Abstract
Background:
The diagnosis of oral malignancy and epithelial dysplasia has traditionally been based upon histopathological evaluation of full thickness biopsy from lesional tissue. As many studies had shown that incisional biopsy could cause progression of the tumors, many alternative methods of collection of samples had been tested. Oral brush biopsy is a transepithelial biopsy where it collects cells from basal cell layer noninvasively.
Aim:
To assess the diagnostic accuracy of brush biopsy when compared to histopathology in a group of patients with features of potentially malignancy.
Materials and Methods:
In the present study, 60 cases of clinically diagnosed leukoplakia are selected and subjected to histopathology and brush biopsy.
Results and Conclusion:
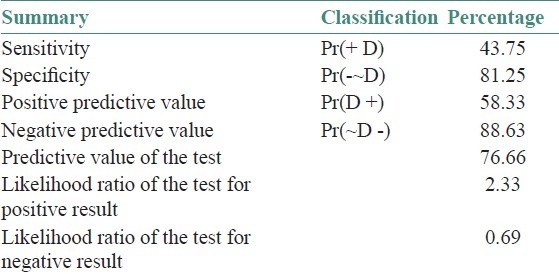
Results showed that of 16 dysplasia cases confirmed by histopathology, only 12 were positively reported in oral brush biopsy. In 44 cases, the reports are same for histopathology and brush biopsy. The sensitivity of oral brush biopsy is 43.5% and specificity is 81.25% with a positive predictive value of 58.3%. Oral brush biopsy with molecular markers like tenascin and keratins can be an accurate diagnostic test.
Keywords: Brush biopsy, leukoplakia, sensitivity, specificity
INTRODUCTION
Detection of cancer in the early asymptomatic stage improves the cure rates and quality of life of the patient by minimizing extensive, debilitating treatments and can be conservatively managed with minimal surgical morbidity and 100% survival.[1] Early cancerous lesions are asymptomatic and vary in clinical presentations as they do not have ulcerations, indurations, elevations, bleeding, and cervical adenopathy as in case of advanced cancers.[1]
The significance of evaluation of leukoplakic lesions, which is the most common precursor of oral cancer, aids in prognostic implications. Leukoplakia has varied clinical appearance without any symptoms. But, it may show severe dysplasia, carcinoma in-situ, or frank carcinoma. The cytological examination had failed to diagnose cases of dysplasia or malignancy accurately as that of the histopathology. In the oral cavity, the cytology has been of limited use due to the superficial cells collected and the keratin layer that is present. As a result, deeper epithelial abnormalities are not detected.[2] In earlier days, cotton swabs were used for collection of smears and this was followed by sponge, wooden, or metal spatulas, where only superficial layer cells are collected.[3]
The basis for development of newer techniques for collection of cells is, dysplasia starts in basal layers (stratum germinatum) and extends to all the layers of the epithelium.[4] In order to collect the basal layer cells in a new transepithelial, noninvasive technique was developed by the Oral CDx laboratories. In this technique, the smears obtained contain cells from all the layers of the epithelium and has improved diagnostic applications for mass screening campaigns, without the need for surgery and surgically trained personnel for taking the biopsy. The concept developed in western countries has been established and its use in South Indian population has not been validated. This confirmatory study intends to validate the use of this novel technology in the study population from South India.
MATERIALS AND METHODS
The present study is done on 60 patients who are referred to the outpatient Department of SIBAR Institute of Dental Sciences between June 2008 and June 2010, with clinical diagnosis suggestive of oral leukoplakia.
The criteria of inclusion were as follows:
Diagnosing the oral lesions clinically as leukoplakia by proper case history and clinical examination.
Patients are treated for 1-2 weeks with antifungal and antibiotics to rule out other lesions or infections.
All the lesions selected are more than 1 cm in size.
No patients with obvious symptoms of pain or swelling are included in the study.
First, the lesion is brush biopsied according to the manufacturer's guidelines and then scalpel biopsy was performed. All the specimens are formalin-fixed, processed in graded alcohols, and stained with hematoxylin and eosin stains. Patient information form is filled and mailed to Oral CDx India Ltd., Mumbai, for computer evaluation by neural network-based image processing system, specifically designed to detect oral precancerous and cancerous cells.
The Results of Oral CDx were classified into the following four categories:
Negative - No epithelial abnormality.
Atypical - Abnormal epithelial changes of uncertain diagnostic significance.
Positive - Definitive cellular evidence of epithelial dysplasia or carcinoma.
Inadequate - Incomplete transepithelial biopsy specimen.
The histopathological grading of dysplasia is according to 2005 WHO.[5] Modified classification, where two grades are given. They are as follows:
No/questionable/mild - Low risk.
Moderate/severe - High risk.
The gender, age, and demographics including site, habits were collected from the case history. The clinical, histopathological, and Oral CDx was obtained. Descriptive statistics are presented for the variables. 2 × 2 table was used to calculate the sensitivity and specificity of the diagnostic tests.
RESULTS
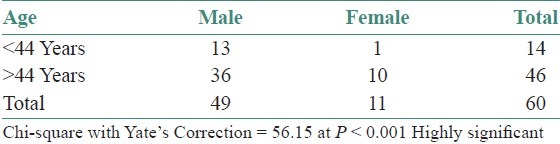
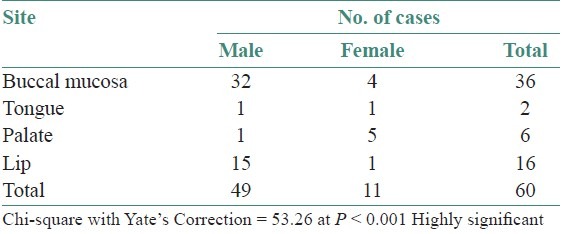
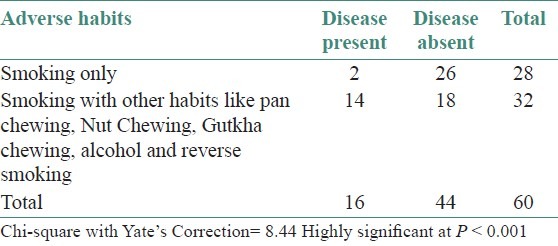
The study group consisted of 60 cases, of which 49 were males and 11 were female patients [Table 1]. The age of the patients ranged from 29 to 70 years with mean average age of 48.9 years. Most of the cases fall in the age group of third and fourth decades of life (P < 0.001) [Table 2 and Graph 1]. The common sites of occurrence of the lesion in this study were buccal mucosa in 36 cases. Lip (16), palate (6), and Tongue (2) were sites of predilection for other cases [Table 3 and Graph 2]. In the present study, tobacco smoking is present in all the cases and reverse smoking with chuttas were seen in three female patients only. Other habits like alcohol intake, pan chewing, and betel nut chewing along with tobacco smoking is seen in 32 cases [Table 4]. In the present study group, the clinical diagnosis was homogenous leukoplakia (43 cases), homogenous and erythematous leukoplakia (3 cases), and speckled leukoplakia (14 cases).
Table 1.
Gender distribution of study subjects
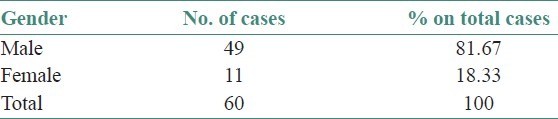
Table 2.
Age distribution of study subjects
Graph 1.
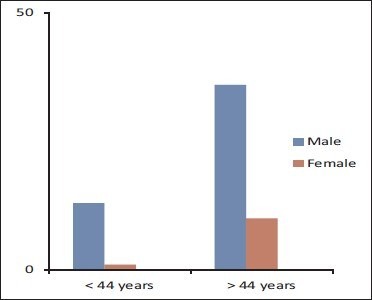
Age wise distribution of study subjects
Table 3.
Distribution of study subjects by site of occurrence
Graph 2.
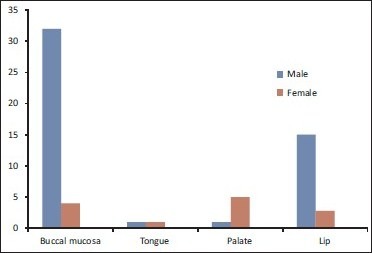
Distribution of study subjects by site of occurrence
Table 4.
Correlation of adverse habits with disease
The Results showed that 16 cases were positive for dysplasia in histopathology. Of the 16 cases, two cases showed well-differentiated squamous cell carcinoma and in 14 cases hyperorthokeratosis with mild dysplasia. The Results obtained by brush biopsy revealed 12 cases with abnormal cells. Two cases of 12 abnormal oral brush biopsy cases showed positive cells for dysplasia or carcinoma [Table 5]. Two cases which were reported as well-differentiated squamous cell carcinomas in histopathology had been reported as positive for carcinoma in oral brush biopsy. The histopathological reports and brush biopsy reports were similar in 44 cases.
Table 5.
Comparison of the oral brush biopsy test with histopathology
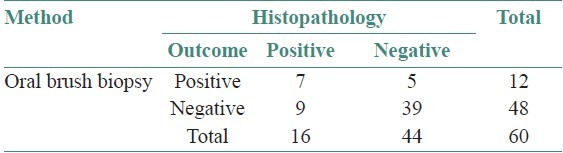
Of 14 cases with hyperorthokeratosis and mild dysplasia in histopathology, only ten cases had been reported as atypical cells present in brush biopsy. Four positive cases for dysplasia in histopathology were reported negative for dysplasia in oral brush biopsy. The sensitivity of oral brush biopsy is 43.5% and specificity is 81.25% with a positive predictive value of 58.3% [Table 6].
Table 6.
Showing the sensitivity, specificity, and PPD values
DISCUSSION
The subtle clinical features of pre-cancer and early oral cancers are difficult to diagnose and hinder their recognition. The pre-cancerous and early cancerous lesions are asymptomatic. Studies showed that more than 25% of dentists failed to recognize the true nature of innocuous looking but potentially malignant lesions.[6]
Deeper epithelial abnormalities often went undetected due to the cytological technique and thickness of the keratin layer often present in the lesional areas.[2] In India, on the other hand, oral cancer represents a major health problem constituting up to 40% of all cancers and is the most prevalent cancer in males and the third most prevalent in females.[7] At the screening centers, it is difficult to do scalpel biopsy for each lesion, because of the lack of specialist services or due to patients’ compliance.
The transepithelial brush biopsy technique was designed to address this deficiency which allows harvesting the cells from both superficial and deep regions of epithelium. This minimally invasive technique can be used as chair side test to assess the benign looking lesions. The purported benefits would then include adequate sampling via a minimally invasive procedure.[8]
Dysplasia and early carcinomas are asymptomatic and commonly misinterpreted as benign lesions or innocuous oral problems. The inconspicuous nature of these lesions or misleading perception of practitioners may primarily be responsible for the advanced stages of these tumors at the time of discovery.[6] Leukoplakia is a potential malignant lesion which should be followed periodically both by clinical examination and biopsy. There is statistically significant difference between smokers’ and non-smokers’ in keratinization of the oral cavity.[9]
In the present study, an interesting feature is, the patients were unaware of the white lesions as they were asymptomatic. They were diagnosed as leukoplakic lesions at the time of screening. The history revealed habit of smoking for longer duration ranging from 8 to 45 years with frequency of 10 to 15 smokes per day. Smoking of tobacco is seen in all the cases and some cases had habit of betel nut chewing, pan chewing, and alcohol intake along with smoking of tobacco, as seen in many studies.[10]
In the studies done by Sciubba et al., Christian et al., Poatea et al., and Scheifele et al., the site of predilection for leukoplakia is buccal mucosa.[8,10–12] The most common site for occurrence of leukoplakia is also buccal mucosa in the present study. There are 36 cases in the study group with buccal mucosa involvement. The age of the study group ranged from 29 to 70 years with mean average age 48.9 years. The other studies also showed that the mean average age is fourth and fifth decades of life.[4,10]
In the present study, only clinically diagnosed oral leukoplakia were included. Till date, the studies conducted are biased as the lesions at the time of screening were not subjected to both brush biopsy and scalpel biopsy. In the present study, we had performed both oral brush biopsy and scalpel biopsy. Earlier studies included lesions with obvious symptoms, i.e. class I patients[4] or performed incisional biopsy when there is abnormal brush biopsy.[11,12]
Comparison of the histopathological reports with the brush biopsy reports revealed that they are similar in 44 cases in the study group. Four cases with mild dysplasia histopathologically had been reported as negative for dysplasia in oral brush biopsy. As our data show, it is conceivable that the false-negative rate is significantly higher than reported (4 of 60 cases).
In the previous study done by Sciubba in 1999, the analysis should be considered as incomplete because 517 of the 699 negative brush samples (73.9%) were not followed with definitive incisional biopsy for diagnostic confirmation. In a study by Svrisky et al. in 2002, of 55 cases of negative brush biopsies, four cases had dysplasia in histopathological examination.[13]
In the present study, the sensitivity and specificity are 43.5% and 81.25%, respectively, with a positive predictive value of 58.3%. The low sensitivity may be due to sample size or performing incisional and brush biopsy of the same lesion which had not been done in other studies.
In a retrospective study done by Poate et al. in 2004 on 112 patients, a sensitivity of 71%, specificity of 32%, and a positive predictive value of 44% were reported. They found 6 of 15 negative brush biopsy cases to have dysplasia or carcinoma present in the scalpel biopsy, underscoring the potential for false negative Results.
Christian in 2002 studied on dentists and dental hygienists comprising of 930 individuals, only the abnormal brush biopsies underwent scalpel biopsy. In their study, the negative brush biopsies were not subjected to the golden standard of scalpel biopsy.
In a study by Scheifele et al. in 2004, the sensitivity and specificity are 61% and 97%, respectively. They had included squamous cell carcinoma and oral lichen planus which skewed the sensitivity, specificity, and positive predictive values to increase.[14]
The noninvasive nature of the Oral CDx system should obviate some of the reluctance of general dental practitioners who may have to undertake the invasive investigation of suspicious lesions and/or perhaps reduce referral of patients for the investigation of disease which are unlikely to be potentially malignant.[4]
Some studies concluded that the oral brush biopsy technique shows promise but before any firm conclusions can be reached, a study needs to be conducted in a sufficient cohort of subjects where both brush biopsy and scalpel biopsy are performed on each participant.[14] This technique may be useful in the non-compliant patient who is unlikely to come back for a follow-up examination or accept an immediate referral to an oral surgeon. Despite the overall uncertainty of this particular technology as an oral cancer diagnostic or case-finding aid, the judicious use of the brush cytology in these scenarios may be clinically useful.
CONCLUSION
This is a hospital-based sample study which does not fully represent the patients of a general practitioner, and this is exactly the target group of Oral CDx. The study may be biased by the fact that only clinically diagnosed leukoplakia were subjected for Oral CDx brush biopsy.
The oral brush biopsy technique surely eliminates the need for surgical procedure in asymptomatic doubtful lesions, but the diagnostic accuracy should be assessed before its use in routine clinical practice. Oral brush biopsy along with advanced markers and cytomorphometric analysis can be future promising aids in non-surgical biopsy for prediction of malignancy with less morbidity. The sensitivity and specificity should be estimated in a large sample, where both brush biopsy and conventional histopathology need to be performed in all red and white lesions.
ACKNOWLEDGMENTS
The authors sincerely thank Dr. V. V. V. Prasad, Senior lecturer, in Department of Preventive and community Medicine, Siddhartha Medical College, for his cooperation in statistical analysis.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Kalmar JR. Advances in the detection and diagnosis of oral precancerous and cancerous lesions. oral Maxillofacial Surg Clin N Am. 2006;18:465–82. doi: 10.1016/j.coms.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 2.Potter TJ, Summerlin DJ, Campbell JH. Oral malignancies associated with negative transepithelial brush biopsy. J Oral Maxillofac Surg. 2003;61:674–7. doi: 10.1053/joms.2003.50136. [DOI] [PubMed] [Google Scholar]
- 3.King OH. Intra oral exfoliative cytology technics. Acta Cytol. 1963;7:327–9. [PubMed] [Google Scholar]
- 4.Sciubba JJ. Improving detection of precancerous and cancerous oral lesions computer-assisted analysis of the oral brush biopsy. J Am Dent Assoc. 1999;30:1445–57. doi: 10.14219/jada.archive.1999.0055. [DOI] [PubMed] [Google Scholar]
- 5.Warnakulasuriya S, Reibel J, Bouquot J, Dabelsteen E. Oral epithelial classification systems: Predictive value, utility, weakness and scope for improvement. J Oral Pathol Med. 2008;37:127–33. doi: 10.1111/j.1600-0714.2007.00584.x. [DOI] [PubMed] [Google Scholar]
- 6.Yellowitz J, Horowitz AM, Goodman HS. Knowledge, opinions and practices of general dentists regarding oral cancer: A pilot survey. J Am Dent Assoc. 1998;129:579–83. doi: 10.14219/jada.archive.1998.0275. [DOI] [PubMed] [Google Scholar]
- 7.Mehrotra R, Singh MK, Pandya S. The use of an oral brush biopsy without computer-assisted analysis in the evaluation of oral lesions: A study of 94 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:246–53. doi: 10.1016/j.tripleo.2008.02.030. [DOI] [PubMed] [Google Scholar]
- 8.Sciubba JJ. Oral cancer and its detection history-taking and the diagnostic phase of management. J Am Dent Assoc. 2001;2:132. [PubMed] [Google Scholar]
- 9.Zimmermann ER, Zimmermann AL. Effects of race, age, smoking habits, oral and systemic disease on oral exfoliative cytology. J Dent Res. 1965;44:627. doi: 10.1177/00220345650440040301. [DOI] [PubMed] [Google Scholar]
- 10.Poatea TW, Buchanana JA, Hodgsona TA, Speightb PM, Barrettb AW, Molesb DR, et al. An audit of the efficacy of the oral brush biopsy technique in a specialist oral medicine unit. Oral Oncol. 2004;40:829–34. doi: 10.1016/j.oraloncology.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Christian DC. Computer-assisted analysis of oral brush biopsies at an oral cancer screening program. J Am Dent Assoc. 2002;133:357–62. doi: 10.14219/jada.archive.2002.0175. [DOI] [PubMed] [Google Scholar]
- 12.Scheifele C, Schmidt-Westhausen AM, Dietrich T, Reichar PA. The sensitivity and specificity of the Oral CDx technique: Evaluation of 103 cases. Oral Oncol. 2004;40:824–8. doi: 10.1016/j.oraloncology.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Svirsky JA, Burns JC, Carpenter WM, Cohen DM, Bhattacharyya I, Fantasia JE, et al. Comparison of computer-assisted brush biopsy Results with follow up scalpel biopsy and histology. gen Dent. 2002;50:500–3. [PubMed] [Google Scholar]
- 14.Lingen MW, Kalmar JR, Karrison T. Critical evaluation of diagnostic aids for the detection of oral cancer. Oral Oncol. 2008;44:10–22. doi: 10.1016/j.oraloncology.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


