Abstract
We describe five cases of verruciform xanthoma (VX). The patients, all males, presented with single warty verrucous lesions of 0.5–2 cm size that had been diagnosed clinically as viral warts (four cases) and leukoplakia (one case). Two patients had the lesion in the oral cavity, two on the genital mucosa, and one on the scrotal skin. Histopathology was diagnostic, with verrucous and papillomatous epidermal hyperplasia with the silhouette of a viral wart but with numerous foamy histiocytes packed in the elongated dermal papillae. Columns of deep parakeratosis and neutrophils in the upper spinous layers, with a dermal plasma cell infiltrate were the other histopathologic findings. Excision of the lesions was curative, without recurrences, in the two patients who had lesions in the oral cavity; follow-up was not available in the cases with genital lesions. VX is an uncommon but distinctive clinicopathologic entity affecting the oral and genital mucosa that may be mistaken for benign, premalignant, and malignant conditions. VX can be diagnosed with certainty only on histopathologic examination.
Keywords: Foam cells, verruciform xanthoma, viral wart
Introduction
What was known?
Verruciform xanthoma in Indian literature has been described in the oral cavity but not from genital skin
Verruciform xanthoma (VX) is an uncommon clinicopathologic entity that primarily affects the oral and genital mucosa. Clinically, it presents as a sessile, papillary, granular, or verrucous lesion that is often mistaken for a viral wart. Collections of numerous foam cells in the elongated dermal papillae is a diagnostic feature of VX.
Shafer,[1] in 1971, described 15 cases of this condition in the oral cavity and coined the term ‘verruciform xanthoma.’ Following this first report, several cases were reported confirming VX as a distinctive clinicopathologic entity that presents clinically as a single verrucous or warty plaque and is characterized histologically by papillomatous epidermal hyperplasia with parakeratosis and the presence of neutrophils in the upper spinous layers. The histologic hallmark of this lesion, however, is the presence of numerous foam cells in the elongated dermal papillae.[2,3]
VX also occurs in nonoral sites and the first report of involvement of an extraoral site (vulva) was by Santa Cruz in 1979.[4] Since then, several reports of VX in nonoral sites, especially on anogenital skin, have appeared in literature.[5–8] VX has a slight male preponderance, with a reported male:female ratio of 1.1: 1.[9]
In this paper we describe five cases of this uncommon entity.
Case Report
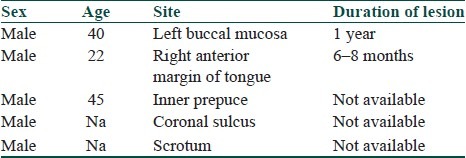
Review of biopsies received in consultation over the past 12 years (1999–2010) revealed five cases [Table 1] that fit in with the clinicopathological diagnosis of VX.
Table 1.
Description of cases
All five cases were in males and presented with single, asymptomatic, verrucous/warty lesions that had gradually grown in size over several months. Two cases occurred in the oral mucosa: One, about 2.5 cm in size, occurred on the left lower buccal mucosa at the level of the 1st and 2nd left molar teeth [Figure 1] and the other on the anterior right margin of the tongue as a raised verrucous papule. Both patients were smokers and case 1 also had history of chewing tobacco for 8 years before presentation. There was no bleeding from the lesions and no history of sensitivity to hot or spicy foods. There was no other relevant medical history. The clinical diagnosis in the first case was leukoplakia, while in the second it was viral wart.
Figure 1.

Verrucous plaque on the left buccal mucosa (case 1)
Cases 3 and 4 developed single flat warty lesions on the penile skin, on the inner prepuce in case 3 and on the dorsum of the penis just proximal to the coronal sulcus in case 4. Case 5 had a single lesion on the scrotal skin. The clinical diagnosis in each of these cases was viral wart. Further clinical details and sexual history was not available for these patients.
Case 1 was screened for serum lipids and all values were found to be within normal limits.
Biopsy findings in all five cases were similar and consisted of papillomatous and digitate epidermal hyperplasia, with some incurving of peripheral rete, giving the overall silhouette of a wart [Figure 2]. The upper spinous layers were infiltrated by several neutrophils that aggregated on the surface of the lesion [Figure 3]. The elongated dermal papillae were stuffed with foamy histiocytes with small central nuclei and abundant finely vacuolated cytoplasm [Figure 4]. Parakeratosis was not evident in all cases but was very prominent in case 2 [Figure 5], with surface and deep invaginations of columns of parakeratosis throughout the hyperplastic epidermis. The base of the exophytic epidermal lesions had moderately dense infiltrates of plasma cells.
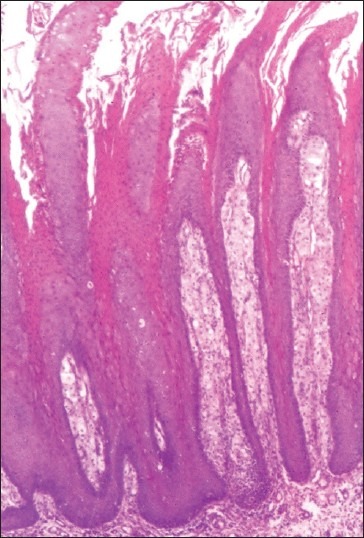
Figure 2.
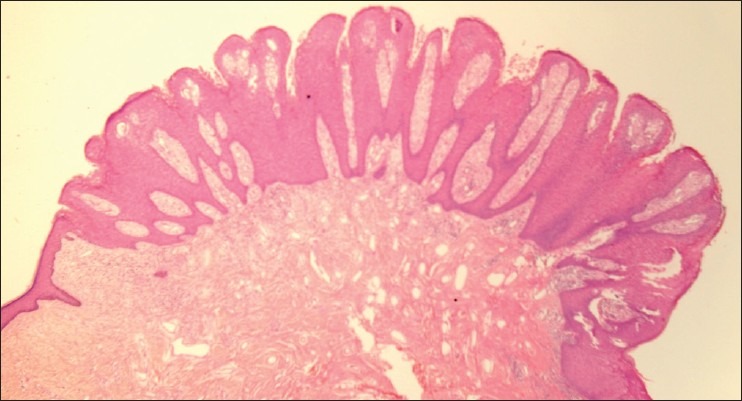
Exophytic papillomatous epidermal hyperplasia with silhouette of wart (H and E; 20×) (case 3)
Figure 3.
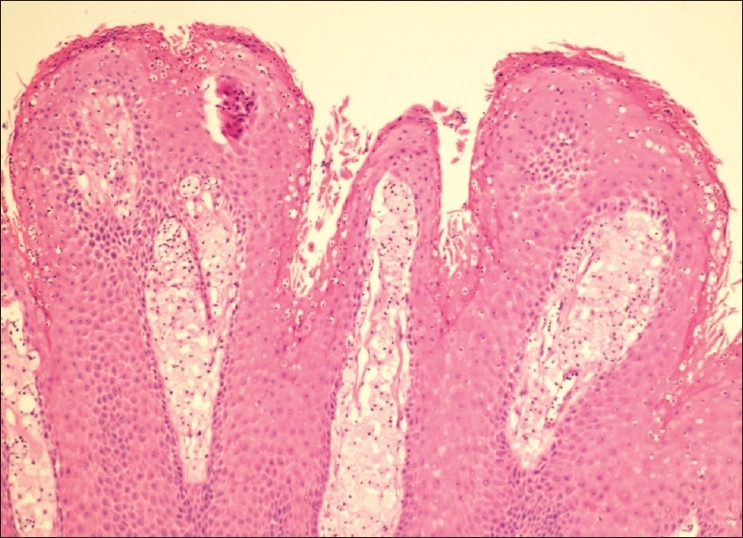
Neutrophils in the upper spinous layers, with foamy histiocytes in the dermal papillae (H and E; 100×) (case 3)
Figure 4.
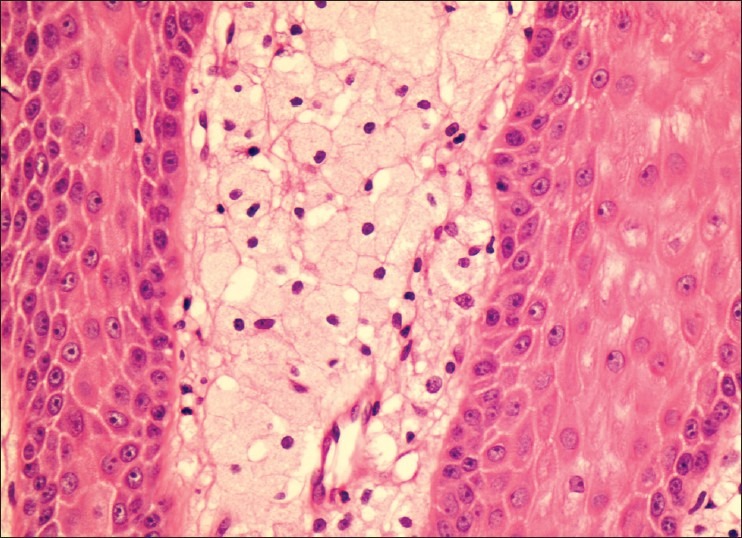
Elongated dermal papillae stuffed with foam cells (H and E; 400×) (case 3)
Figure 5.
Deep invaginated columns of parakeratosis (H and E; 40×) (case 2)
Features of human papilloma virus (HPV) infection, namely hypergranulosis and koilocytosis, were not seen in any of the biopsies.
The lesions were excised, with no recurrence, in cases 1 and 2; the others cases were lost to follow-up.
Discussion
VX is an uncommon entity and we could find only two publications on the subject in Indian literature (a total of three cases, all in the oral cavity).[10,11] The three cases of genital VX that we report are, to the best of our knowledge, the first report of nonoral VX from India. This may be due to lack of awareness of this condition or possibly reluctance to biopsy warty lesions of the genital mucosa and instead to treat them as viral warts/condylomata, which is the usual clinical diagnosis.
On the basis histomorphologic appearance the epithelial changes of VX have been been divided into three groups[9]–verrucous, papillary, and flat—and these epithelial changes reflect the clinical picture of the lesion. The diagnostic histological finding of all VX, however, whether intra- or extraoral in location, is the presence of foam cells that fill the dermal papillae and submucosal space. These foam cells have been shown to have monocyte/macrophage lineage.[9]
Two aspects of this condition remain unresolved, namely the etiology and the pathogenesis of lipid-laden macrophages in the dermal papillae and submucosa.
Because the clinical appearance and histological silhouette closely resembles HPV-induced lesions like verrucae and condylomata and because the common sites of occurrence of VX is the oral and anogenital skin and mucosa (sites common for HPV infection), HPV infection has always been a strong contender as the etiologic agent for this condition. Most authors have not found any evidence for the presence of HPV in these lesions;[12–14] however, contrary findings of multiple HPV DNA in VX have also been reported.[15]
Regarding the pathogenesis of lipid-laden macrophages in the dermal papillae, Zegarelli[16] proposed that initial damage to keratinocytes by an inciting agent is followed by degeneration of keratinocytes, which attracts dermal dendrocytes to engulf the debris and these develop into foam cells due to ingestion of lipids from the degenerating keratinocytes in the subepithelial dermis.
The probable pathogenesis of VX has been postulated to be as follows:[12] ‘following keratinocyte damage by an as yet unknown inciting agent, cytokines chemotactic for neutrophils are released, with rapid growth of the epidermis leading to the verruciform architecture and parakeratosis. The damaged and degenerating keratinocytes that move downwards into the papillary dermis and submucosal region are engulfed by dendritic cells, which develop into foam cells, losing in the process their normal histiocytic markers and stain negative for factor XIIIa.’
Xanthomatous changes in the papillary dermis, similar to that in VX, have been described in association with several diseases, including mycosis fungoides,[17] epithelial nevi,[18,19] and dystrophic epidermolysis bullosa.[20,21] The changes may histologically resemble true VX and are considered to be a form of dystrophic xanthomatosis that possibly arises due to repeated epidermal or dermal damage, with accumulation of lipids within macrophages.
Simple excision of the lesion appears to be curative; however, a 30-year-old woman with a recurrent VX of the vulva 8 years after initial treatment has been described in literature.[22]
To conclude, VX may be confused clinically with benign, premalignant, and malignant lesions like viral genital warts (condylomata acuminata), leukoplakia, and verrucous carcinoma, and may even be associated with squamous cell carcinoma.[23]
Genital warts induced by HPV are almost always multiple and therefore a single asymptomatic verrucous lesion on the oral or genital mucosa should always be subjected to biopsy to confirm the diagnosis and rule out malignancy. A definite diagnosis of VX can only be made on histopathologic examination.
This series is, to the best of our knowledge, the first report of extraoral lesions of VX from India. We report these cases to increase awareness regarding this rather rare but distinctive condition that should be considered in the differential diagnoses of solitary verrucous lesion on mucosal sites, both oral and genital.
What is new?
Nonoral (genital skin) verruciform xanthoma is described for the first time in Indian cases.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Shafer W. Verruciform xanthoma. Oral Surg. 1971;31:784–9. doi: 10.1016/0030-4220(71)90134-4. [DOI] [PubMed] [Google Scholar]
- 2.Buchner A, Hansen LS, Merell PW. Verruciform xanthoma of the oral mucosa. Report of five cases and review of the literature. Arch Dermatol. 1981;117:563–5. [PubMed] [Google Scholar]
- 3.Nowparast B, Howell FV, Rick GM. Verruciform xanthoma. A clinico-pathologic review and report of fifty four cases. Oral Surg. 1981;51:619–25. doi: 10.1016/s0030-4220(81)80012-6. [DOI] [PubMed] [Google Scholar]
- 4.Santa Cruz DJ, Martin SA. Verruciform xanthoma of the vulva. Report of two cases. Am J Clin Pathol. 1979;71:224–8. doi: 10.1093/ajcp/71.2.224. [DOI] [PubMed] [Google Scholar]
- 5.Al-Nafussi AI, Azzopardi JG, Salm R. Verruciform xanthoma of skin. Histopathology. 1985;9:245–52. doi: 10.1111/j.1365-2559.1985.tb02439.x. [DOI] [PubMed] [Google Scholar]
- 6.Geiss DF, Del Rosso JQ, Murphy V. Verruciform xanthoma of the glans penis: A benign simulator of genital malignancy. Cutis. 1993;51:369–72. [PubMed] [Google Scholar]
- 7.Kimura S. Verruciform xanthoma of the scrotum. Arch Dermatol. 1984;120:1378–9. [PubMed] [Google Scholar]
- 8.Lonsdale RN. Verruciform xanthoma of the penis. Br J Urol. 1992;70:574–5. [PubMed] [Google Scholar]
- 9.Philipsen HP, Reichart PA, Takata T, Ogawa I. Verruciform xanthoma: Biological profile of 282 oral lesions based on literature and survey with nine new cases from Japan. Oral Oncol. 2003;39:325–36. doi: 10.1016/s1368-8375(02)00088-x. [DOI] [PubMed] [Google Scholar]
- 10.Chandran S, Krishnaswami H. Verruciform xanthoma: A case report. Indian J Pathol Microbiol. 1996;39:307–8. [PubMed] [Google Scholar]
- 11.Sah K, Kale AD, Hallikerimath S. Two cases of oral verruciform xanthoma. J Oral Maxillofac Pathol. 2008;12:41–4. [Google Scholar]
- 12.Mohsin SK, Lee MW, Amin MB, Stoler MH, Eyzaguirre E, Ma CK, et al. Cutaneous verruciform xanthomna: A report of five cases investigating the etiology and nature of xanthomatous cells. Am J Surg Pathol. 1998;22:479–87. doi: 10.1097/00000478-199804000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Helm KF, Hopfl RM, Kreider JW, Lookingbill DP. Verruciform xanthoma in an immunocompromised patient. A case report and immunohistochemical study. J Cut Pathol. 1993;20:84–6. doi: 10.1111/j.1600-0560.1993.tb01256.x. [DOI] [PubMed] [Google Scholar]
- 14.Orchard GE, Jones EW, Jones RR. Verruciform xanthoma: An immunohistochemical study. Br J Biomed Sci. 1994;51:28–34. [PubMed] [Google Scholar]
- 15.Rohwedder A, Murphy M, Carlson FA. Multiple HPV DNA identified in verruciform xanthoma by nested polymerase chain reaction with degenerate consensus primers. J Cutaneous Pathol. 2003;30:344–6. doi: 10.1034/j.1600-0560.2003.00074.x. [DOI] [PubMed] [Google Scholar]
- 16.Zegarelli DJ, Zegarelli-Schmidt EC, Zegarelli EV. Verruciform xanthoma: A clinical, light microscopic and electron microscopic study of two cases. Oral Surg. 1974;38:725–34. doi: 10.1016/0030-4220(74)90393-4. [DOI] [PubMed] [Google Scholar]
- 17.McCadden ME, Glick AD, King LE., Jr Mycosis fungoides associated with dystrophic xanthomatosis. Arch Dermatol. 1987;123:91–4. [PubMed] [Google Scholar]
- 18.Grosshans E, Laplanche G. Verruciform xanthoma or xanthomatous transformation of inflammatory epidermal nevus? J Cutaneous Pathol. 1981;8:382–4. doi: 10.1111/j.1600-0560.1981.tb01025.x. [DOI] [PubMed] [Google Scholar]
- 19.Palestine RF, Winkelman RK. Verruciform xanthoma in an epithelial nevus. Arch Dermatol. 1982;118:688–91. [PubMed] [Google Scholar]
- 20.Cooper TW, Santa Cruz DJ, Bauer EA. Verruciform xanthoma: Occurrence in eroded skin in a patient with recessive dystrophic epidermolysis bullosa. J Am Acad Dermatol. 1983;8:463–7. doi: 10.1016/s0190-9622(83)70050-2. [DOI] [PubMed] [Google Scholar]
- 21.Orpin SD, Scott C, Rajaratnam R, Colloby PS, Heagerty A. A rare case of recessive dystrophic epidermolysis bullosa and verruciform xanthoma. Clin Expt Dermatol. 2009;34:49–51. doi: 10.1111/j.1365-2230.2008.02888.x. [DOI] [PubMed] [Google Scholar]
- 22.Reich O, Reganer S. Recurrent verruciform xanthoma of the vulva. Int J Gynaec Pathol. 2004;23:75–7. doi: 10.1097/01.pgp.0000101143.79462.f7. [DOI] [PubMed] [Google Scholar]
- 23.Mannes KD, Dekle C, Requena L, Sangueza O. Verruciform xanthoma associated with SCC. Am J Dermatopathol. 1999;21:66–9. doi: 10.1097/00000372-199902000-00015. [DOI] [PubMed] [Google Scholar]


