Abstract
Background:
It has been suggested that patients with mental illness wait longer for care than other patients in the emergency department. We determined wait times for patients with and without mental health diagnoses during crowded and noncrowded periods in the emergency department.
Methods:
We conducted a population-based retrospective cohort analysis of adults seen in 155 emergency departments in Ontario between April 2007 and March 2009. We compared wait times and triage scores for patients with mental illness to those for all other patients who presented to the emergency department during the study period.
Results:
The patients with mental illness (n = 51 381) received higher priority triage scores than other patients, regardless of crowding. The time to assessment by a physician was longer overall for patients with mental illness than for other patients (median 82, interquartile range [IQR] 41–147 min v. median 75 [IQR 36–140] min; p < 0.001). The median time from the decision to admit the patient to hospital to ward transfer was markedly shorter for patients with mental illness than for other patients (median 74 [IQR 15–215] min v. median 152 [IQR 45–605] min; p < 0.001). After adjustment for other variables, patients with mental illness waited 10 minutes longer to see a physician compared with other patients during noncrowded periods (95% confidence interval [CI] 8 to 11), but they waited significantly less time than other patients as crowding increased (mild crowding: −14 [95% CI −12 to −15] min; moderate crowding: −38 [95% CI −35 to −42] min; severe crowding: −48 [95% CI −39 to −56] min; p < 0.001).
Interpretation:
Patients with mental illness were triaged appropriately in Ontario’s emergency departments. These patients waited less time than other patients to see a physician under crowded conditions and only slightly longer under noncrowded conditions.
In a 2008 report, the Schizophrenia Society of Ontario recommended adding a psychiatric wait times component to the Ontario government’s Emergency Room Wait Times Strategy.1 They suggested that patients who present to the emergency department in psychiatric distress wait longer for care than other patients and that they are given a low priority triage score2 (all patients are assigned a triage score when they first arrive at the emergency department, which may determine when and where they are seen by a physician).3 The Kirby Report, a senate report on mental illness and addiction in Canada, also decried differential emergency care for patients with mental illness.4
A recent study found that patients with acute myocardial infarction are given lower priority care in the emergency department if they have a charted history of depression.5 However, whether patients who present to the emergency department for mental illness receive slower care than other patients is not known. In this study, we compared the emergency department wait times and triage scores for patients with affective and psychotic disorders to those for other patients, both in noncrowded conditions and during periods of crowding. Because we believe that triage nurses apply triage principles consistently to all emergency patients while physicians may be less likely to adhere to the guidelines, we hypothesized that there would be no “down-triage” (assigning a lower priority triage score) of these patients, but that patients with mental illness would have longer delays to see a physician, relative to other patients.
Methods
Data sources and study population
This retrospective cohort study received ethics approval from Sunnybrook Health Sciences Centre. The cohort was created using the Canadian Institutes of Health Information’s National Ambulatory Care Reporting System, an administrative database that contains anonymized data for all visits to emergency departments in Ontario.
Using this database, we identified patients aged 18–105 with a valid Ontario Health Insurance Plan number and a primary emergency department diagnosis of an affective or psychotic disorder (Box 1) between Apr. 1, 2007, and Mar. 31, 2009. The primary diagnosis is the first diagnosis written on the emergency chart by the emergency physician, irrespective of whether the patient is admitted to hospital or discharged from the emergency department. “Discharged” refers only to patients who were discharged from the emergency department to their place of residence. We excluded anxiety and stress-related disorders (International Classification of Disease [ICD-10] codes F40–F48) because the accuracy of these codes may be poor (Dr. Jan Huxx, personal communication, 2009). We included only index visits (first eligible visit within the study period) and patients whose chief complaint was psychiatric (Box 1).6 The related complaint was necessary because it would be expected to affect the triage categorization.
Box 1: International classification of disease (ICD-10) codes6 used to define the study cohort.
-
Primary emergency department diagnosis entered in NACRS
F20–F29: schizophrenia, schizotypal and delusional disorders
F30–F39: mood [affective] disorders
F99: unspecified mental disorder
R45.8: other symptoms and signs involving emotional state, suicidal ideation
X60–X84: intentional self-harm
-
Related chief complaint* in NACRS
F20–F29: psychosis
F30–F39: depression
R44: hallucinations
R45: emotional state, suicidal ideation
R46: bizarre appearance/behaviour
Note: NACRS = National Ambulatory Care Reporting System.
Defined as “the symptom, complaint, problem or reason for seeking emergency medical care.”
We excluded patients seen at pediatric emergency departments and those seen at the single free-standing psychiatric emergency department (where emergency care would proceed in a markedly different way). The same exclusion criteria were applied to index visits during the same period for all other patients in the National Ambulatory Care Reporting System, who formed the comparison group.
Outcome measures
The primary outcome was time to see an emergency physician (time to physician assessment), which we defined as time from triage to first assessment by the physician. Secondary outcome measures included triage categorization and time from hospital admission orders to physical departure from the emergency department (admission decision to ward transfer) for an in-hospital bed (only patients admitted to hospital were included in this outcome). The latter was defined as the time from when the physician wrote the admission order to the time when the patient physically left the emergency department for the ward. These outcomes are all collected in the National Ambulatory Care Reporting System.
We determined triage categorization using the Canadian Triage and Acuity Scale,3 which is based on clinical descriptors. The use of this system is mandatory in Ontario’s emergency departments. A trained triage nurse assigns a triage score to every patient who presents to the emergency department. The score is based on illness acuity, and there are 5 levels: resuscitation (score of 1), emergent (2), urgent (3), less urgent (4) and nonurgent (5), each with a recommended time to be seen by a physician: immediately, within 15 minutes, 30 minutes, 1 hour and within 2 hours, respectively. Guidelines for patients whose chief complaint is mental health–related are summarized in Box 2.3,7 Given that scores of 1 and 5 are relatively rare among patients with mental illness, we condensed the categories into 3 levels to ensure appropriate sample sizes in each triage level (1–2, 3, 4–5).
Box 2: Canadian Triage and Acuity Scale guidelines for patients with a mental health–related presenting complaint.
Recommended Triage Score* and description
2: Display “acute psychosis/extreme agitation”
3: Have normal vital signs but are experiencing “acute psychosis and/or [are] suicidal”
4: Are “suicidal/depressed” but have “normal vital signs and are not agitated”
5: Have other, milder psychiatric complaints, including access to care
A score of 1 is not a standard score assigned to patients with mental illness, but it could be used, as per Canadian Triage and Acuity Scale guidelines,3,7 in rare instances (e.g., actively violent patient who requires restraint, or actively suicidal patient who is attempting to run from the emergency department prior to physician assessment).
Methods of measurement
We used length of stay in the emergency department as a measure of crowding. Length of stay is a good proxy for crowding8,9 and is commonly used in crowding research.10–12 This variable is calculated by dividing the day into three 8-hour periods and determining the median length-of-stay of all patients who were present in the emergency department during that period. Length-of-stay was defined as the time from triage until final emergency department disposition, and it was calculated for patients with a similar illness priority (triage score of either 1–3 or 4–5). Included in this measure were patients admitted but waiting for a bed in the hospital. We divided crowding into 4 levels based on median length of stay: 0–3 hours (no crowding), 3–6 hours (mild crowding), 6–9 hours (moderate crowding) and > 9 hours (severe crowding). We used a simplified version of the above crowding measure solely for the analysis of triage scores and how they change with crowding; this simplified version excluded triage categorization because triage was being measured in this analysis.
Statistical analysis
We compared time to physician assessment and the time from admission decision to ward transfer (hereafter referred to as wait times) using median wait times for the study cohort relative to all other emergency patients, overall and by triage level. The results are presented by triage level because illness acuity should be the main determinant of wait time. Next, we compared median wait times at different levels of crowding.
We evaluated the adjusted wait times using quantile regression, which is appropriate when times are right-skewed; quantile regression models on the median value.13 Model covariates included age, sex, time of day of presentation to the emergency department, day of the week, arrival type (ambulance or other), triage level (1–2, 3 or 4–5), hospital type (teaching, community or small) and emergency department crowding. Interaction terms for mental illness with crowding and triage level were tested.
Results
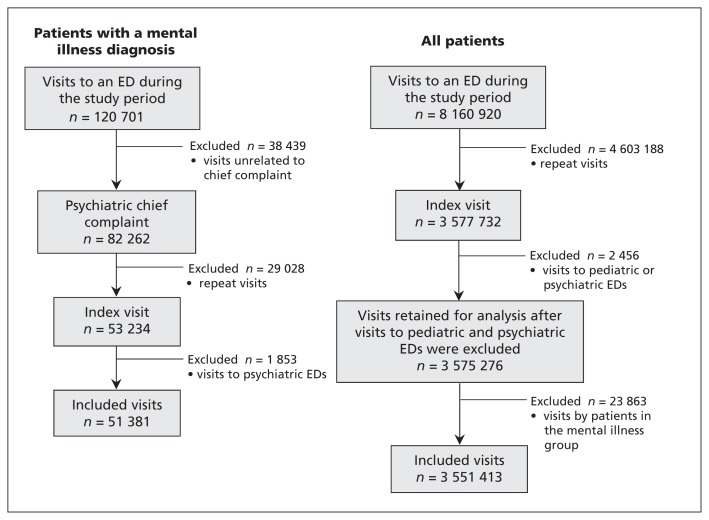
Of the 120 701 emergency department visits by patients with a primary diagnosis of affective (70.0%) or psychotic disorder (30.0%), there were 51 381 visits that met our inclusion criteria (Figure 1). The included visits were by patients who were younger than other emergency patients, with a similar proportion of females (Table 1).
Figure 1:
Flow chart for development of the study cohort (visits by adults aged 18–105 years from April 2007 to March 2009). ED = emergency department.
Table 1:
Baseline characteristics of the study cohort (patients with a primary emergency department diagnosis of a mood [affective] disorder or psychotic disorder and a related chief complaint)
| Characteristic | Primary diagnosis of mental illness | Other diagnosis |
|---|---|---|
| Index visits, no. | 51 381 | 3 551 413 |
| Age, mean ± SD | 40.0 ± 15.3 | 48.0 ± 19.7 |
| Female (%) | 26 252 (51.1) | 1 855 625 (52.3) |
| Arrived by ambulance (%) | 8 270 (16.1) | 499 071 (14.1) |
| Time to physician assessment,* median (IQR), min | 82 (41–147) | 75 (36–140) |
| Time to physician assessment, mean ± SD, min | 110 ± 107 | 103 ± 387 |
| Length-of-stay, median (IQR), min | 266 (147–493) | 171 (92–302) |
| Admissions, no. (%) | 21 089 (41.0) | 362 209 (10.2) |
| Decision to admit time, median (IQR)†, min | 74 (15–215) | 152 (45–605) |
| Decision to admit time, mean ± SD, min | 374 ± 1 639 | 531 ± 2 467 |
| Crowding status, no (%) | ||
| No crowding‡ | 14 151 (28.5) | 1 585 295 (48.1) |
| Mild crowding | 28 026 (56.5) | 1 429 061 (42.2) |
| Moderate crowding | 6 496 (13.1) | 287 056 (8.5) |
| Severe crowding | 966 (1.9) | 38 848 (1.1) |
Note: IQR = interquartile range, SD = standard deviation.
20.8% of patients had missing or unknown values.
10.2% of patients had missing or unknown values.
A small proportion (3.4%) of visits could not be assigned to a crowding level because of low numbers of patients in that emergency department during a specific period.
Most patients with mental illness received a triage score of 3 and had higher priority scores than other emergency department patients (Table 2). Despite receiving higher priority scores, the median time to assessment by a physician was 7 minutes longer for patients in the mental illness group than in the control group (Table 1). However, there was an interaction between triage score and time to assessment (p < 0.001). In the high priority group, patients with mental illness waited 19 minutes (unadjusted) longer to see a physician, while in the low priority group they waited 12 minutes longer. In triage category 3 (most patients), they waited 1 minute longer than other patients (Table 2).
Table 2:
Unadjusted wait times and triage scores for patients with a primary diagnosis of mental illness or another diagnosis
| Primary diagnosis of mental illness n = 51 381 |
Other diagnosis n = 3 551 413 |
p value | |
|---|---|---|---|
| Time to physician assessment, median (IQR), min | |||
| Triage category 1/2 | 70 (35–130) | 51 (25–110) | < 0.001 |
| Triage category 3 | 89 (45–155) | 88 (44–163) | 0.5 |
| Triage category 4/5 | 83 (40–150) | 71 (35–130) | < 0.001 |
| Time from admission decision to ward transfer, median (IQR), min | |||
| Triage category 1/2 | 88 (24–260) | 161 (46–640) | < 0.001 |
| Triage category 3 | 70 (15–204) | 156 (48–623) | < 0.001 |
| Triage category 4/5 | 55 (5–150) | 100 (13–346) | < 0.001 |
| Triage score, no. (%) | |||
| 1–2 | 14 027 (27.3) | 508 765 (14.3) | < 0.001 |
| 3 | 27 668 (53.9) | 1 415 701 (39.9) | < 0.001 |
| 4–5 | 9 686 (18.9) | 1 626 947 (45.8) | < 0.001 |
Note: IQR = interquartile range.
There was also an interaction between triage score and time between admission decision and ward transfer (p < 0.001). The median time between decision and transfer was 78 minutes shorter overall for patients with mental illness (Table 1), and it was 73, 86 and 45 minutes shorter in the high, middle and low priority triage categories, respectively (Table 2).
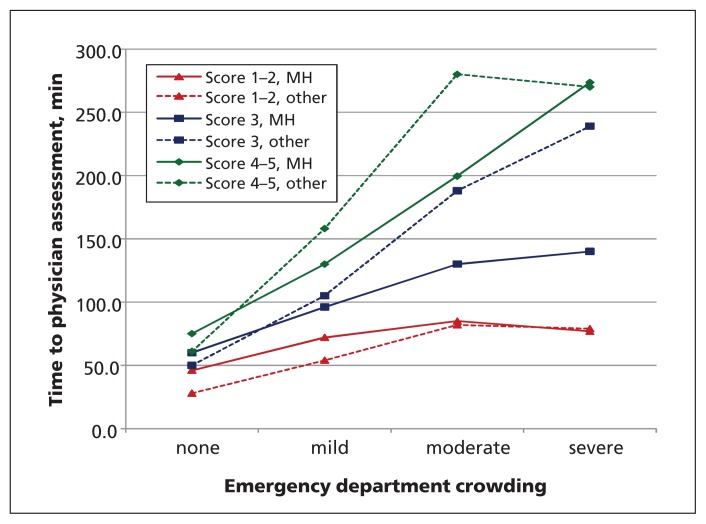
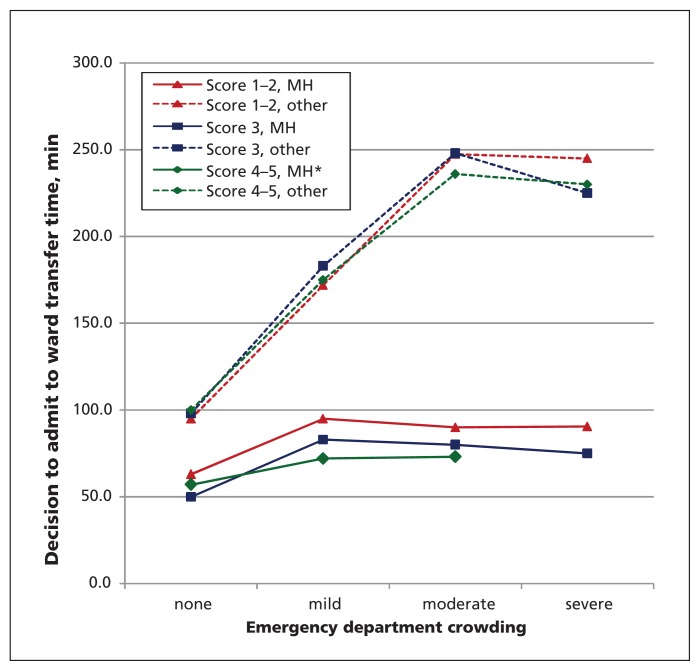
During periods of crowding, patients with mental illness appeared to be affected less than other patients, with shorter delays during crowded periods, relative to other patients (Table 3). As crowding increased, delays in time to physician assessment were greater for other patients compared to patients with mental illness in all triage groups (Figure 2). The time between admission decision and ward transfer had a similar relation (Figure 3).
Table 3:
Wait times by level of crowding in the emergency department for patients with a primary diagnosis of mental illness or another primary diagnosis
| Primary diagnosis; median (IQR) | Unadjusted analysis | Adjusted analysis | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Mental illness n = 51 381 |
Other n = 3 551 413 |
Difference between patient types | p value | Difference between patient types (95% CI) | p value | |
| Time to physician assessment,*min | ||||||
|
| ||||||
| Not crowded | 62 (32–110) | 56 (30–97) | 8 | < 0.001 | 10 (8 to 11) | < 0.001 |
|
| ||||||
| Mild crowding | 90 (47–156) | 104 (50–179) | −14 | < 0.001 | −14 (−12 to −15) | < 0.001 |
|
| ||||||
| Moderate crowding | 110 (55–202) | 143 (60–268) | −33 | < 0.001 | −39 (−35 to −42) | < 0.001 |
|
| ||||||
| Severe crowding | 96 (48–211) | 146 (51–332) | −50 | < 0.001 | −48 (−39 to −56) | < 0.001 |
|
| ||||||
| Decision to admit time† | ||||||
|
| ||||||
| Not crowded | 55 (8–144) | 97 (25–287) | −42 | < 0.001 | −5 (0 to −9) | 0.002 |
|
| ||||||
| Mild crowding | 86 (24–255) | 179 (58–705) | −93 | < 0.001 | −59 (−56 to −63) | < 0.001 |
|
| ||||||
| Moderate crowding | 86 (24–246) | 247 (77–865) | −161 | < 0.001 | −128 (−121 to −134) | < 0.001 |
|
| ||||||
| Severe crowding | 83 (23–260) | 238 (64–774) | −155 | < 0.001 | −106 (−86 to −134) | < 0.001 |
Note: CI = confidence interval, IQR = interquartile rage.
20.8% of patients had missing or unknown values.
10.2% of patients had missing or unknown values.
Figure 2:
Median time to physician assessment among patients with a mental illness diagnosis (continuous lines) versus other patients (dashed lines) in the emergency department at 4 levels of crowding. Scores are based on the Canadian Triage and Acuity Scale guidelines. Note: MH = patient whose primary diagnosis in the emergency department was mental illness and who had a related chief complaint.
Figure 3:
Median time from decision to admit the patient to ward transfer in patients with a mental illness diagnosis (continuous lines) versus all other emergency department patients (dashed lines), at 4 levels of crowding. *Value omitted because of a small sample size of admitted, low-acuity patients who were seen in severely crowded settings. Scores are based on the Canadian Triage and Acuity Scale guidelines. Note: MH = patient whose primary diagnosis in the emergency department was mental illness and who had a related chief complaint.
In the adjusted analysis, in noncrowded conditions, patients with mental illness waited 10 minutes longer than other patients to see a physician (Table 3). During periods of crowding, the adjusted time to physician assessment of patients with mental illness was affected less than the wait times of other patients: calculated wait times to see a physician during mild, moderate and severe crowding were 14, 39 and 48 minutes less, respectively, for patients with mental illness relative to other emergency department patients (Table 3). In noncrowded conditions, patients with mental illness waited an adjusted 5 minutes less from decision to admit to actual emergency department departure than other patients, and they waited 59, 128, and 106 minutes less during periods of mild, moderate, and severe crowding, respectively. The results for patients with affective disorders and patients with psychotic disorders were similar (data not shown).
In the time to physician assessment model, there was a significant interaction between triage level and patient type in the high priority group (p < 0.001). In this group, patients with mental illness waited an adjusted 30 (95% confidence interval [CI] 28 to 32) minutes longer than other patients. In the model of time from admission decision to ward transfer, there were significant interactions for the low (p < 0.004) and high priority groups (p < 0.001). In the high priority group, patients with mental illness waited 14 (95% CI 9 to −20) minutes longer than other patients. In the low priority group, patients with mental illness waited 19 (95% CI 12 to 27) minutes less than other patients.
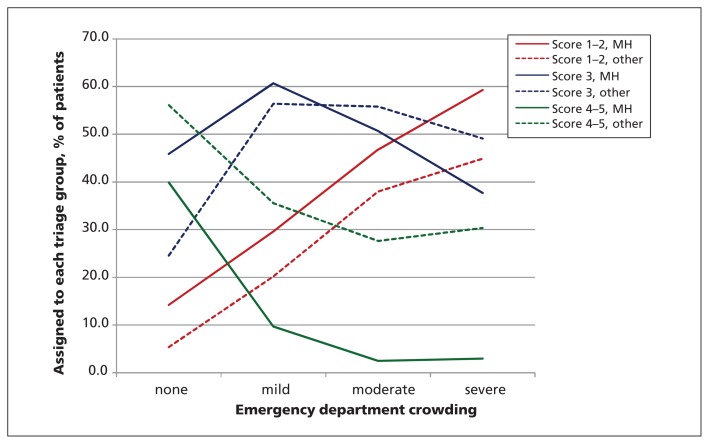
During periods of crowding, there was no evidence of down-triaging patients with mental illness. As the median length of stay increased, the proportion of patients with mental illness in the lowest priority group did not increase; instead, the proportion decreased in the lowest group and increased in the higher priority group (Figure 4). The effect was similar but weaker among other emergency department patients.
Figure 4:
Percentage of patients assigned to each triage score at each level of emergency department crowding, by patient type. For example, during periods with no crowding, 40% (continuous green line) of patients with mental illness were assigned a low priority triage score. As crowding increased, the proportion of patients with mental illness assigned to these scores decreased to 10%, then 2.5%. For other patients, the proportion who received low priority scores also decreased as crowding increased (dashed green line), but remained above 25% of those patients. Scores are based on the Canadian Triage and Acuity Scale guidelines. Note: MH = patient whose primary diagnosis in the emergency department was mental illness and who had a related chief complaint.
Interpretation
In this population-based study, we found that patients with mental illness waited slightly longer than other patients to receive emergency care when the emergency department was not crowded. Our data showed that 29% of these patients were seen during noncrowded conditions; thus, a substantial proportion of patients with mental illness experienced a small delay to see a physician, relative to other patients in the emergency department.
However, upon closer inspection, it was only patients in the highest priority triage group who waited longer than other high priority patients when the department was not crowded. One could argue that, in the higher priority group, prioritization may be justified by a known higher rate of death in certain groups, such as patients having a myocardial infarction (who are also assigned a triage score of 2), given that there is time-sensitive therapy available.6,14
Perhaps surprisingly, as crowding increased, the delays experienced by patients with mental illness were actually lesser than the delays experienced by other patients; this is in contrast to concerns that these patients are disproportionately affected by crowding in the emergency department.8,10 For time to physician assessment, this effect may be partly explained by the presence of dedicated psychiatric teams in some emergency departments. In Ontario, these teams are available in many emergency departments that see a high volume of psychiatric patients (academic centres and some large community hospitals); these are the same centres that experience crowding.15
We found no evidence of down-triaging patients with mental illness during periods of crowding. As well, as crowding increased, the time spent waiting in the emergency department for a hospital bed was markedly less for patients with mental illness than for other patients. This may be because of the relative effect of prolonged wait times experienced by patients waiting for a bed in an internal medicine ward,16 by those who require a monitored bed (not required by psychiatric patients) and by protection of psychiatric beds for these patients (preserving access that does not occur for medicine patients, for example). The presence of a psychiatric team in the emergency department (unlike many other specialties) may also facilitate shorter departure times.
Comparison with other studies
We found that the majority of patients with mental illness (52%) were given a triage score of 3, which is consistent with Canadian guidelines.3 Similar to the findings of a previous study,17 triage scores were higher for patients with mental illness than for other patients. Our findings support our belief that triage nurses follow the guidelines, and do not systematically “down-triage” patients with mental illness. Instead, our results show an increase in high priority triage scores during periods of crowding, which was greater than what occurred for other patients. This may be explained in part by low priority patients choosing to leave when they are made aware of the wait times; these patients may seek help elsewhere or at a later time, leaving behind higher priority patients who are too sick to leave. As well, triage nurses may “up-triage” patients during periods of crowding in hopes that they will be seen sooner by a physician.
Limitations
We were unable to account for emergency department psychiatric services in our models, although we did account for teaching hospital status, where most psychiatric teams would be located. In addition, we did not collect data for patients escorted by police, which could affect wait times (police are not permitted to leave before the patient has been seen by a physician). Length-of-stay is not a perfect measure of crowding in the emergency department, but it is as accurate as more complex measures.8
Wait times were missing for many patients: 20.8% of patients were missing data for time to physician assessment and 10.2% were missing data for admission decision to ward transfer. This is unavoidable when using databases that contain data for several million people; however, the data were missing from the outcome variable, with less than 1% missing data from the model covariates, thus complete case analysis is satisfactory.18
The ICD-10 coding has not been validated for patients with a mental illness, and coding errors would result in misclassification bias, which could dilute the strength of our findings. We excluded patients with diagnoses of anxiety and stress-related disorders because the ICD-10 coding may be poor. It is possible that these patients wait longer to be assessed by a physician, and inclusion of these patients might alter our results.
Because we used only index visits in our analyses, we measured wait times by individual patient; if the analysis were performed by emergency department visit, the results might be different. Many patients with mental illness visit the emergency department often and may wait longer if staff familiar with them feel that they are safe to wait. Alternatively, these patients may be seen more quickly because the physician can efficiently address the patient’s complaint using previous management approaches.
Conclusion
Patients in Ontario with mental illness waited slightly longer to see a physician than other patients when the emergency department was not crowded, specifically patients who were given a high priority triage score. Other indicators, such as time to receive a hospital bed and triage categorization, also suggest that these patients do not receive slower care. The wait times for patients with mental illness will likely improve with the overall Emergency Room Wait Time Strategy and with similar strategies implemented in other provinces and regions.
Acknowledgements
Clare Atzema was supported by the Practice Plan of the Department of Emergency Services at Sunnybrook Health Sciences, the Department of Medicine, University of Toronto, and the Sunnybrook Research Institute. Michael Schull was supported by an Applied Chair in Health Services and Policy Research from the Canadian Institutes of Health Research (CIHR), Paul Kurdyak was supported by a New Investigator Award from CIHR, and Peter Austin was supported by a Career Investigator Award from the Heart and Stroke Foundation of Ontario.
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Clare Atzema had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Clare Atzema, Michael Schull, Paul Kurdyak, Andrew Wilton and Marian Vermuelan were involved in study concept and design. Clare Atzema acquired the data. Clare Atzema, Peter Austin and Andrew Wilton performed the statistical analysis. Clare Atzema, Peter Austin, Andrew Wilton, Michael Schull, Marian Vermuelan and Natasja Menezes analyzed and interpreted the data. Clare Atzema drafted the manuscript, which was critically revised for important intellectual content by all other authors. All authors approved of the final version of the manuscript submitted for publication.
Funding: This project was supported in part by a Dean’s Fund Award from the University of Toronto. The University of Toronto had no involvement in the design or conduct of the study, data management or analysis, or manuscript preparation, review, or authorization for submission. This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
References
- 1.Ministry of Health and Long Term Care Ontario targets shorter ER times. Toronto (ON): The Ministry; 2009. Available: http://news.ontario.ca/mohltc/en/2009/02/ontario-targets-shorterer-times.html (accessed 2012 Oct. 31). [Google Scholar]
- 2.Schizophrenia Society of Ontario Reducing emergency room wait times for people in psychiatric distress: recommendations from the Schizophrenia Society of Ontario. Toronto (ON): The Society; 2008. Available: www.schizophrenia.on.ca/images/stories/sso_er_paper_final_oct_20_2008.pdf (accessed 2012 Oct. 31). [Google Scholar]
- 3.Beveridge R, Clarke B, Janes L, et al. Implementation Guidelines for The Canadian Emergency Department Triage & Acuity Scale (CTAS). 1998. Available: http://caep.ca/sites/default/files/caep/files/ctased16.pdf (accessed 2012 Oct. 31).
- 4.Kirby MJL, Keon WJ. Out of the shadows at last: transforming mental health, mental illness and addiction services in Canada. Ottawa (ON): Parliament of Canada; 2006. Available: www.parl.gc.ca/39/1/parlbus/commbus/senate/com-e/soci-e/rep-e/rep02may06-e.htm (accessed 2012 Oct. 31). [Google Scholar]
- 5.Atzema CL, Schull MJ, Tu JV. The effect of a charted history of depression on emergency department triage and outcomes in patients with acute myocardial infarction. CMAJ 2011;183:663–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fibrinolytic Therapy Trialists’ (FTT) Collaborative Group Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Lancet 1994;343:311–22 [PubMed] [Google Scholar]
- 7.Bullard MJ, Unger B, Spence J, et al. Revisions to the Canadian Emergency Department Triage Acuity Scale (CTAS) adult guidelines. CJEM 2008;10:136–42 [DOI] [PubMed] [Google Scholar]
- 8.Hwang U, McCarthy ML, Aronsky D, et al. Measures of crowding in the emergency department: a systematic review. Acad Emerg Med 2011;18:527–38 [DOI] [PubMed] [Google Scholar]
- 9.McCarthy ML, Zeger SL, Ding R, et al. Crowding delays treatment and lengthens emergency department length of stay, even among high-acuity patients. Ann Emerg Med 2009;54:492–503 [DOI] [PubMed] [Google Scholar]
- 10.Diercks DB, Roe MT, Chen AY, et al. Prolonged emergency department stays of non-ST-segment-elevation myocardial infarction patients are associated with worse adherence to the American College of Cardiology/American Heart Association guidelines for management and increased adverse events. Ann Emerg Med 2007;50:489–96 [DOI] [PubMed] [Google Scholar]
- 11.Pines JM, Localio AR, Hollander JE, et al. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med 2007;50:510–6 [DOI] [PubMed] [Google Scholar]
- 12.Schull MJ, Kiss A, Szalai JP. The effect of low-complexity patients on emergency department waiting times. Ann Emerg Med 2007;49:257–64, 264.e1 [DOI] [PubMed] [Google Scholar]
- 13.Austin PC, Schull MJ. Quantile regression: a statistical tool for out-of-hospital research. Acad Emerg Med 2003;10:789–97 [DOI] [PubMed] [Google Scholar]
- 14.De Luca G, Suryapranata H, Ottervanger JP, et al. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation 2004;109:1223–5 [DOI] [PubMed] [Google Scholar]
- 15.Bond K, Ospina B, Blitz S, et al. Frequency, determinants, and impact of overcrowding on emergency departments in Canada: a national survey of emergency department directors Healthc Q 2007;10:32–40 [DOI] [PubMed] [Google Scholar]
- 16.Wong HJ, Morra D, Caesar M, et al. Understanding hospital and emergency department congestion: an examination of inpatient admission trends and bed resources. CJEM 2010;12:18–26 [DOI] [PubMed] [Google Scholar]
- 17.Knott JC, Pleban A, Taylor D, et al. Management of mental health patients attending Victorian emergency departments. Aust N Z J Psychiatry 2007;41:759–67 [DOI] [PubMed] [Google Scholar]
- 18.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med 2011;30:377–99 [DOI] [PubMed] [Google Scholar]