Abstract
Patients with cancer have an impaired T cell response that can decrease the potential therapeutic benefit of cancer vaccines and other forms of immunotherapy. The establishment of a chronic inflammatory environment in patients with cancer plays a critical role in the induction of T cell dysfunction. The accumulation of myeloid-derived suppressor cells (MDSC) in tumor bearing hosts is a hallmark of malignancy-associated inflammation and a major mediator of the induction of T cell suppression in cancer. Recent findings in tumor bearing mice and cancer patients indicate that the increased metabolism of L-Arginine (L-Arg) by MDSC producing Arginase I inhibits T cell lymphocyte responses. Here, we discuss some of the most recent concepts of how MDSC expressing Arginase I may regulate T cell function in cancer and suggest possible therapeutic interventions to overcome this inhibitory effect.
Keywords: MDSC, tumor immunology, arginine
INTRODUCTION
Modern concepts in carcinogenesis including the viral etiology of certain malignancies, the presence of mutated onco-proteins, and the over-expression of certain normal antigens, support the concept that antigen specific immune responses can be generated to control tumor growth. However, three decades of clinical trials in cancer immunotherapy have also made evident that tumor cells develop sophisticated mechanisms to evade the immune response. Extensive research has characterized multiple pathways triggered by the tumor microenvironment that result in the impairment of T cell anti-tumor responses. A better understanding of these molecular and cellular mechanisms is expected to enable the development of therapies to modulate the immune response for the benefit of the cancer patients.
Although most researchers agree that the malignant cells trigger the events that ultimately lead to T cell dysfunction, the intermediaries in this process vary, including regulatory T cells, plasmacytoid dendritic cells, suppressor macrophages, and more recently myeloid-derived suppressor cells (MDSC). The latter subpopulation of immune cells has recently become the focus of much research because of novel observations demonstrating their ability to regulate T cell responses, among others, by controlling the availability of the amino-acid L-Arginine (L-Arg). In this review, we will discuss some of the most recent concepts of how MDSC metabolizing L-Arg regulate T cell function in disease, and suggest possible therapeutic applications to inhibit their suppressive activity.
Alterations of the Immune Response in cancer
A dysfunctional immune response in cancer patients manifested by the loss of delayed type hypersensitivity was demonstrated several decades ago (Miescher et al., 1986; Miescher et al., 1988; Whiteside et al., 1988; Whiteside and Rabinowich, 1998). Initial explanations included the development of “blocking antibodies”, the production of suppressor factors and the generation of suppressor macrophages (Hellstrom et al., 1971; Hellstrom, Hellstrom, and Nelson, 1983; Varesio et al., 1979). However, the significance of these findings on the progression of the disease was unknown. Although cancer patients generally do not develop the characteristic opportunistic infections seen in patients immunosuppressed by high doses of chemotherapy, they show impaired T cell responses against bacterial and/or chemical antigens (Miescher et al., 1986; Miescher et al., 1988; Whiteside et al., 1988; Whiteside and Rabinowich, 1998).
This suggests that tumors have the ability to suppress T responses. In accordance, several animal tumor models and many clinical trials demonstrated that immunotherapy in both mice and patients with advanced tumors failed to achieve a therapeutic response as a result of the loss of T cell responses (Reviewed in Gattinoni et al., 2006; Sharma et al., 2011). In addition, several vaccine trials demonstrated the progression of tumors in spite of a robust T cell response (Stevenson, 2005). The development of cellular and molecular models leading to T cell anergy provided important insights on how cancer (and chronic inflammatory diseases) could selectively induce T cell dysfunction (Rabinovich, Gabrilovich, and Sotomayor, 2007).
This provided the basis for the discovery of several mechanisms including the role of immunoregulatory molecules in antigen presenting cells (APCs) such as B7.1, B7.2, B7-H1 and B7-H4 (Dong et al., 1999; Klausner, Lippincott-Schwartz, and Bonifacino, 1990; Kryczek et al., 2006b; Kryczek et al., 2006a), the development of regulatory T cells (McHugh et al., 2001; McHugh and Shevach, 2002), and the tumor-induced accumulation of MDSC (Bronte and Zanovello, 2005; Gabrilovich, 2004; Pekarek et al., 1995; Seung et al., 1995). Although most models are in agreement that tumor cells are the initiators of the suppressor phenomenon, they also conclude that APCs, in the form of macrophages, dendritic cells, and MDSC, play a central role in directly inducing T cell anergy (McHugh et al., 2001; McHugh and Shevach, 2002).
In fact, Gabrilovich et al. (1998); Zarour et al. (1996); and Dolcetti et al (2010) demonstrated that vascular endothelial growth factor (VEGF), granulocytic colony stimulating factor (G-CSF), and granulocytic-monocytic colony stimulating factor (GM-CSF) produced by tumor cells arrested the differentiation of myeloid cells, resulting in immature myeloid cells that induce T cell dysfunction. These myeloid cells blocked T cell responses by producing IL-10, TGF-β and prostaglandin E2 (PGE2)(Young, Newby, and Wepsic, 1987). Furthermore, an increased accumulation of these immature myeloid cells was found in patients with head and neck, breast, and lung cancer (Almand et al., 2000; Almand et al., 2001).
Intensive research has also focused in determining mechanisms by which T cells become suppressed in tumor-bearing hosts. Results showed that T cells from cancer patients and tumor bearing mice had multiple, but discrete changes in the expression of signal transduction molecules, including a decreased expression of the T cell receptor ζ chain (CD3ζ), a diminished tyrosine kinases p56lck, p59fyn, and an inability to upregulate Jak-3 and to translocate NFkBp65, all of which resulted in a diminished in vitro T cell response (Ghosh et al., 1994; Li et al., 1994; Mizoguchi et al., 1992).
These alterations were accompanied by a diminished ability to mobilize Ca++ and a decreased tyrosine phosphorylation (Mizoguchi et al., 1992), providing a possible molecular explanation for the T cell dysfunction in cancer. These initial findings in mice were confirmed in patients with renal cell carcinoma, melanoma, Hodgkin’s disease, ovarian cancer, colon carcinoma, and cervical cancer among others (Finke et al., 1993; Kono et al., 1996a; Zea et al., 1995). Preliminary studies also showed that patients with melanoma or head and neck tumors had a decreased survival time if expressing low levels of CD3ζ (Kuss et al., 1999; Zea et al., 1995). The absence of a mechanism to explain these changes and the apparent lack of specificity of these alterations created some initial controversy around these observations.
Later, Otsuji et al. (1996) and Kono et al. (Kono et al., 1996a; Kono et al., 1996b) demonstrated that the co-incubation of activated murine peritoneal macrophages with T cells induced the loss of CD3ζ chain. This phenomenon could be blocked by oxygen radical scavengers and was therefore thought to be mediated by hydrogen peroxide (Corsi et al., 1998). Similarly, Schmielau et al described an increased number of activated neutrophils in peripheral blood of patients with pancreatic and breast cancer who also had a diminished expression of CD3ζ chain (Schmielau and Finn, 2001). In addition, Baniyash and colleagues proposed that chronic stimulation of T cells by specific antigens led to the decreased expression of CD3ζ chain leading to the induction of anergy (Bronstein-Sitton et al., 2003). However, none of these models fully reproduced the multiple alterations found in T cells of cancer patients.
Metabolism of L-Arg by Myeloid Cells
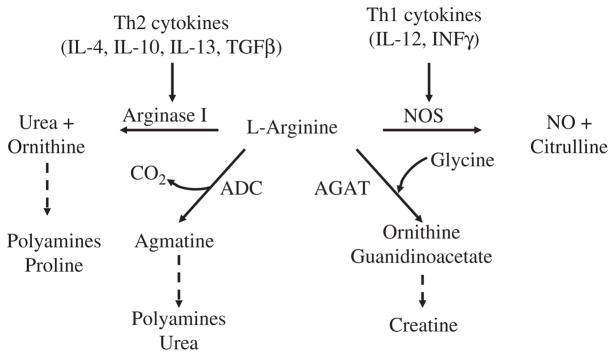
L-Arg is the substrate for four enzymes that exist as multiple isoforms: nitric oxide synthases (NOS1, NOS2, and NOS3), arginases (Arginase I and II), Arginine: glycine amidinotransferase (AGAT), and L-Arg decarboxylase (ADC) (Figure 1). Dietary L-Arg is taken up by intestinal epithelial cells and traverses the plasma membrane via the y+ system of cationic amino acid transporters (CAT) (Closs et al., 2004). Inside the cell, L-Arg is metabolized by NOS enzymes to produce citrulline and nitric oxide, the latter of which plays an important role in cytotoxic mechanisms and vasodilatation (Amber et al., 1991; Hibbs, Jr., Taintor, and Vavrin, 1987). Alternatively, arginase I and arginase II metabolize L-Arg to L-ornithine and urea, the first being the precursor for the production of polyamines essential for cell proliferation and the second an important mechanism for detoxification of protein degradation (Morris, Jr., 2002). ADC converts L-Arg to agmatine, which in turn is converted to putrescine and urea by agmatinase. ADC and AGAT appear to be less involved in the immune reponse. Mammalian ADC is highly expressed in brain (Iyo et al., 2006; Zhu et al., 2004), while AGAT is expressed in brain and heart (Cullen et al., 2006; Item et al., 2001).
Figure 1. L-Arg metabolism.
For the sake of simplicity, emphasis is on enzymes that directly metabolize L-Arg. This diagram should not be interpreted to indicate that all of these enzymes are expressed simultaneously in any given cell type. Th2 cytokines lead to the increase expression of arginase I, while Th1 cytokines increase inducible NOS. ADC, Arginine decarboxylase; AGAT, arginine: glycine amidinotransferase; NO, nitric oxide; NOS, nitric oxide synthase.
The expression of arginase I and NOS2 in murine macrophages is differentially regulated by Th1 and Th2 cytokines (Hesse et al., 2001; Munder et al., 1999). Stimulation of murine macrophages with IFN-γ up-regulates NOS2 exclusively, while IL-4, IL-10 and IL-13 induce arginase I (Munder, Eichmann, and Modolell, 1998; Rutschman et al., 2001) (Figure 1). The mitochondrial isoform arginase II is not significantly modulated by Th1 or Th2 cytokines (Rodriguez et al., 2003). The inhibition of arginase I leads to an increased NOS2 expression and consequently promotes NO production (Chicoine et al., 2004). Conversely, upregulation of arginase I inhibits NOS activity and contributes to the pathophysiology of several disease processes, including vascular dysfunction and asthma (Zhang et al., 2004).
The mechanism of inhibition of NOS2 expression by arginase I appears to be mediated by L-Arg depletion, which blocks the translation of NOS2 (Lee et al., 2003). In addition, low levels of nitric oxide induce nitrosylation of cysteine residues of arginase I, which increases the biological activity of arginase I, further reducing L-Arg (Santhanam et al., 2007).
Activation of murine macrophages with Th1 or Th2 cytokines also has different effects on the extra-cellular levels of L-Arg. Peritoneal macrophages stimulated with IL-4 plus IL-13 increase the expression of Arginase I and cationic amino acid transporter 2B (CAT-2B), which results in a rapid increase in the uptake of extra-cellular L-Arg with the consequent reduction of L-Arg in the microenvironment. In contrast, macrophages stimulated with IFN-γ preferentially express NOS2, do not increase CAT-2B, and do not deplete L-Arg from the microenvironment (Rodriguez et al., 2003).
Recent data from the arginase I and arginase II knockout mice confirm that only arginase I is able to deplete serum levels of L-Arg (Deignan et al., 2006; Iyer et al., 2002). Similarly, in vitro co-culture experiments showed that only macrophages producing arginase I, but not those expressing NOS2, caused the prolonged loss of CD3ζ and inhibited T cell proliferation. The addition of arginase inhibitors or exogenous L-Arg reversed the CD3ζ loss and reestablished T cell proliferation (Rodriguez et al., 2003). These results were confirmed with macrophages from arginase I conditional knockout mice (Unpublished findings).
Effects of L-Arg Starvation in T cells
The association of L-Arg metabolism and T cell responses was established through experiments showing that the thymic involution and decrease in T cells seen in mice undergoing extensive surgery was prevented by the injection of LArg (1). Our initial experiments demonstrated that culturing T cells in tissue culture medium with L-Arg levels <50 μM resulted in a significant decrease in cell proliferation (2). In addition, T cells activated in a L-Arg free environment developed all the alterations previously described in tumor bearing mice and cancer patients, i.e., the decreased expression of CD3ζ, an inability to upregulate Jak-3, and a decreased translocation of NFkB-p65 (Zea et al., 2004).
Although the initial results suggested that the low T cell proliferation was the result of a decreased CD3ζ expression, we found that T cells cultured in the absence of L-Arg had an increased production of IL-2 and high expression of early activation markers CD25, CD69, CD122, and CD132. In addition, T cells activated with PMA, which bypasses the T cell receptor, also failed to proliferate (3), confirming that the suppressive effect induced by the absence of L-Arg was not caused by a decrease in the T cell receptor signaling.
Later, Rodriguez et al. showed that activated T cells cultured in the absence of L-Arg were arrested in the G0-G1 phase of the cell cycle, while cells cultured with L-Arg progressed into the S and G2-M phases (Rodriguez, Quiceno, and Ochoa, 2007). Association of D-type cyclins (Cyclin D1, D2 and D3) and cyclin-dependent kinase 4 (cdk4) and cdk6 regulate the progression of T cells through early G1 and later into the S phase of the cell cycle (Kato, 1997). Our results showed that T cells cultured in the absence of L-Arg were unable to up-regulate cyclin D3 and cdk4, but increased cdk6 expression (Rodriguez, Quiceno, and Ochoa, 2007). In addition, silencing of cyclin D3 in T cells induced a similar inhibition of proliferation as that seen in the absence of L-Arg. Interestingly, LArg starvation impaired the expression of cyclin D3 and cdk4 in T cells through a decreased mRNA stability and diminished translational rate (Rodriguez et al., 2010; Rodriguez, Quiceno, and Ochoa, 2007).
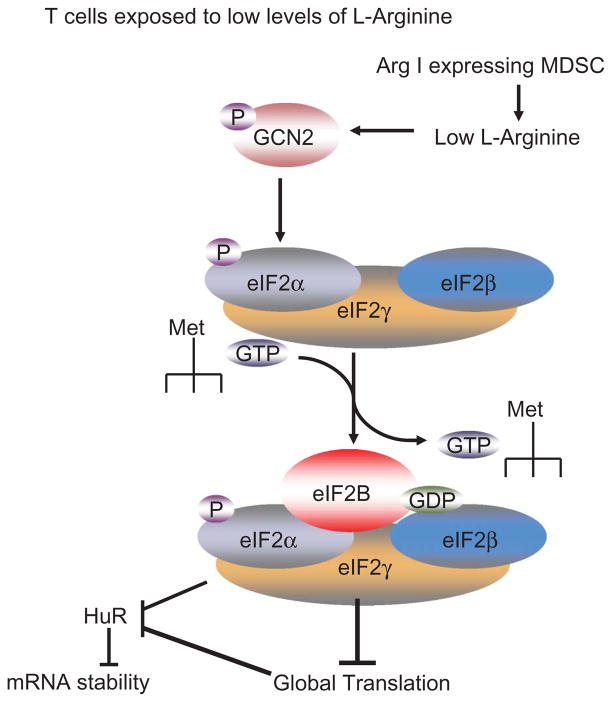
Previous results have suggested the mechanisms by which amino acid starvation impairs global translation. Accumulation of empty aminoacyl tRNAs caused by amino acid starvation, activates GCN2 kinase which phosphorylates the translation initiation factor eIF2α. The phosphorylated form of eIF2α binds with high affinity to eIF2B, blocking its ability to exchange GDP for GTP, which inhibits the binding of the eIF2 complex to methionine aminoacyl tRNA. This results in a decreased initiation of global protein synthesis.
Our recent results suggest that T cells cultured in the absence of L-Arg display a decrease in global translation, which associates with higher levels of phospho-eIF2α (Rodriguez et al., 2010) (Figure 2). In addition, the global decrease in translation impairs the expression of RNA-binding protein HuR, thereby inhibiting mRNA stability of mRNA containing AUUA rich elements (Rodriguez et al., 2010). However, it is still unknown whether phospho-eIF2α is the only mediator of the arrest in translation induced by the absence of L-Arg. Furthermore, T cells from GCN2 knockout mice do not show an arrest in cell cycle or a decrease in proliferation when cultured in medium without L-Arg, suggesting the potential role of GCN2 on the alterations induced by the absence of L-Arg (Rodriguez, Quiceno, and Ochoa, 2007).
Figure 2. Control of T cell translation by MDSC.
Metabolism of L-arginine by MDSC leads to a decrease in the extra cellular availability of arginine, which in T cells activates GCN2 kinase, thereby leading to the phosphorylation of eIF2a. This leads to a global decrease in translation and to the low expression of mRNA stabilizing protein HuR.
Arginase I Expression in MDSC Infiltrating Tumors
Several tumor lines including non-small lung carcinoma and breast carcinoma have been shown to express arginase (Chang, Liao, and Kuo, 2001; Singh et al., 2000; Suer et al., 1999). This has been thought to be a mechanism for the production of polyamines needed to sustain the rapid proliferation of tumor cells. Results from our laboratory suggest instead that arginase I is preferentially expressed in MDSC infiltrating tumors, which inhibits T cell function and represents a possible mechanism of tumor evasion (Rodriguez et al., 2004). Although the majority of the studies suggested that MDSC suppress T cell function, few reports initially showed the absence of this effect. These discrepancies were the result of MDSC isolated from different tissues (lymph node vs spleen vs tumor) or even in the differential tumor model. In addition, it is also accepted that MDSC initially accumulate to fight tumors, but are changed in their phenotype as tumor progresses and chronic inflammation establishes. Therefore, timing also plays a major role.
Two important subsets of MDSC have been reported based on their expression of CD11b, LY6G and LY6C. Granulocytic MDSC have a CD11b+ LY6G+ LY6Clow phenotype, whereas monocytic MDSC are CD11b+ LY6G− LY6Chigh (Youn et al., 2008). Although these populations have been identified, it is still unclear the biology and the mechanisms of the accumulation of these cells in disease. So far, monocytic MDSC appear to be precursors of macrophages and dendritic cells, whereas granulocytic MDSC are formed by mature and immature polymorphonuclear cells (Gabrilovich and Nagaraj, 2009). Granulocytic and monocytic populations of immature myeloid cells (iMC) with a phenotype similar to MDSC are present in the bone marrow of healthy mice (Bronte et al., 2000; Kusmartsev et al., 2004; Sinha, Clements, and Ostrand-Rosenberg, 2005a). However, recent publications suggest that MDSC although morphologically similar to iMC, display a high T cell suppressive capability, whereas iMC lacks it (Solito et al., 2011; Youn et al., 2012).
Depletion of both MDSC subpopulation using anti-GR-1 antibodies induced an anti-tumor effect mediated by CD8+ T cells (Holda, Maier, and Claman, 1985; Pekarek et al., 1995; Seung et al., 1995). Furthermore, we and others previously reported the existence of CD11b+ LY6G− LY6C− MDSC in tumors, which have a similar phenotype that of alternatively activated macrophages (Dolcetti et al., 2010; Rodriguez et al., 2004). Even though there are variations in cell morphology and maturation markers between different tumor models and between murine and human tumors, these myeloid cells suppress T cell function. In addition, accumulating literature now describes the role of MDSC in angiogenesis and in the promotion of the pre metastatic niche (Granot et al., 2011; Toh et al., 2011).
Granulocytic MDSCs are the major source of arginase I in tumor bearing hosts (Rodriguez et al., 2004), whereas tumor-associated monocytic MDSC metabolize L-Arg through NOS2 (Youn et al., 2008).
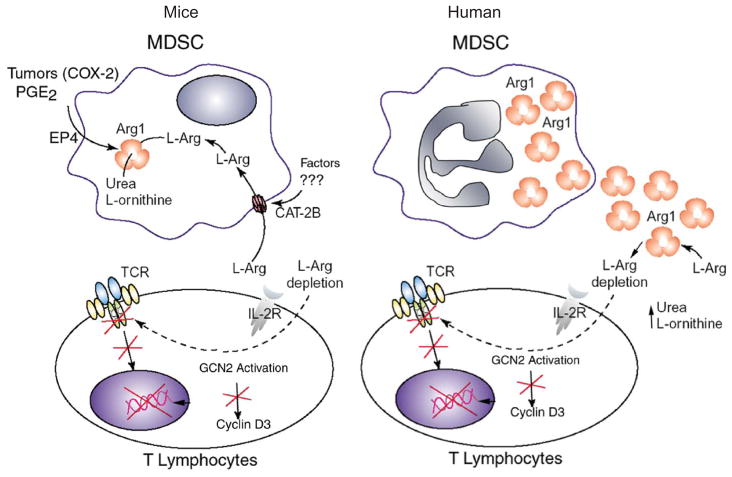
Our data suggests that the primary mechanism by which MDSC induce T cell tolerance is by depleting extra cellular L-Arg through Arginase I (Rodriguez et al., 2005; Rodriguez et al., 2003; Rodriguez et al., 2004) (Figure 3). The addition of arginase I inhibitors Nor-NOHA or NOHA in vitro, or its injection into tumor-bearing mice prevents the loss of T cell function and results in an immune-mediated anti-tumor response, which inhibits tumor growth in a dose-dependent manner. The inhibition in tumor growth caused by Nor NOHA, does not happen in tumor-bearing scid mice, strongly suggesting that the anti-tumor effect caused arginase I inhibition is dependent on lymphocyte function (Rodriguez et al., 2004).
Figure 3. T cell dysfunction induced by arginase I.
Tumor cells expressing COX-2 and releasing PGE2 induces the expression of arginase I and CAT-2B in MDSC. This leads to a reduction of extra cellular levels of L-Arg, which finally activates GCN2 and blocks the expression of multiple genes including CD3 z, cyclin D3 and cdk4. A similar reduction occurs in patients with cancer, but through the release of arginase into the extracellular environment.
MDSC may also cause T cell tolerance through cell to cell contact. This mechanism appears to require the co-expression of arginase I and NOS2 (Bronte and Zanovello, 2005). The addition of NOS2 and arginase inhibitors to co-cultures of MDSC and activated T cells completely reestablishes T cell function (Bronte et al., 2003). It is possible that this phenomenon is in part mediated by the production of peroxinitrites. Under limiting amounts of L-Arg, NOS2 produces peroxinitrites (ONOO−), a highly reactive oxidizing agent that nitrates proteins and induces T cell apoptosis (Kusmartsev and Gabrilovich, 2005). This appears to affect the conformational flexibility of the T cell antigen receptor and its interaction with MHC by inducing nitration of T cell antigen receptor proteins in CD8+ cells.
Thus, MDSC directly disrupt the binding of specific peptides on MHC to CD8+ T cells (Lu et al., 2011; Nagaraj et al., 2007). In addition, peroxinitrites induce apoptosis in activated T cells (Kasic et al., 2011). MDSC co-expressing arginase I and NOS2 primarily impair CD8+ T cell function (Kusmartsev and Gabrilovich, 2005; Rodriguez et al., 2004; Sinha, Clements, and Ostrand-Rosenberg, 2005a; Van Ginderachter et al., 2006) by blocking their ability to secrete IFN-γ when stimulated with specific antigens (Gabrilovich et al., 2001; Kusmartsev et al., 2004), and inducing apoptosis (Kusmartsev and Gabrilovich, 2005). This suppression requires the production of IL-13 and IFN-γ (Gallina et al., 2006; Sinha, Clements, and Ostrand-Rosenberg, 2005b; Sinha, Clements, and Ostrand-Rosenberg, 2005a) and signaling through STAT1 transcription factor (Kusmartsev and Gabrilovich, 2005). In addition, MDSC have been shown to produce high levels of stem cell factor (SCF) when stimulated by IFNγ and IL10 (Huang et al., 2006). Blocking of SCF signaling in MDSC significantly impairs their ability to generate regulatory T cells (Pan et al., 2008), preventing a fundamental mechanism by which MDSC induce T cell suppression.
MDSC in Human Tumors
Human MDSC phenotypes vary significantly ranging from immature myeloid cells (Sica and Bronte, 2007; Solito et al., 2011) to activated granulocytes (Rodriguez et al., 2009). They have been reported to express a wide range of markers including CD11b, CD14, CD15, CD33, VEGFR and CD66b (reviewed in (Greten, Manns, and Korangy, 2011)). A retrospective study of patients with metastatic renal cell carcinoma (RCC) demonstrated a 6–10 fold increase in arginase activity in the peripheral blood mononuclear cells (PBMC), as compared to normal controls (Zea et al., 2005). Separation of the different subpopulations in the PBMC of these patients demonstrated that the major source for arginase were granulocytes, which separated with the PBMC when centrifuged over ficoll-hypaque (Rodriguez et al., 2009). In addition, T cell proliferation and IFN-γ production in vitro was re-established after the depletion of MDSC.
In the same patient population, there was an inverse statistical correlation between arginase activity and MDSC numbers with the expression of CD3ζ chain in T cells (Figure 3). A similar sub-population of activated granulocytes had previously been described by Schmielau and Finn (Schmielau and Finn, 2001) in patients with pancreatic cancer, where they demonstrated a correlation between the presence of activated granulocytes and alterations in T cells such as reduced CD3ζ expression and decreased cytokine production (Schmielau and Finn, 2001). Furthermore, results from clinical trials using IL-2 in patients with renal cell carcinoma and melanoma have shown a clear association between poor clinical responses and high numbers of granulocytes in peripheral blood (Rodgers, Rees, and Hancock, 1994).
Although human MDSC express high levels of arginase I, this does not appear to be upregulated by cytokines or other signals, suggesting the possibility of a constitutively expression of arginase I in human MDSC. Furthermore, human MDSC do not uptake L-Arg. Instead, arginase I stored in primary (Munder et al., 2005) or gelatinase granules (Jacobsen et al., 2007) is released to the microenvironment inducing a significant decrease in L-Arg levels, which impairs T cell function and CD3ζ chain expression (Kropf et al., 2007; Munder et al., 2006; Zea et al., 2005) (Figure 3). In fact, the release of arginase I into the sera of renal cell carcinoma patients induced a decrease in plasma of L-Arg levels to <50μM and an increase in ornithine levels demonstrating that arginase I not only had a metabolic effect (L-Arg depletion), but also a negative effect on the T cell response (Zea et al., 2005).
Regulation and Activation of MDSC in Cancer
Different cytokines participate in the recruitment of MDSC from the bone marrow, including VEGF and GM-CSF (Dolcetti et al., 2010). In addition, serum levels of VEGF directly correlated with numbers of MDSC in the blood and spleen (Ohm and Carbone, 2001) and have been associated with poor prognosis in cancer patients. Tumor derived VEGF has been previously associated with an arrest in dendritic cells maturation (Gabrilovich et al., 1998; Oyama et al., 1998) through the inhibition in Nf-κβ signaling. Treatment of MDSC with all-trans retinoic acid appears to counter this inhibition and promotes MDSC differentiation into mature APC (Kusmartsev et al., 2003). Increased levels of GM-CSF have also been associated with MDSC-dependent suppression which was reversed by the use of neutralizing antibodies to GM-CSF (Bronte et al., 2000).
Similar effects on MDSC have been suggested with other growth factors including Fms-like tyrosine kinase 3 (Flt3) ligand (Solheim et al., 2007), stem cell factor (SCF) (Pan et al., 2008) and S100 calcium binding protein A9 (S100A9) (Cheng et al., 2008). Furthermore, blocking of MDSC accumulation in tumor-bearing hosts with antibodies against Gr-1, CD11b, and colony stimulating factor 1 (CSF1), using the inhibitor of CSF1 receptor (CSFR1/c-kit), sunitinib, or using the anti-metabolites gemcitabine (GEM) and 5-fluorouracil (5-FU) has shown to partially restore T cell function in tumor bearing hosts (Gabrilovich and Nagaraj, 2009; Ko et al., 2010; Kusmartsev et al., 2008; Le et al., 2009; Mundy-Bosse et al., 2011; Pan et al., 2008; Toh et al., 2011; Vincent et al., 2010). However, it remains unclear the effects of the mentioned chemotherapy agents in the accumulation of specific sub populations of MDSC. I.e. Sunitinib blocks the proliferation of monocytic MDSC, while impairing granulocytic MDSC survival (Ko et al., 2010). This important question is being tested in ongoing research in several labs.
We used the 3LL murine lung carcinoma model to further determine what factors might be inducing the production of arginase I in the MDSC infiltrating tumors. MDSC isolated from 3LL tumors and placed in culture in regular medium, loose arginase I expression within 24 hours. However, if freshly isolated MDSC were co-cultured in transwells with 3LL cells or with 3LL supernatants they maintained arginase I expression, suggesting that the induction of arginase I was caused by soluble factor(s) produced by tumor cells (Rodriguez et al., 2005).
Cytokines such as IL-4, IL-13, TGF-β and others were not detected in the supernatants of the 3LL single cell suspensions. Instead, we detected a very high expression of the inducible cyclooxygenase-2 (COX-2) and an increased production of prostanoids including PGE2. The addition of COX-2 inhibitors or silencing of COX-2 in 3LL cells, completely blocked their ability to induce arginase I in MDSC (Rodriguez et al., 2005).
The effect of PGE2 on MDSC was dependent on the expression of the E-prostanoid receptor (EP4) on MDSC and was associated with an increased cAMP levels (Rodriguez et al., 2005). Consequently, treatment of tumor bearing mice with COX-2 inhibitor sc-58125 decreased the expression of arginase I in MDSC infiltrating the tumor and induced an immune-mediated anti-tumor effect (Rodriguez et al., 2005). Similar results have been reported in mice bearing the 4T1 breast carcinoma where the treatment with the COX-2 inhibitor SC-58236 reduced the accumulation of MDSC in the spleen in an EP2 dependant manner (Sinha et al., 2007).
In addition celecoxib, a selective COX-2 inhibitor was able to inhibit the induction of colon tumors in Swiss mice treated with 1,2-dimethylhydrazine diHCl-(1,2-DMH) (Talmadge et al., 2007). Other factors may also play a role in the induction of arginase in MDSC including hypoxia-inducible factor 1 (HIF-1) and HIF-2 (Reviewed in (Semenza, 2003)), IL-4, IL-13 and IFNγ (Gallina et al., 2006).
Furthermore, although the mechanisms controlling the induction of arginase I in MDSC have been partially identified in mice, the factors mediating the activation of MDSC in cancer patients remain unclear. A recent publication by Rotondo et al. (2009) suggests the possible role of tumor derived IL-8 on the release of arginase from human MDSC. In addition, Solito et al. (2011) showed that a combination of G-CSF and GM-CSF induce a heterogeneous promyelocyte population with characteristics of MDSC. Future clinical approaches either inhibiting the factors leading to the accumulation of human MDSC or depleting MDSC can be predicted. This will create an opportunity for combination with different chemotherapy agents, cancer vaccines, and/or other forms of immunotherapy.
MDSC: LESSONS FROM OTHER DISEASES AND FUTURE APPLICATIONS
The advent of immunotherapy of cancer made apparent that in spite of powerful biological agents that could prime tumor specific T cells, tumors had sophisticated mechanisms to escape the immune response, including MDSC. MDSC however are not unique to cancer. Trauma patients and patients with chronic infections including active pulmonary tuberculosis also have increased numbers of MDSC expressing arginase I that inhibit T cell function. This data suggests that MDSC may represent a normal process triggered by tissue damage (danger signal) with the aim of protecting the integrity of the tissues and “healing” the initial injury. A demonstration of this mechanism was described in the late 1980s by Albina et al. (1989) studying the healing of surgical wounds.
They described that the tissue surrounding a surgical wound was initially infiltrated by cells expressing iNOS, which would most likely eliminate offending agents contaminating the wound. This surge was followed by cells expressing arginase I which metabolize L-Arg to ornithine, which in turn would trigger the synthesis of collagen by fibroblasts, ultimately leading to the healing of the surgical wound. The local depletion of L-Arg would also prevent T cells from infiltrating a healing tissue. In cancer or chronic infections, tissue damage would also trigger a similar response with the proliferation of fibroblasts producing collagen aimed at isolating and healing the damaged tissue (i.e., malignant growth).
As a matter of fact, many tumors are surrounded by dense fibrous tissue that makes difficult its surgical excision. The major difference between both disease processes (surgical wound vs malignant tumor) is that the surgical wounds heal, thus, ending the role for arginase producing MDSC. In contrast, malignant tumors do not stop growing and destroying tissue (would not “heal”) promoting instead a chronic inflammatory process mediated by MDSC. The continuous production of arginase I would ultimately lead to the depletion of L-Arg from the microenvironment and the development of T cell anergy.
Therefore, it is our hypothesis that tumors “hijack” a normal healing process making it instead a vicious cycle that results in the inhibition of a potentially protective T cell anti-tumor response. Although this is likely to be an oversimplified version of the complex mechanisms triggered in vivo, it provides a model to understand a complex event in the development of cancer, which could enable the design new therapeutic approaches to interrupt this dysfunctional response.
In summary, our understanding of the role that MDSC play in the progression of tumors has significantly increased during the last 10 years. Multiple approaches have been taken to block MDSC suppression including the use of all-transretinoic acid (Kusmartsev et al., 2003), inhibiting nitric oxide function with nitro-aspirin (De et al., 2005), inhibiting phphodiesterase-5 (Serafini et al., 2006), blocking arginase activity with specific arginase inhibitors (Rodriguez et al., 2004), blocking of MDSC accumulation using antibodies against Gr-1, CD11b, and CSF, or using chemotherapy agents sunitinib, GEM, or 5-FU (Gabrilovich and Nagaraj, 2009; Ko et al., 2010; Kusmartsev et al., 2008; Le et al., 2009; Mundy-Bosse et al., 2011; Pan et al., 2008; Toh et al., 2011; Vincent et al., 2010). It is likely that the appropriate combination of inhibitors blocking MDSC function and stimuli protecting T cells may overcome this powerful tumor-derived mechanism that impairs the promise of cancer immunotherapy.
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Contributor Information
Patrick Raber, Email: praber@lsuhsc.edu.
Augusto C. Ochoa, Email: aochoa@lsuhsc.edu.
Paulo C. Rodríguez, Email: prodri1@lsuhsc.edu.
References
- Albina JE, Caldwell MD, Henry WL, Jr, Mills CD. Regulation of macrophage functions by L-arginine. J Exp Med. 1989;169:1021–1029. doi: 10.1084/jem.169.3.1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almand B, Clark JI, Nikitina E, van Beynen J, English NR, Knight SC, Carbone DP, Gabrilovich DI. Increased production of immature myeloid cells in cancer patients: a mechanism of immunosuppression in cancer. J Immunol. 2001;166:678–689. doi: 10.4049/jimmunol.166.1.678. [DOI] [PubMed] [Google Scholar]
- Almand B, Resser JR, Lindman B, Nadaf S, Clark JI, Kwon ED, Carbone DP, Gabrilovich DI. Clinical significance of defective dendritic cell differentiation in cancer. Clin Cancer Res. 2000;6:1755–1766. [PubMed] [Google Scholar]
- Barbul A, Rettura G, Levenson SM, Seifter E. Arginine: a thymotropic and wound-healing promoting agent. Surg Forum. 1977;28:101–103. [PubMed] [Google Scholar]
- Bronstein-Sitton N, Cohen-Daniel L, Vaknin I, Ezernitchi AV, Leshem B, Halabi A, Houri-Hadad Y, Greenbaum E, Zakay-Rones Z, Shapira L, Baniyash M. Sustained exposure to bacterial antigen induces interferon-gamma-dependent T cell receptor zeta down-regulation and impaired T cell function. Nat Immunol. 2003;4:957–964. doi: 10.1038/ni975. [DOI] [PubMed] [Google Scholar]
- Bronte V, Apolloni E, Cabrelle A, Ronca R, Serafini P, Zamboni P, Restifo NP, Zanovello P. Identification of a CD11b(+)/Gr-1(+)/CD31(+) myeloid progenitor capable of activating or suppressing CD8(+) T cells. Blood. 2000;96:3838–3846. [PMC free article] [PubMed] [Google Scholar]
- Bronte V, Serafini P, De Santo C, Marigo I, Tosello V, Mazzoni A, Segal DM, Staib C, Lowel M, Sutter G, Colombo MP, Zanovello P. IL-4-induced arginase 1 suppresses alloreactive T cells in tumor-bearing mice. J Immunol. 2003;170:270–278. doi: 10.4049/jimmunol.170.1.270. [DOI] [PubMed] [Google Scholar]
- Bronte V, Zanovello P. Regulation of immune responses by L-arginine metabolism. Nat Rev Immunol. 2005;5:641–654. doi: 10.1038/nri1668. [DOI] [PubMed] [Google Scholar]
- Chang CI, Liao JC, Kuo L. Macrophage arginase promotes tumor cell growth and suppresses nitric oxide-mediated tumor cytotoxicity. Cancer Res. 2001;61:1100–1106. [PubMed] [Google Scholar]
- Cheng P, Corzo CA, Luetteke N, Yu B, Nagaraj S, Bui MM, Ortiz M, Nacken W, Sorg C, Vogl T, Roth J, Gabrilovich DI. Inhibition of dendritic cell differentiation and accumulation of myeloid-derived suppressor cells in cancer is regulated by S100A9 protein. J Exp Med. 2008;205:2235–2249. doi: 10.1084/jem.20080132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chicoine LG, Paffett ML, Young TL, Nelin LD. Arginase inhibition increases nitric oxide production in bovine pulmonary arterial endothelial cells. Am J Physiol Lung Cell Mol Physiol. 2004;287:L60–L68. doi: 10.1152/ajplung.00194.2003. [DOI] [PubMed] [Google Scholar]
- Closs EI, Simon A, Vekony N, Rotmann A. Plasma membrane transporters for arginine. J Nutr. 2004;134:2752S–2759S. doi: 10.1093/jn/134.10.2752S. [DOI] [PubMed] [Google Scholar]
- Corsi MM, Maes HH, Wasserman K, Fulgenzi A, Gaja G, Ferrero ME. Protection by L-2-oxothiazolidine-4-carboxylic acid of hydrogen peroxide-induced CD3zeta and CD16zeta chain down-regulation in human peripheral blood lymphocytes and lymphokine-activated killer cells. Biochem Pharmacol. 1998;56:657–662. doi: 10.1016/s0006-2952(98)00085-9. [DOI] [PubMed] [Google Scholar]
- Cullen ME, Yuen AH, Felkin LE, Smolenski RT, Hall JL, Grindle S, Miller LW, Birks EJ, Yacoub MH, Barton PJ. Myocardial expression of the arginine:glycine amidinotransferase gene is elevated in heart failure and normalized after recovery: potential implications for local creatine synthesis. Circulation. 2006;114:I16–I20. doi: 10.1161/CIRCULATIONAHA.105.000448. [DOI] [PubMed] [Google Scholar]
- De Santo C, Serafini P, Marigo I, Dolcetti L, Bolla M, Del Soldato P, Melani C, Guiducci C, Colombo MP, Iezzi M, Musiani P, Zanovello P, Bronte V. Nitroaspirin corrects immune dysfunction in tumor-bearing hosts and promotes tumor eradication by cancer vaccination. Proc Natl Acad Sci USA. 2005;102:4185–4190. doi: 10.1073/pnas.0409783102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deignan JL, Livesay JC, Yoo PK, Goodman SI, O’Brien WE, Iyer RK, Cederbaum SD, Grody WW. Ornithine deficiency in the arginase double knockout mouse. Mol Genet Metab. 2006;89:87–96. doi: 10.1016/j.ymgme.2006.04.007. [DOI] [PubMed] [Google Scholar]
- Dolcetti L, Peranzoni E, Ugel S, Marigo I, Fernandez Gomez A, Mesa C, Geilich M, Winkels G, Traggiai E, Casati A, Grassi F, Bronte V. Hierarchy of immunosuppressive strength among myeloid-derived suppressor cell subsets is determined by GM-CSF. Eur J Immunol. 2010;40:22–35. doi: 10.1002/eji.200939903. [DOI] [PubMed] [Google Scholar]
- Dong H, Zhu G, Tamada K, Chen L. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med. 1999;5:1365–1369. doi: 10.1038/70932. [DOI] [PubMed] [Google Scholar]
- Finke JH, Zea AH, Stanley J, Longo DL, Mizoguchi H, Tubbs RR, Wiltrout RH, O’Shea JJ, Kudoh S, Klein E, Ochoa AC. Loss of T-cell receptor zeta chain and p56 lck in T-cells infiltrating human renal cell carcinoma. Cancer Res. 1993;53:5613–5616. [PubMed] [Google Scholar]
- Gabrilovich D. Mechanisms and functional significance of tumour-induced dendritic-cell defects. Nat Rev Immunol. 2004;4:941–952. doi: 10.1038/nri1498. [DOI] [PubMed] [Google Scholar]
- Gabrilovich D, Ishida T, Oyama T, Ran S, Kravtsov V, Nadaf S, Carbone DP. Vascular endothelial growth factor inhibits the development of dendritic cells and dramatically affects the differentiation of multiple hematopoietic lineages in vivo. Blood. 1998;92:4150–4166. [PubMed] [Google Scholar]
- Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9:162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrilovich DI, Velders MP, Sotomayor EM, Kast WM. Mechanism of immune dysfunction in cancer mediated by immature Gr-1+ myeloid cells. J Immunol. 2001;166:5398–5406. doi: 10.4049/jimmunol.166.9.5398. [DOI] [PubMed] [Google Scholar]
- Gallina G, Dolcetti L, Serafini P, De Santo C, Marigo I, Colombo MP, Basso G, Brombacher F, Borrello I, Zanovello P, Bicciato S, Bronte V. Tumors induce a subset of inflammatory monocytes with immunosuppressive activity on CD8+ T cells. J Clin Invest. 2006;116:2777–2790. doi: 10.1172/JCI28828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gattinoni L, Powell DJ, Jr, Rosenberg SA, Restifo NP. Adoptive immunotherapy for cancer: building on success. Nat Rev Immunol. 2006;6:383–393. doi: 10.1038/nri1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh P, Sica A, Young HA, Ye J, Franco JL, Wiltrout RH, Longo DL, Rice NR, Komschlies KL. Alterations in NF kappa B/Rel family proteins in splenic T-cells from tumor-bearing mice and reversal following therapy. Cancer Res. 1994;54:2969–2972. [PubMed] [Google Scholar]
- Granot Z, Henke E, Comen EA, King TA, Norton L, Benezra R. Tumor entrained neutrophils inhibit seeding in the premetastatic lung. Cancer Cell. 2011;20:300–314. doi: 10.1016/j.ccr.2011.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greten TF, Manns MP, Korangy F. Myeloid derived suppressor cells in human diseases. Int Immunopharmacol. 2011;11:802–807. doi: 10.1016/j.intimp.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellstrom I, Sjogren HO, Warner G, Hellstrom KE. Blocking of cell-mediated tumor immunity by sera from patients with growing neoplasms. Int J Cancer. 1971;7:226–237. doi: 10.1002/ijc.2910070206. [DOI] [PubMed] [Google Scholar]
- Hellstrom KE, Hellstrom I, Nelson K. Antigen-specific suppressor (“blocking”) factors in tumor immunity. Biomembranes. 1983;11:365–388. [PubMed] [Google Scholar]
- Hesse M, Modolell M, La Flamme AC, Schito M, Fuentes JM, Cheever AW, Pearce EJ, Wynn TA. Differential regulation of nitric oxide synthase-2 and arginase-1 by type 1/type 2 cytokines in vivo: granulomatous pathology is shaped by the pattern of L-arginine metabolism. J Immunol. 2001;167:6533–6544. doi: 10.4049/jimmunol.167.11.6533. [DOI] [PubMed] [Google Scholar]
- Hibbs JB, Jr, Taintor RR, Vavrin Z. Macrophage cytotoxicity: role for L-arginine deiminase and imino nitrogen oxidation to nitrite. Science. 1987;235:473–476. doi: 10.1126/science.2432665. [DOI] [PubMed] [Google Scholar]
- Holda JH, Maier T, Claman HN. Murine graft-versus-host disease across minor barriers: immunosuppressive aspects of natural suppressor cells. Immunol Rev. 1985;88:87–105. doi: 10.1111/j.1600-065x.1985.tb01154.x. [DOI] [PubMed] [Google Scholar]
- Huang B, Pan PY, Li Q, Sato AI, Levy DE, Bromberg J, Divino CM, Chen SH. Gr-1+CD115+ immature myeloid suppressor cells mediate the development of tumor-induced T regulatory cells and T-cell anergy in tumor-bearing host. Cancer Res. 2006;66:1123–1131. doi: 10.1158/0008-5472.CAN-05-1299. [DOI] [PubMed] [Google Scholar]
- Item CB, Stockler-Ipsiroglu S, Stromberger C, Muhl A, Alessandri MG, Bianchi MC, Tosetti M, Fornai F, Cioni G. Arginine:glycine amidinotrans-ferase deficiency: the third inborn error of creatine metabolism in humans. Am J Hum Genet. 2001;69:1127–1133. doi: 10.1086/323765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyer RK, Yoo PK, Kern RM, Rozengurt N, Tsoa R, O’Brien WE, Yu H, Grody WW, Cederbaum SD. Mouse model for human arginase deficiency. Mol Cell Biol. 2002;22:4491–4498. doi: 10.1128/MCB.22.13.4491-4498.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyo AH, Zhu MY, Ordway GA, Regunathan S. Expression of arginine decarboxylase in brain regions and neuronal cells. J Neurochem. 2006;96:1042–1050. doi: 10.1111/j.1471-4159.2005.03544.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen LC, Theilgaard-Monch K, Christensen EI, Borregaard N. Arginase 1 is expressed in myelocytes/metamyelocytes and localized in gelatinase granules of human neutrophils. Blood. 2007;109:3084–3087. doi: 10.1182/blood-2006-06-032599. [DOI] [PubMed] [Google Scholar]
- Kasic T, Colombo P, Soldani C, Wang CM, Miranda E, Roncalli M, Bronte V, Viola A. Modulation of human T-cell functions by reactive nitrogen species. Eur J Immunol. 2011;41:1843–1849. doi: 10.1002/eji.201040868. [DOI] [PubMed] [Google Scholar]
- Kato JY. Control of G1 progression by D-type cyclins: key event for cell proliferation. Leukemia. 1997;11(Suppl 3):347–351. [PubMed] [Google Scholar]
- Klausner RD, Lippincott-Schwartz J, Bonifacino JS. The T cell antigen receptor: insights into organelle biology. Annu Rev Cell Biol. 1990;6:403–431. doi: 10.1146/annurev.cb.06.110190.002155. [DOI] [PubMed] [Google Scholar]
- Ko JS, Rayman P, Ireland J, Swaidani S, Li G, Bunting KD, Rini B, Finke JH, Cohen PA. Direct and differential suppression of myeloid-derived suppressor cell subsets by sunitinib is compartmentally constrained. Cancer Res. 2010;70:3526–3536. doi: 10.1158/0008-5472.CAN-09-3278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kono K, Ressing ME, Brandt RM, Melief CJ, Potkul RK, Andersson B, Petersson M, Kast WM, Kiessling R. Decreased expression of signal-transducing zeta chain in peripheral T cells and natural killer cells in patients with cervical cancer. Clin Cancer Res. 1996a;2:1825–1828. [PubMed] [Google Scholar]
- Kono K, Salazar-Onfray F, Petersson M, Hansson J, Masucci G, Wasserman K, Nakazawa T, Anderson P, Kiessling R. Hydrogen peroxide secreted by tumor-derived macrophages down-modulates signal-transducing zeta molecules and inhibits tumor-specific T cell-and natural killer cell-mediated cytotoxicity. Eur J Immunol. 1996b;26:1308–1313. doi: 10.1002/eji.1830260620. [DOI] [PubMed] [Google Scholar]
- Kropf P, Baud D, Marshall SE, Munder M, Mosley A, Fuentes JM, Bangham CR, Taylor GP, Herath S, Choi BS, Soler G, Teoh T, Modolell M, Muller I. Arginase activity mediates reversible T cell hyporesponsiveness in human pregnancy. Eur J Immunol. 2007;37:935–945. doi: 10.1002/eji.200636542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kryczek I, Wei S, Zou L, Zhu G, Mottram P, Xu H, Chen L, Zou W. Cutting edge: induction of B7-H4 on APCs through IL-10: novel suppressive mode for regulatory T cells. J Immunol. 2006a;177:40–44. doi: 10.4049/jimmunol.177.1.40. [DOI] [PubMed] [Google Scholar]
- Kryczek I, Zou L, Rodriguez P, Zhu G, Wei S, Mottram P, Brumlik M, Cheng P, Curiel T, Myers L, Lackner A, Alvarez X, Ochoa A, Chen L, Zou W. B7-H4 expression identifies a novel suppressive macrophage population in human ovarian carcinoma. J Exp Med. 2006b;203:871–881. doi: 10.1084/jem.20050930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusmartsev S, Cheng F, Yu B, Nefedova Y, Sotomayor E, Lush R, Gabrilovich D. All-trans-retinoic acid eliminates immature myeloid cells from tumor-bearing mice and improves the effect of vaccination. Cancer Res. 2003;63:4441–4449. [PubMed] [Google Scholar]
- Kusmartsev S, Gabrilovich DI. STAT1 signaling regulates tumor-associated macrophage-mediated T cell deletion. J Immunol. 2005;174:4880–4891. doi: 10.4049/jimmunol.174.8.4880. [DOI] [PubMed] [Google Scholar]
- Kusmartsev S, Nefedova Y, Yoder D, Gabrilovich DI. Antigen-specific inhibition of CD8+ T cell response by immature myeloid cells in cancer is mediated by reactive oxygen species. J Immunol. 2004;172:989–999. doi: 10.4049/jimmunol.172.2.989. [DOI] [PubMed] [Google Scholar]
- Kusmartsev S, Su Z, Heiser A, Dannull J, Eruslanov E, Kubler H, Yancey D, Dahm P, Vieweg J. Reversal of myeloid cell-mediated immunosuppres-sion in patients with metastatic renal cell carcinoma. Clin Cancer Res. 2008;14:8270–8278. doi: 10.1158/1078-0432.CCR-08-0165. [DOI] [PubMed] [Google Scholar]
- Kuss I, Saito T, Johnson JT, Whiteside TL. Clinical significance of decreased zeta chain expression in peripheral blood lymphocytes of patients with head and neck cancer. Clin Cancer Res. 1999;5:329–334. [PubMed] [Google Scholar]
- Le HK, Graham L, Cha E, Morales JK, Manjili MH, Bear HD. Gemcitabine directly inhibits myeloid derived suppressor cells in BALB/c mice bearing 4T1 mammary carcinoma and augments expansion of T cells from tumor-bearing mice. Int Immunopharmacol. 2009;9:900–909. doi: 10.1016/j.intimp.2009.03.015. [DOI] [PubMed] [Google Scholar]
- Lee J, Ryu H, Ferrante RJ, Morris SM, Jr, Ratan RR. Translational control of inducible nitric oxide synthase expression by arginine can explain the arginine paradox. Proc Natl Acad Sci USA. 2003;100:4843–4848. doi: 10.1073/pnas.0735876100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Liu J, Park JK, Hamilton TA, Rayman P, Klein E, Edinger M, Tubbs R, Bukowski R, Finke J. T cells from renal cell carcinoma patients exhibit an abnormal pattern of kappa B-specific DNA-binding activity: a preliminary report. Cancer Res. 1994;54:5424–5429. [PubMed] [Google Scholar]
- Lu T, Ramakrishnan R, Altiok S, Youn JI, Cheng P, Celis E, Pisarev V, Sherman S, Sporn MB, Gabrilovich D. Tumor-infiltrating myeloid cells induce tumor cell resistance to cytotoxic T cells in mice. J Clin Invest. 2011;121:4015–4029. doi: 10.1172/JCI45862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RS, Shevach EM. Cutting edge: depletion of CD4+CD25+ regulatory T cells is necessary, but not sufficient, for induction of organ-specific autoimmune disease. J Immunol. 2002;168:5979–5983. doi: 10.4049/jimmunol.168.12.5979. [DOI] [PubMed] [Google Scholar]
- McHugh RS, Shevach EM, Margulies DH, Natarajan K. A T cell receptor transgenic model of severe, spontaneous organ-specific autoimmunity. Eur J Immunol. 2001;31:2094–2103. doi: 10.1002/1521-4141(200107)31:7<2094::aid-immu2094>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Miescher S, Stoeck M, Qiao L, Barras C, Barrelet L, von Fliedner V. Preferential clonogenic deficit of CD8-positive T-lymphocytes infiltrating human solid tumors. Cancer Res. 1988;48:6992–6998. [PubMed] [Google Scholar]
- Miescher S, Whiteside TL, Carrel S, von Fliedner V. Functional properties of tumor-infiltrating and blood lymphocytes in patients with solid tumors: effects of tumor cells and their supernatants on proliferative responses of lymphocytes. J Immunol. 1986;136:1899–1907. [PubMed] [Google Scholar]
- Mizoguchi H, O’Shea JJ, Longo DL, Loeffler CM, McVicar DW, Ochoa AC. Alterations in signal transduction molecules in T lymphocytes from tumor-bearing mice. Science. 1992;258:1795–1798. doi: 10.1126/science.1465616. [DOI] [PubMed] [Google Scholar]
- Morris SM., Jr Regulation of enzymes of the urea cycle and arginine metabolism. Annu Rev Nutr. 2002;22:87–105. doi: 10.1146/annurev.nutr.22.110801.140547. [DOI] [PubMed] [Google Scholar]
- Munder M, Eichmann K, Modolell M. Alternative metabolic states in murine macrophages reflected by the nitric oxide synthase/arginase balance: competitive regulation by CD4+ T cells correlates with Th1/Th2 phenotype. J Immunol. 1998;160:5347–5354. [PubMed] [Google Scholar]
- Munder M, Eichmann K, Moran JM, Centeno F, Soler G, Modolell M. Th1/Th2-regulated expression of arginase isoforms in murine macrophages and dendritic cells. J Immunol. 1999;163:3771–3777. [PubMed] [Google Scholar]
- Munder M, Mollinedo F, Calafat J, Canchado J, Gil-Lamaignere C, Fuentes JM, Luckner C, Doschko G, Soler G, Eichmann K, Muller FM, Ho AD, Goerner M, Modolell M. Arginase I is constitutively expressed in human granulocytes and participates in fungicidal activity. Blood. 2005;105:2549–2556. doi: 10.1182/blood-2004-07-2521. [DOI] [PubMed] [Google Scholar]
- Munder M, Schneider H, Luckner C, Giese T, Langhans CD, Fuentes JM, Kropf P, Mueller I, Kolb A, Modolell M, Ho AD. Suppression of T-cell functions by human granulocyte arginase. Blood. 2006;108:1627–1634. doi: 10.1182/blood-2006-11-010389. [DOI] [PubMed] [Google Scholar]
- Mundy-Bosse BL, Lesinski GB, Jaime-Ramirez AC, Benninger K, Khan M, Kuppusamy P, Guenterberg K, Kondadasula SV, Chaudhury AR, La Perle KM, Kreiner M, Young G, Guttridge DC, Carson WE., III Myeloid-derived suppressor cell inhibition of the IFN response in tumor-bearing mice. Cancer Res. 2011;71:5101–5110. doi: 10.1158/0008-5472.CAN-10-2670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagaraj S, Gupta K, Pisarev V, Kinarsky L, Sherman S, Kang L, Herber DL, Schneck J, Gabrilovich DI. Altered recognition of antigen is a mechanism of CD8+ T cell tolerance in cancer. Nat Med. 2007;13:828–835. doi: 10.1038/nm1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohm JE, Carbone DP. VEGF as a mediator of tumor-associated immuno-deficiency. Immunol Res. 2001;23:263–272. doi: 10.1385/IR:23:2-3:263. [DOI] [PubMed] [Google Scholar]
- Otsuji M, Kimura Y, Aoe T, Okamoto Y, Saito T. Oxidative stress by tumor-derived macrophages suppresses the expression of CD3 zeta chain of T-cell receptor complex and antigen-specific T- cell responses. Proc Natl Acad Sci USA. 1996;93:13119–13124. doi: 10.1073/pnas.93.23.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oyama T, Ran S, Ishida T, Nadaf S, Kerr L, Carbone DP, Gabrilovich DI. Vascular endothelial growth factor affects dendritic cell maturation through the inhibition of nuclear factor-kappa B activation in hemopoietic progenitor cells. J Immunol. 1998;160:1224–1232. [PubMed] [Google Scholar]
- Pan PY, Wang GX, Yin B, Ozao J, Ku T, Divino CM, Chen SH. Reversion of immune tolerance in advanced malignancy: modulation of myeloid derived suppressor cell development by blockade of SCF function. Blood. 2008;111:219–228. doi: 10.1182/blood-2007-04-086835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekarek LA, Starr BA, Toledano AY, Schreiber H. Inhibition of tumor growth by elimination of granulocytes. J Exp Med. 1995;181:435–440. doi: 10.1084/jem.181.1.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabinovich GA, Gabrilovich D, Sotomayor EM. Immunosuppressive strategies that are mediated by tumor cells. Annu Rev Immunol. 2007;25:267–296. doi: 10.1146/annurev.immunol.25.022106.141609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers S, Rees RC, Hancock BW. Changes in the phenotypic characteristics of eosinophils from patients receiving recombinant human interleukin-2 (rhIL-2) therapy. Br J Haematol. 1994;86:746–753. doi: 10.1111/j.1365-2141.1994.tb04824.x. [DOI] [PubMed] [Google Scholar]
- Rodriguez PC, Ernstoff MS, Hernandez C, Atkins M, Zabaleta J, Sierra R, Ochoa AC. Arginase I-producing myeloid-derived suppressor cells in renal cell carcinoma are a subpopulation of activated granulocytes. Cancer Res. 2009;69:1553–1560. doi: 10.1158/0008-5472.CAN-08-1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez PC, Hernandez CP, Morrow K, Sierra R, Zabaleta J, Wyczechowska DD, Ochoa AC. L-arginine deprivation regulates cyclin D3 mRNA stability in human T cells by controlling HuR expression. J Immunol. 2010;185:5198–5204. doi: 10.4049/jimmunol.1001224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez PC, Hernandez CP, Quiceno D, Dubinett SM, Zabaleta J, Ochoa JB, Gilbert J, Ochoa AC. Arginase I in myeloid suppressor cells is induced by COX-2 in lung carcinoma. J Exp Med. 2005;202:931–939. doi: 10.1084/jem.20050715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez PC, Quiceno DG, Ochoa AC. L-arginine availability regulates T-lymphocyte cell-cycle progression. Blood. 2007;109:1568–1573. doi: 10.1182/blood-2006-06-031856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez PC, Quiceno DG, Zabaleta J, Ortiz B, Zea AH, Piazuelo MB, Delgado A, Correa P, Brayer J, Sotomayor EM, Antonia S, Ochoa JB, Ochoa AC. Arginase I production in the tumor microenvironment by mature myeloid cells inhibits T-cell receptor expression and antigen-specific T-cell responses. Cancer Res. 2004;64:5839–5849. doi: 10.1158/0008-5472.CAN-04-0465. [DOI] [PubMed] [Google Scholar]
- Rodriguez PC, Zea AH, DeSalvo J, Culotta KS, Zabaleta J, Quiceno DG, Ochoa JB, Ochoa AC. L-arginine consumption by macrophages modulates the expression of CD3zeta chain in T lymphocytes. J Immunol. 2003;171:1232–1239. doi: 10.4049/jimmunol.171.3.1232. [DOI] [PubMed] [Google Scholar]
- Rotondo R, Barisione G, Mastracci L, Grossi F, Orengo AM, Costa R, Truini M, Fabbi M, Ferrini S, Barbieri O. IL-8 induces exocytosis of arginase 1 by neutrophil polymorphonuclears in nonsmall cell lung cancer. Int J Cancer. 2009;125:887–893. doi: 10.1002/ijc.24448. [DOI] [PubMed] [Google Scholar]
- Rutschman R, Lang R, Hesse M, Ihle JN, Wynn TA, Murray PJ. Cutting edge: Stat6-dependent substrate depletion regulates nitric oxide production. J Immunol. 2001;166:2173–2177. doi: 10.4049/jimmunol.166.4.2173. [DOI] [PubMed] [Google Scholar]
- Santhanam L, Lim HK, Lim HK, Miriel V, Brown T, Patel M, Balanson S, Ryoo S, Anderson M, Irani K, Khanday F, Di Costanzo L, Nyhan D, Hare JM, Christianson DW, Rivers R, Shoukas A, Berkowitz DE. Inducible NO synthase dependent s-nitrosylation and activation of arginase1 contribute to age-related endothelial dysfunction. Circ Res. 2007;101:692–702. doi: 10.1161/CIRCRESAHA.107.157727. [DOI] [PubMed] [Google Scholar]
- Schmielau J, Finn OJ. Activated granulocytes and granulocyte-derived hydrogen peroxide are the underlying mechanism of suppression of t-cell function in advanced cancer patients. Cancer Res. 2001;61:4756–4760. [PubMed] [Google Scholar]
- Semenza GL. Targeting HIF-1 for cancer therapy. Nat Rev Cancer. 2003;3:721–732. doi: 10.1038/nrc1187. [DOI] [PubMed] [Google Scholar]
- Serafini P, Meckel K, Kelso M, Noonan K, Califano J, Koch W, Dolcetti L, Bronte V, Borrello I. Phosphodiesterase-5 inhibition augments endogenous antitumor immunity by reducing myeloid-derived suppressor cell function. J Exp Med. 2006;203:2691–2702. doi: 10.1084/jem.20061104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seung LP, Rowley DA, Dubey P, Schreiber H. Synergy between T-cell immunity and inhibition of paracrine stimulation causes tumor rejection. Proc Natl Acad Sci USA. 1995;92:6254–6258. doi: 10.1073/pnas.92.14.6254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma P, Wagner K, Wolchok JD, Allison JP. Novel cancer immunotherapy agents with survival benefit: recent successes and next steps. Nat Rev Cancer. 2011;11:805–812. doi: 10.1038/nrc3153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sica A, Bronte V. Altered macrophage differentiation and immune dysfunction in tumor development. J Clin Invest. 2007;117:1155–1166. doi: 10.1172/JCI31422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh R, Pervin S, Karimi A, Cederbaum S, Chaudhuri G. Arginase activity in human breast cancer cell lines: N(omega)-hydroxy-L- arginine selectively inhibits cell proliferation and induces apoptosis in MDA-MB-468 cells. Cancer Res. 2000;60:3305–3312. [PubMed] [Google Scholar]
- Sinha P, Clements VK, Fulton AM, Ostrand-Rosenberg S. Prostaglandin E2 promotes tumor progression by inducing myeloid-derived suppressor cells. Cancer Res. 2007;67:4507–4513. doi: 10.1158/0008-5472.CAN-06-4174. [DOI] [PubMed] [Google Scholar]
- Sinha P, Clements VK, Ostrand-Rosenberg S. Interleukin-13-regulated M2 macrophages in combination with myeloid suppressor cells block immune surveillance against metastasis. Cancer Res. 2005b;65:11743–11751. doi: 10.1158/0008-5472.CAN-05-0045. [DOI] [PubMed] [Google Scholar]
- Sinha P, Clements VK, Ostrand-Rosenberg S. Reduction of myeloid-derived suppressor cells and induction of M1 macrophages facilitate the rejection of established metastatic disease. J Immunol. 2005a;174:636–645. doi: 10.4049/jimmunol.174.2.636. [DOI] [PubMed] [Google Scholar]
- Solheim JC, Reber AJ, Ashour AE, Robinson S, Futakuchi M, Kurz SG, Hood K, Fields RR, Shafer LR, Cornell D, Sutjipto S, Zurawski S, LaFace DM, Singh RK, Talmadge JE. Spleen but not tumor infiltration by dendritic and T cells is increased by intravenous adenovirus-Flt3 ligand injection. Cancer Gene Ther. 2007;14:364–371. doi: 10.1038/sj.cgt.7701018. [DOI] [PubMed] [Google Scholar]
- Solito S, Falisi E, az-Montero CM, Doni A, Pinton L, Rosato A, Francescato S, Basso G, Zanovello P, Onicescu G, Garrett-Mayer E, Montero AJ, Bronte V, Mandruzzato S. A human promyelocytic-like population is responsible for the immune suppression mediated by myeloid-derived suppressor cells. Blood. 2011;118:2254–2265. doi: 10.1182/blood-2010-12-325753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson FK. Update on cancer vaccines. Curr Opin Oncol. 2005;17:573–577. doi: 10.1097/01.cco.0000181406.60213.c7. [DOI] [PubMed] [Google Scholar]
- Taheri F, Ochoa JB, Faghiri Z, Culotta K, Park HJ, Lan MS, Zea AH, Ochoa AC. L-Arginine regulates the expression of the T-cell receptor zeta chain (CD3zeta) in Jurkat cells. Clin Cancer Res. 2001;7:958s–965s. [PubMed] [Google Scholar]
- Talmadge JE, Hood KC, Zobel LC, Shafer LR, Coles M, Toth B. Chemoprevention by cyclooxygenase-2 inhibition reduces immature myeloid suppressor cell expansion. Int Immunopharmacol. 2007;7:140–151. doi: 10.1016/j.intimp.2006.09.021. [DOI] [PubMed] [Google Scholar]
- Toh B, Wang X, Keeble J, Sim WJ, Khoo K, Wong WC, Kato M, Prevost-Blondel A, Thiery JP, Abastado JP. Mesenchymal transition and dissemination of cancer cells is driven by myeloid-derived suppressor cells infiltrating the primary tumor. PLoS Biol. 2011;9:e1001162–1001177. doi: 10.1371/journal.pbio.1001162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ginderachter JA, Meerschaut S, Liu Y, Brys L, De Groeve K, Hassanzadeh Ghassabeh G, Raes G, De Baetselier P. Peroxisome proliferator-activated receptor gamma (PPARgamma) ligands reverse CTL suppression by alternatively activated (M2) macrophages in cancer. Blood. 2006;108:525–535. doi: 10.1182/blood-2005-09-3777. [DOI] [PubMed] [Google Scholar]
- Varesio L, Giovarelli M, Landolfo S, Forni G. Suppression of proliferative response and lymphokine production during the progression of a spontaneous tumor. Cancer Res. 1979;39:4983–4988. [PubMed] [Google Scholar]
- Vincent J, Mignot G, Chalmin F, Ladoire S, Bruchard M, Chevriaux A, Martin F, Apetoh L, Rebe C, Ghiringhelli F. 5-Fluorouracil selectively kills tumor-associated myeloid-derived suppressor cells resulting in enhanced T cell-dependent antitumor immunity. Cancer Res. 2010;70:3052–3061. doi: 10.1158/0008-5472.CAN-09-3690. [DOI] [PubMed] [Google Scholar]
- Whiteside TL, Miescher S, Moretta L, von Fliedner V. Cloning and proliferating precursor frequencies of tumor-infiltrating lymphocytes from human solid tumors. Transplant Proc. 1988;20:342–343. [PubMed] [Google Scholar]
- Whiteside TL, Rabinowich H. The role of Fas/FasL in immunosuppression induced by human tumors. Cancer Immunol Immunother. 1998;46:175–184. doi: 10.1007/s002620050476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youn JI, Collazo M, Shalova IN, Biswas SK, Gabrilovich DI. Characterization of the nature of granulocytic myeloid-derived suppressor cells in tumor-bearing mice. J Leukoc Biol. 2012;91:167–181. doi: 10.1189/jlb.0311177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youn JI, Nagaraj S, Collazo M, Gabrilovich DI. Subsets of myeloid-derived suppressor cells in tumor-bearing mice. J Immunol. 2008b;181:5791–5802. doi: 10.4049/jimmunol.181.8.5791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youn JI, Nagaraj S, Collazo M, Gabrilovich DI. Subsets of myeloid-derived suppressor cells in tumor-bearing mice. J Immunol. 2008a;181:5791–5802. doi: 10.4049/jimmunol.181.8.5791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young MR, Newby M, Wepsic HT. Hematopoiesis and suppressor bone marrow cells in mice bearing large metastatic Lewis lung carcinoma tumors. Cancer Res. 1987;47:100–105. [PubMed] [Google Scholar]
- Zarour H, De Smet C, Lehmann F, Marchand M, Lethe B, Romero P, Boon T, Renauld JC. The majority of autologous cytolytic T-lymphocyte clones derived from peripheral blood lymphocytes of a melanoma patient recognize an antigenic peptide derived from gene Pmel17/gp100. J Invest Dermatol. 1996;107:63–67. doi: 10.1111/1523-1747.ep12298177. [DOI] [PubMed] [Google Scholar]
- Zea AH, Curti BD, Longo DL, Alvord WG, Strobl SL, Mizoguchi H, Creekmore SP, O’Shea JJ, Powers GC, Urba WJ. Alterations in T cell receptor and signal transduction molecules in melanoma patients. Clin Cancer Res. 1995;1:1327–1335. [PubMed] [Google Scholar]
- Zea AH, Rodriguez PC, Atkins MB, Hernandez C, Signoretti S, Zabaleta J, McDermott D, Quiceno D, Youmans A, O’Neill A, Mier J, Ochoa AC. Arginase-producing myeloid suppressor cells in renal cell carcinoma patients: a mechanism of tumor evasion. Cancer Res. 2005;65:3044–3048. doi: 10.1158/0008-5472.CAN-04-4505. [DOI] [PubMed] [Google Scholar]
- Zea AH, Rodriguez PC, Culotta KS, Hernandez CP, DeSalvo J, Ochoa JB, Park HJ, Zabaleta J, Ochoa AC. l-Arginine modulates CD3zeta expression and T cell function in activated human T lymphocytes. Cell Immunol. 2004;232:21–31. doi: 10.1016/j.cellimm.2005.01.004. [DOI] [PubMed] [Google Scholar]
- Zhang C, Hein TW, Wang W, Miller MW, Fossum TW, McDonald MM, Humphrey JD, Kuo L. Upregulation of vascular arginase in hypertension decreases nitric oxide-mediated dilation of coronary arterioles. Hypertension. 2004;44:935–943. doi: 10.1161/01.HYP.0000146907.82869.f2. [DOI] [PubMed] [Google Scholar]
- Zhu MY, Iyo A, Piletz JE, Regunathan S. Expression of human arginine decarboxylase, the biosynthetic enzyme for agmatine. Biochim Biophys Acta. 2004;1670:156–164. doi: 10.1016/j.bbagen.2003.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]