fistula used for hemodialysis. JAMA. 1978;240:142–3. [PubMed] [Google Scholar]
- 79.Husarik D, Vavricka SR, Mark M, Schaffner A, Walter RB. Assessment of digital clubbing in medical inpatients by digital photography and computerized analysis. Swiss Med Wkly. 2002;132:132–8. doi: 10.4414/smw.2002.09907. [DOI] [PubMed] [Google Scholar]
- 80.Stavem P. Instrument for estimation of clubbing. Lancet. 1959;2:7–8. doi: 10.1016/s0140-6736(59)92109-9. [DOI] [PubMed] [Google Scholar]
- 81.Cudowicz P, Wraith DG. An evaluation of the clinical significance of clubbing in common lung disorders. Br J Tuberc Dis Chest. 1957;51:14–31. doi: 10.1016/s0366-0869(57)80051-3. [DOI] [PubMed] [Google Scholar]
- 82.Mellins RB, Fishman AP. Digital casts for the study of clubbing of the fingers. Circulation. 1996;33:143–5. doi: 10.1161/01.cir.33.1.143. [DOI] [PubMed] [Google Scholar]
- 83.Bentley D, Moore A, Shwachman H. Finger clubbing: A quantitative survey by analysis of the shadowgraph. Lancet. 1976;2:164–7. doi: 10.1016/s0140-6736(76)92343-6. [DOI] [PubMed] [Google Scholar]
- 84.Lovibond JL. Diagnosis of clubbed fingers. Lancet. 1938;1:363–4. [Google Scholar]
- 85.Regan GM, Tagg B, Thomson ML. Subjective assessment and objective measurement of finger clubbing. Lancet. 1967;1:530–2. doi: 10.1016/s0140-6736(67)92111-3. [DOI] [PubMed] [Google Scholar]
- 86.Myers KA, Farquhar DR. The rational clinical examination. Does this patient have clubbing? JAMA. 2001;286:341–7. doi: 10.1001/jama.286.3.341. [DOI] [PubMed] [Google Scholar]
- 87.Mellins RB, Fishman AP. Digital casts for the study of clubbing of the fingers. Circulation. 1966;33:143–5. doi: 10.1161/01.cir.33.1.143. [DOI] [PubMed] [Google Scholar]
- 88.Sly RM, Ghazanshahi S, Buranakul B, Puapan P, Gupta S, Warren R, et al. Objective assessment for digital clubbing in Caucasian, Negro, and oriental subjects. Chest. 1973;64:687–9. doi: 10.1378/chest.64.6.687. [DOI] [PubMed] [Google Scholar]
- 89.Gosney MA, Gosney JR, Lye M. Carcinoma of the bronchus. Thorax. 1990;45:545–7. doi: 10.1136/thx.45.7.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yorgancioğlu A, Akin M, Demtray M, Derelt S. The relationship between digital clubbing and serum growth hormone level in patients with lung cancer. Monaldi Arch Chest Dis. 1996;51:185–7. [PubMed] [Google Scholar]
- 91.Brouwers AA, Vermeij-Keers C, van Zoelen EJ, Gooren LJ. Clubbed fingers: The claws we lost? Med Hypotheses. 2004;62:321–4. doi: 10.1016/S0306-9877(03)00300-1. [DOI] [PubMed] [Google Scholar]
- 92.Dickinson CJ, Martin JF. Megakaryocytes and platelet clumps as the cause of finger clubbing. Lancet. 1987;2:1434–5. doi: 10.1016/s0140-6736(87)91132-9. [DOI] [PubMed] [Google Scholar]
- 93.Atkinson S, Fox SB. Vascular endothelial growth factor (VEGF)-A and platelet-derived growth factor (PDGF) play a central role in the pathogenesis of digital clubbing. J Pathol. 2004;203:721–8. doi: 10.1002/path.1565. [DOI] [PubMed] [Google Scholar]
- 94.Angel-Moreno Maroto A, Martínez-Quintana E, Suárez-Castellano L, Pérez-Arellano JL. Painful hypertrophic osteoarthropathy successfully treated with octreotide. The pathogenetic role of vascular endothelial growth factor (VEGF) Rheumatology (Oxford) 2005;44:1326–7. doi: 10.1093/rheumatology/keh720. [DOI] [PubMed] [Google Scholar]
- 95.Silveri F, De Angelis R, Argentati F, Brecciarolli D, Muti S, Cervini C. Hypertrophic osteoarthropathy: Endotheliumand platelet function. Clin Rheumatol. 1996;15:435–9. doi: 10.1007/BF02229639. [DOI] [PubMed] [Google Scholar]
- 96.Mitlak BH, Finkelman RD, Hill EL, Li J, Martin B, Smith T, et al. The effect of systemically administered PDGF-BB on the rodent skeleton. J Bone Miner Res. 1996;11:238–4. doi: 10.1002/jbmr.5650110213. [DOI] [PubMed] [Google Scholar]
- 97.Tariq M, Azeem Z, Ali G, Chishti MS, Ahmad W. Mutation in the HPGD gene encoding NAD+ dependent 15 hydroxyprostaglandin dehydrogenase underlies isolated congenital nail clubbing (ICNC) J Med Genet. 2009;46:14–20. doi: 10.1136/jmg.2008.061234. [DOI] [PubMed] [Google Scholar]
- 98.Uppal S, Diggle CP, Carr IM, Fishwick CW, Ahmed M, Ibrahim GH, et al. Mutations in15-hydroxyprostaglandin dehydrogenase cause primary hypertrophic osteoarthropathy. Nat Genet. 2008;40:789–93. doi: 10.1038/ng.153. [DOI] [PubMed] [Google Scholar]
- 99.Pilbeam CC, Raisz LG. Prostaglandins, leukotrienes and bone. In: Curtis-Prior P, editor. The Eicosanoids. UK: John Wiley and Sons, Ltd. NJ; 2004. pp. 289–98. [Google Scholar]
- 100.Ensor CM, Tai HH. 15-Hydroxyprostaglandin dehydrogenase. J Lipid Mediat Cell Signal. 1995;12:313–9. doi: 10.1016/0929-7855(95)00040-w. [DOI] [PubMed] [Google Scholar]
- 101.Currie AE, Gallagher PJ. The pathology of clubbing: Vascular changes in the nail bed. Br J Dis Chest. 1988;82:382–5. doi: 10.1016/0007-0971(88)90092-7. [DOI] [PubMed] [Google Scholar]
- 102.Stein RA. Digital clubbing: Finally a gene. Nature Genetics. 2008;40:789–93. [Google Scholar]
- 103.Asai S, Asada K, Miyachi H. Clubbed fingers in patients with inflammatory gingival hyperplasia. Intern med. 2005;44:1307–11. doi: 10.2169/internalmedicine.44.1307. [DOI] [PubMed] [Google Scholar]
- 104.Field AS, Jr, Gray FD., Jr The width of the nail fold capillary stream in clubbing. Chest. 1962;41:631–7. doi: 10.1378/chest.41.6.631. [DOI] [PubMed] [Google Scholar]
- 105.Moreira AL, Porto NS, Moreira JS, Ulbrich-Kulczynski JM, Irion KL. Clubbed fingers: Radiological evaluation of the nail bed thickness. Clin Anat. 2008;21:314–8. doi: 10.1002/ca.20623. [DOI] [PubMed] [Google Scholar]
- 106.Rault R, Carpenter B. Pseudoclubbing in chronic renal failure. Q J Med. 1989;73:1063–9. [PubMed] [Google Scholar]
- 107.De Giorgi V, Sestini S, Massi D, Panelos J, Papi F, Alfaioli B, et al. Acquired pseudoclubbing of a fingernail caused by spontaneous subungual haemangioma. J Eur Acad Dermatol Venereol. 2008;22:1501–3. doi: 10.1111/j.1468-3083.2008.02686.x. [DOI] [PubMed] [Google Scholar]
- 108.Wavreille G, Baroncini M, Rtaimate M. A rare cause of pseudoclubbing (pseudohippocratic finger): The acrometastasis.A case report. Chir Main. 2009;28:381–3. doi: 10.1016/j.main.2009.08.012. [DOI] [PubMed] [Google Scholar]
- 109.Farzaneh-Far A. Images in clinical medicine. Pseudoclubbing. N Engl J Med. 2006;354:e14. doi: 10.1056/NEJMicm031107. [DOI] [PubMed] [Google Scholar]
- 110.Santiago MB, Lima I, Feitosa AC, Braz Ade S, Miranda LG. Pseudoclubbing: Is It different from clubbing? Semin Arthritis Rheum. 2009;38:452–7. doi: 10.1016/j.semarthrit.2008.01.018. [DOI] [PubMed] [Google Scholar]


