Abstract
Background:
Last year, our pathology informatics fellowship added informatics-based interactive case studies to its existing educational platform of operational and research rotations, clinical conferences, a common core curriculum with an accompanying didactic course, and national meetings.
Methods:
The structure of the informatics case studies was based on the traditional business school case study format. Three different formats were used, varying in length from short, 15-minute scenarios to more formal multiple hour-long case studies. Case studies were presented over the course of three retreats (Fall 2011, Winter 2012, and Spring 2012) and involved both local and visiting faculty and fellows.
Results:
Both faculty and fellows found the case studies and the retreats educational, valuable, and enjoyable. From this positive feedback, we plan to incorporate the retreats in future academic years as an educational component of our fellowship program.
Conclusions:
Interactive case studies appear to be valuable in teaching several aspects of pathology informatics that are difficult to teach in more traditional venues (rotations and didactic class sessions). Case studies have become an important component of our fellowship's educational platform.
Keywords: Case study method, clinical informatics training, clinical informatics, informatics fellowship training, informatics teaching, pathology informatics fellowship, pathology informatics training, pathology informatics, retreats
FELLOWSHIP TRAINING IN PATHOLOGY INFORMATICS
Pathologists analyze blood, fluids, and tissue. From that analysis they provide accurate, quantitative, and, ultimately, clinically actionable information to physicians. The maintenance, care, and communication of pathology information is so important to healthcare that, over the past several decades, a pathology subspecialty has developed specifically focused on the study and management of information, information systems and processes – Pathology Informatics. In fact, several formal fellowships are currently available in Pathology Informatics.[1] These are not currently accredited by the Accreditation Council for Graduate Medical Education (ACGME) and the optimal way of teaching pathologists to become informaticians has not yet been completely defined. In this technical note, we discuss an innovative method for communicating to fellows some of the more difficult-to-teach Pathology Informatics topics and how that applies to the collective body of knowledge for Pathology Informatics training as a whole.
RELEVANT ASPECTS OF THE HEALTHCARE PATHOLOGY INFORMATICS FELLOWSHIP TRAINING PROGRAM
Our Pathology Informatics fellowship program was established in 2007, with the first fellow officially completing the program in 2009. The program operates across multiple sites, consisting of two large academic medical centers and a large community hospital. The fellowship is overseen by an Education Committee, which is responsible for all education policy development, approval of new training programs, and strategic educational initiatives throughout the healthcare system. A formal charter, known as the “Program Description and Written Curriculum”, defines the structure and operation of the program and has been accepted by the Education Committee. This acceptance represents the healthcare system Office of Graduate Medical Education's (GME) approval of the program.
There are presently 11 active faculty members within the fellowship program with several additional associate faculty members distributed across the three main sites of the fellowship. Of the 11 active faculty members, 8 are clinical faculty and practice across a broad range of pathology subspecialties, combining their informatics skills with their subspecialty knowledge. Of the 11 faculty members, 3 are purely research-based and offer research rotations and opportunities for fellows.
THE FELLOWSHIP PROGRAM'S EDUCATIONAL STRUCTURE
The fellowship program employs several educational mechanisms that fit together to prepare fellows to become pathology informaticians:
Operational Rotations
Fellows work with faculty, information services (IS) teams, and leadership committees on active, usually complex, long-term projects in the department or health system. These projects tend to involve specific areas of informatics such as data management, laboratory information system (LIS) operations, and imaging and are dependent upon current active projects within one of our healthcare system's hospitals.
Research Rotations
Fellows perform informatics research in one or more of our facilities under the mentorship of our faculty.
Clinical Concentrations
Fellows are encouraged to attend one or more traditional Pathology or Laboratory Medicine conferences in a diagnostic subspecialty of the fellow's interest, in addition to having the ability to participate in elective clinical rotations.
The Core Curriculum and Didactic Course
Fellows attend a required, 92-hour series of didactic sessions over a 2-year cycle, led by the fellowship program director or other relevant faculty. The course is guided by a formal, core curriculum that has a curated, comprehensive reading list covering the wide scope of pathology informatics. Details of the core curriculum didactic course have been submitted for publication and are in press.[2]
National Meetings
Fellows must attend at least one national meeting and are urged to present at that meeting. National meetings in Pathology Informatics, such as the Association of Pathology Informatics (API)-sponsored Pathology Informatics meeting or the College of American Pathologists (CAP)-sponsored Pathology Visions meeting are strongly encouraged in addition to the other major pathology national meetings. Fellows are also encouraged to attend international working groups (e.g., Diagnostic Imaging and Communications in Medicine, Health Level 7). Attending such meetings helps fellows understand the scope, scale, and current thoughts in the field, in addition to giving them opportunities to meet other pathology informaticians.
Retreats
Fellows attend a series of required, 1 or 2 day-long group activities taught by either local or visiting faculty that are focused on decision-making, management, and governance issues relevant to the practice of operational and research Pathology Informatics. The retreats were incorporated into the fellowship in 2011 at the request of the fellows. The current retreats are open to active fellows in formal Pathology Informatics fellowship programs across the nation. The retreats teach through interactive scenarios and case studies and are the central topic of this communication.
Of the six components of the fellowship, the first three (operational rotations, research rotations, and clinical concentrations) are individualized to meet the interests and expected career paths of each fellow. A rotation schedule is tailored to the fellow in a series of meetings between him/her and the program director. This process starts prior to the fellowship and is then fine-tuned throughout the fellow's training. The overall goal of this individualized approach is to provide the fellow a depth of knowledge in one or two relatively specialized areas of Pathology Informatics through a “hands-on” educational experience that fits the interests and career goals of each candidate. In fact, this approach has been recently formalized through the creation of multiple fellowship tracks, a process that allows for easier understanding and customization of a fellow's educational experience.[3]
The three remaining components of the fellowship constitute the backbone (referred to as the “common core”) of the fellowship program and emphasize the common knowledge and skill sets that all graduating fellows should possess. These components, the completion of the core curriculum and didactic course, attendance at national meetings, and participation in the retreats, are mandatory requirements for all fellows and have been designed to provide a broad informatics knowledge set across the entire field, independent of individual fellow interests or career path.
Together, the six components that make up our fellowship program allow for both individualized specialization and a common core breadth of knowledge in Pathology Informatics. Additional information concerning the structure and operations of the fellowship program, including how each of the educational components has been implemented, how they relate to the ACGME six core competencies, and how they compare to recently proposed Clinical Informatics training programs requirements, have been published previously.[4]
THE PURPOSE AND RATIONALE FOR THE RETREATS
The focus of pathology training in informatics has changed over the years. Early on, in the infancy of Pathology Informatics, the emphasis mainly surrounded information technology (IT) issues in the laboratory, such as computer hardware, operating systems, electronic communications, word processing, spreadsheets, databases, and programming.[5] Over the past 20 years, however, as these IT components have become both ubiquitous and standard within laboratories, the role of informatics in pathology has shifted from interacting with basic IT components to more operational, administrative, managerial, and leadership roles instead.
This shift in both the focus and role of Pathology Informatics necessitates an equal shift in the way we train future pathology informaticians. Unfortunately, most graduating pathology residents (i.e., our entering Pathology Informatics fellows) do not have much experience with these new skills sets. Recently, a white paper from the CAP and the Association of Pathology Chairs (APC) identified a number of gaps in pathology residency education, of which at least six are directly pertinent to the practice of Pathology Informatics. These areas include interpersonal and communication skills, ability to recognize limitations, readiness to practice independently, professionalism, management, and preparation in laboratory medical direction and management.[6]
We would like to add to this list additional skills we have found necessary for the success of pathology informaticians: project management, team leading, effective leadership, negotiation, conflict management, consensus-building, decision-making, thinking on one's feet, navigating hospital and departmental leadership, recruitment, and resolving human resources issues. By their nature, these skill sets are difficult to teach in a rotation or didactic course and most often require more than just passive class time. One or two classes, even ones devoted exclusively to each of the aforementioned topics, have extremely varying penetrance for fellows. While informative, they cannot replace first-hand experience in these matters.
Furthermore, as digital healthcare information has exploded, the role of the pathology informatician has evolved from being behind-the-scenes to more front-and-center within both the department and the healthcare institution. Pathology informaticians now play important roles as both the face and spokesperson for the department in regards to enterprise projects (e.g., the implementation of a new healthcare information system), in addition to being both a leader and liaison between pathologists, laboratory technical staff, vendors, and central IT for pathology-based projects.
Interestingly, in a recent survey performed in our fellowship program, the majority of our fellows indicated that one of the reasons for choosing to do a Pathology Informatics fellowship was to better position themselves to become leaders within their future departments and healthcare institutions.[3]
However, our fellows also felt that the skill sets mentioned above were the most challenging to prepare for as they contemplated the transition from fellowship to a real world job in Pathology Informatics.
The goals and concerns of our fellows are not unique. A recent study of five Chief Medical Information Officers showed that the skills they felt to be the most important in the successful performance of their job were leadership, communication, and consensus-building. In addition, these individuals also stated a desire to be part of senior physician executive teams, and that they did not want to be viewed as “just techie doctors.”[7]
Thus, despite their importance to informatics fellow education, tackling the issue of teaching these skills sets is difficult. They are not extensively taught in medical school, nor are they truly integrated into the graduated responsibility model of pathology residencies or fellowships. Another solution, therefore, is to look outside the typical “medical education” box – in this case, by looking at the business school model.
In many ways, informatics governance, management, and leadership skill sets directly overlap with those that are fundamental to business school curricula. Furthermore, business schools face many of the same challenges in their student body that informatics programs do. Like informatics fellows, most business school students are not ready to make important, real-world decisions. Merging two laboratories and their information systems has many of the same issues as merging two companies, and the notion of an informatics fellow managing the former situation is almost as unlikely as a business school student managing the latter.
However, there is a method that business schools have employed successfully to train these fundamental skill sets – the interactive case study. In early 2011, one of our fellows (and the first author on this paper) proposed adapting the case study model to Pathology Informatics fellowship training in a series of 1 to 2-day fellowship retreats. This concept was implemented over the course of three retreats this academic year (summer 2011, winter 2012, and spring 2012).
INTRODUCING THE CASE STUDY METHOD
The case study is a time-honored teaching method used at many business schools that provides a more active environment for learning managerial skills as compared with traditional, lecture-based classes. With the case study, an instructor presents a scenario, ideally based off of a real-life situation, and students work together as a team to come up with one or more plausible solutions. The primary goal of the case study method is for students to put themselves in the position of leaders and managers for the given scenario. They must analyze the situation, decide on one or more courses of action, and provide proper qualitative and quantitative evidence to support their decisions.[8]
One of the major strengths to this method is that, as presented, there should be no single “right” answer to the case study. The paths that case studies can take are not necessarily linear, with most scenarios leading to a variety of alternative courses of action. A wide array of viable paths should be explored during the course of the discussion. In fact, instructors at times will let students choose and follow a less preferable, or “wrong,” course of action in order to allow them to discover what happens when such a choice is made.[9]
Case studies can be of varying lengths, ranging from just a paragraph to extremely long, complicated versions exceeding over 20 pages. For a truly successful case study experience, students are expected to read the case beforehand, understand the issues involved, and come prepared to provide answers for whatever the facilitator might ask. As these cases are typically based on real events, data such as costs, revenue, and personnel management are customarily written into the case. For some case studies, an addendum is passed out at the conclusion describing what actually happened in the real-life business situation, thus allowing the students to compare their solution(s) to actual events.
ADAPTING THE CASE STUDY METHOD TO PATHOLOGY INFORMATICS TRAINING
As mentioned before, many of the skill sets a fellow needs in order to become a successful pathology informatician are hard to teach in the traditional classroom setting. Instead, the case study method, as described above, seems to lend itself more readily to this type of teaching, emphasizing activity and participation with decision-making.
There are three main hurdles to overcome in order to adapt this teaching method to pathology informatics fellowship training: (1) committed faculty participation, with faculty experienced in a wide array of pathology informatics topics, amenable to leading the case studies, (2) pre-developed and appropriately themed pathology informatics case studies, and (3) the participation of an adequate quorum of fellows to better simulate activities such as brainstorming, consensus-building, and decision-making by a group of individuals that happens as real-world informatics challenges are solved.
Unfortunately, while some fellowships may be able to fulfill the first two requirements internally, the third is the most difficult to achieve as most Pathology Informatics fellowships only have one to two fellows at a given time. Therefore, in order to maximize this experience, all of the Pathology Informatics fellows across the country (10 fellows in total) were invited to participate in the case study method, in the form of dedicated fellowship retreats.
Similar to the business method, Pathology Informatics faculty members are asked to create and facilitate cases from their area(s) of expertise, ideally calling upon their own work experiences. In light of the nature of the case study method (teaching managerial and leadership skills), instructors are encouraged to create case studies that revolve around operational issues and problems. Examples of operational cases include implementing a new LIS, choosing between two technologies or platforms, or developing a plan for implementing barcoding in a pathology laboratory. Often these cases are based on lessons learned early in the instructor's career, and as these situations are manipulated in the presentation, both good and bad choices that were made or considered can become valuable learning experiences.
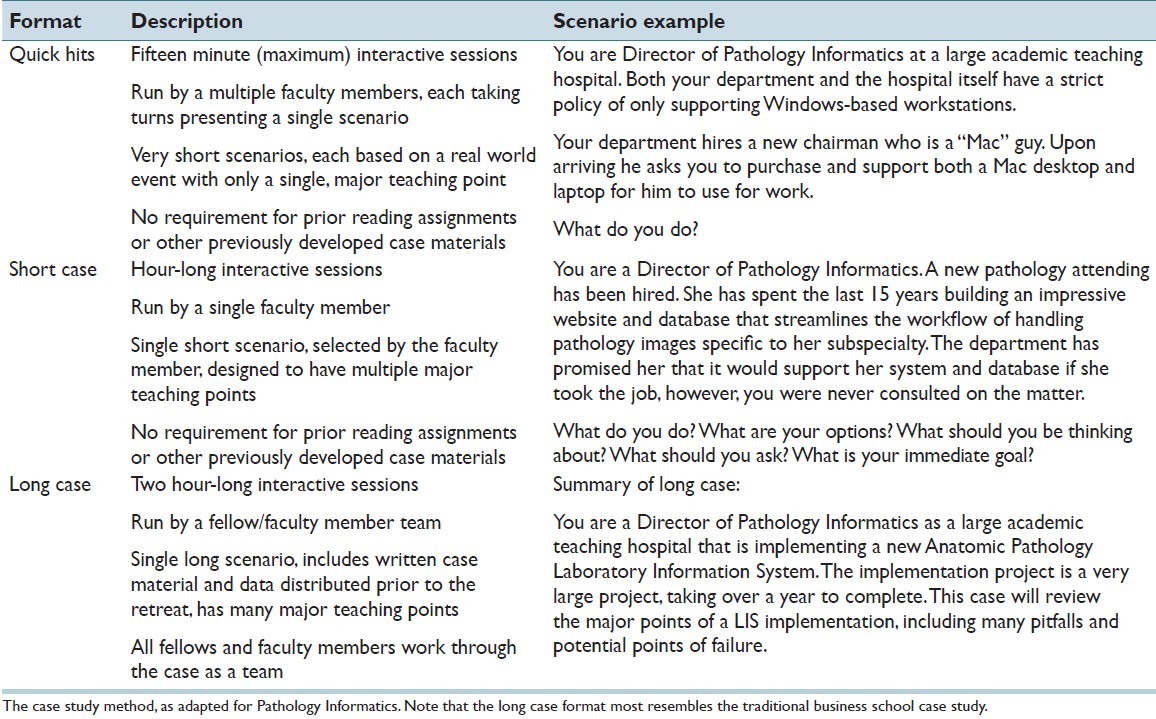
One area in which our pathology informatics adaptation of the case study method differs from the customary business school case study is in the length and complexity of the cases. Currently, the majority of our case studies take the form of short scenarios. In general, the faculty present their scenarios and the guide the group, via questions and additional information, through the major points of each case. In our retreats, there are three main categories of cases: the 15 minute Quick Hit, 1-hour Short Case, and 2-hour Long Case [Table 1].
Table 1.
Pathology informatics case study formats and examples
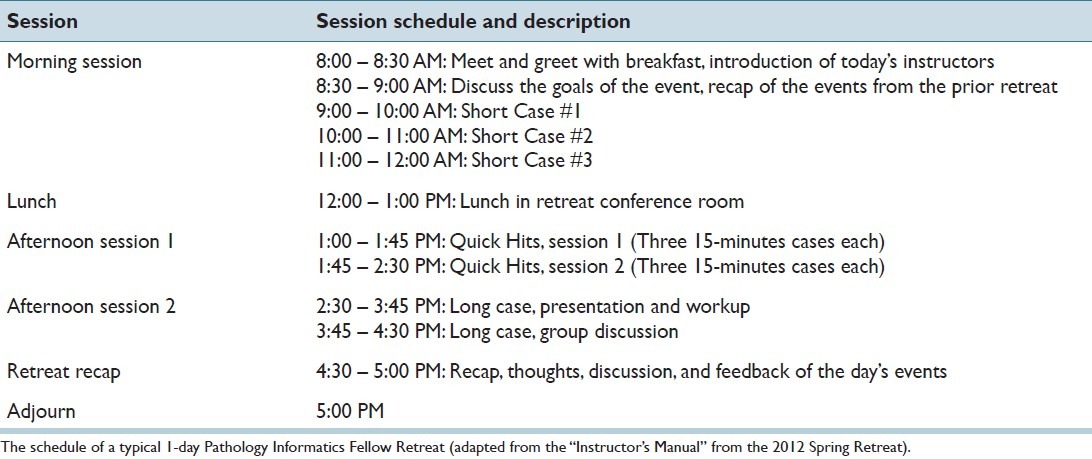
To date, the retreats have lasted for 1-2 days. A schedule for a typical 1-day retreat is shown in Table 2. For the 2-day retreat, the second day was a half-day long and covered two additional Long Cases presented by the faculty.
Table 2.
Schedule of a typical one-day long retreat
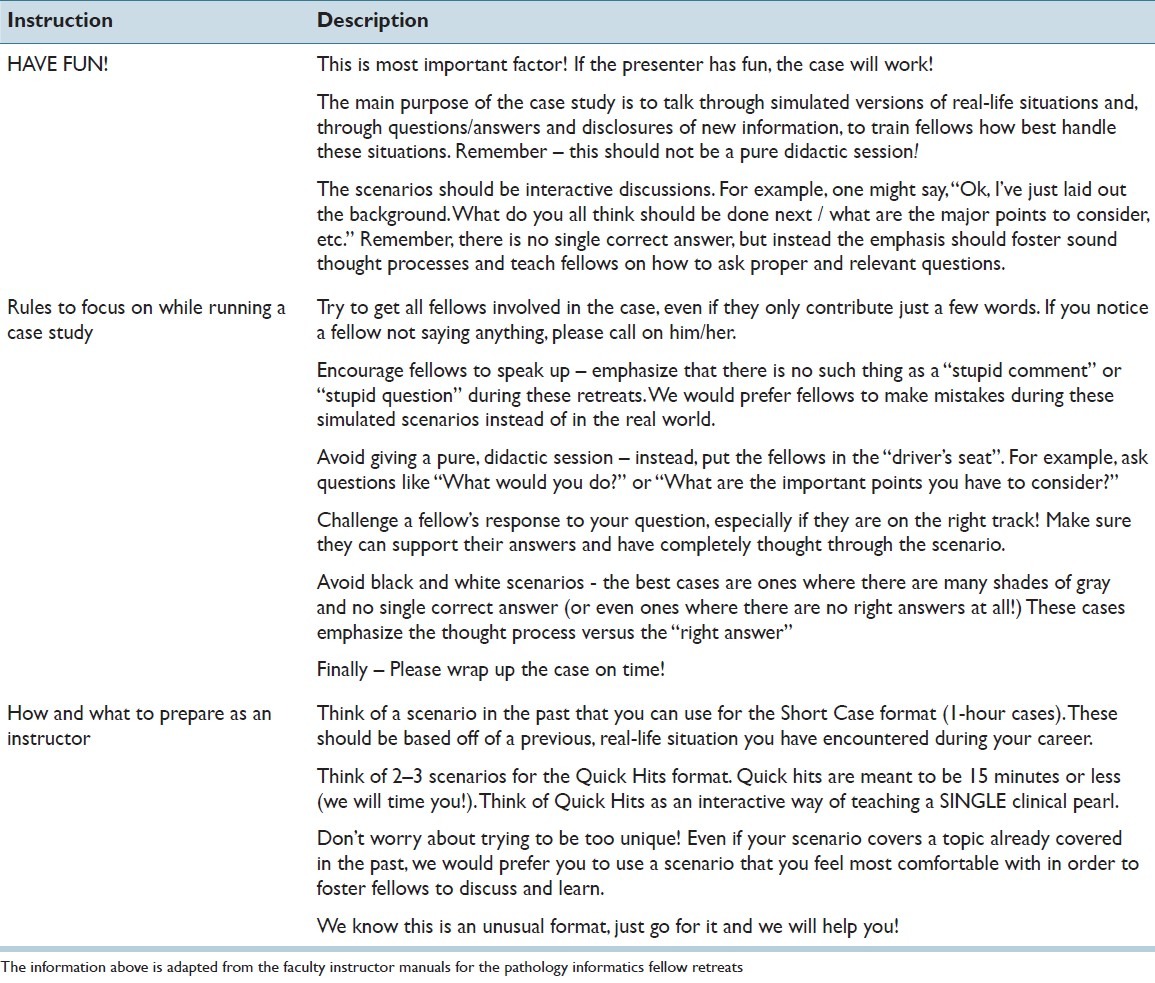
One of the main reasons we had to make our case studies shorter than typical business school cases was because the vast majority of our participating faculty had limited formal experience teaching by this method. In order to adequately prepare our faculty instructors, we provided an instructor's guide for each retreat, emphasizing the major concepts of the case study method. A shortened version of one of the instructor's guides is presented in Table 3.
Table 3.
Faculty instructions for a successful retreat
THE RETREATS IN 2011–2012
Each retreat was led by three to four instructors composed of either local or visiting faculty. On average, there were 10 pathology informatics fellows present for each retreat, in addition to 1–3 rotating residents and/or medical students as well, both local and visiting. Each retreat was held in a private conference room at one of our academic medical centers.
The events of each retreat are summarized below.
Summer 2011
This was a 2-day retreat with visiting instructors from Emory University, the Cleveland Clinic Foundation, and the Henry Ford Hospital System, with the retreat concentrating on a wide range of leadership and management issues. The participating faculty and fellows are shown in Figure 1. For the Quick Hits, the faculty described a few of their more unusual cases, such as a request for the status of a project that did not exist, a laboratory barcoding system that mysteriously stopped working every night at midnight, and cases that were signed out in the LIS but mysteriously never made it to the electronic medical record. The Short Cases focused on project management, successful communications within departments and teams, and managing expectations, cost vs benefit analyses, and system integration issues. The Long Cases focused on meaningful use in pathology laboratories and LOINC (Logical Observation Identifiers Names and Codes), ICD-10 (International Statistical Classification of Diseases, 10th revision), and laboratory requirements under HIPAA (Health Insurance Portability and Accountability Act).
Figure 1.
Pathology informatics faculty and fellows at the summer 2011 retreat
Winter 2012
This was a 1-day retreat, with the instructors composed of three local faculty from our own program and a visiting faculty member from Weill Cornell Medical College. The retreat was composed of three Short Cases and one Long Case; no Quick Hits were done. The topics covered were more architectural in nature, such as exploring the elements and considerations of provider order entry (POE) systems, going through the planning and implementation of a new outreach interface, and discussing considerations involved with the setup of next-generation DNA sequencing molecular laboratories.
Spring 2012
This was a 1-day retreat with visiting instructors from Yale University, the University of Michigan, and the University of Pittsburgh. The retreat focused primarily on leadership and communication scenarios and was composed of two rounds of Quick Hits, three Short Cases, and a single Long Case [Table 3]. Scenario topics included implementation of a new online frozen section reporting system, implementation of a new enterprise master patient index (EMPI), pitfalls in setting up data sharing and research collaborations between large academic institutions, and leadership challenges encountered during the implementation of a new LIS.
CONCLUSIONS AND THE FUTURE OF THE RETREATS
During the 2011–2012 academic year, our program (with assistance from the faculty from Cleveland Clinic, Cornell, Emory, Henry Ford, Michigan, Pittsburgh, and Yale) implemented a series of educational retreats open to all active pathology informatics fellows from formal fellowship programs. These retreats were based on the case study method made popular by business schools, using interactive scenarios and cases to teach fellows principles of decision-making, analytic thought, leadership, management, and communications in the practice of Pathology Informatics. These retreats complement the other educational tools in our program (operational rotations, research rotations, clinical concentration, the core curriculum and didactic course, and participation in national meetings).
While education has been the primary driver of the retreats, there is also an important social component that has emerged. This secondary driver embodies the idea that pathologists willing to commit 1 or 2 years of pathology informatics training should have the opportunities to get to know their compatriots in other programs and to learn from faculty from outside of their program. The main reason that we chose to host three retreats over the 2011–2012 academic year was to give all of the active pathology informatics fellows in the country a chance to meet on a quarterly basis (three informatics retreats and the Pathology Informatics 2011 meeting).
From the perspective of both the educational and social standpoints, the retreats to date have been successful. While we have yet to achieve the level of sophistication using case studies as seen in the business school setting, participating fellows uniformly feel that the retreats have created a very positive and effective teaching environment (post-retreat surveys, data not shown). Further, the fellows have expressed great satisfaction in being able to interact and learn from experienced faculty from other institutions, and the faculty have enjoyed teaching and getting to know the fellows in this format. One faculty member stated that the information shared at these retreats by the group of faculty might have prevented some early mistakes had the faculty member been able to attend such a retreat prior to taking a position as an informatics director. The most commonly used word to describe the retreat experience, by both the fellows and faculty, was “fun”.
We plan to offer the retreats again in the future, starting with the 2012–2013 academic year. With each year that we do this, the faculty will continue to improve on presenting case studies; further, the faculty and fellows are considering additional ways of enhancing the retreat's educational and social experience. As with many new initiatives, the main long-term risk to hosting these retreats is financial. As the number of pathology informatics fellows continues to grow across the country, the ability to fund each fellow's travel to and from the retreats will become increasingly compromised. We believe, however, that physically meeting at single, common location is important to the success of these retreats, and thus we will continue to look into mechanisms that will allow for long-term support of this educational experience.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2012/3/1/41/103995
REFERENCES
- 1.Pathologyinformatics.org. Training Opportunities in Pathology Informatics. Association for Pathology Informatics. c2011. [Last cited on 2012 Apr 15]. Available from: http://www.pathologyinformatics.org/content/training-opportunities-pathologyinformatics .
- 2.McClintock DS, Levy BP, Lane WJ, Lee RE, Baron JM, Klepeis VE, et al. A core curriculum for clinical fellowship training in pathology informatics. J Pathol Inform. 2012;3:31. doi: 10.4103/2153-3539.100364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levy BP, McClintock DS, Lee RE, Lane WJ, Klepeis VE, Baron JM, et al. Different tracks for pathology informatics fellowship training: Experiences of and input from trainees in a large multisite fellowship program. J Pathol Inform. 2012;3:30. doi: 10.4103/2153-3539.100362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gilbertson JR, McClintock DS, Lee RE, Onozato M, Kuo FC, Beckwith BA, et al. Clinical fellowship training in pathology informatics: A program description. J Pathol Inform. 2012;3:11. doi: 10.4103/2153-3539.93893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peters M, Clark IR. Pathologists and training in information technology. J Clin Pathol. 1992;45:187–7. doi: 10.1136/jcp.45.3.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Talbert ML, Ashwood ER, Brownlee NA, Clark JR, Horowitz RE, Lepoff RB, et al. College of American Pathologists; Association of Pathology Chairs. Resident preparation for practice: A white paper from the College of American Pathologists and Association of Pathology Chairs. Arch Pathol Lab Med. 2009;133:1139–47. doi: 10.5858/133.7.1139. [DOI] [PubMed] [Google Scholar]
- 7.Hersh W. The Health Information Technology Workforce: Estimations of demands and a framework for requirements. Appl Clin Inform. 2010;1:197–212. doi: 10.4338/ACI-2009-11-R-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hammond JS. Learning by the case method. Harv Bus Rev. 1976:4. [Google Scholar]
- 9.Ellet W. Case study handbook: How to read, discuss, and write persuasively about cases. Boston: Harvard Business Press; 2007. [Google Scholar]