Abstract
Aim and Objective:
The present study is undertaken to study the ultra structural features of muscle tissue in moderate and advanced stages of oral submucous fibrosis along with retrospective analysis of 80 cases of oral submucous fibrosis ( osmf) 0 during the period of year 2002 to 2005.
Materials and Methods:
Five patients with moderate and advanced stages of osmf0 were screened from outpatients department of oral diagnosis, sri Ramachandra dental college and hospital. After a detailed case history, they were subjected to incisional biopsy from an area of buccal mucosa with maximum palpable fibrotic bands.the specimens were cut into two halves, one half was fixed in 10% formalin for routine processing. Second half was fixed in 2.5% glutaraldehyde for electron microscopic examination.
Results:
Prospective study of muscle fibres from moderate and advanced stages of osmf0 revealed varying changes in high proportion of muscle fibres which includes, irregularity of surface of fibre,sarcolemmal foldings, reduplicated basement membrane, loss and alterations in the myofilaments, hypercontraction of myofibrils, Z line abnormalities, internal nucleus, autophagic vacuoles. These features are suggestive of muscle atrophy and necrosis.
Conclusion:
Within the limitations of this study, it can be concluded that the ultra structural features In moderate and advanced stages of osmf0 were best studied. These muscle changes can be manifestation of disease, atrophy being secondary to the limited functional activity of the muscles which is brought about by fibrosis or it could be essential part of the disease process itself.
Keywords: Atrophy, necrosis, sarcolemma, autophagic vacuoles, internal nucleus
INTRODUCTION
Oral submucous fibrosis is a chronic disease of insidious onset of unknown etiology affecting the oral and oropharyngeal region characterized by progressive fibrosis of oral submucous. The connective tissue change of oral submucous fibrosis is characterized by deposition of dense collagen fibers in oral mucosa, which develops a hyalinized appearance in moderately and advanced stages of disease. It shows fragmentation and elastic degeneration of collagen.[1–4]
Only few studies regarding morphological changes in muscle cells either at light microscope or electron microscope levels have been carried out. Thus the purpose of the present study is to find out whether collagen accumulation along with muscle degeneration plays a role in the reduced mouth opening in oral submucous fibrosis. This study is exclusively restricted to morphological changes in muscle tissues in oral sub mucous fibrosis along with retrospective analysis of 80 cases of oral submucous fibrosis. Recently revolutionized electron microscope makes it an ever more powerful tool to study the muscle status in oral submucous fibrosis.
MATERIALS AND METHODS
A retrospective study of 80 cases of oral submucous fibrosis (OSMF) that were retrieved from the files of the department of oral pathology, Sri Ramachandra Dental College, Chennai from the year 2002-2005 and parameters including age, sex, habits, clinical features were taken into consideration. A prospective study of 5 patients who had restricted mouth opening where chosen for ultra microscopic examination of muscle statues in moderately and advanced stages of OSMF.
A detailed case history highlighting their habits, complaints and chief clinical features were recorded. Incisional biopsy was taken from an area of buccal mucosa with maximum palpable fibrotic bands. All the biopsy specimens were deep enough (1 cm) to include muscle in it. The biopsy specimens were cut into two halves, one half was immediately fixed in 10% formalin and was sent for processing and paraffin embedded. Sections 4-5 micron thick were cut and routinely stained with hematoxylin and eosin.
The second half of the biopsy specimen were cut into slices of appropriate size (1 mm) for electron microscopic examination and fixed in 2.5% glutaraldehyde followed by osmiumtetroxide. Two healthy patients were also included in electron microscope study for morphological comparison of normal muscle with that of muscle changes in oral submucous fibrosis
RESULTS
Retrospective study of OSMF
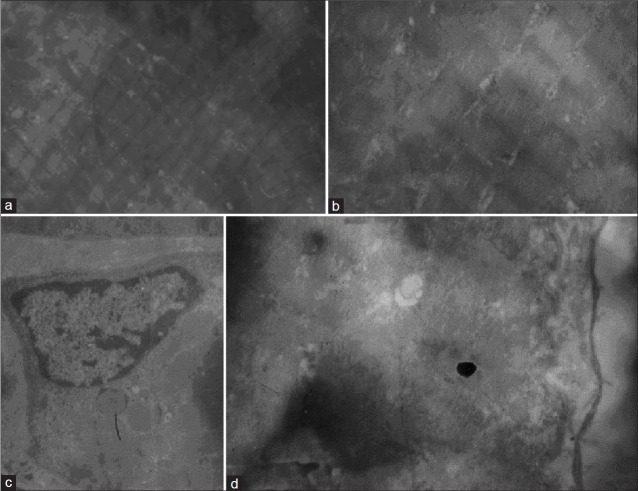
Retrospective study revealed a male predilection of OSMF ratio being 4.3:1. Maximum number of cases in the study was recorded between the age of 20-29 [Charts 1 and 2]. No case was recorded above 70 years. The site of predilection was buccal mucosa followed by retromolar area, labial mucosa, tongue, soft palate and floor of the mouth [Chart 3]. Muscle changes were invariably seen in approximately 90% [Chart 4] of the histopathological sections. Some showed loss of normal striation pattern and accumulation of homogenous eosinophilic material [Figure 1a]. Fibres disintegrate into flocculent collection of eosinophilic material indicating degeneration was also seen [Figure 1b].
Chart 1.
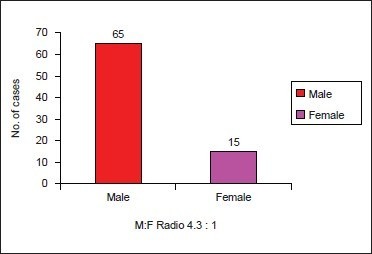
Sex distribution
Chart 2.
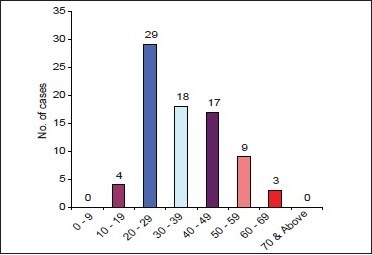
Age distribution of OSMF
Chart 3.
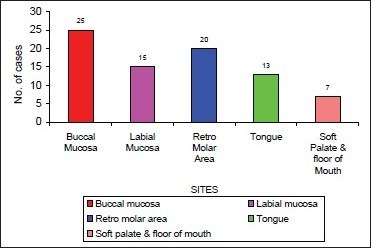
Common site in oral cavity
Chart 4.
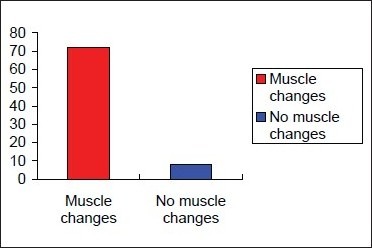
Presence of muscle change
Figure 1.
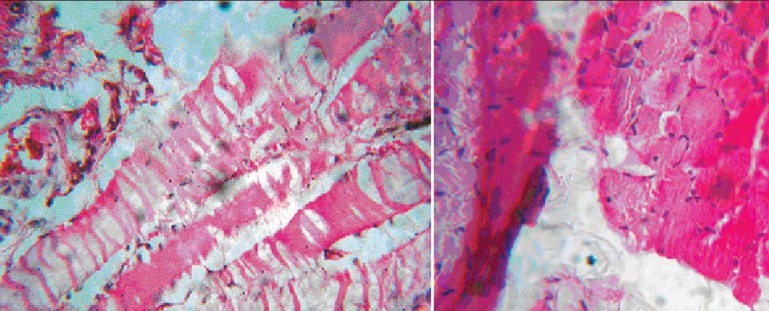
(a) Loss of striation in muscle; (b) Floculant material showing degeneration
EM features observed
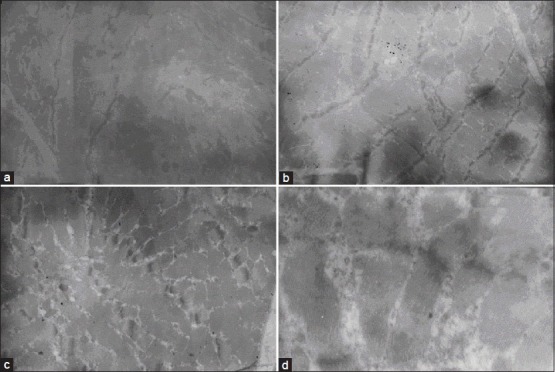
The EM study was exclusively restricted to muscle status of the specimen. Examination of tissues from patients with no evidence of restricted mouth opening showed majority of muscle fibres which appeared normal. These fibres showed no ultra structural changes in rest of their cytoplasmic organelles and their nuclei appeared normal. Normal muscles showed major components of each fibre in longitudinal section. Sarcomere and myofibrils with clear striation patterns of A and I bands and Z lines was observed [Figures 2a and b]. Nucleus beneath the plasma membrane of sarcolemma and basement membrane external to plasma membrane was also seen [Figure 2c].
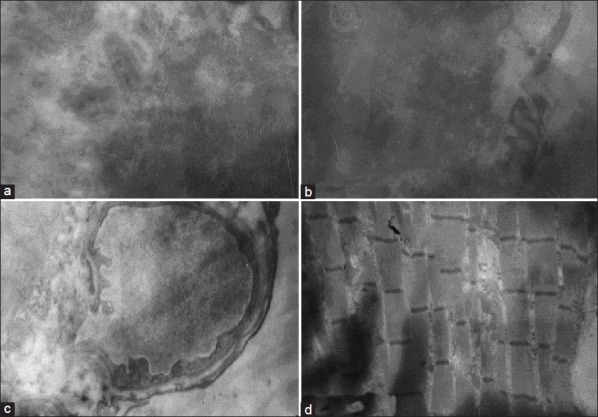
Figure 2.
(a) Em showing normal muscle showing sarcomer; (b) Higher magnification of normal muscle; (c) Nucles benath plasma membrane; (d) Folding on the surface of sarcolemma
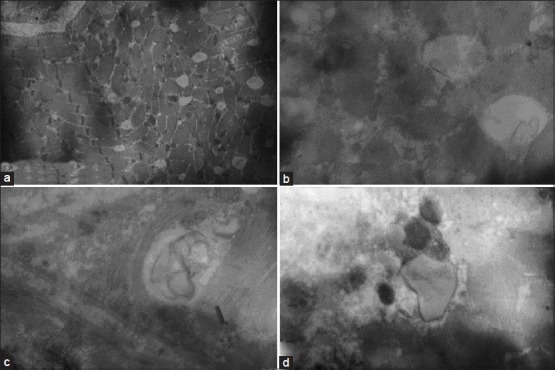
The following ultra structural features were identified in the tissues from patients with moderately and advanced stages of oral submucous fibrosis. A common feature was irregularity of the surface of the fibre showing foldings of sarcolemma, which indicates atrophy. The sarcolemma showed villa like folds into extracellular space [Figure 3a]. Replicated basement membrane suggestive of atrophy was also evident [Figure 3b]. Thickened basement membrane of capillary was present adjacent to muscle fibers showing pathological changes [Figure 3c]. Loss and alterations in the myofilaments were observed. Myofilaments loss involving both focal area and whole of the fibre were identified. This change caused narrowing of the myofibrils and excessive splitting of the bundles [Figure 3d]. The space between the myofibrillar loss were occupied by sarcoplasmic components like mitochondria, homogenous substance (may be glycogen). Replaced mitochondria showed variation in shapes and size [Figure 4a]. Hyper contraction of myofibrils was evident in few areas. It involved both focal and wide spread areas indicating early stage of necrosis [Figure 4b]. The characteristic myofilament structure is lost completely and replaced by amorphous granular material in few fibres suggesting the late stages of necrosis [Figure 4c]. Selective loss or abnormalities of particular regions of the sarcomere was present. Z line abnormalities like thickening of Z line and irregular Z lines [Figure 4d], Z line streaming and complete loss of Z lines [Figure 5a] were observed.
Figure 3.
(a) Villa like fold into extracellular space; (b) Replicated basement membrane; (c) Blood capillary in muscle showing thickened basement membrane; (d) Loss of myofilaments
Figure 4.
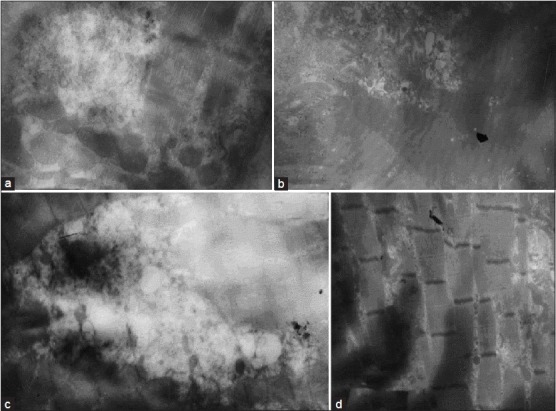
(a) Loss of myofilament structures; (b) Hyper contraction of myofibrils; (c) Showing amorphous granular material; (d) Showing z line abnormalities
Figure 5.
(a) Complete loss of Z line; (b) Myofibrills with irregular striations; (c) Complete loss of normal striation and haphazardly arranged fibres; (d) Higher magnification showing complete loss of normal striation and haphazardly arranged fibres
Myofibrils undergoing varying degrees of disorganization, disorientation and disruption were identified. Some fibres showed loss of normal striation and some showed haphazardly arranged fibres with still identifiable sarcomere. Internal nucleus was also seen in between the myofibrils indicating the pathological changes of the muscle [Figures 5b–d]. In spite of severe degenerative changes seen in the muscle fibres of these patients, macrophages were rarely found. Numerous of fibres showed vacuolated appearance. These vacuoles are interpreted to be autophagic vacuoles [Figure 6a]. Autophagy involves isolation of a portion of the fibre by a membrane and digestion of the contents by acid hydrolases. The morphology of the remaining debris or residual bodies was variable and was dense, membranous, vesicular or granular [Figure 6b]. The vacuole contained some granular material in it, probably phagocytosed muscle fibre [Figures 6c and d].
Figure 6.
(a) Fibres showing vacuolated appearance; (b) Higher magnification showing vacuolated appearance; (c) Mictograph showing autophagic vacuoles containing dense, vesicular material and membranous; (d) Vacuole showing dense material
DISCUSSION
OSMF is a chronic debilitating disease which largely affects people on the Indian subcontinent and South East Asia. Since its association with oral epithelial dysplasia and cancer, OSMF is considered to be a premalignant condition.[5] Our study showed male predilection in contrast to study carried out by Pindborg et al. In addition none of their cases were below the age of 20 years. In our study, there were few cases below the age 20 and also disease was prevalent in the age group of 20-29 years. Study by AZIZ (1997)[6] showed most patients are aged 45-54. This is consistent with the result observed by Pindborg et al.
Study by Mani and Singh[7] on the connective tissue changes showed marked increase in the collagen deposition with increasing clinical severity of OSMF indicating this may be the basic tissue change and often a variable infiltration of lamina propria with chronic inflammatory cells. In our study, increased deposition and hyalinization of collagen bundles was invariably seen in all the patients. Morphological changes in muscle cells either at light or ultra structural levels have not been demonstrated in OSMF. However, Advani[8] reported involvement of the muscles in the fibrosis process and presented illustration showing replacement of the muscle by fibrous tissue. Binnie and Cawson[9] also stated that the characteristic features of OSMF under light microscope was a homogenous, collagenous subepithelial zone in which degenerating muscle fibres could be seen. Similarly in our study almost 72 cases, out of 80 (90%) showed muscle changes in varying stages of degeneration.
Small, angular fibres are indicative of initial phase of atrophy that was observed in our study. Swollen muscle fibre with no cross striations and filled with a homogeneous eosinophilic material is called as hyaline degeneration.[10] This feature was noted in significant number of cases in our study. Ibres disintegrate into floccular collections of eosinophilic material.[10]
Transmission electron microscope study of 5 patients with OSMF was carried out to confirm the muscle changes observed under LM and all the 5 patients included in study were diagnosed moderate or severe clinically. Control sections showed normal muscle fibre with plasma membrane and basement membrane. The myofibrils showed a clear striation pattern of A and I bands and Z lines. Mitochondria, lipid and glycogen were present between the myofibrils.
Ultra structural findings of muscle degeneration in OSMF was carried out by Labban and Caniff[11] in which the control muscle fibres showed compression of sarcomeres and accumulation of homogenous material adjacent to it. This feature was not observed in our study. The control muscle showed absolute normal appearance.
In our study an array of findings were observed in muscle tissue of almost all the 5 OSMF patients included in the study, which showed varying degrees of muscle changes including atrophy, degeneration and necrosis of fibres. A common feature of atrophy is irregularity of the surface of the fibre and foldings of sarcolemma. This finding was observed in our study indicating that muscle fibres in OSMF undergo atrophy. Along with this, replicated basement membrane was also identified in our study which signifies the atrophic change again. Labbon and Canniff[11] study showed blood vessels with widely dilated often with an attenuated endothelial lining. Our study showed blood vessels with thickened capillary basement membrane. This feature is observed in the rheumatoid arthritis.[12] Significance of this feature in OSMF is yet to be investigated. Loss and alteration in the myofilaments are the most common abnormalities observed in diseased muscle.[13] The degree of disruption and loss is variable depending on the severity of the disease process. Both focal and widespread loss of myofilaments was observed in our study. Focal loss of myofilaments and some areas showing narrowing and splitting of myofibrils were present. These areas of focal loss of myofibrils were replaced by mitochondria and other sarcoplasmic components including glycogen. The mitochondria were varying in their shapes and size.
Earlier stages of necrosis are thought to involve the hyper contraction or over contraction of myofibrils. The areas affected by hyper contraction may be focal or extensive. Both focal and extensive areas of hyper contraction were observed in our study. Band of very much contracted myofibrils and sarcomeres were seen in many sections indicating earlier stages of necrosis. The characteristic myofilament structure is lost completely and replaced by amorphous granular material. These fibres correspond to the pale disrupted fibres seen in histological and histochemical techniques and this appearance is thought to be the end stages of series of events leading to necrosis. This feature was present in our study, showing both focal and complete loss of myofilaments and myofibrils and replaced amorphous material suggesting end stages of necrosis. This is consistent with the features observed in severely necrotic fibres by Cullen and Fulthorpe (1975).[14]
Selective loss or abnormalities of particular regions of the sarcomere may also occur in diseased muscle. Z lines abnormalities like irregular Z line, thickening of Z lines, Z line streaming, Z line loss were observed in our study. Z line streaming was common structural alteration associated with myofibrilar damage.[15]
Complete loss of striations and banding pattern was evident in some sections showing disoriented and haphazardly arranged fibres. Such banding pattern loss is seen in Duchenne muscular dystrophy. Changes in muscle nuclei is a vital sign indicating pathological change in the fibre.[13] Accordingly, in our study, internal nuclei was observed in a central location of the fibres showing myofibrilar loss and disorientation. Primary lysosomes are difficult to identify in skeletal muscle but features associated with their activity can be seen in a variety of structures where myofibre destruction occurs. These include autophagic vacuoles. Many sections in our study showed vacuolated appearance of muscle fibre.
Higher magnified view of these vacuoles showed clear membrane bound vacuole containing some dense, membraneous, granular material (may be phagocytosed fibre). These structures are called Autophagic vacuoles.[13] Autophagy involves isolation of a portion of the fibre by a membrane and digestion of the contents by acid hydrolases. The morphological changes observed in muscle fibres from patients with restricted mouth opening appear to be progressive and probably lead to muscle fibre necrosis. This is confirmed by the finding of large number of muscle fibre in various stages of degeneration and necrosis.
Animal experiment and observation of diseased human muscle fibres suggest that at least two cellular mechanisms lead to necrosis.[16] One of these is characterized by localized defects of the plasma membrane and other involves formation of autophagic vacuoles. Both these changes are evident in our study. However, the final stages of both the processes are identical, the plasma membrane of the fibre vanishes within the necrotic segment and myofilaments disintegrate into a fine granular substance.[17] Extensive muscle damage in OSMF shows that restricted mouth opening would appear to depend not only on subepithelial fibrosis but also on the extent of muscle damage, as extensive degeneration appears to be the most prominent feature observed in our study. Thus the muscle fibres showing changes such as degeneration and necrosis also play a role along with subepithelial fibrosis in pathogenesis of the disease which is seen clinically as trismus in OSMF.
SUMMARY AND CONCLUSION
OSMF is regarded as a disease of collagen metabolic disorder showing increased collagen production along with decreased collagen degradation. Our study showed apart from increased collagen accumulation there was increased extent of muscle damage too. This muscle changes can be a manifestation of disease, atrophy being secondary to the limited functional activity of the muscles which is brought about by fibrosis or whether it is an essential part of the diseases process itself. Thus, understanding these events will help in better therapeutic intervention of the disease in future. Is there any possible intervention that could be aimed at treating the muscle damage along with fibrosis, since restricted mouth opening not only depends on subepithelial fibrosis but also on the extent of muscle damage and if implemented would there be any positive significance in the prognosis. This question has to be answered through further researches.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Desa JV. Submucous fibrosis of the palate and cheek. Ann Otol Rhinol Laryngol. 1957;66:1143–59. doi: 10.1177/000348945706600420. [DOI] [PubMed] [Google Scholar]
- 2.Sirsat SM, Khanolkar VR. Histological, electron microscope and enzyme studies of submucous fibrosis of the palate. J Pathol Bacteriol. 1960;79:53–8. doi: 10.1002/path.1700790107. [DOI] [PubMed] [Google Scholar]
- 3.Sharan J. Histopathological observations on cases of submucous fibrosis of the oral cavity. Indian J Pathol Microbiol. 1959;2:150. [Google Scholar]
- 4.Shieh TY, Yang JF. Collagenase activity in oral submucous fibrosis. Proc Natl Sci Counc Repub China B. 1992;16:106–10. [PubMed] [Google Scholar]
- 5.PindBorg JJ. Is SMF a precancerous condition oral cavity? Ind J Dent. 1972;22:474. [PubMed] [Google Scholar]
- 6.Aziz SR. Oral submucous fibrosis: An unusual disease. J N J Dent Assoc. 1997;68:17–9. [PubMed] [Google Scholar]
- 7.Mani NJ. Studies on oral submucous fibrosis. IV. Connective tissue changes. J Oral Med. 1977;32:70–4. [PubMed] [Google Scholar]
- 8.Advani DG. MDS thesis. University of Bombay; 1982. Histopathological studies before and after kepacort in Oral submucous fibrosis; p. 83. [Google Scholar]
- 9.Binnie WH, Cawson RA. A new ultra structural finding in oral submuscous fibrosis. Br J Dermatol. 1972;86:286–90. doi: 10.1111/j.1365-2133.1972.tb02230.x. [DOI] [PubMed] [Google Scholar]
- 10.Bethlem J. Introduction and Atlas. Amsterdam – London: North- Holland Publishing Company; 1970. Muscle Pathology. [Google Scholar]
- 11.El Labban NG, Canniff JP. Ultra structural findings of muscle degeneration in oral submucous fibrosis. J Oral Pathol. 1985;14:709–17. doi: 10.1111/j.1600-0714.1985.tb00550.x. [DOI] [PubMed] [Google Scholar]
- 12.Stephens HR, Duance VC, Dunn MJ, Bailey AJ, Dubowitz V. Collagen types in neuromuscular diseases. J Neurol Sci. 1982;53:45–62. doi: 10.1016/0022-510x(82)90079-x. [DOI] [PubMed] [Google Scholar]
- 13.Dubowitz V. 2nd ed. London: Bailliere Tindall; 1985. Muscle Biopsy- A practical approach. [Google Scholar]
- 14.Cullen MJ, Fulthorpe JJ. Stages in fibre breakdown in Duchenne muscular dystrophy. An electron microscopic study. J Neurol Sci. 1975;24:179–200. doi: 10.1016/0022-510x(75)90232-4. [DOI] [PubMed] [Google Scholar]
- 15.Cullen MJ, Fullthorpe JJ. Phagocytosis of the A band following Z line and I band loss. Its significance in skeletal muscle breakdown. J Pathol. 1982;138:129–43. doi: 10.1002/path.1711380204. [DOI] [PubMed] [Google Scholar]
- 16.Schmalbruch H. The muscular dystrophies. In: Mastaglia FL, Walton J, editors. Skeletal muscle pathology. London: Churchill Livingstone; 1982. p. 238. [Google Scholar]
- 17.Milhorat AT, Shafiq SA, Goldstone L. Changes in muscle structures in dystrophic patients, carries and normal siblings seen by electron microcopy; correlation with levels of serum creatinephosphokinase (CPK) Ann N Y Acad Sci. 1966;138:246–92. doi: 10.1111/j.1749-6632.1966.tb41170.x. [DOI] [PubMed] [Google Scholar]