Abstract
Suicidal behavior and alcohol use are major public health concerns in the United States; however the association between these behaviors has received relatively little empirical attention. The relative lack of research in this area may be due in part to the absence of theory explaining the alcohol use-suicidality link in the general adult population. The present article expands upon Conner, McCloskey, and Duberstein’s (2008) model of suicide in individuals with alcoholism and proposes a theoretical framework that can be used to explain why a range of adult alcohol users may engage in suicidal behaviors. Guided by this model, we review and evaluate the evidence on the associations among several constructs that may contribute to suicidal behaviors in adult alcohol consumers. The current framework should inform future research and facilitate further empirical analyses on the interactive effects among risk factors that may contribute to suicidal behaviors. Once the nature of these associations is better understood among alcohol using adults, more effective suicide prevention programs may be designed and implemented.
Alcohol Use and Suicidal Behaviors among Adults: A Synthesis and Theoretical Model
Prevalence of Alcohol Use and Suicidal Behaviors
Suicidal behavior and alcohol use are major public health concerns in the United States (Centers for Disease Control and Prevention [CDC], 2007; Substance Abuse and Mental Health Services Administration [SAMHSA], 2009). Approximately 32,000 people die by suicide every year, making it the 11th leading cause of death in the United States (Kung, Hoyert, Xu, & Murphy, 2008). Researchers examining the prevalence of suicidal ideation in population studies have found rates that vary between 2.6% for recent suicidal thoughts to 14.1% for lifetime ideation (Kessler et al., 2005; Nock et al., 2008). Further, suicidal ideation is often the precursor of later suicide-related behavior (Crosby, Cheltenham, & Sacks, 1999), as approximately 32% of life-time suicide ideators eventually attempt suicide (Kessler, Berglund, Borges, Nock, & Wang, 2005; Kessler et al., 2005).
Alcohol use is common in Western society; it has been estimated that 90% of people consume alcohol at some point in their lives (Schuckit, 2005; Sher, 2006a). Moreover, researchers have found prevalence estimates of regular alcohol consumption in the United States to approach 50% (Dawson, Grant, Stinson, & Chou, 2004; Kessler et al., 2004) and roughly 12–15% of Americans have met criteria for alcohol dependence (Kessler & Wang, 2008; Rehm, Taylor, & Room, 2006). There are a variety of models that have been proposed to explain alcohol addiction including the social learning model, cognitive behavioral model, processual cause theory, common cause model, disease model, and moral model. A discussion of these models of addiction is beyond the scope of the current manuscript; however, we direct the reader to Margolis and Zweben’s (2011) for a recent comprehensive review of models and theories of alcohol addiction. The high prevalence of alcohol-related problematic behavior is also well documented (Johnson, O’Malley, Bachman, & Schulenburg, 2007) as are the associated consequences, which can include suicide (e.g., Ellis & Trumpower, 2008; Kisch, Leino, & Silverman, 2005). It is, therefore, important for researchers to examine alcohol use as a possible risk factor for subsequent engagement in suicidal behavior. Additionally, more universal models need to be developed and tested to explore this relation in the general population.
Association Between Alcohol Use and Suicidal Behaviors
Several studies indicate a strong association between alcohol use and suicidal behaviors (e.g., Borges, Walters, & Kessler, 2000; Conner, Li, Meldrum, Duberstein, & Conwell, 2003; Lamis, Malone, Langhinrichsen-Rohling, & Ellis, 2010). Specifically, alcohol use has been associated with increased rates of suicide ideation, attempts, and completions in cross-sectional studies (e.g., Crosby, Espitia-Hardeman, Hill, Ortega, & Clavel-Arcas, 2009; Kessler, Borges, & Walters, 1999; Schaffer, Jeglic, & Stanley, 2008). For example, Powell and colleagues (2001) found that drinking frequency, drinking quantity, and binge drinking were all associated with a greater likelihood of a serious suicide attempt. Additionally, there is substantial evidence in prospective longitudinal research that increased alcohol consumption predicts a higher frequency of suicide ideation (Wilcox et al., 2010), attempts (Robinson et al., 2010), and completions (Flensborg-Madsen et al., 2009).
Alcohol use is also associated with an increased likelihood of subsequent alcohol abuse and dependence (Hingson, Heeren, & Winter, 2006), which have been found to be related to suicidal behaviors (Sher, 2006b; Wojner et al., 2009). In a national survey, Kessler, Borges, and Walters (1999) found that alcohol dependent individuals are at a 4.6 times greater risk for suicidal ideation and a 6.5 times greater risk for attempted suicide than their nonalcoholic counterparts. Empirical reviews of cohort studies (Wilcox, Conner, & Caine, 2004) have demonstrated that heavy drinking and alcohol use disorders are strongly associated with completed suicide. Similarly, reviews of psychological autopsy studies (Cavanagh, Carson, Sharpe, & Lawrie, 2003; Giner et al., 2007) have found that chronic alcohol abuse, acute abuse, and dependence were present in 21% to 46% of all suicide deaths.
Acute alcohol use has also been implicated as a potent risk factor for attempted and completed suicide among individuals with and without a history of alcohol abuse or dependence (Brady, 2006; Lejoyeux et al., 2008; Powell et al., 2001). In a review of the literature, Cherpitel, Borges, and Wilcox (2004) found that on average 37% of suicide completers had been consuming alcohol at the time of their death. Furthermore, researchers directly measuring acute alcohol use by either the breath analyzer test or post-mortem blood alcohol level found a significant positive association between recent alcohol consumption and suicide attempts and completions (Borges & Rosovsky, 1996; Crosby et al., 2009). Likewise, two other studies examining case reports of suicide attempts further support the hypothesized relation between alcohol use and subsequent suicidal behavior (Hawton, Haigh, Simkin, & Fagg, 1995; Meilman, Pattis, & Kraus-Zeilmann, 1994). The researchers in both studies found that alcohol was a contributing factor in many of the suicide attempts. One explanation for the relation between the acute effects of alcohol intake and suicidal behavior is that intoxicated individuals use more lethal means (e.g., firearms) when attempting suicide, which often results in death (Sher et al., 2009). Although acute and chronic alcohol use and dependence promote risk for suicide ideation, attempts, and completions, several other interrelated risk factors contribute to an alcohol user’s engagement in suicidal behaviors.
Existing Models of the Relation Between Alcohol use and Suicidal Behaviors
Only a few models have been proposed to understand the role of alcohol use in suicidal behavior in adult populations (e.g., Conner, McClosky, & Duberstein, 2008; Hufford, 2001). These theoretical models describe the relationship as causal (i.e., alcohol precedes suicidal behavior) and suggest that alcohol use increases the likelihood of suicidal behavior through other established risk factors (e.g., depressive state). Although the models are in agreement that alcohol use is causally prior to suicidal behavior, disentangling the possible pathways from alcohol use to suicide is challenging, especially when theorized mediating or moderating variables are included in the models. It is, thus, important to consider the role of established contributory variables and the complex relationship each has to one another as well as with alcohol use and suicidal behaviors to better understand what drives an individual to overcome the most basic human instinct of all: self-preservation. Two of the existing conceptual frameworks (cusp catastrophe model and diathesis-stress model) are briefly discussed below.
Cusp Catastrophe Model
Hufford’s (2001) cusp catastrophe model attempts to explain the relationship between alcohol use and suicidal behavior by identifying two distinct pathways. Specifically, the distal (i.e., chronic use/alcohol dependence) and proximal (i.e., acute use/intoxication) pathways associated with alcohol use as well a host of other related variables form the cusp catastrophe model. The theory also distinguishes between several other distal (e.g., psychological disorders) and proximal (e.g., interpersonal loss) risk factors that may contribute to suicidal behavior, which Hufford (2001) describes as “any observable behavior engaged in for the purpose of bringing about immediate self-destruction” (p.798). The cusp catastrophe model posits that in order to transform underlying suicide vulnerability (i.e., distal risk) into immediate suicide risk and ultimate engagement in suicidal behaviors, proximal risk factors must be present. The model also theorizes that alcohol can decrease an individual’s capability to cope effectively. In sum, Hufford suggests that against a backdrop of alcohol dependence, distal (e.g., co-morbid psychopathology) and proximal (e.g., psychological distress) suicide risk factors may increase the probability that one will engage serious suicidal behavior.
Diathesis-Stress Model
Conner and colleagues’ (2008) diathesis-stress model identifies two sets of variables that may interact with each other to increase the risk of attempting and/or completing suicide among individuals dependent on alcohol. In this model, the researchers suggest that there are key predisposing and precipitating factors, which may contribute to an alcoholic’s suicidal act (Conner & Duberstein, 2004). The predisposing and precipitating factors in this model are analogous to the distal and proximal factors in the cusp catastrophe model. Specifically, predisposing risk factors are enduring vulnerabilities that increase the potential for an individual to engage in suicidal behaviors. Precipitating risk factors are events or mental health status changes (e.g., onset of a depressive episode), which may occur within close proximity of the time an individual is contemplating suicide or attempting to carry out his or her suicidal plans, which ultimately increase suicide risk. The model proposes that aggression/impulsivity and severe alcoholism increase the probability that interpersonal difficulties will occur and having a predisposition to negative affect and hopelessness may in turn cause a depressive episode and/or increase the likelihood that an individual will engage in a suicidal act (Conner et al., 2008). This conceptual framework is important because it considers the interrelationship of many suicide risk factors that are known to be common among individuals with alcoholism. However, there are some shortcomings with this specific diathesis-stress model explaining suicidal behaviors in individuals with alcoholism, which are emphasized and modified in the proposed theoretical model.
Limitations of Existing Models
The present comprehensive framework, which has expanded upon Conner and colleagues’ (2008) model, was developed to explain the role that predisposing factors may play in increasing (moderating) the risk for suicide among alcohol users in the general adult population. The first key advance is that, whereas extant models examine alcohol dependence and its association with suicidal behaviors, which precludes generalizability to other alcohol using samples, the current framework considers alcohol use at different levels (e.g., moderate drinkers, social drinkers, episodic drinkers, chronic abusers) making the model relevant to several adult populations. Second, some theorists investigate suicide attempts or completions as the ultimate outcome variable in their existing models, which often makes testing difficult given the low base-rate of these behaviors. In the present model, suicidal behaviors include ideation and attempts, which can be effectively assessed and encompass a range of behaviors on the suicidality continuum. Third, the present explanatory model extends existing work by presenting novel mediating and moderating effects among variables relating to suicidal behaviors beyond those incorporated in the current literature. Lastly, the theoretical framework incorporates additional risk factors that are especially relevant to individuals who consume alcohol.
Proposed Theoretical Model Relating Alcohol Use and Suicidal Behavior
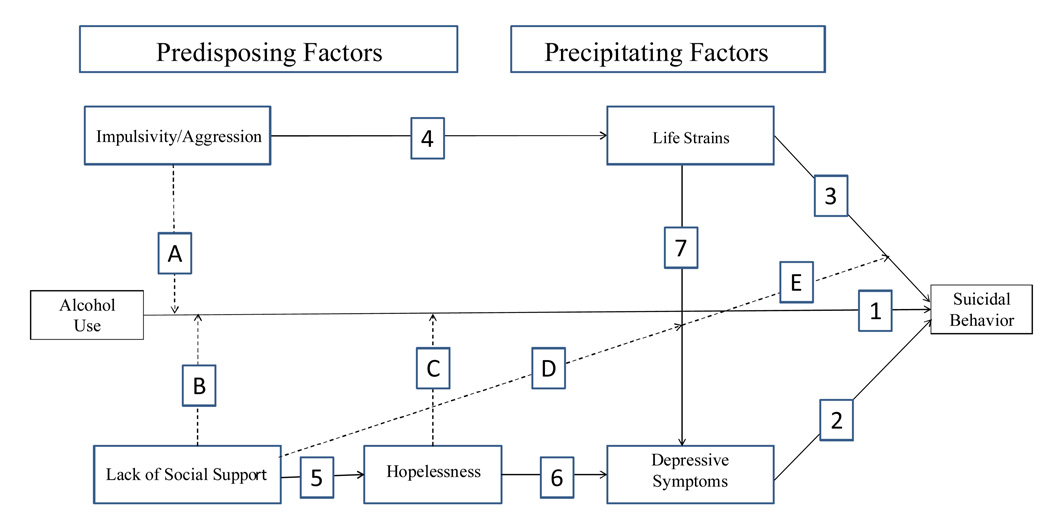
The purpose of the current paper is to review the literature on specific predisposing and precipitating risk factors for suicide among adults who consume alcohol and to provide a conceptual model, which may guide future research, have clinical implications, and enhance prevention efforts. The proposed theoretical framework (Figure 1) integrates previous research on the relations among alcohol use and several predisposing and precipitating factors for suicide in order to identify individuals who may be at an elevated risk for suicidal behaviors. It should be noted that the conceptual model depicted in Figure 1 is intended to highlight these other factors. Direct relations between alcohol use and the proposing factors, while not depicted, are included in this literature review. The framework incorporates aspects from the cusp catastrophe (Hufford, 2001) and diathesis-stress (Conner et al., 2008) models, but includes additional variables which are theorized to play an important role in the alcohol use-suicidality link. The unique suicide risk factors in the proposed model are social support (Arria et al., 2009; Joiner, 2005), depressive symptoms (in contrast to major depressive episode as presented in the diathesis-stress model; Lamis, Malone, & Langhinrichsen-Rohling, 2010), and alcohol-related problems (e.g., missed school or work, got into fights with others while drinking; Lamis & Malone, 2011). We propose that these risk factors, in combination with previously recognized constructs from past models, work in concert to exacerbate the risk for an alcohol-using individual to engage in suicidal behavior.
Figure 1.
Conceptual model of relations among the predisposing and precipitating factors and their moderation of the alcohol-suicide link.
Note. Direct and mediating paths are represented by solid lines and numbers. Broken lines and letters indicate moderating effects. Life strains include interpersonal difficulties, negative life events, and alcohol-related problems.
The framework was constructed to aid in understanding the interrelations among suicide risk factors associated with alcohol use. Specifically, we propose that aggression/impulsivity among individuals who consume higher levels of alcohol may lead to an increased risk of experiencing interpersonal difficulties, negative life events, and alcohol-related problems (these precipitating factors will hereafter be referred to as life strains when categorized as a group). These life strains in turn may precipitate depressive symptoms and/or cause an individual to be more likely to engage in suicidal behaviors, especially when in a context of low levels of social support. Moreover, the model implies that individuals who lack sufficient social support are more likely to have thoughts of or attempt suicide and experience depressive symptoms following life strains. Thus, the lack of social support acts as both a direct contributor to hopelessness and moderates life strains to increase the likelihood of developing depressive symptoms and engaging in suicidal behaviors.
Although many risk factors for suicide are known to exist in adult populations, not all of them can readily be incorporated into any one framework in the current state of the field. Expressly, our model does not reflect genetic influences (e.g., serotonin transported genotype), which have been found to significantly contribute to suicidal behaviors (Courtet et al., 2004) but will not be discussed further. Moreover, the framework does not address acute alcohol intoxication at the time of suicide. The construct “alcohol use” is included to illustrate the acute and chronic effects of alcohol consumption on the various risk factors for suicide; however, only chronic use is identified in the present model as having a direct association with suicidal behaviors in the present theoretical model, though acute alcohol use is discussed as it pertains to certain other variables which we do include. We chose this simplification on the grounds that acute alcohol intoxication, as it directly relates to suicidal behaviors may be more relevant for individuals with alcoholism as opposed to individuals who use alcohol in moderation. In addition, investigating levels of chronic alcohol use and its relation with key predisposing and precipitating risk factors for suicide should provide sufficient information about alcohol as a contributing factor to why individuals may consider or attempt to end their own lives.
Alcohol Use and Suicidal Behavior: A Conceptual Model
The proposed conceptual model of suicidal behavior among adults who consume alcohol is depicted in Figure 1. The summary in this section is presented without citations for the sake of clarity; a detailed review of the literature follows. Predisposing factors (impulsivity/aggression, lack of social support, hopelessness) are theorized to increase or moderate risk for suicidal behaviors among alcohol users (path 1). Specifically, impulsivity/aggression (path A) is conceptualized as an externalizing variable in the model, social support (path B) is considered an interpersonal construct, and hopelessness (path C) is defined as an internalizing construct. Furthermore, in addition to the moderating role that social support plays in amplifying the risk for suicidal behaviors among alcohol users (i.e., path B), a lack of social support also functions as a moderator for other relationships contributing to suicidality in the model, which are discussed in more detail below. All of these moderating predisposing factors are represented by dotted lines in Figure 1 and are proposed to place individuals at an elevated risk for engaging in suicidal behaviors.
As the theoretical framework suggests, individuals who consume alcohol are more likely to be impulsive and/or aggressive, which in turn promotes risk for experiencing life strains (path 4) including interpersonal difficulties, negative life events, and alcohol-related problems. Similarly, alcohol users who lack social support are more likely to feel hopeless (path 5) which increases their risk of experiencing depressive symptoms (path 6), especially in the context of life strains. Consequently, individuals who encounter these life strains can take one of two paths according to the model. First, it is proposed that a direct pathway from life strains to suicidal behaviors (path 3) may occur and a lack of social support moderates (increases) this association (path E). In essence, the likelihood that an individual will subsequently engage in suicidal behaviors following life strains is increased if they lack sufficient social support networks. Second, alcohol users who experience life strains may begin to suffer from symptoms of depression (path 7) and a lack of social support may also moderate this relationship (path D). Correspondingly, on this pathway, the connection between life strains and depressive symptoms is strengthened when individuals who consume alcohol lack adequate social support. Moreover, depressive symptoms are a frequent precursor of suicidal behaviors (path 2) and may also mediate the relation between life strains and suicidality (paths 7 and 2), particularly among alcohol consumers. In sum, the interrelationship among all of the elements in the proposed model confers significant risk for the engagement in suicidal behaviors among alcohol users.
Organization of Proposed Model
Topics are organized as they become relevant in the proposed theoretical framework (see Figure 1). Ideally, all articles will include adult populations; however, some research presented is comprised of alternative samples as there were no available studies on the population of interest (i.e. adults). We introduce, discuss, and integrate relevant empirical research articles among adults and/or adult aged alcohol consumers related to: 1) alcohol use and its association with predisposing risk factors for suicide (i.e., impulsivity/aggression, lack of social support, hopelessness); 2) the associations between predisposing and precipitating risk factors for suicide; 3) the associations among precipitating risk factors (i.e. life strains and depressive symptoms); 4) the associations between precipitating risk factors and suicidal behaviors; 5) methodological considerations for future research; 6) implications for prevention and treatment; and 7) summary and conclusions.
REVIEW OF EMPIRICAL LITERATURE
Relation of Alcohol Use to Predisposing Suicide Risk Factors
The variables (i.e., impulsivity/aggression, social support, hopelessness) discussed are associated with alcohol use and have been identified as important risk factors for suicidal behavior (Arria et al., 2009; Stephenson, Pena-Shaff, & Quirk, 2006). In the proposed model, these variables are conceptualized as predisposing risk factors for suicide that are particularly relevant for individuals who consume alcohol. Specifically, alcohol users are more likely to engage in impulsive and aggressive behaviors, lack social support, and experience hopelessness. These predisposing factors, in turn, increase the risk for experiencing precipitating factors directly related to suicidal behaviors among individuals who consume alcohol. The association between predisposing and precipitating risk factors for suicide, as well as moderating and mediating effects of specific constructs, are discussed as they become relevant in the theoretical framework.
Alcohol Use and Impulsivity/Aggression
Research has shown that individuals who consume alcohol are at a higher risk of engaging in impulsive and aggressive behaviors (Bacskai, Czobor, & Gerevich, 2008). One recent study (Magid & Colder, 2007) demonstrated that individuals who expressed a lack of premeditation and high sensation seeking, both personality traits that researchers (e.g., Whiteside & Lynam, 2001) have proposed are important dimensions constituting the construct of impulsivity, engaged in increased levels of alcohol consumption. These findings are consistent with previous research (e.g., Dick et al., 2010) suggesting that there is a strong association between impulsivity and alcohol use.
Although there is a wealth of data supporting the impulsivity-alcohol use link, there is controversy regarding the causality of this relationship. Some researchers (e.g., Carlson, Johnson, & Jacobs, 2010; Krueger, Markon, Patrick, Benning, & Kramer, 2007) assert that impulsivity is predictive of later alcohol use, while others (e.g., Goldstein & Volkow, 2002; Marczinski, Abroms, Van Selst, & Fillmore, 2005) believe that increased alcohol use may trigger impulsive behavior. As Goldstein and Volkow (2002) and others (e.g., Bond, 1998; Lyvers, 2000) have concluded, acute and chronic alcohol use may induce disinhibitory states in which individuals engage in impulsive and sensation seeking behaviors that they would normally hold back. Conversely, Krueger and colleagues (2007) found that problematic impulsivity independently contributed to externalizing disorders and impulsivity plays a significant role in alcohol use behaviors, suggesting that impulsive individuals may have difficulty refraining from consuming alcohol even when faced with the possibility of encountering negative consequences. Additional research has shown impulsivity to be positively related to earlier drinking onset (Zernicke, Cantrell, Finn, & Lucas, 2010), binge drinking (Carlson et al., 2010), alcohol abuse (Benjamin & Wulfert, 2005), and alcoholism (Dom, Hulstijn, & Sabbe, 2006). Regardless of the causality of the association between impulsivity and alcohol use, there is a large body of evidence connecting these two behaviors in a variety of samples.
Aggression is another important behavioral characteristic that has been reported to be associated with alcohol use (Giancola, 2002; Krueger et al., 2007; Tremblay & Ewart, 2005). Although impulsivity and aggression are correlated traits and may have an underlying biological component (Bailey & Ostrov, 2008), research has shown aggression to be a distinct construct significantly related to alcohol use even after controlling for impulsive behaviors (Parrott & Giancola, 2006). In a recent study, Gerevich, Bacskai, and Czobor (2007) compared trait-aggression levels between inpatient with alcoholism and a sample drawn from the general population. They identified significantly higher levels of trait aggression in the individuals with alcohol dependence. In a follow-up study, the same researchers (Bacskai et al., 2008) found significant correlations between alcohol use and aggression in the inpatient and population samples. In a regression analysis, however, their results demonstrated a significant association between alcohol use and aggression in the population sample, but not in the clinical inpatient sample, suggesting that lesser quantities of alcohol may be needed to initiate the same aggressive response in the alcohol-dependent individuals than it does in non-dependent individuals (Bacskai et al., 2008). This outcome supports the notion that aggression and alcohol use are related in a range of adult populations.
Acute alcohol consumption has also been found to be related to aggression in a number of other studies (e.g., Fals-Stewart, 2003). Chermack and Blow (2002) revealed that general alcohol consumption patterns, as well as alcohol use on the day of the conflict situation, were significantly associated with aggression and aggression severity. The results of this study not only replicate findings from previous research (e.g., Swahn, Simon, Hammig, & Guerrero, 2004) suggesting general alcohol consumption is associated with aggression, but also lend support to the contention that acute alcohol use is a potent predictor of aggressive behaviors. To explain the acute alcohol use-aggression link, Giancola (2002) proposes that aggressive behaviors occur when an intoxicated individual experiences a temporary state of lowered inhibitions and impairment in cognitive functioning resulting in the inability to control aggressive thoughts and actions. In sum, there is a wealth of literature on the relation between the overlapping traits of impulsivity and aggression and alcohol use, and although the nature of these associations is not completely understood, it is imperative that these constructs continue to be investigated, especially as they relate to other problem behaviors.
Alcohol Use and Social Support
Alcohol use and social support have been found to be related in multiple studies (e.g., Borsari & Carey, 2006; Menagi, Harrell, & June, 2008). Social support is defined in many ways throughout the literature (Williams, Barclay, & Schmied, 2004); however, the broad construct of social support refers to the availability of support from interpersonal relationships with family, friends, and/or a significant others, which provide formal and informal sources of help (Fowler & Hill, 2004; Zimet, Dahlem, Zimet, & Farley, 1988). A lack of quality relationships, peer interactions, and alienation from others may facilitate drinking (Borsari & Carey, 2006). Pauley and Hesse (2009) found that social support from others was negatively related to the quantity of alcohol consumed in a sample of college students. Further, in a multi-wave prospective study, Peirce, Frone, Russell, Cooper, and Mudar (2000) demonstrated that increased alcohol consumption leads to reduced contact with family, friends, and groups. This finding is in line with previous research suggesting that solitary drinkers consume more alcohol and are at an increased risk for developing alcohol problems than are individuals who consume alcohol in social situations (Gonzalez, Bradizza, & Collins, 2009). Similarly, Zalenski, Levey-Thors, and Schiaffino (1998) found that participants who perceived less social support from their friends and family reported consuming higher amounts of alcohol than individuals who experienced adequate or elevated levels of social support. The above empirical research findings lend credence to the assertion that the quality and quantity of social support networks and interpersonal relationships may have a reciprocal negative association with alcohol consumption in adult populations.
Alcohol Use and Hopelessness
Hopelessness has been defined as a group of negative expectancies concerning oneself and ones’ future life (Beck, Weissman, Lester, & Trexler, 1974), and has been found to be associated with a host of health risk behaviors including alcohol use and abuse (Ilhan, Demirbas, & Dogan, 2007). Sitharthan, Hough, Sitharthan, and Kavanaugh (2001) found that problem drinking and alcohol dependence were both significantly correlated with hopelessness in adult samples. Longitudinal research has also shown that binge drinking predicts subsequent decreases in perceived life chances, which is an assessment of achieving future adaptive life goals (Griffin, Botvin, Nichols, & Scheir, 2004). The authors of this longitudinal work concluded that individuals who binge drink may be less likely to believe they will achieve future success in life (e.g., finding a job that pays well) in turn developing a sense of hopelessness (Griffin et al., 2004). Conversely, Bolland (2003) found that hopelessness predicted high levels of weekly alcohol consumption and binge drinking in a large sample of predominantly African-American youth. This finding is consistent with the self-medication hypothesis (Khantzian, 1997), which proposes that individuals consume alcohol to regulate negative affect and relieve feelings of hopelessness. The available research linking alcohol use to hopelessness suggests that the variables may have a reciprocal relationship, which supports previous studies (e.g., Jaffee, & D'Zurilla, 2009). Although the temporal relationship between these two variables remains unclear, the salience of their observed association should not be ignored by future researchers.
The Associations between Predisposing and Precipitating Factors for Suicidal Behavior
In keeping with the current model, we argue that individuals who use alcohol are at an elevated risk of being predisposed to specific risk markers, which in turn, increases their likelihood of experiencing precipitating factors (i.e., life strains, depressive symptoms), which subsequently may contribute to suicidal behaviors. The relationship between predisposing and precipitating risk factors for suicide among alcohol users is complex and the path to suicidal behaviors is not consistent. For example, depressive symptoms may mediate the relationship between life strains and suicidal behavior; yet, an individual who is experiencing a life strain does not necessarily have to be depressed to have suicidal thoughts or attempt suicide. Nevertheless, the risk for suicide is at its highest when all of the variables in the model are present and work together in the proposed manner.
Further, only one of the life strains (i.e., interpersonal difficulties, negative life events, and alcohol-related problems) needs to be present to confer a heightened risk for depressive symptoms and suicide among alcohol consumers and the risk is progressively amplified as the number and severity of life strains increases. Although these life strains are similar and have been found to be correlated in some studies (e.g., Löckenhoff, Terracciano, Patriciu, Eaton, & Costa, 2009), they are distinct constructs that often result in negative outcomes due to one’s impulsivity and aggressive personality and/or behaviors. In order to distinguish among these related variables, the following definitions are provided. Interpersonal difficulties are recurrent problems relating to others that characterize an individuals’ functioning in interpersonal situations and are sources of subjective distress (Horowitz, 2004). Negative life events in the proposed model refer to recent events evaluated by an individual as having a negative influence on his or her quality of life (Sarason, Johnson, & Siegel, 1978) such as legal difficulties or a death in the family, but excluding events involving interpersonal conflicts. Alcohol-related problems are defined as adverse consequences directly related to alcohol use including mild (e.g., hangover, embarrassed yourself while intoxicated) to more severe consequences (e.g., DUI, workplace dismissal, motor vehicle accident) as a result of the individual’s drinking behavior (Devos-Comby, & Lange, 2008). Although it is clear that these life strains often overlap, the source of the negative outcomes can be quite different and have been included in the model to capture all of the experiences which may cause distress in one’s life. These variables and their relation to impulsivity/aggression are discussed in turn.
Impulsivity/Aggression and Interpersonal Difficulties
Many stressful life events and problems along with how they are managed can be explained by an individual’s inherent personality traits (Connor-Smith, & Flachsbart, 2007). Cluster B personality disorders, particularly borderline personality disorder (BPD) and antisocial personality disorder (ASPD), include symptoms of aggression and impulsivity as well as tumultuous interpersonal relationships (American Psychiatric Association, 2000). As previously noted, impulsivity and aggression are correlated traits that may share biological underpinnings (Bailey & Ostrov, 2008; Mann, Brent, & Arango, 2001), and impulsive and aggressive behaviors have been found to precede interpersonal difficulties in a number of studies (e.g., Tragesser & Robinson, 2009; Rogge, Bradbury, Hahlweg, Engl, & Thurmaier, 2006).
Some researchers (e.g., Mann, Waternaux, Haas, & Malone, 1999; Siever, 2002) have argued for a construct combining these two characteristics into a single variable. Mann and colleagues (1999) suggest that a trait factor, aggression/impulsivity, which assesses externally directed aggression and impulsivity concurrently, predisposes one to an increased risk of engaging in suicidal acts. Research has shown that this combined factor, which has also been termed “impulsive aggression” is associated with interpersonal difficulties (Conner, Duberstein, Conwell, & Caine, 2003; Poulin & Boivin, 2000). Koenigsberg and colleagues (2001) found that higher levels of impulsive aggression were significantly related to unstable interpersonal relationships in a sample of personality disordered patients. Similarly, Tragesser and Robinson (2009) corroborated these findings in a sample of undergraduate college students. These results support the contention that individuals who possess impulsive and aggressive personality traits and display these behaviors are prone to interpersonal difficulties.
Moreover, in a longitudinal study of young adult newlywed couples, Rogge and Bradburry (1999) found that aggression in early marriage successfully distinguished between married couples and those who were either separated or divorced 4 years later lending further evidence to the assertion that aggression may be a risk factor for subsequent interpersonal difficulties. The finding linking impulsivity and aggression to interpersonal difficulties should come as no surprise given that individuals who are aggressive and who exhibit poor impulse control are more likely to disrupt an interpersonal relationship due to their hostile behaviors toward others. The use of alcohol may contribute to aggressive and impulsive behaviors (Parrot & Giancola, 2006), which in turn potentiates an increased risk for experiencing interpersonal difficulties (Preuss, Koller, Barnow, Eikmeier, & Soyka, 2006; Quigley & Leonard, 1999). This theorized temporal pattern is in line with the proposed conceptual model of predisposing factors influencing precipitating factors for suicide among alcohol users.
Impulsivity/Aggression and Negative Life Events
Researchers have found significant positive correlations between negative life events, aggression (Rowe, Maughan, & Eley, 2006), and impulsivity (Wingenfeld et al., 2009). Mauchnik, Schmahl, and Bohus (2005) and other researchers (e.g., Wagner, Baskaya, Dahmen, Lieb, & Tadic, 2010) assert that negative life events and stressors are important correlates of impulsive aggression in adult patients diagnosed with BPD. Although much of the literature on the relations of these variables has been conducted in personality disordered samples (e.g., Beauchaine, Klein, Crowell, Derbidge, & Gatzke-Kopp, 2009), the available research on non-psychiatric populations has shown similar associations. For example, Haden, Scarpa, and Stanford (2008) found significant positive associations between impulsive aggression and negative life events in a college student sample. In line with this result and further supporting the proposed theoretical model, Taylor (2005) found that Cluster B personality disorder symptoms (impulsivity, erratic behavior) in college students significantly contributed to the likelihood of experiencing negative life events, and the relationship between these two variables was more robust when the individual also met criteria for alcohol abuse. This finding suggests that individuals who consume alcohol and display impulsive and aggressive behaviors are more prone to negative life events, with the exception of an event out of their control (e.g., death in the family). These negative life events may, in turn, place an individual at an increased risk for subsequent depression and/or suicidal behaviors.
Impulsivity/Aggression and Alcohol-Related Problems
Research has consistently shown an association between initial alcohol consumption and the development of later alcohol-related problems (Livingston & Room, 2009; Park, 2004). Moreover, several studies have demonstrated that alcohol users who act impulsively and/or aggressively are at an increased risk to experience alcohol-related negative consequences (Magid, Maclean, & Colder, 2007; Simons, Carey, & Gaher, 2004). Simons, Gaher, Correia, Hansen, and Christopher (2005) reported that impulsivity was directly associated with alcohol-related problems in a sample of young adults suggesting that impaired impulse control leads to behaviors that may cause an individual to experience negative consequences related to alcohol use. Congruent with this result and previous longitudinal research (e.g., Simons, 2003), a similar study (Leeman, Toll, Taylor, & Volpicelli, 2009) investigated impulsivity and alcohol-related problems both cross-sectionally and prospectively among undergraduate college students. The authors found that impulsivity was significantly correlated with alcohol-related problems at Time 1 (i.e., freshman year), and impulsivity at Time 1 prospectively predicted alcohol-related problems at Time 2 (i.e., senior year) even after controlling for alcohol-related problems at Time 1 (Leeman et al., 2009). They concluded that impulsivity is a strong predictor of subsequent alcohol-related problems in young adult drinkers (Leeman et al., 2009). These studies suggest that individuals who act impulsively and may not consider the possible negative consequences of their actions are more prone to engage in problem drinking. This same pattern of increased risk of experiencing alcohol-related problems is evident in individuals who consume alcohol and behave in an aggressive manner.
Much of the available research on aggressive behaviors and alcohol related-problems has been conducted among individuals involved in intimate relationships (e.g., Quigley & Leonard, 1999). For example, Keller, El-Sheikh, Keiley, and Liao (2009) reported that verbal and physical aggression in couples was a significant predictor of alcohol-related problems over time and concluded that aggression may cause stress and inhibit coping abilities, which in turn results in individuals being more susceptible to experience alcohol-related problems. In a related study (Lamis, Malone, & Langhinrichsen-Rohling, 2010) conducted in college women, the researchers observed a significant positive correlation between psychological aggression, as measured by the psychological aggression subscale of the Conflict Tactics Scale – 2 (Straus, Hamby, Boney-McCoy, & Sugarman, 1996), and alcohol-related problems. The authors of this work propose a model suggesting that women involved in a psychologically aggressive relationship may turn to alcohol as a coping mechanism for the emotional pain, which may then place them at an increased risk for developing and experiencing alcohol-related problems (Lamis et al., 2010). Although the results generated from these studies indicate a relation between aggressive relationship behaviors and alcohol-related problems, the current model theorizes that aggression of any nature confers risk of experiencing alcohol-related problems in adults. The model further proposes that when an individual acts both impulsively and aggressively, he/she is at the highest risk of problem drinking. In keeping with the present theoretical framework, we argue that alcohol-related problems in addition to negative life events and interpersonal difficulties promote risk for depression and suicidal behaviors, especially when an individual does not have a strong social support network and experiences feelings of hopelessness.
Low Social Support, Hopelessness, and Depressive Symptoms
Recent research has consistently reported significant associations among social support, hopelessness, and depression, all of which have been found to predict suicidal behavior (King et al., 2009). In keeping with the present model, we offer support from previous research and argue for the theorized relations among these variables (see Figure 1). Specifically, a lack of social support is assumed to be causally prior to hopelessness, which in turn is modeled as occurring prior to depressive symptoms. Although these psychological and interpersonal factors for suicide are related to each other, only a handful of studies have examined the causal nature of these associations and considered the possible mediating role of hopelessness in the social support-depressive symptoms link.
Researchers have found a lack of social support to be significantly associated with increased hopelessness in numerous studies (e.g., Golden et al., 2009). Social support from family and peers, in particular, seem to be a strong predictor of hopelessness in samples of adolescents and young adults (Chioqueta & Stiles, 2007; Kerr, Preuss, & King, 2006). For example, Thompson, Mazza, Herting, Randell, and Eggert (2005) demonstrated a lack of family support was a stronger predictor of hopelessness than it was for depression. The researchers also tested potential mediating effects of hopelessness and depression in the relation between lack of family social support and suicidal behaviors. They found that the lack of family social support indirectly influenced suicidal behavior through its effects on both hopelessness and depression (Thompson et al., 2005). Moreover, in a longitudinal investigation of spinal cord injury sufferers, Beedie and Kennedy (2002) found that quality, but not quantity of social support was a significant negative predictor of hopelessness, suggesting that one’s perceived satisfaction with the social support received is more important than amount with regards to experiencing subsequent feelings of hopelessness.
In another longitudinal study, Johnson and colleagues (2001) reported that a lack of social support predicted increases in hopelessness, which in turn predicted an increase in depression. Further analyses revealed that hopelessness partially mediated the prospective association between lack of social support and depressive symptoms (Johnson et al., 2001) supporting the temporal precedence of these factors in the proposed theoretical model. There is a large body of research indicating a strong correlation between hopelessness and depressive symptoms (Hirsch, Wolford, LaLonde, Brunk, & Parker-Morris, 2009; Soares, Macassa, Grossi, & Viitasara, 2008). Much less longitudinal research has been conducted examining the causal direction of these constructs, particularly in the absence of other possible confounding variables. In the prospective studies identified (e.g., Alford, Lester, Patel, Buchanan, & Giunta, 1995; Hankin, Abramson, Miller, & Haeffel, 2004; Joiner, Wingate, & Otamendi, 2005), hopelessness significantly predicted depressive symptoms, but not vice versa. In a sample of university students, Joiner and colleagues (2005) found that hopelessness at Time 1 (baseline) significantly predicted increases in depressive symptoms from Time 1 to Time 2 (5 weeks later) even after controlling for interpersonal life stressors. Moreover, results from a similar longitudinal study of young adults (Alford et al., 1995) revealed that hopelessness at baseline significantly predicted depressive symptoms 4 weeks later above and beyond negative life events. These corroborated findings are consistent with prior research (e.g., Rholes, Riskind, & Neville, 1985) suggesting that hopelessness precedes depression in adults and further supports the proposed theoretical framework.
The Associations among Precipitating Factors
Life Strains and Depressive Symptoms
Multiple studies (e.g., Geisner, Larimer, & Neighbors, 2004; Uhrlass & Gibb, 2007) have demonstrated that individuals who have encountered interpersonal difficulties, negative life events, and/or alcohol related problems are at an increased risk of developing and experiencing depressive symptoms. For example, Murphy, McDevitt-Murphy, and Barnett (2005) found that young adults who experience alcohol-related problems report a diminished global sense of well-being and less life-satisfaction. Consistent with these results, previous research (e.g., Martens et al., 2008) has revealed similar findings providing support for the relation between alcohol-related problems and depressive symptoms. Taken together, these results indicate that the negative consequences associated with alcohol use may precipitate the onset and development of depressive symptoms in adult populations.
Likewise, depressive symptoms have been shown to be a significant correlate of interpersonal difficulties (Barrett & Barber, 2007) and negative life events (Bjorck & Thurman, 2007). In a longitudinal study of university undergraduate students, O’Neill, Cohen, Tolpin, and Gunthert (2004) found interpersonal difficulties and negative life events to prospectively predict depressive symptoms. These findings are in accordance with the results from a national survey population study where the researchers reported recent interpersonal problems and life events to be significantly associated with depression (Jordanova et al., 2007). Further, researchers (e.g., Rafnsson, Jonsson, & Windle, 2006; Sher et al., 2008) have found these life strains to be significant predictors of depression and depressive symptoms among alcohol users. Although the above studies clearly reveal a link between life strains and depressive symptoms, the mechanisms underlying this relation are often unclear. One central cognitive theory that has been posited and makes an effort to elucidate these associations is the hopelessness theory of depression (Abramson, Metalsky, & Alloy, 1989).
The hopelessness theory of depression presents a vulnerability-stress model that postulates that a negative attributional style will contribute to increases in depressive symptomatology following the occurrence of negative life events (Abramson et al., 1989). The stress that often accompanies life strains has been implicated in the onset and course of depression (Hammen, 2005; Safford, Alloy, Abramson, & Crossfield, 2007); however, not every individual who experiences life strains and associated distress suffers from symptoms of depression (Caspi et al., 2003). According to the hopelessness theory of depression (Abramson et al.), an individual who encounters a negative life event (or more generally a life strain in the current model) and attributes this event to stable and global causes (i.e., negative attributional style) should be more vulnerable to develop depressive symptoms. Moreover, the theory posits that hopelessness predicts depressive symptoms and is a proximal cause of “hopelessness depression”, a subtype of depression (Alloy et al., 2000). The hopelessness theory of depression has been supported by a number of prospective studies (e.g., Hankin, Fraley, & Abela, 2005; Hankin et al., 2004); however, results appear to be more consistent in adult populations as opposed to child and adolescent samples (Gibb & Coles, 2005). For instance, Hankin and colleagues (2004) demonstrated that stressful life events significantly predicted depressive symptomatology in a short term (5 weeks) follow-up, a long term (2 year) follow-up, and a 3 time point longitudinal design study in a sample of undergraduate students. Although negative attributional style is not incorporated into the current proposed model as a contributory cause for the development and course of depressive symptoms, the hopelessness theory of depression provides additional support for the influences that life strains and hopelessness have on depressive symptoms in adults.
Further evidence supporting the current model is presented in the expanded hopelessness theory of depression (Panzarella, Alloy, & Whitehouse, 2006), which includes the effect of social support as a protective factor against experiencing depressive symptoms. Specifically, the expanded theory proposes that social support reduces the likelihood that an individual will experience depressive symptoms after encountering a life strain by acting as a buffer in the relationship (Panzarella et al., 2006). Indeed, Panzarella and associates (2006) found that higher levels of adaptive inferential feedback, a specific subtype of social support, were associated with more adaptive inferences to negative life events encountered as well as reduced levels of depressive symptoms and hopelessness depression in a longitudinal investigation of young adults. These findings are in line with the buffer theory of social support (Cohen & Wills, 1985), which suggests that individuals who believe they can rely on others for support may not perceive life strains to be as significant or detrimental to their well-being as those who do not have strong support networks. Cohen and Wills (1985) also theorize that the degree of support provided by others attenuates the response to life strains by decreasing the likelihood of making maladaptive inferences and promoting adaptive coping strategies. This buffering effect of social support in the relationship between life strains and depressive symptoms lends evidence to the contention that social support may act as a moderating variable between these constructs in the proposed theoretical framework.
The Direct Association between Precipitating Factors and Suicidal Behaviors
Depressive Symptoms and Suicidal Behaviors
Research has consistently shown that depressive symptoms are a frequent precursor to suicidal ideation and attempts (Nock et al., 2009; Wilcox, 2010). Findings from a nationally representative sample of young adults demonstrated that the majority of individuals (94.9%) who seriously considered suicide also reported experiencing severe depressive symptoms at least once during the previous 12 months (Kisch et al., 2005). Along these lines, individuals with severe symptoms of depression were more likely to have current thoughts of suicide than those with mild to moderate symptoms (Garlow et al., 2008). Further, depressive symptoms have also been found to predict subsequent suicide attempts (Verona, Sachs-Ericsson, & Joiner, 2004). In a longitudinal study of young adults, Nrugham, Holen, and Sund (2010) revealed that suicide attempters experienced persistent and significantly higher levels of depressive symptoms than nonattempters. Similarly, Oquendo and colleagues (2004) found that severity of depressive symptoms at baseline prospectively predicted future suicidal acts. Although the proposed theoretical framework does not focus on the act of completed suicide, it is important to note its relationship with depression and depressive symptoms given the robust nature of the association between this predictor and outcome variable.
Major depression is the psychiatric disorder most strongly associated with completed suicide (Gotlib & Hammen, 2002), and the rate for suicide among individuals diagnosed with major depressive disorder has been estimated to be 20 times higher than that of the general population (American Association of Suicidology, 2010; Coryell & Young, 2005). Similar conclusions were reached in a meta-analysis conducted by Bostwick and Pankratz (2000) who demonstrated that depressed individuals have elevated lifetime suicide rates of between 2% and 9% as compared to a less than 1% rate of suicide in the general population. Moreover, according to psychological autopsy studies, approximately 90% of individuals who commit suicide have a diagnosable mental disorder, and more than half of all people who fall victim to suicide are clinically depressed at the time of suicide (Cavanagh et al., 2003; Hawton & van Heerington, 2009). The above results linking depressive symptoms to suicide ideation, attempts, and completions provide support for one of two pathways in the proposed theoretical framework leading to suicidal behaviors. However, further evidence for the model may be observed by examining depressive symptoms as a mediator in the life strains-suicidal behaviors relationship and by investigating the role of alcohol use in the interplay among these variables.
Research has demonstrated that depressive symptoms may serve as a mediator in the relation between life strains and suicidal behavior (Konick & Gutierrez, 2005). Konick and Gutierrez (2005) proposed a mediational model with negative life events as the independent variable, suicide ideation as the dependent variable, and depressive symptoms as the mediator. The researchers found that depressive symptoms mediated the pathway between negative life events and suicide ideation suggesting that individuals who encounter negative life events may often experience depressive symptoms, which in turn places them at an increased risk of having thoughts about suicide (Konick & Gutierrez, 2005). Arria and colleagues (2009) provided additional support for the significant associations among these variables in adults. Specifically, the researchers demonstrated that high levels of interpersonal conflict with a parent increased the likelihood that an individual would report thoughts of suicide, and elevated levels of depressive symptomatology and a lack of social support strengthened this relationship (Arria et al., 2009). These results accord with previous studies (e.g., Kisch et al., 2005; Tuisku et al., 2009) and lend credence to the supposition that life strains, depressive symptoms, and a lack of social support are interrelated and confer risk for the engagement in suicidal behaviors. Moreover, research has demonstrated that alcohol use may promote an additional risk for suicide among individuals who are faced with a stressful life event while experiencing depressive symptoms (Ilgen et al., 2009; Dejong, Overholser, & Stockmeier, 2010). For instance, Conner, Beautrais, and Conwell (2003) reported that depressive symptoms and life strains (i.e., partner-relationship disruptions, financial difficulties) were significantly more frequent among adult alcoholic suicide attempters than community controls. Although these studies indicate a pathway from life strains to suicidal behaviors through depressive symptoms, there is also data indicating a direct path from life strains to suicidal behaviors even in the absence of depression.
Life Strains and Suicidal Behaviors
Life strains (i.e., interpersonal difficulties, negative life events, alcohol-related problems) have been found to precede suicidal behaviors in a number of studies (e.g., Joiner & Rudd, 2000; Windle & Windle, 2005). Weyrauch, Roy-Byrne, Katon, and Wilson (2001) and others (e.g., Conner et al., 2003) have demonstrated that several life strains including disrupted interpersonal relationships, financial concerns, and legal difficulties were common among adults who made a serious suicide attempt that required hospitalization. In a similar study, Baca-Garcia and associates (2007) corroborated these findings by revealing that suicide attempters were significantly more likely to have experienced partner conflicts and/or other interpersonal conflicts than controls without a suicide attempt history. Consistent with these results and further supporting the life strains-suicidal behaviors association, Lamis, Malone, and Langhinrichsen-Rohling (2010) found that psychological abuse involvement and alcohol-related problems significantly predicted suicide risk in college women. Another study (Kaslow et al., 2002) concluded that recent negative or stressful life events, alcohol-related problems, depressive symptoms, and a lack of social support from family and friends differentiated suicide attempters from nonattempters in a sample of adult women. The findings that life strains and a lack of social support networks are predictive of suicidality is in accordance with the results from previous research (Jeglic, Pepper, Vanderhoff, & Ryabchenko, 2007; Kaslow et al., 1998) revealing that social support is a significant moderator in the association between interpersonal difficulties and suicidal behaviors. Indeed, multiple studies (e.g., Compton, Thompson, & Kaslow, 2005; Joiner et al., 2009; Wilcox et al., 2010) have provided robust evidence that social support serves as a protective factor for suicidal behaviors in a number of diverse adult populations. Taken together, the results from the above studies add to the growing body of research suggesting that life strains are important risk factors for suicidal behaviors and social support may moderate this relationship.
Limitations of the Current Model
The current theoretical framework reflects an attempt to better explain the association between alcohol use and suicidal behaviors by integrating several underlying mechanisms presumed to increase the risk for suicidality in adults. However, some limitations of the model must be noted. First, confounding of demographic characteristics (e.g., gender, ethnicity) with risk factors for suicide was not addressed. As an example, it is well established that women are twice as likely as men to experience depressive symptoms (Nolen-Hoeksema, 2001), whereas men exhibit more impulsive and aggressive behaviors than women (Moffitt, Caspi, Rutter, & Silva, 2001). Interactions between demographic characteristics and risk factors in the model should be considered as the model is tested and refined. Second, the role of genetics in suicidal behaviors was not incorporated in the model. Although research has consistently shown that there is a genetic component involved in suicidal behavior (Courtet et al., 2004; Wasserman, et al., 2007) and in risk factors for suicide (e.g., impulsivity; Kreek, Nielsen, Butelman, & LaForge, 2005), the focus of the current model is on psychological, environmental, and interpersonal factors relating to suicidal behaviors among alcohol users. Third, the acute effects of alcohol intoxication at the time an individual has suicidal thoughts or makes an attempt were beyond the scope of the psychosocial emphasis of this model. Acute alcohol misuse has been shown to be a potent risk factor for subsequent suicidal behavior (Cherpitel et al., 2004; Sher et al., 2009); however, conceptually acute alcohol use may be most relevant to individuals with alcoholism. Another reason why acute use of alcohol was left out of the model is that chronic alcohol use was presumed to be associated with all of the risk factors for suicidal behavior either directly or indirectly, so including the direct effect of acute alcohol use on suicide was deemed unnecessary for this report. Despite these possible limitations, the current model provides a conceptual framework that identifies important additional predisposing and precipitating risk factors for suicidal behaviors and guides understanding of the interrelationships among these variables in alcohol users.
Methodological Considerations for Future Research
We have reviewed the empirical literature on several risk factors for suicidal behavior among individuals who consume alcohol and incorporated these risk factors into a theoretical framework. In our review, we have noted several methodological shortcomings in this area of research. First, the measurement of alcohol use and suicidal behaviors is often limited. For example, many studies assessing these constructs use self-report data, which raises the potential issue of bias due to socially desirable responding. One possible solution to this problem is to employ more sophisticated, objective measures such as the implicit association test (Nock et al., 2010) to assess suicide cognitions and the alcohol stroop task (Cox, Yeates, & Regan, 1999) to assess drinking behavior in addition to self-report instruments measuring these variables. Another measurement weakness in the alcohol literature is that alcohol use is often measured by a single item, which raises issues of reliability and validity. Research in this area should make an effort to utilize detailed psychometrically sound alcohol use measures, such as the Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). Similarly, suicidal behaviors are often assessed through single items measuring suicidal ideation and attempts. It will be important for future researchers to employ measures assessing these behaviors with instruments that have been shown to be reliable and valid.
Other methodological considerations for future research include sample selection and design issues. Many of the samples used to investigate the connection between alcohol use and suicidal behaviors are heavy alcohol consumers, individuals with alcoholism, or suicide attempters seeking medical attention. Studies examining suicidal behaviors and risk factors among adults with varying levels of alcohol use are necessary to more clearly elucidate these relations. Further, the majority of studies on alcohol use and suicide use cross-sectional or retrospective research designs, which hampers causal interpretation of associations among variables. Future longitudinal work in this area, particularly exploring the roles of specific mediators and moderators, is warranted. If researchers consider these methodological limitations and make efforts to overcome their deficiencies, a better understanding of the association between alcohol use and suicidal behaviors can be achieved and enhanced prevention strategies may be developed. However, it is important to note that these suggestions for future research will require significant resources. Thus, it will be necessary for funding sources to continue to advance efforts providing resources to programs and research projects investigating the relation between alcohol use and suicide risk.
Implications for Prevention and Treatment
Our theoretical framework, expanding on existing models, is intended to guide basic research and inform applied work to reduce suicidal behaviors among adult alcohol consumers. In the literature review and the current model, we identified numerous risk factors for suicide that are especially pertinent for individuals who drink alcohol. The model also illustrates mechanisms underlying the distal and proximal risk for suicidal behaviors as well as explaining the nature of these associations. Conceptualizing suicidal behavior through the current theoretical framework may have several practical implications. For example, mental health professionals and prevention specialists could use this model to effectively assess individuals for these predisposing (e.g., impulsivity/aggression, lack of social support) and precipitating (e.g., life strains, depressive symptoms) factors in order to reduce suicide risk. Consequently, individuals who have several of these risk factors may need to be assessed for suicidal behaviors on a regular basis or referred to treatment. Risk assessment grounded in the proposed theory, if empirically supported, will facilitate successful identification of adults at risk for suicide. In addition to assessment, preventative intervention programs that target these identified risk factors and the mediational mechanisms presumed to underlie suicidality should be designed specifically for adults who consume higher levels of alcohol. In terms of clinical care and treatment, mental health professionals should directly address the risk factors incorporated in the model to effectively reduce suicide behaviors in this at-risk population. In sum, the conceptual framework illuminating the relation between alcohol use and suicidal behaviors has many promising implications for the reduction of suicidality in adults.
Summary and Conclusions
The association between alcohol use and suicidal behaviors is complex and not completely understood, particularly in adult populations with varying degrees of alcohol consumption. This review has highlighted evidence identifying a number of risk factors in a proposed theoretical framework that contribute to suicidal behaviors among alcohol users. The studies reviewed in the context of the underlying theory offer several lines of research worthy of investigation. The present model demonstrates that there may be multiple pathways to suicidal behaviors and provides several empirically testable research questions and hypotheses for future investigators to consider. For example, future studies could investigate which pathway from life strains to suicidal behaviors is more likely for an impulsive/aggressive individual, given a certain level of alcohol use.
Another potential avenue for continued research suggested by the present framework is to examine the moderating effects of social support on depressive symptoms and suicidal behaviors after individuals with different levels of alcohol use (i.e., low, moderate, high) experience a life strain. It is important to evaluate the various mediating and moderating effects among risk factors in order to successfully explain the association between alcohol use and suicidal behaviors in adults. The proposed model should guide future research and facilitate further empirical analyses on the interactive effects among risk factors that may contribute to suicidal behaviors in alcohol users. Further investigation of the interrelations among the model variables should aid in the understanding of suicide in this high-risk group. Once the nature of these associations is better understood among alcohol-using adults, more effective suicide prevention programs may be designed and implemented.
References
- Abramson L, Metalsky G, Alloy L. Hopelessness depression: A theory-based subtype of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- Alford B, Lester J, Patel R, Buchanan J. Hopelessness predicts future depressive symptoms: A prospective analysis of cognitive vulnerability and cognitive content specificity. Journal of Clinical Psychology. 1995;51:331–339. doi: 10.1002/1097-4679(199505)51:3<331::aid-jclp2270510303>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- Alloy L, Abramson L, Hogan M, Whitehouse W, Rose D, Robinson M, et al. The Temple-Wisconsin cognitive vulnerability to depression project: Lifetime history of Axis I psychopathology in individuals at high and low cognitive risk for depression. Journal of Abnormal Psychology. 2000;109:403–418. [PubMed] [Google Scholar]
- American Association of Suicidology. Facts about suicide and depression. Washington, DC: American Association of Suicidology; 2010. [fact sheet] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., text rev. Washington, DC: Author; 2000. [Google Scholar]
- Arria A, O’Grady K, Caldeira K, Vincent K, Wilcox H, Wish E. Suicide ideation among college students: A multivariate analysis. Archives of Suicide Research. 2009;13:230–246. doi: 10.1080/13811110903044351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baca-Garcia E, Parra C, Perez-Rodriguez M, Sastre C, Torres R, Saiz-Ruiz J, et al. Psychosocial stressors may be strongly associated with suicide attempts. Stress and Health: Journal of the International Society for the Investigation of Stress. 2007;23:191–198. [Google Scholar]
- Bácskai E, Czobor P, Gerevich J. Heavy drinking as a differential predictor of physical aggression in clinical and general populations. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2008;32:668–672. doi: 10.1016/j.pnpbp.2007.11.016. [DOI] [PubMed] [Google Scholar]
- Bailey CA, Ostrov JM. Differentiating forms and functions of aggression in emerging adults: Associations with hostile attribution biases and normative beliefs. Journal of Youth and Adolescence. 2008;37:713–722. [Google Scholar]
- Barrett M, Barber J. Interpersonal profiles in major depressive disorder. Journal of Clinical Psychology. 2007;63:247–266. doi: 10.1002/jclp.20346. [DOI] [PubMed] [Google Scholar]
- Beauchaine T, Klein D, Crowell S, Derbidge C, Gatzke-Kopp L. Multifinality in the development of personality disorders: A biology × sex × environment interaction model of antisocial and borderline traits. Development and Psychopathology. 2009;21:735–770. doi: 10.1017/S0954579409000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A, Weissman A, Lester D, Trexler L. The measurement of pessimism: The Hopelessness Scale. Journal of Consulting and Clinical Psychology. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Beedie A, Kennedy P. Quality of social support predicts hopelessness and depression post spinal cord injury. Journal of Clinical Psychology in Medical Settings. 2002;9:227–234. [Google Scholar]
- Benjamin L, Wulfert E. Dispositional correlates of addictive behaviors in college women: Binge eating and heavy drinking. Eating Behaviors. 2005;6:197–209. doi: 10.1016/j.eatbeh.2003.08.001. [DOI] [PubMed] [Google Scholar]
- Bjorck J, Thurman J. Negative life events, patterns of positive and negative religious coping, and psychological functioning. Journal for the Scientific Study of Religion. 2007;46:159–167. [Google Scholar]
- Bolland J. Hopelessness and risk behaviour among adolescents living in high-poverty inner-city neighborhoods. Journal of Adolescence. 2003;26:145–158. doi: 10.1016/s0140-1971(02)00136-7. [DOI] [PubMed] [Google Scholar]
- Bond A. Drug-induced behavioural disinhibition: Incidence, mechanisms and therapeutic implications. CNS Drugs. 1998;9:41–57. [Google Scholar]
- Borges G, Walters EE, Kessler RC. Associations of substance use, abuse and dependence with subsequent suicidal behaviour. American Journal of Epidemiology. 2000;151:781–789. doi: 10.1093/oxfordjournals.aje.a010278. [DOI] [PubMed] [Google Scholar]
- Borges G, Rosovsky H. Suicide attempts and alcohol consumption in an emergency room sample. Journal of Studies on Alcohol. 1996;57:543–548. doi: 10.15288/jsa.1996.57.543. [DOI] [PubMed] [Google Scholar]
- Borsari B, Carey K. How the quality of peer relationships influences college alcohol use. Drug and Alcohol Review. 2006;25:361–370. doi: 10.1080/09595230600741339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick J, Pankratz V. Affective disorders and suicide risk: A reexamination. The American Journal of Psychiatry. 2000;157:1925–1932. doi: 10.1176/appi.ajp.157.12.1925. [DOI] [PubMed] [Google Scholar]
- Brady J. The association between alcohol misuse and suicidal behavior. Alcohol & Alcoholism. 2006;41:473–478. doi: 10.1093/alcalc/agl060. [DOI] [PubMed] [Google Scholar]
- Carlson S, Johnson S, Jacobs P. Disinhibited characteristics and binge drinking among university student drinkers. Addictive Behaviors. 2010;35:242–251. doi: 10.1016/j.addbeh.2009.10.020. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt T, Taylor A, Craig I, Harrington H, et al. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Cavanagh J, Carson A, Sharpe M, Lawrie S. Psychological autopsy studies of suicide: A systematic review. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2003;33:395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System. [Accessed May 3, 2010];2007 Available at http://www.cdc.gov/injury/wisqars/index.html.
- Chermack S, Blow F. Violence among individuals in substance abuse treatment: The role of alcohol and cocaine consumption. Drug and Alcohol Dependence. 2002;66:29–37. doi: 10.1016/s0376-8716(01)00180-6. [DOI] [PubMed] [Google Scholar]
- Cherpitel CL, Borges GL, Wilcox HC. Acute alcohol use and suicidal behavior: A review of the literature. Alcoholism: Clinical and Experimental Research. 2004;28:18–28. doi: 10.1097/01.alc.0000127411.61634.14. [DOI] [PubMed] [Google Scholar]
- Chioqueta A, Stiles T. The relationship between psychological buffers, hopelessness, and suicidal ideation: Identification of protective factors. Crisis: The Journal of Crisis Intervention and Suicide Prevention. 2007;28:67–73. doi: 10.1027/0227-5910.28.2.67. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Compton M, Thompson N, Kaslow N. Social environment factors associated with suicide attempt among low-income African Americans: The protective role of family relationships and social support. Social Psychiatry and Psychiatric Epidemiology. 2005;40:175–185. doi: 10.1007/s00127-005-0865-6. [DOI] [PubMed] [Google Scholar]
- Conner K, Beautrais A, Conwell Y. Risk factors for suicide and medically serious suicide attempts among alcoholics: Analyses of Canterbury suicide project data. Journal of Studies on Alcohol. 2003;64:551–554. doi: 10.15288/jsa.2003.64.551. [DOI] [PubMed] [Google Scholar]
- Conner KR, Duberstein PR. Predisposing and precipitating factors for suicide among alcoholics: Empirical review and conceptual integration. Alcoholism: Clinical and Experimental Research. 2004;28:6S–17S. doi: 10.1097/01.alc.0000127410.84505.2a. [DOI] [PubMed] [Google Scholar]
- Conner K, Duberstein P, Conwell Y, Caine E. Reactive aggression and suicide: Theory and evidence. Aggression and Violent Behavior. 2003;8:413–432. [Google Scholar]
- Conner K, McCloskey M, Duberstein P. Psychiatric risk factors for suicide in the alcohol-dependent patient. Psychiatric Annals. 2008;38:742–748. [Google Scholar]
- Conner K, Li Y, Meldrum S, Duberstein P, Conwell Y. The role of drinking in suicidal ideation: Analyses of Project MATCH data. Journal of Studies on Alcohol. 2003;64:402–408. doi: 10.15288/jsa.2003.64.402. [DOI] [PubMed] [Google Scholar]
- Connor-Smith J, Flachsbart C. Relations between personality and coping: A meta-analysis. Journal of Personality and Social Psychology. 2007;93:1080–1107. doi: 10.1037/0022-3514.93.6.1080. [DOI] [PubMed] [Google Scholar]
- Coryell W, Young E. Clinical predictors of suicide in primary major depressive disorder. Journal of Clinical Psychiatry. 2005;66:412–417. doi: 10.4088/jcp.v66n0401. [DOI] [PubMed] [Google Scholar]
- Courtet P, Picot M, Bellivier F, Torres S, Jollant F, Michelon C, et al. Serotonin transporter gene may be involved in short-term risk of subsequent suicide attempts. Biological Psychiatry. 2004;55:46–51. doi: 10.1016/j.biopsych.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Cox W, Yeates G, Regan C. Effects of alcohol cues on cognitive processing in heavy and light drinkers. Drug and Alcohol Dependence. 1999;55:58–58. doi: 10.1016/s0376-8716(98)00186-0. [DOI] [PubMed] [Google Scholar]
- Crosby A, Espitia-Hardeman V, Hill H, Ortega L, Clavel-Arcas C. Alcohol and suicide among racial/ethnic populations—17 states, 2005–2006. JAMA: Journal of the American Medical Association. 2009;302:733–734. [Google Scholar]
- Crosby A, Cheltenham M, Sacks J. Incidence of suicidal ideation and behavior in the United States, 1994. Suicide and Life-Threatening Behavior. 1999;29:131–140. [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Toward the attainment of low-risk drinking goals: A 10-year progress report. Alcoholism: Clinical and Experimental Research. 2004;28:1371–1387. doi: 10.1097/01.alc.0000139811.24455.3e. [DOI] [PubMed] [Google Scholar]
- DeJong T, Overholser J, Stockmeier C. Apples to oranges?: A direct comparison between suicide attempters and suicide completers. Journal of Affective Disorders. 2010;124:90–97. doi: 10.1016/j.jad.2009.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devos-Comby L, Lange J. Standardized measures of alcohol-related problems: A review of their use among college students. Psychology of Addictive Behaviors. 2008;22:349–361. doi: 10.1037/0893-164X.22.3.349. [DOI] [PubMed] [Google Scholar]
- Dick D, Smith G, Olausson P, Mitchell S, Leeman R, O'Malley S, et al. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biology. 2010;15:217–226. doi: 10.1111/j.1369-1600.2009.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dom G, Hulstijn W, Sabbe B. Differences in impulsivity and sensation seeking between early- and late-onscoholics. Addictive Behaviors. 2006;31:298–308. doi: 10.1016/j.addbeh.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Ellis TE, Trumpower D. Health risk behaviors and suicidal ideation: A preliminary study of cognitive and developmental factors. Suicide and Life-Threatening Behavior. 2008;38:251–259. doi: 10.1521/suli.2008.38.3.251. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W. The occurrence of partner physical aggression on days of alcohol consumption: A longitudinal diary study. Journal of Consulting and Clinical Psychology. 2003;71(1):41–52. doi: 10.1037//0022-006x.71.1.41. [DOI] [PubMed] [Google Scholar]
- Flensborg-Madsen T, Knop J, Mortensen E, Becker U, Sher L, Grønbæk M. Alcohol use disorders increase the risk of completed suicide — Irrespective of other psychiatric disorders. A longitudinal cohort study. Psychiatry Research. 2009;167:123–130. doi: 10.1016/j.psychres.2008.01.008. [DOI] [PubMed] [Google Scholar]
- Fowler D, Hill H. Social support and spirituality as culturally relevant factors in coping among African American women survivors of partner abuse. Violence Against Women. 2004;10:1267–1282. [Google Scholar]
- Garlow S, Rosenberg J, Moore J, Haas A, Koestner B, Hendin H, et al. Depression, desperation, and suicidal ideation in college students: Results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depression and Anxiety. 2008;25:482–488. doi: 10.1002/da.20321. [DOI] [PubMed] [Google Scholar]
- Geisner I, Larimer M, Neighbors C. The relationship among alcohol use, related problems, and symptoms of psychological distress: Gender as a moderator in a college sample. Addictive Behaviors. 2004;29:843–848. doi: 10.1016/j.addbeh.2004.02.024. [DOI] [PubMed] [Google Scholar]
- Gerevich J, Bácskai E, Czobor P. Aggression levels in treatment seeking inpatients with alcohol-related problems compared to levels in the general population in Hungary. Journal of Nervous and Mental Disease. 2007;195:669–672. doi: 10.1097/NMD.0b013e31812001fc. [DOI] [PubMed] [Google Scholar]
- Giancola P. Alcohol-related aggression during the college years: Theories, risk factors, and policy implications. Journal of Studies on Alcohol. 2002;14:129–139. doi: 10.15288/jsas.2002.s14.129. [DOI] [PubMed] [Google Scholar]
- Gibb B, Coles M. Development of psychopathology: A vulnerability-stress perspective. Thousand Oaks, CA US: Sage Publications; 2005. Cognitive vulnerability-stress models of psychopathology: A developmental perspective; pp. 104–135. [Google Scholar]
- Giner L, Carballo J, Guija J, Sperling D, Oquendo M, Garcia-Parajua P, et al. Psychological autopsy studies: The role of alcohol use in adolescent and young adult suicides. International Journal of Adolescent Medicine and Health. 2007;19:99–113. doi: 10.1515/ijamh.2007.19.1.99. [DOI] [PubMed] [Google Scholar]
- Golden J, Conroy R, Bruce I, Denihan A, Greene E, Kirby M, et al. Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. International Journal of Geriatric Psychiatry. 2009;24:694–700. doi: 10.1002/gps.2181. [DOI] [PubMed] [Google Scholar]
- Goldstein RZ, Volkow ND. Drug addiction and its underlying neurobiological basis: Neuroimaging evidence for the involvement of the frontal cortex. American Journal of Psychiatry. 2002;159:1642–1652. doi: 10.1176/appi.ajp.159.10.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez V, Bradizza C, Collins R. Drinking to cope as a statistical mediator in the relationship between suicidal ideation and alcohol outcomes among underage college drinkers. Psychology of Addictive Behaviors. 2009;23:443–451. doi: 10.1037/a0015543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotlib I, Hammen C. Handbook of depression. New York, NY US: Guilford Press; 2002. [Google Scholar]
- Griffin K, Botvin G, Nichols T, Scheier L. Low perceived chances for success in life and binge drinking among inner-city minority youth. Journal of Adolescent Health. 2004;34:501–507. doi: 10.1016/j.jadohealth.2003.07.026. [DOI] [PubMed] [Google Scholar]
- Haden S, Scarpa A, Stanford M. Validation of the Impulsive/Premeditated Aggression Scale in college students. Journal of Aggression, Maltreatment & Trauma. 2008;17:352–373. [Google Scholar]
- Hammen C. Stress And Depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hankin B, Abramson L, Miller N, Haeffel G. Cognitive vulnerability-stress theories of depression: Examining affective specificity in the prediction of depression versus anxiety in three prospective studies. Cognitive Therapy and Research. 2004;28:309–345. [Google Scholar]
- Hankin B, Fraley R, Abela J. Daily depression and cognitions about stress: Evidence for a traitlike depressogenic cognitive style and the prediction of depressive symptoms in a prospective daily diary study. Journal of Personality and Social Psychology. 2005;88:673–685. doi: 10.1037/0022-3514.88.4.673. [DOI] [PubMed] [Google Scholar]
- Hawton K, van Heeringen K. Suicide. Lancet. 2009;373:1372–1381. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- Hawton K, Haigh R, Simkin S, Fagg J. Attempted suicide in Oxford University students, 1976–1990. Psychological Medicine. 1995;25:179–188. doi: 10.1017/s0033291700028208. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Winter MR. Age at drinking onset and alcohol dependence: Age at onset, duration, and severity. Archives of Pediatric and Adolescent Medicine. 2006;160:739–746. doi: 10.1001/archpedi.160.7.739. [DOI] [PubMed] [Google Scholar]
- Hirsch J, Wolford K, LaLonde S, Brunk L, Parker-Morris A. Optimistic explanatory style as a moderator of the association between negative life events and suicide ideation. Crisis: The Journal of Crisis Intervention and Suicide Prevention. 2009;30:48–53. doi: 10.1027/0227-5910.30.1.48. [DOI] [PubMed] [Google Scholar]
- Horowitz LM. Interpersonal foundations of psychopathology. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- Hufford M. Alcohol and suicidal behavior. Clinical Psychology Review. 2001;21:797–811. doi: 10.1016/s0272-7358(00)00070-2. [DOI] [PubMed] [Google Scholar]
- Ilgen M, Chermack S, Murray R, Walton M, Barry K, Wojnar M, et al. The association between partner and non-partner aggression and suicidal ideation in patients seeking substance use disorder treatment. Addictive Behaviors. 2009;34:180–186. doi: 10.1016/j.addbeh.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilhan I, Demirbas H, Dogan Y. Psychosocial factors in alcohol use-related problems of working youth. Substance Use & Misuse. 2007;42:1537–1544. doi: 10.1080/10826080701212444. [DOI] [PubMed] [Google Scholar]
- Jaffee W, D'Zurilla T. Personality, problem solving, and adolescent substance use. Behavior Therapy. 2009;40:93–101. doi: 10.1016/j.beth.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Jeglic E, Pepper C, Vanderhoff H, Ryabchenko K. An analysis of suicidal ideation in a college sample. Archives of Suicide Research. 2007;11:41–56. doi: 10.1080/13811110600897176. [DOI] [PubMed] [Google Scholar]
- Johnson J, Alloy L, Panzarella C, Metalsky G, Rabkin J, Williams J, et al. Hopelessness as a mediator of the association between social support and depressive symptoms: Findings of a study of men with HIV. Journal of Consulting and Clinical Psychology. 2001;69:1056–1060. doi: 10.1037//0022-006x.69.6.1056. [DOI] [PubMed] [Google Scholar]
- Johnson L, O’Malley P, Bachman J, Schulenberg J. Monitoring the future national survey results on drug use, 1975–2005: Volume II, College students and adults aged 19–45. Bethesda, MD: National Institute on Drug Abuse; 2007. [Google Scholar]
- Joiner TE., Jr . Why people die by suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Joiner T, Conwell Y, Fitzpatrick K, Witte T, Schmidt N, Berlim M, et al. Four studies on how past and current suicidality relate even when 'everything but the kitchen sink' is covaried. Journal of Abnormal Psychology. 2005;114:291–303. doi: 10.1037/0021-843X.114.2.291. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Coyne JC. The interactional nature of depression: Advances in interpersonal approaches. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- Joiner T, Rudd M. Intensity and duration of suicidal crisis vary as a function of previous suicide attempts and negative life events. Journal of Consulting and Clinical Psychology. 2000;68:909–916. doi: 10.1037/0022-006X.68.5.909. [DOI] [PubMed] [Google Scholar]
- Joiner T, Van Orden K, Witte T, Selby E, Ribeiro J, Lewis R, et al. Main predictions of the interpersonal–psychological theory of suicidal behavior: Empirical tests in two samples of young adults. Journal of Abnormal Psychology. 2009;118:634–646. doi: 10.1037/a0016500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner T, Wingate L, Otamendi A. An interpersonal addendum to the hopelessness theory of depression: Hopelessness as a stress and depression generator. Journal of Social and Clinical Psychology. 2005;24:649–664. [Google Scholar]
- Jordanova V, Stewart R, Goldberg D, Bebbington P, Brugha T, Singleton N, et al. Age variation in life events and their relationship with common mental disorders in a national survey population. Social Psychiatry and Psychiatric Epidemiology. 2007;42:611–616. doi: 10.1007/s00127-007-0209-9. [DOI] [PubMed] [Google Scholar]
- Kaslow N, Thompson M, Meadows L, Jacobs D, Chance S, Gibb B, et al. Factors that mediate and moderate the link between partner abuse and suicidal behavior in African American women. Journal of Consulting and Clinical Psychology. 1998;66:533–540. doi: 10.1037//0022-006x.66.3.533. [DOI] [PubMed] [Google Scholar]
- Kaslow N, Thompson M, Okun A, Price A, Young S, Bender M, et al. Risk and protective factors for suicidal behavior in abused African American women. Journal of Consulting and Clinical Psychology. 2002;70:311–319. doi: 10.1037//0022-006x.70.2.311. [DOI] [PubMed] [Google Scholar]
- Keller P, El-Sheikh M, Keiley M, Liao P. Longitudinal relations between marital aggression and alcohol problems. Psychology of Addictive Behaviors. 2009;23:2–13. doi: 10.1037/a0013459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr D, Preuss L, King C. Suicidal adolescents' social support from family and peers: Gender-specific associations with psychopathology. Journal of Abnormal Child Psychology. 2006;34:103–114. doi: 10.1007/s10802-005-9005-8. [DOI] [PubMed] [Google Scholar]
- Kessler R, Berglund P, Borges G, Nock M, Wang P. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA: Journal of the American Medical Association. 2005;293:2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- Kessler R, Berglund P, Chiu W, Demler O, Heeringa S, Hiripi E, et al. The US National Comorbidity Survey Replication (NCS-R): Design and field procedures. International Journal of Methods in Psychiatric Research. 2004;13:69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Berglund P, Demler O, Jin R, Merikangas K, Walters E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters MS. Prevalence of and risk factors for lifetime suicide attempts in the national comorbidity survey. Archives of General Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Kessler R, Wang P. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annual Review of Public Health. 2008;29:115–129. doi: 10.1146/annurev.publhealth.29.020907.090847. [DOI] [PubMed] [Google Scholar]
- Khantzian E. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- King C, Klaus N, Kramer A, Venkataraman S, Quinlan P, Gillespie B. The Youth-Nominated Support Team–Version II for suicidal adolescents: A randomized controlled intervention trial. Journal of Consulting and Clinical Psychology. 2009;77:880–893. doi: 10.1037/a0016552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisch J, Leino EV, Silverman MM. Aspects of suicidal behavior, depression, and treatment in college students: Results from the spring 2000 national college health assessment survey. Suicide and Life-Threatening Behavior. 2005;35:3–13. doi: 10.1521/suli.35.1.3.59263. [DOI] [PubMed] [Google Scholar]
- Koenigsberg H, Harvey P, Mitropoulou V, New A, Goodman M, Silverman J, et al. Are the interpersonal and identity disturbances in the borderline personality disorder criteria linked to the traits of affective instability and impulsivity? Journal of Personality Disorders. 2001;15:358–370. doi: 10.1521/pedi.15.4.358.19181. [DOI] [PubMed] [Google Scholar]
- Konick L, Gutierrez P. Testing a model of suicide ideation in college students. Suicide and Life-Threatening Behavior. 2005;35:181–192. doi: 10.1521/suli.35.2.181.62875. [DOI] [PubMed] [Google Scholar]
- Kung HC, Hoyert DL, Xu JQ, Murphy SL. National vital statistics reports, 56. Hyattsville MD: National Center for Health Statistics; 2008. Deaths: Final data for 2005. [PubMed] [Google Scholar]
- Kreek M, Nielsen D, Butelman E, LaForge K. Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addiction. Nature Neuroscience. 2005;8:1450–1457. doi: 10.1038/nn1583. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamis DA, Malone PS. Alcohol-related problems and risk of suicide among college students: The mediating roles of belongingness and burdensomeness. Suicide and Life-Threatening Behavior. 2011;41:543–553. doi: 10.1111/j.1943-278X.2011.00052.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamis DA, Malone PS, Langhinrichsen-Rohling J. Intimate partner psychological aggression and suicide proneness in college women: Alcohol related problems as a potential mediator. Partner Abuse. 2010;1:169–185. doi: 10.1891/1946-6560.1.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamis DA, Malone PS, Langhinrichsen-Rohling J, Ellis TE. Body investment, depression, and alcohol use as risk factors for suicide proneness in college students. Crisis: The Journal of Crisis Intervention and Suicide Prevention. 2010;31:118–127. doi: 10.1027/0227-5910/a000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeman R, Toll B, Taylor L, Volpicelli J. Alcohol-induced disinhibition expectancies and impaired control as prospective predictors of problem drinking in undergraduates. Psychology of Addictive Behaviors. 2009;23:553–563. doi: 10.1037/a0017129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejoyeux M, Huet F, Claudon M, Fichelle A, Casalino E, Lequen V. Characteristics of suicide attempts preceded by alcohol consumption. Archives of Suicide Research. 2008;12:30–38. doi: 10.1080/13811110701800699. [DOI] [PubMed] [Google Scholar]
- Livingston M, Room R. Variations by age and sex in alcohol-related problematic behaviour per drinking volume and heavier drinking occasion. Drug and Alcohol Dependence. 2009;101:169–175. doi: 10.1016/j.drugalcdep.2008.12.014. [DOI] [PubMed] [Google Scholar]
- Löckenhoff C, Terracciano A, Patriciu N, Eaton W, Costa P. Self-reported extremely adverse life events and longitudinal changes in Five-Factor Model personality traits in an urban sample. Journal of Traumatic Stress. 2009;22:53–59. doi: 10.1002/jts.20385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyvers M. 'Loss of control' in alcoholism and drug addiction: A neuroscientific interpretation. Experimental and Clinical Psychopharmacology. 2000;8:225–245. doi: 10.1037//1064-1297.8.2.225. [DOI] [PubMed] [Google Scholar]
- Macdonald S, Erickson P, Wells S, Hathaway A, Pakula B. Predicting violence among cocaine, cannabis, and alcohol treatment clients. Addictive Behaviors. 2008;33:201–205. doi: 10.1016/j.addbeh.2007.07.002. [DOI] [PubMed] [Google Scholar]
- Magid V, Colder C. The UPPS Impulsive Behavior Scale: Factor structure and associations with college drinking. Personality and Individual Differences. 2007;43:1927–1937. [Google Scholar]
- Magid V, MacLean M, Colder C. Differentiating between sensation seeking and impulsivity through their mediated relations with alcohol use and problems. Addictive Behaviors. 2007;32:2046–2061. doi: 10.1016/j.addbeh.2007.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann J, Brent D, Arango V. The neurobiology and genetics of suicide and attempted suicide: A focus on the serotonergic system. Neuropsychopharmacology. 2001;24:467–477. doi: 10.1016/S0893-133X(00)00228-1. [DOI] [PubMed] [Google Scholar]
- Mann J, Waternaux C, Haas G, Malone K. Toward a clinical model of suicidal behavior in psychiatric patients. The American Journal of Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- Marczinski CA, Abroms BD, Van Selst M, Fillmore MT. Alcohol-induced impairment of behavioral control: Differential effects on engaging vs. disengaging responses. Psychopharmacology. 2005;182:452–459. doi: 10.1007/s00213-005-0116-2. [DOI] [PubMed] [Google Scholar]
- Margolis RD, Zweben JE. Models and theories of addiction. In: Margolis RD, Zweben JE, editors. Treating patients with alcohol and other drug problems: An integrated approach. Washington, DC US: American Psychological Association; 2011. pp. 27–58. [Google Scholar]
- Martens M, Martin J, Hatchett E, Fowler R, Fleming K, Karakashian M, et al. Protective behavioral strategies and the relationship between depressive symptoms and alcohol-related negative consequences among college students. Journal of Counseling Psychology. 2008;55:535–541. doi: 10.1037/a0013588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauchnik J, Schmahl C, Bohus M. New findings in the biology of borderline personality disorder. Directions in Psychiatry. 2005;25:197–215. [Google Scholar]
- Meilman PW, Pattis JA, Kraus-Zeilmann D. Suicide attempts and threats on one college campus: Policy and practice. Journal of American College Health. 1994;42:147–154. doi: 10.1080/07448481.1994.9939662. [DOI] [PubMed] [Google Scholar]
- Menagi F, Harrell Z, June L. Religiousness and college student alcohol use: Examining the role of social support. Journal of Religion and Health. 2008;47:217–226. doi: 10.1007/s10943-008-9164-3. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Rutter M, Silva PA. Sex differences in antisocial behavior: Conduct disorder, delinquency and violence in the Dunedin Longitudinal Study. Cambridge, UK: Cambridge University Press; 2001. [Google Scholar]
- Murphy J, McDevitt-Murphy M, Barnett N. Drink and be merry? Gender, life satisfaction, and alcohol consumption among college students. Psychology of Addictive Behaviors. 2005;19:184–191. doi: 10.1037/0893-164X.19.2.184. [DOI] [PubMed] [Google Scholar]
- Nock M, Borges G, Bromet E, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. British Journal of Psychiatry. 2008;192:98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: Findings from the WHO World Mental Health Surveys. PLoS Medicine. 2009;6 doi: 10.1371/journal.pmed.1000123. e1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock M, Park J, Finn C, Deliberto T, Dour H, Banaji M. Measuring the suicidal mind: Implicit cognition predicts suicidal behavior. Psychological Science. 2010;21:511–517. doi: 10.1177/0956797610364762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in depression. Current Directions in Psychological Science. 2001;10:173–176. [Google Scholar]
- Nrugham L, Holen A, Sund A. Associations between attempted suicide, violent life events, depressive symptoms, and resilience in adolescents and young adults. Journal of Nervous and Mental Disease. 2010;198:131–136. doi: 10.1097/NMD.0b013e3181cc43a2. [DOI] [PubMed] [Google Scholar]
- Oberlin B, Grahame N. High-alcohol preferring mice are more impulsive than low-alcohol preferring mice as measured in the delay discounting task. Alcoholism: Clinical and Experimental Research. 2009;33:1294–1303. doi: 10.1111/j.1530-0277.2009.00955.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neill S, Cohen L, Tolpin L, Gunthert K. Affective reactivity to daily interpersonal stressors as a prospective predictor of depressive symptoms. Journal of Social and Clinical Psychology. 2004;23:172–194. [Google Scholar]
- Oquendo M, Galfalvy H, Russo S, Ellis S, Grunebaum M, Burke A, et al. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. The American Journal of Psychiatry. 2004;161:1433–1441. doi: 10.1176/appi.ajp.161.8.1433. [DOI] [PubMed] [Google Scholar]
- Panzarella C, Alloy L, Whitehouse W. Expanded hopelessness theory of depression: On the mechanisms by which social support protects against depression. Cognitive Therapy and Research. 2006;30:307–333. [Google Scholar]
- Park CL. Positive and negative consequences of alcohol consumption in college students. Addictive Behaviors. 2004;29:311–321. doi: 10.1016/j.addbeh.2003.08.006. [DOI] [PubMed] [Google Scholar]
- Park C, Grant C. Determinants of positive and negative consequences of alcohol consumption in college students: Alcohol use, gender, and psychological characteristics. Addictive Behaviors. 2005;30:755–765. doi: 10.1016/j.addbeh.2004.08.021. [DOI] [PubMed] [Google Scholar]
- Parrott D, Giancola P. New research on alcohol abuse and alcoholism. Hauppauge, NY US: Nova Science Publishers; 2006. Alcohol dependence and physical aggression: The mediating effect of dispositional impulsivity; pp. 155–172. [Google Scholar]
- Pauley PM, Hesse C. The effects of social support, depression, and stress on drinking behaviors in a college student sample. Communication Studies. 2009;60:493–508. [Google Scholar]
- Peirce R, Frone M, Russell M, Cooper M, Mudar P. A longitudinal model of social contact, social support, depression, and alcohol use. Health Psychology. 2000;19:28–38. doi: 10.1037//0278-6133.19.1.28. [DOI] [PubMed] [Google Scholar]
- Poulin F, Boivin M. Reactive and proactive aggression: Evidence of a two-factor model. Psychological Assessment. 2000;12:115–122. doi: 10.1037//1040-3590.12.2.115. [DOI] [PubMed] [Google Scholar]
- Powell K, Kresnow J, Mercy J, Potter L, Swann A, Frankowski R, et al. Alcohol consumption and nearly lethal suicide attempts. Suicide and Life-Threatening Behavior. 2001;32:30–41. doi: 10.1521/suli.32.1.5.30.24208. [DOI] [PubMed] [Google Scholar]
- Preuss U, Koller G, Barnow S, Eikmeier M, Soyka M. Suicidal behavior in alcohol-dependent subjects: The role of personality disorders. Alcoholism: Clinical and Experimental Research. 2006;30:866–877. doi: 10.1111/j.1530-0277.2006.00073.x. [DOI] [PubMed] [Google Scholar]
- Quigley B, Leonard K. Husband alcohol expectancies, drinking, and marital-conflict styles as predictors of severe marital violence among newlywed couples. Psychology of Addictive Behaviors. 1999;13:49–59. [Google Scholar]
- Rafnsson F, Jonsson F, Windle M. Coping strategies, stressful life events, problem behaviors, and depressed affect. Anxiety, Stress & Coping: An International Journal. 2006;19:241–257. [Google Scholar]
- Rehm J, Taylor B, Room R. Global burden of disease from alcohol, illicit drugs and tobacco. Drug and Alcohol Review. 2006;25:503–513. doi: 10.1080/09595230600944453. [DOI] [PubMed] [Google Scholar]
- Rholes W, Riskind J, Neville B. The relationship of cognitions and hopelessness to depression and anxiety. Social Cognition. 1985;3:36–50. [Google Scholar]
- Robinson J, Harris M, Harrigan S, Henry L, Farrelly S, Prosser A, et al. Suicide attempt in first-episode psychosis: A 7.4 year follow-up study. Schizophrenia Research. 2010;116:1–8. doi: 10.1016/j.schres.2009.10.009. [DOI] [PubMed] [Google Scholar]
- Rogge R, Bradbury T. Till violence does us part: The differing roles of communication and aggression in predicting adverse marital outcomes. Journal of Consulting and Clinical Psychology. 1999;67:340–351. doi: 10.1037//0022-006x.67.3.340. [DOI] [PubMed] [Google Scholar]
- Rogge R, Bradbury T, Hahlweg K, Engl J, Thurmaier F. Predicting marital distress and dissolution: Refining the two-factor hypothesis. Journal of Family Psychology. 2006;20:156–159. doi: 10.1037/0893-3200.20.1.156. [DOI] [PubMed] [Google Scholar]
- Rowe R, Maughan B, Eley T. Links between antisocial behavior and depressed mood: The role of life events and attributional style. Journal of Abnormal Child Psychology. 2006;34:293–302. doi: 10.1007/s10802-006-9032-0. [DOI] [PubMed] [Google Scholar]
- Safford S, Alloy L, Abramson L, Crossfield A. Negative cognitive style as a predictor of negative life events in depression-prone individuals: A test of the stress generation hypothesis. Journal of Affective Disorders. 2007;99:147–154. doi: 10.1016/j.jad.2006.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: Development of the life experiences survey. Journal of Consulting and Clinical Psychology. 1978;46:932–946. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schaffer M, Jeglic EL, Stanley B. The relationship between suicidal behavior, ideation, and binge drinking among college students. Archives of Suicide Research. 2008;12:124–132. doi: 10.1080/13811110701857111. [DOI] [PubMed] [Google Scholar]
- Schuckit MA. Alcohol-related disorders. In: Sadock BJ, Sadock VA, editors. Kaplan and Sadock’s comprehensive textbook of psychiatry. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. pp. 1168–1188. [Google Scholar]
- Sher L. Alcohol and suicide: Neurobiological and clinical aspects. Science World Journal. 2006a;6:700–706. doi: 10.1100/tsw.2006.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher L. Alcoholism and suicidal behavior: A clinical overview. Acta Psychiatrica Scandinavica. 2006b;113:13–22. doi: 10.1111/j.1600-0447.2005.00643.x. [DOI] [PubMed] [Google Scholar]
- Sher L, Oquendo M, Richardson-Vejlgaard R, Makhija N, Posner K, Mann J, et al. Effect of acute alcohol use on the lethality of suicide attempts in patients with mood disorders. Journal of Psychiatric Research. 2009;43:901–905. doi: 10.1016/j.jpsychires.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher L, Stanley B, Harkavy-Friedman J, Carballo J, Arendt M, Brent D, et al. Depressed patients with co-occurring alcohol use disorders: A unique patient population. Journal of Clinical Psychiatry. 2008;69:907–915. doi: 10.4088/jcp.v69n0604. [DOI] [PubMed] [Google Scholar]
- Siever LJ. Neurobiology of impulsive-aggressive personality-disordered patients. Psychiatric Times. 2002;19:37. [Google Scholar]
- Simons J. Differential prediction of alcohol use and problems: The role of biopsychological and social-environmental variables. The American Journal of Drug and Alcohol Abuse. 2003;29:861–879. doi: 10.1081/ada-120026265. [DOI] [PubMed] [Google Scholar]
- Simons J, Carey K, Gaher R. Lability and impulsivity synergistically increase risk for alcohol-related problems. American Journal of Drug and Alcohol Abuse. 2004;30:685–694. doi: 10.1081/ada-200032338. [DOI] [PubMed] [Google Scholar]
- Simons J, Gaher R, Correia C, Hansen C, Christopher M. An affective-motivational model of marijuana and alcohol problems among college students. Psychology of Addictive Behaviors. 2005;19:326–334. doi: 10.1037/0893-164X.19.3.326. [DOI] [PubMed] [Google Scholar]
- Sitharthan G, Hough M, Sitharthan T, Kavanagh D. The Alcohol Helplessness Scale and its prediction of depression among problem drinkers. Journal of Clinical Psychology. 2001;57:1445–1457. doi: 10.1002/jclp.1108. [DOI] [PubMed] [Google Scholar]
- Soares J, Macassa G, Grossi G, Viitasara E. Psychosocial correlates of hopelessness among men. Cognitive Behaviour Therapy. 2008;37:50–61. doi: 10.1080/16506070701628016. [DOI] [PubMed] [Google Scholar]
- Stephenson H, Pena-Shaff J, Quirk P. Predictors of college student suicidal ideation: Gender differences. College Student Journal. 2006;40:109–117. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: 2009. (Office of Applied Studies, NSDUH Series H-36, HHS Publication No. SMA 09-4434) [Google Scholar]
- Swahn M, Simon T, Hammig B, Guerrero J. Alcohol-consumption behaviors and risk for physical fighting and injuries among adolescent drinkers. Addictive Behaviors. 2004;29:959–963. doi: 10.1016/j.addbeh.2004.02.043. [DOI] [PubMed] [Google Scholar]
- Taylor J. Substance use disorders and cluster B personality disorders: Physiological, cognitive, and environmental correlates in a college sample. American Journal of Drug and Alcohol Abuse. 2005;31:515–535. doi: 10.1081/ada-200068107. [DOI] [PubMed] [Google Scholar]
- Thompson E, Mazza J, Herting J, Randell B, Eggert L. The mediating roles of anxiety, depression, and hopelessness on adolescent suicidal behaviors. Suicide and Life-Threatening Behavior. 2005;35:14–34. doi: 10.1521/suli.35.1.14.59266. [DOI] [PubMed] [Google Scholar]
- Tragesser S, Robinson J. The role of affective instability and UPPS impulsivity in borderline personality disorder features. Journal of Personality Disorders. 2009;23:370–383. doi: 10.1521/pedi.2009.23.4.370. [DOI] [PubMed] [Google Scholar]
- Tremblay P, Ewart L. The Buss and Perry Aggression Questionnaire and its relations to values, the Big Five, provoking hypothetical situations, alcohol consumption patterns, and alcohol expectancies. Personality and Individual Differences. 2005;38:337–346. [Google Scholar]
- Tuisku V, Pelkonen M, Kiviruusu O, Karlsson L, Ruuttu T, Marttunen M. Factors associated with deliberate self-harm behaviour among depressed adolescent outpatients. Journal of Adolescence. 2009;32:1125–1136. doi: 10.1016/j.adolescence.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Uhrlass D, Gibb B. Negative life events, self-perceived competence, and depressive symptoms in young adults. Cognitive Therapy and Research. 2007;31:773–783. [Google Scholar]
- Verona E, Sachs-Ericsson N, Joiner T. Suicide attempts associated with externalizing psychopathology in an epidemiological sample. The American Journal of Psychiatry. 2004;161:444–451. doi: 10.1176/appi.ajp.161.3.444. [DOI] [PubMed] [Google Scholar]
- Wasserman D, Geijer T, Sokolowski M, Rozanov V, Wasserman J. Nature and nurture in suicidal behavior, the role of genetics: Some novel findings concerning personality traits and neural conduction. Physiology & Behavior. 2007;92:245–249. doi: 10.1016/j.physbeh.2007.05.061. [DOI] [PubMed] [Google Scholar]
- Weyrauch K, Roy-Byrne P, Katon W, Wilson L. Stressful life events and impulsiveness in failed suicide. Suicide and Life-Threatening Behavior. 2001;31:311–319. doi: 10.1521/suli.31.3.311.24240. [DOI] [PubMed] [Google Scholar]
- Whiteside S, Lynam D. The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. [Google Scholar]
- Wilcox HC, Arria AM, Caldeira KM, Vincent KB, Pinchevsky GM, O'Grady KE. Prevalence and predictors of persistent suicide ideation, plans, and attempts during college. Journal of Affective Disorders. 2010;127:287–294. doi: 10.1016/j.jad.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox H, Conner K, Caine E. Association of alcohol and drug use disorders and completed suicide: An empirical review of cohort studies. Drug and Alcohol Dependence. 2004;76:S11–S19. doi: 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Williams P, Barclay L, Schmied V. Defining social support in context: A necessary step in improving research, intervention, and practice. Qualitative Health Research. 2004;14:942–960. doi: 10.1177/1049732304266997. [DOI] [PubMed] [Google Scholar]
- Windle M, Windle R. Alcohol consumption and its consequences among adolescents and young adults. In: Galanter M, editor. Recent developments in alcoholism, Vol. 17: Alcohol problems in adolescents and young adults. New York, NY: Kluwer Academic/Plenum; 2005. pp. 67–83. [DOI] [PubMed] [Google Scholar]
- Wingenfeld K, Mensebach C, Rullkoetter N, Schlosser N, Schaffrath C, Beblo T, et al. Relationship between coping with negative life-events and psychopathology: Major depression and borderline personality disorder. Psychology and Psychotherapy: Theory, Research and Practice. 2009;82:421–425. doi: 10.1348/147608309X452416. [DOI] [PubMed] [Google Scholar]
- Wojnar M, Ilgen M, Czyz E, Strobbe S, Klimkiewicz A, Jakubczyk A, et al. Impulsive and non-impulsive suicide attempts in patients treated for alcohol dependence. Journal of Affective Disorders. 2009;115:131–139. doi: 10.1016/j.jad.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaleski E, Levey-Thors C, Schiaffino K. Coping mechanisms, stress, social support, and health problems in college students. Applied Developmental Science. 1998;2:127–137. [Google Scholar]
- Zernicke K, Cantrell H, Finn P, Lucas J. The association between earlier age of first drink, disinhibited personality, and externalizing psychopathology in young adults. Addictive Behaviors. 2010;35:414–418. doi: 10.1016/j.addbeh.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet G, Dahlem N, Zimet S, Farley G. The multidimensional scale of perceived social support. Journal of Personality Assessment. 1988;52:30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]