Abstract
Objectives. We reviewed the English-language literature on the energy burden and environmental impact of health services.
Methods. We searched all years of the PubMed, CINAHL, and ScienceDirect databases for publications reporting energy consumption, greenhouse gas emissions, or the environmental impact of health-related activities. We extracted and tabulated data to enable cross-comparisons among different activities and services; where possible, we calculated per patient or per event emissions.
Results. We identified 38 relevant publications. Per patient or per event, health-related energy consumption and greenhouse gas emissions are quite modest; in the aggregate, however, they are considerable. In England and the United States, health-related emissions account for 3% and 8% of total national emissions, respectively.
Conclusions. Although reducing health-related energy consumption and emissions alone will not resolve all of the problems of energy scarcity and climate change, it could make a meaningful contribution.
Global warming is not a new concern. Since the late 1980s, scientists have described rising surface temperatures and increased climate variability,1–3 concurrent with mounting atmospheric carbon dioxide (CO2) concentrations.4–6 Rising surface temperatures and increasing atmospheric CO2 levels could coexist without one necessarily causing the other, but historical data suggest that this is unlikely,7 and it is difficult to ascribe recent atmospheric CO2 concentrations approaching 400 parts per million6 to natural processes and inherent variation: at no point did preindustrial CO2 levels exceed 300 parts per million.8
Concerns about energy scarcity and rising energy costs are also intensifying. The current global estimate for ultimately recoverable conventional oil is between 2.0 and 4.3 trillion barrels; this compares to cumulative production of 1.13 trillion barrels through 2007. That is, we have already consumed between 20% and 50% of all currently available conventional oil.9
Health professionals have been among the leaders of widespread advocacy for addressing climate change,10–16 as well as expressing mounting concerns about the effects of energy scarcity on public health and health services.17–20 What, though, is the health sector’s contribution to rising atmospheric CO2 levels and dwindling energy reserves? Understanding the energy consumption, greenhouse gas (GHG) emissions, and other environmental burdens associated with health services is important both to identify opportunities to minimize their environmental impact and to better guide their adaptation to a low-carbon economy. We reviewed the extant English-language literature on the energy burden and environmental impact of health services.
METHODS
Our search strategy is shown in Box 1. We searched all years of the PubMed, CINAHL, and ScienceDirect databases for terms intended to be as sensitive, rather than as specific, as possible. To supplement these searches, we conducted a secondary search targeting the Economics, Econometrics, and Finance subject subset of the ScienceDirect database with the search phrase “carbon footprint.” In addition, we manually searched the January 2009 through February 2011 tables of contents of 12 energy and environmental journals. Finally, we manually searched the reference lists of all identified papers to identify additional relevant articles. Our final update of the search was on March 4, 2011.
Search Strategies in Literature Review of Environmental Impact of Health Services
| PubMed and CINAHL |
| 1. exp greenhouse effect/ |
| 2. exp energy-generating resources/ |
| 3. 1 and 2 |
| 4. greenhouse gases.mp. |
| 5. greenhouse gasses.mp. |
| 6. carbon footprint.mp. |
| 7. carbon emissions.mp. |
| 8. 3 or 4 or 5 or 6 or 7 |
| 9. limit to English |
| ScienceDirect |
| 1. TITLE-ABSTR-KEY |
| ambulance |
| or hospital |
| 2. ALL |
| greenhouse gas* |
| or carbon footprint |
| or emissions |
| 3. 1 and 2 |
| Hand-searched tables of contents |
| Ecological Economics |
| Energy |
| Land Use Policy |
| Energy Economics |
| Energy Policy |
| Renewable Energy |
| Environmental Impact Assessment Review |
| Global Environmental Change |
| Journal of Cleaner Production |
| Journal of Environmental Economics and Management |
| Energy Conversion and Management |
Note. ABSTR = abstract; exp = explode; mp = multiple parameters; * = truncated (includes gas, gases, gasses, etc.).
We classified identified articles with a method similar to that used in previous public health–related literature surveys21,22 as original research, brief reports and research letters, advocacy articles and letters (including from trade journals), government agency reports, editorials and commentaries, and news items. For articles that reported energy consumption or emissions in health or medical settings, 1 author (L. H. B.) extracted and tabulated data to enable cross-comparisons among different activities and services; where possible, per patient or per event emissions were calculated. We classified energy and emissions inventories as scope 1, arising from direct energy consumption; scope 2, arising from purchased energy consumption, including electricity and commercial travel; scope 3, emissions arising from upstream and downstream production and waste disposal processes; and complete life cycle, representing the sum of scope 1, scope 2, and scope 3 emissions.23–25
RESULTS
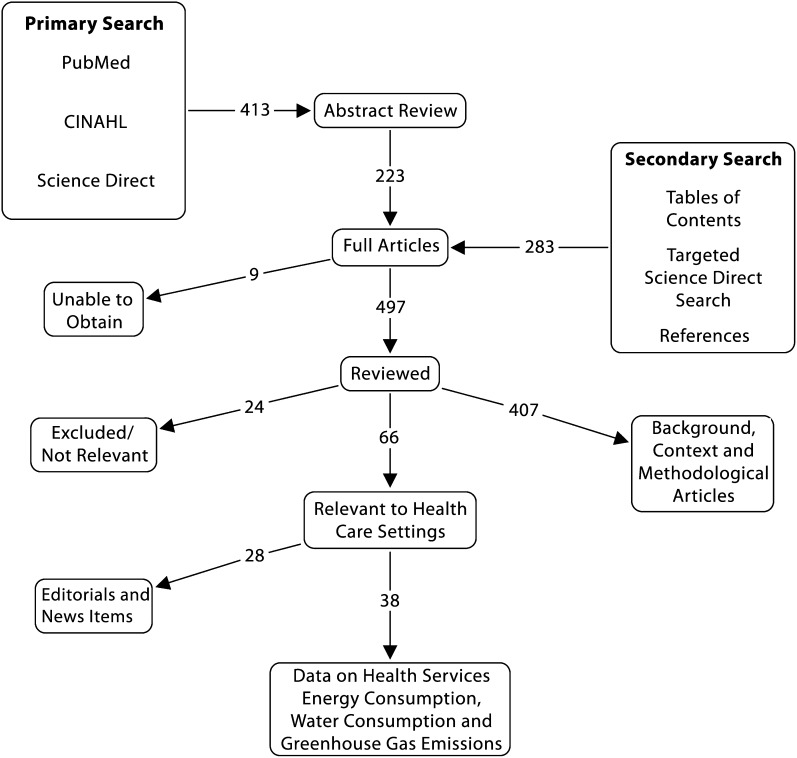
Figure 1 shows the search process and results at each step. The vast majority of the 497 articles identified for review addressed background related to GHG emissions and climate change or described methodological approaches to energy and emissions accounting. Sixty-six unique publications addressed energy consumption or GHG emissions by health-related activities. Twenty-eight (42%) of the publications were editorials, commentaries, nonresearch articles, or news items that did not contain any data; 38 (58%) of the publications provided data in some form, which we analyzed.
FIGURE 1—
Search process and search results at each step in literature review of environmental impact of health services.
National-Level Health Service Emissions
The most aggressive attempt to quantify health-related GHG emissions was undertaken by England’s National Health Service (NHS). An estimate derived from NHS expenditure data supplemented with more detailed data on building energy consumption and travel calculated the complete life cycle carbon footprint of the NHS for calendar year 2004 to be 21.3 million metric tons of CO2 equivalents, or approximately 3% of all emissions in England.26 Upstream and downstream (scope 3) emissions associated with procurement of supplies and equipment and disposal of wastes accounted for approximately 60% of the emissions; acquisition of pharmaceuticals was the greatest single contributor, accounting for 21% of total NHS emissions. A 2007 update estimated CO2 emissions generated by the NHS to be 21 million metric tons,27 with a projected increase to 23 million metric tons by 2020 in the absence of significant reductions in energy consumption.28
In the United States, Chung and Meltzer used published data on health expenditures for 2007 to calculate annual health care sector emissions.29 Complete life cycle emissions totaled 545.5 million metric tons of CO2 equivalents, with 46% being direct (scope 1 and scope 2) emissions from energy consumption and 54% being indirect (scope 3) emissions associated with upstream and downstream processes, including procurements. US health care sector emissions represented approximately 8% of the country's total GHG emissions for that year.
Hospitals and Health Facilities
Hospitals consume energy to provide lighting, power medical equipment, heat water, and supply heating and air conditioning.30–36 They also produce waste, from both single-use disposable supplies and waste water.35,37 Finally, indirect energy and environmental impacts are associated with their purchasing activities.35
Hospitals consume more energy than other nonresidential buildings per square meter of floor space, in part because of their continuous operation.32 The reported annual scope 1 and scope 2 energy consumption per square meter of floor space, or energy intensity, of hospitals, clinics, and other health facilities is remarkably consistent over both geography and time (Table 1), ranging roughly between 230 and 330 kilowatt hours per square meter,2,30–34 with the exception of 1 report from a single hospital in Spain.36 Murray et al. estimated that in 2001, the energy consumption of small health facilities in Scotland translated into 86 kilograms per square meter of scope 1 and scope 2 CO2 emissions.33 At that time, approximately 10% of Scotland’s electricity production came from renewable resources.38 Calculation of current GHG emissions from those facilities and the facilities represented in the other studies would have to take into account the current local energy mix (electricity, natural gas, etc.) and the primary fuel source used by their electricity supplier (coal, hydro, nuclear, etc.).
TABLE 1—
Studies of Energy Intensity of Hospitals and Other Health Facilities
| Country, Facilities, and Dates | Annual Energy Intensity, kWh/m2 |
| Greece32 | |
| Hospitals, health centers, and clinics, 1980 | 235 |
| Hospitals, health centers, and clinics, 2001 | 233 |
| Hospitals, health centers, and clinics, 2010 (projected) | 236 |
| Scotland33: small health buildings, 2001 | 310 |
| Poland30 | |
| University hospital, heat/hot water only, 2005–2008 | 268 |
| Provincial hospital, heat/hot water only, 2005–2008 | 327 |
| Malaysia34: public hospital, 2008 | 234 |
| Spain36 | |
| Hospital, total energy use, ∼2005 | 494 |
| Hospital, electricity only, ∼2005 | 169 |
| Thailand31: average of 79 hospitals, electricity only, 1996–2006 | 149 |
Heating domestic hot water requires substantial energy in hospitals; for example, it accounted for approximately 20% of the energy burden of 2 Polish hospitals.30 Conversion to water-saving taps is one strategy for reducing hospitals’ energy consumption and environmental impact.39,40 Other possible mechanisms include purchasing equipment with variable-speed electric motors,34 designing spaces to accentuate natural ventilation,41 and complying with modern building energy codes.31 Hospitals can also supplement their energy acquisition with on-site power generation, which can both save money36,42,43 and reduce GHG emissions.42,44 Chemical–electrical fuel cells42,44,45 and solar technologies44,46 have also been advocated as ways hospitals can reduce commercial energy consumption and lower GHG emissions. The payback time on the initial investment, however, currently makes these strategies economically nonviable: the most optimistic estimate is 11.5 years,46 and most estimates range from 20 to 30 years,42,44 which far exceeds the usable life of the proposed systems.
Surgery
Citing 2 multicenter trials that concluded that surgical management of gastric reflux is at least as efficacious—as measured by symptom recurrence and quality-adjusted life years—as medical management for gastric reflux, Gatenby argued that patients and physicians might consider the respective environmental impacts of the 2 approaches.47 He used data on expenditure-based emission intensities for the NHS and estimated that the initial complete life cycle carbon emissions from reflux surgery were nearly 7 times greater than from medical management, but that emissions from continuing treatment were much lower for surgical patients: 30 versus 100 kilograms of CO2 equivalents per year. He calculated that the surgical approach would become “carbon-efficient in the 9th post-operative year.”47(p73)
A 2009 study compared the paper and plastic waste, as well as the electricity consumed by specialized equipment, for the phacoemulsification and modified phacosection techniques for cataract surgery.48 Researchers also examined the number of patient visits required for the procedure and estimated the emissions associated with patient travel. The modified phacosection technique produced 280 grams less plastic waste and 8 grams less paper waste and used 0.168 kilowatt hours less electricity than did the phacoemulsification technique. Furthermore, the authors estimated that the ability to complete the entire modified phacosection procedure in a single visit—instead of the 5-visit strategy (referral, preoperative assessment, and postoperative appointments) used in phacoemulsificaiton—reduced travel-related CO2 emissions by 29.8 kilograms per procedure. Extrapolating these scope 1 and scope 2 findings to the 10.2 million cataract operations performed each year worldwide, the authors concluded,
The global impact of ophthalmology services is much less than 1 coal-fired power station per annum; nevertheless, ophthalmologists can reduce the ophthalmology carbon footprint and the impact of their practice without jeopardizing patient care.48(p203)
Two studies have explored the environmental impact of medical gases. Gilliam et al. evaluated direct CO2 emissions from laparoscopic surgeries.49 They estimated that a C-sized cylinder of compressed CO2 should last approximately 4 procedures and that each cylinder releases only 0.0009 metric tons (∼1 kg) of CO2 into the atmosphere. They concluded that “laparoscopic surgery uses only tiny amounts of CO2, [and] its impact on global warming is minimal.”49(p573) Ryan and Nielsen determined the 20-year global warming potentials of 3 common anesthetic gases—sevoflurane, isoflurane, and desflurane—and then applied them to clinical scenarios to estimate their relative environmental impacts.50 At a constant fresh gas flow rate of 2 liters per minute, sevoflurane had the lowest CO2 equivalents emissions (6.9 kg/h), followed by isoflurane (15.6 kg/h) and desflurane (187.2 kg/h). However, when the different flow rates at which the gases could be administered because of their different potencies were taken into account, emissions from isoflurane were similar to those of sevoflurane (3.9–7.8 kg/h), but emissions from desflurane remained significantly higher (46.8 kg/h). It is notable that neither of these studies considered the life cycle emissions associated with producing, bottling, and distributing medical gases, which could be substantial: approximately 4.6 metric tons of CO2 equivalents are emitted for every $1000 in purchases from US industrial gas manufacturers.51
Water Consumption
Dialysis consumes 120 to 800 liters of fresh water per treatment, depending on the type (clinic vs home) and duration of the therapy session.52–54 Much of that water is discarded in the reverse osmosis process that creates the dialysis fluid, and it is known as reject water. It is essentially bacteria free, with pH, turbidity, and electrolyte characteristics not unlike those of municipal and industrial water supplies.52–54 Recycling of reject water for gray water uses—for example, irrigating lawns or flushing toilets—has been advocated and has been tried in some settings.52 Recycling reject water is estimated to be less costly than generating fresh water through reverse osmosis of sea water.54 This practice, however, is not widespread. Only 2 of 58 renal units in England, Scotland, and Wales that participated in a survey on sustainability in kidney care reported having facilities for recycling reject water.55
Hot water production and consumption are significant issues for hospitals. Two studies evaluated water consumption during surgical scrubbing. Somner et al. observed scrubbing at 2 Scottish hospitals, one with elbow-controlled taps and one with knee-controlled taps; they measured the duration of tap activation with a stopwatch.40 Where the tap was elbow activated, the water ran for a mean of 2 minutes and 23 seconds per scrub; where the tap was knee activated, it was on for a mean of 1 minute and 7 seconds. This translated into a difference of 5.7 liters of water per scrub, and the authors estimated that changing all surgical sinks in the United Kingdom from elbow- to knee-activated taps would save approximately 11 000 gigajoules (3 000 000 kWh) in energy for heating water each year.
Jones conducted a similar study, collecting water from the drains of 3 different types of scrub bays used in a standardized 5-minute scrub routine: one with an elbow-controlled tap, one with a spring-loaded foot-controlled tap, and one with a motion sensor–controlled tap.39 When the water flow was turned off between rinses, the volume of water consumed was similar across the 3 types of taps (6.7–7.5 L), but only the spring-loaded foot-controlled tap turned off automatically between rinses. When taps ran continuously, they consumed 3 times as much water, and if taps were left continuously opened at a high flow rate, the amount of water consumed exceeded 50 liters per scrub. He concluded that water consumption for surgical scrubbing could “be reduced at an organizational level by either retrofitting older facilities or, when building new ones, by selecting the most water-sparing plumbing fixtures.”39(p320)
Other Health Service and Health-Related Activities
In 2011, a collaborative of Canadian and US emergency medical services agencies reported their energy consumption and carbon footprint for 1 year.56 Ten agencies reported scope 1 and scope 2 energy consumption to support ground ambulance operations, with emissions totaling 13 890 metric tons of CO2 equivalents. This equated to an average of 45.5 kilograms of CO2 equivalents per ambulance response, or 3.7 kilograms of CO2 equivalents per capita. Extrapolating these results to the entire US population, these authors estimated that emergency medical services in the nation produce between 660 000 and 1.6 million metric tons of scope 1 and scope 2 GHG emissions each year, or less than 1% of all health sector emissions. Diesel and gasoline consumption were responsible for 71.6% of the emergency services–related emissions.
The Sustainable Trials Study Group reported the emissions associated with the CRASH (Corticosteroid Randomisation After Significant Head Injury) trial, which evaluated the effect of corticosteroid administration on outcomes of adults with head injury.57 The 5-year trial recruited 10 008 participants from 49 nations. Scope 1 and scope 2 emissions for 1 year of the trial totaled 126 metric tons of CO2 equivalents; the investigators extrapolated emissions for the full 5-year trial to be 630 metric tons of CO2 equivalents, or approximately 63 kilograms of CO2 equivalents per study participant. The coordination center was responsible for 39% of the emissions, with nearly all of its emissions arising from electricity consumption. Distribution of study medications and documents was responsible for 28% of the emissions, and travel accounted for 23%. Recently, the investigators reported that they were able to substantially reduce study-related emissions in the CRASH-2 trial, primarily through increased efficiency in participant recruitment.58
In a letter to the British Medical Journal, Smith et al. described 3 examples of potential GHG emission reductions from use of telemedicine.59 They reported annual CO2 equivalents reductions of 705 kilograms for a United Kingdom neurologist, 39 metric tons for an Australian pediatric burns consultation service, and 33 220 metric tons from avoided home health visits in Canada. More recently, physicians at the University of California, Davis described their 5-year experience providing telemedicine consultations, speculating that the travel avoided by offering that service resulted in savings of 714 000 liters of gasoline and 1700 metric tons of CO2 emissions.60 Neither of these publications, however, reported original empirical research per se. Furthermore, the Canadian data described by Smith et al. was not referenced,59 and the cited articles describing the experiences of the United Kingdom neurologist61 and Australian burns unit62 did not contain the emissions data reported in the letter. These unsubstantiated reports raise the intuitive point that telemedicine could reduce health care–related travel and thus emissions, but more rigorous research is needed.
Several letters in the medical literature addressed the environmental impact of attendance at medical conferences, calling on organizations and individuals to purchase carbon offsets for their meeting-related travel and to use video conferencing to minimize travel-related emissions.63–66 The reported emissions from health-related activities are summarized in Table 2.
TABLE 2—
Reported Greenhouse Gas Emissions From Health Services
| Service/Procedure | Impact |
| Health care26,29 | Emits 21.3 million metric tons CO2e/y (England) |
| Emits 426 kg CO2e per capita/y (England) | |
| Emits 545.5 million metric tons CO2e/y (United States) | |
| Emits 1510 kg CO2e per capita/y (United States) | |
| Hospitals wards41 | Emit 48–171 kg CO2e/m2/y (varies by ventilation system) |
| Small health buildings33 | Emit 86 kg CO2e/m2 annually |
| EMS systems56 | Emit 45.5 kg CO2e/ambulance response (North America) |
| Emit 3.7 kg CO2e per capita/y (North America) | |
| Surgical reflux control47 | Emits 1081 kg CO2e/patient, plus 30.8 kg CO2e/y thereafter |
| Medical reflux control47 | Emits 164 kg CO2e/patient, plus 100 kg CO2e/y thereafter |
| Cataract surgery48 | Emits 37.3 kg CO2/operation (business as usual) |
| Emits 7.5 kg CO2/operation (1-stop strategy) | |
| Laparoscopic surgery49 | Emits 0.23 kg CO2/operation (from CO2 gas cylinders) |
| Anesthetic gases50 | Emit 7–187 kg CO2e/hour of administration |
| Clinical trials57 | Emit 63kg CO2e/participant |
| Emit 324 kg CO2e/primary endpoint event | |
| Telemedicine59,60 | Avoids 39 kg CO2/consultationa |
| Avoids 2.9 kg CO2e/home health visit avoideda | |
| Avoids 131 kg CO2/consultationa | |
| Medical meetings64,65 | Emit 723 kg CO2e/participant (American Thoracic Society)a |
| Emit 227 kg CO2e/participant (European Respiratory Society)a |
Note. CO2e = carbon dioxide equivalents; EMS = emergency medical services.
Anecdotal, secondary, or inferred data.
DISCUSSION
Despite widespread advocacy for action and leadership among physicians and other health professionals,10–16 the health sector is poorly represented in empirical studies of energy consumption and GHG emissions. We found that energy consumption by hospitals and other health facilities is the most widely studied aspect of health-related energy consumption and emissions, with much of that work undertaken by environmental, engineering, and architectural researchers.
The most sophisticated analysis of health-related emissions to date was undertaken by the NHS, demonstrating that its activities were responsible for 21.3 million metric tons of CO2 equivalents emissions in 2004 (426 kg/person).26 A more cursory examination found that US health services were responsible for 545.5 million metric tons of CO2 equivalents emissions in 2007 (1510 kg/person).29 Some of this difference in per capita health-related emissions is likely an artifact of using input–output analysis and aggregated emissions per unit of expenditure to calculate the respective carbon footprints. The difference might also be partly attributable to the structure of health services as well as health care consumption patterns in these 2 countries: per capita health expenditures in the United States are roughly 240% higher than in the United Kingdom.67 We did not find reports on aggregate health system emissions from other nations; to the extent that other nations’ health systems, energy infrastructures, and economic structures differ from those of the United States and the United Kingdom, their health-related emissions likely differ as well.
Perhaps the most important common finding of the US and United Kingdom studies was the substantial ( > 50%) contribution of indirect, scope 3 emissions to health services’ carbon footprint. This highlights the importance of evaluating complete life cycle inventories, including scope 3 emissions, when exploring health-related emissions. The fossil energy consumption and related emissions represented in the scope 1 and scope 2 carbon footprints of health services do not adequately characterize their total environmental impact, as is true of most products and services.24,25,68 If upstream and downstream effects are not considered in an organization’s environmental impact, emission reduction strategies could lower scope 1 and scope 2 emissions, and total emissions from upstream or downstream processes could actually rise.24 That is, direct emissions from an organization’s activities could decrease while total emissions into the atmosphere, the ultimate target of GHG mitigation efforts, could increase.
Emissions from health services are comparable to those of other important economic sectors. In the United States, for example, emissions from the agriculture sector total approximately 500 million metric tons of CO2 equivalents annually, representing around 7% of total national emissions.69 The waste management sector is responsible for approximately 3% of total emissions in the United Kingdom.70 Still, in light of the scale of global emissions—49 billion metric tons of CO2 equivalents in 200471—health services’ energy consumption and emissions may seem negligible. A comparison of US health sector emissions with total Australian emissions is instructive, however. In 2007 and 2008, Australia’s GHG emissions totaled 547 million and 553 million metric tons of CO2 equivalents, respectively72; US health sector emissions are of the same scale as Australia’s total national emissions. Although reducing health-related emissions alone would not solve all of the problems caused by GHGs and climate change, it could make a meaningful contribution: a 10% reduction in emissions from just the US health system would have the same atmospheric impact as a 10% reduction in emissions from the entire Australian economy.
Some health systems are already taking steps to minimize their environmental impact, most notably the systematic efforts of the NHS.28 A recent survey of 14 directors of primary care trusts in southwest England found that 7 were pursuing sustainability strategies, including the sourcing of green energy, green travel policies such as supporting cycling to work, procurement policies designed to minimize packaging and waste, and sourcing of local food products for cafeterias.73 Examples of other logical steps that health systems could take to reduce their energy and GHG consumption are incorporating natural ventilation and green building concepts when constructing or renovating health facilities31,41,44 and including more hybrid vehicles in the corporate fleet.74 Health systems and health professionals should not underestimate their potential influence on broader sustainability efforts; their stature within the community makes them ideal advocates.
A more practical and perhaps more immediate concern is how mounting energy scarcity, increasing energy costs, and societal pressures to reduce emissions might actually pose a threat to the delivery of health services. Health facilities depend on energy to operate,75 and energy costs have been shown to contribute to health care price inflation.20 Also, the plastics commonly used in medical equipment and medical supplies require petroleum feedstock.20,76 Understanding the energy consumption and emissions associated with health services is important not only to identify opportunities to minimize their environmental impact, but also to facilitate their adaptation to a low-carbon economy. Managing GHG emissions is managing energy consumption, and vice versa. It is a win–win proposition.
Our findings must be considered in the context of the limitations and biases inherent in the included studies and the limitations of our search and review processes. Only 2 of the studies we identified explored emissions from entire health systems; the remaining studies primarily provided data from single facilities that might not be representative of entire health systems, disciplines, or subspecialties. Many of the studies relied on existing financial or energy consumption data that had been collected for other purposes, which might have resulted in some information bias. Finally, our search was limited to English-language publications, and a single investigator conducted data abstraction.
Per patient or per event, health-related emissions are modest; in the aggregate, however, they are considerable. The literature provides evidence that modified practices can reduce the energy consumption of and emissions from some health services and activities. Interdisciplinary studies involving researchers from the health, energy, environmental, and economics disciplines are crucially needed to guide practice modifications and to establish a foundation for policy initiatives to ensure both the environmental and economic sustainability of health services.
Human Participant Protection
No protocol approval was required because no human participants were involved.
References
- 1.Hansen J, Lebedeff S. Global trends of measured surface air temperature. J Geophys Res. 1987;92(D11):13345–13372 [Google Scholar]
- 2.Hansen J, Lebedeff S. Global surface air temperatures: update through 1987. Geophys Res Lett. 1988;15(4):323–326 [Google Scholar]
- 3.Urban FE, Cole JE, Overpeck JT. Influence of mean climate change on climate variability from a 155-year tropical Pacific coral record. Nature. 2000;407(6807):989–993 [DOI] [PubMed] [Google Scholar]
- 4.Piver WT. Global atmospheric changes. Environ Health Perspect. 1991;96:131–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Solomon S, Qin D, Manning Met al. Climate Change 2007: The Physical Science Basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK: Cambridge University Press; 2007 [Google Scholar]
- 6. National Oceanic and Atmospheric Administration, Earth System Research Laboratory, Global Monitoring Division. Recent Mauna Loa CO2. Available at: http://www.esrl.noaa.gov/gmd/ccgg/trends. Accessed June 28, 2010.
- 7.Genthon G, Barnola JM, Raynaud Det al. Vostok ice core: climatic response to CO2 and orbital forcing changes over the last climatic cycle. Nature. 1987;329:414–418 [Google Scholar]
- 8.Barnola JM, Raynaud D, Korotkevich YS, Lorius C. Vostok ice core provides 160,000-year record of atmospheric CO2. Nature. 1987;329:408–414 [Google Scholar]
- 9.Sorrell S, Speirs J, Bentley R, Brandt A, Miller R. Global oil depletion: a review of the evidence. Energy Policy. 2010;38(9):5290–5295 [Google Scholar]
- 10.Butler CD. Lightening our carbon footprint: economics, norms and doctors. Med J Aust. 2010;192(9):485–486 [DOI] [PubMed] [Google Scholar]
- 11.Kefford RF. Medical heat for climate change. Med J Aust. 2006;184(11):582. [DOI] [PubMed] [Google Scholar]
- 12.Santa Barbara J. Foul weather ahead and we’re low on gas. Croat Med J. 2006;47(4):665–668 [PMC free article] [PubMed] [Google Scholar]
- 13.Sarfaty M, Abouzaid S. The physician’s response to climate change. Fam Med. 2009;41(5):358–363 [PubMed] [Google Scholar]
- 14.Sellman J, Hamilton JD. Global climate change and human health. Minn Med. 2007;90(3):47–50 [PubMed] [Google Scholar]
- 15.Simpson M. Reducing NHS carbon footprint: time for a culture change. BMJ. 2008;336(7649):848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woodruff RE, McMichael AJ, Hales S. Action on climate change: no time to delay. Med J Aust. 2006;184(11):539–540 [DOI] [PubMed] [Google Scholar]
- 17.Frumkin H, Hess J, Vindigni S. Peak petroleum and public health. JAMA. 2007;298(14):1688–1690 [DOI] [PubMed] [Google Scholar]
- 18.Hanlon P, McCartney G. Peak oil: will it be public health’s greatest challenge? Public Health. 2008;122(7):647–652 [DOI] [PubMed] [Google Scholar]
- 19.Wilkinson P. Peak oil: threat, opportunity or phantom? Public Health. 2008;122(7):664–666 [DOI] [PubMed] [Google Scholar]
- 20.Hess J, Bednarz D, Bae J, Pierce J. Petroleum and health care: evaluating and managing health care’s vulnerability to petroleum supply shifts. Am J Public Health. 2011;101(9):1568–1579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sanson-Fisher RW, Campbell EM, Htun AT, Bailey LJ, Millar CJ. We are what we do: research outputs of public health. Am J Prev Med. 2008;35(4):380–385 [DOI] [PubMed] [Google Scholar]
- 22.Sanson-Fisher RW, Campbell EM, Perkins JJ, Blunden SV, Davis BB. Indigenous health research: a critical review of outputs over time. Med J Aust. 2006;184(10):502–505 [DOI] [PubMed] [Google Scholar]
- 23.Council of Australian Governments Expert Group on Streamlining Greenhouse and Energy Reporting National Greenhouse and Energy Reporting Streamlining Protocol. Canberra: Commonwealth of Australia; 2009 [Google Scholar]
- 24.Matthews HS, Hendrickson CT, Weber CL. The importance of carbon footprint estimation boundaries. Environ Sci Technol. 2008;42(16):5839–5842 [DOI] [PubMed] [Google Scholar]
- 25.Purman JR. Tracking Your Carbon Footprint: A Step-by-Step Guide to Understanding and Inventorying Greenhouse Gas Emissions. New York, NY: iUniverse; 2008 [Google Scholar]
- 26.Sustainable Development Commission, Stockholm Environment Institute. NHS England Carbon Emissions Carbon Footprinting Report. London, UK: Sustainable Development Commission; 2008 [Google Scholar]
- 27.Saving Carbon, Improving Health. London, UK: NHS Sustainable Development Unit; 2010 [Google Scholar]
- 28.Brockway P. NHS at forefront of carbon modelling. Health Estate. 2010;64(9):33–38 [PubMed] [Google Scholar]
- 29.Chung JW, Meltzer DO. Estimate of the carbon footprint of the US health care sector. JAMA. 2009;302(18):1970–1972 [DOI] [PubMed] [Google Scholar]
- 30.Bujak J. Heat consumption for preparing domestic hot water in hospitals. Energy Build. 2010;42(7):1047–1055 [Google Scholar]
- 31.Chirarattananon S, Chaiwiwatworakul P, Hien VD, Rakkwamsuk P, Kubaha K. Assessment of energy savings from the revised building energy code of Thailand. Energy. 2010;35(4):1741–1753 [Google Scholar]
- 32.Gaglia AG, Balaras CA, Mirasgedis S, Georgopoulou E, Sarafidis Y, Lalas DP. Empirical assessment of the Hellenic non-residential building stock, energy consumption, emissions and potential energy savings. Energy Conversion Manag. 2007;48(4):1160–1175 [Google Scholar]
- 33.Murray J, Pahl O, Burek S. Evaluating the scope for energy-efficiency improvements in the public sector: benchmarking NHSScotland’s smaller health buildings. Energy Policy. 2008;36(3):1236–1242 [Google Scholar]
- 34.Saidur R, Hasanuzzaman M, Yogeswaran S, Mohammed HA, Hossain MS. An end-use energy analysis in a Malaysian public hospital. Energy. 2010;35(12):4780–4785 [Google Scholar]
- 35.Daschner FD, Dettenkofer M. Protecting the patient and the environment—new aspects and challenges in hospital infection control. J Hosp Infect. 1997;36(1):7–15 [DOI] [PubMed] [Google Scholar]
- 36.Renedo CJ, Ortiz A, Mañana M, Silió D, Pérez S. Study of different cogeneration alternatives for a Spanish hospital center. Energy Build. 2006;38(5):484–490 [Google Scholar]
- 37.Karagiannidis A, Papageorgiou A, Perkoulidis G, Sanida G, Samaras P. A multi-criteria assessment of scenarios on thermal processing of infectious hospital wastes: a case study for Central Macedonia. Waste Manag. 2010;30(2):251–262 [DOI] [PubMed] [Google Scholar]
- 38. Scottish Government. Renewable energy. Available at: http://www.scotland.gov.uk. Accessed November 28, 2011.
- 39.Jones EE. Water use in the surgical scrub: surgeons can reduce their environmental footprint. ANZ J Surg. 2009;79(5):319–320 [DOI] [PubMed] [Google Scholar]
- 40.Somner JEA, Stone N, Koukkoulli A, Scott KM, Field AR, Zygmunt J. Surgical scrubbing: can we clean up our carbon footprints by washing our hands? J Hosp Infect. 2008;70(3):212–215 [DOI] [PubMed] [Google Scholar]
- 41.Lomas KJ, Ji Y. Resilience of naturally ventilated buildings to climate change: advanced natural ventilation and hospital wards. Energy Build. 2009;41(6):629–653 [Google Scholar]
- 42.Bizzarri G, Morini GL. Greenhouse gas reduction and primary energy savings via adoption of a fuel cell hybrid plant in a hospital. Appl Therm Eng. 2004;24(2–3):383–400 [Google Scholar]
- 43.Lozano MA, Ramos JC, Carvalho M, Serra LM. Structure optimization of energy supply systems in tertiary sector buildings. Energy Build. 2009;41(10):1063–1075 [Google Scholar]
- 44.Bizzarri G, Morini GL. New technologies for an effective energy retrofit of hospitals. Appl Therm Eng. 2006;26(2–3):161–169 [Google Scholar]
- 45.Damberger TA. Fuel cells for hospitals. J Power Sources. 1998;71(1–2):45–50 [Google Scholar]
- 46.Tsoutsos T, Aloumpi E, Gkouskos Z, Karagiorgas M. Design of a solar absorption cooling system in a Greek hospital. Energy Build. 2010;42(2):265–272 [Google Scholar]
- 47.Gatenby PAC. Modelling the carbon footprint of reflux control. Int J Surg. 2011;9(1):72–74 [DOI] [PubMed] [Google Scholar]
- 48.Somner J, Scott K, Morris D, Gaskell A, Shepherd I. Ophthalmology carbon footprint: something to be considered? J Cataract Refract Surg. 2009;35(1):202–203 [DOI] [PubMed] [Google Scholar]
- 49.Gilliam AD, Davidson B, Guest J. The carbon footprint of laparoscopic surgery: should we offset? Surg Endosc. 2008;22(2):573. [DOI] [PubMed] [Google Scholar]
- 50.Ryan SM, Nielsen CJ. Global warming potential of inhaled anesthetics: application to clinical use. Anesth Analg. 2010;111(1):92–98 [DOI] [PubMed] [Google Scholar]
- 51. Carnegie–Mellon University Green Design Institute. Economic input-output life cycle assessment (EIO-LCA), US 2002. Purchaser price model. Available at: http://www.eiolca.net. Accessed December 15, 2010.
- 52.Agar JWM. Conserving water in and applying solar power to haemodialysis: ‘green dialysis’ through wiser resource utilization. Nephrology (Carlton). 2010;15(4):448–453 [DOI] [PubMed] [Google Scholar]
- 53.Agar JWM, Simmonds RE, Knight R, Somerville CA. Using water wisely: new, affordable, and essential water conservation practices for facility and home hemodialysis. Hemodial Int. 2009;13(1):32–37 [DOI] [PubMed] [Google Scholar]
- 54.Tarrass F, Benjelloun M, Benjelloun O. Recycling wastewater after hemodialysis: an environmental analysis for alternative water sources in arid regions. Am J Kidney Dis. 2008;52(1):154–158 [DOI] [PubMed] [Google Scholar]
- 55.Connor A, Mortimer F. The green nephrology survey of sustainability in renal units in England, Scotland and Wales. J Ren Care. 2010;36(3):153–160 [DOI] [PubMed] [Google Scholar]
- 56.Blanchard IE, Brown LH. Carbon footprinting of North American emergency medical services systems. Prehosp Emerg Care. 2011;15(1):23–29 [DOI] [PubMed] [Google Scholar]
- 57.Sustainable Trials Study Group Towards sustainable clinical trials. BMJ. 2007;334(7595):671–673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Subaiya S, Hogg E, Roberts I. Reducing the environmental impact of trials: a comparison of the carbon footprint of the CRASH-1 and CRASH-2 clinical trials. Trials. 2011;12(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Smith AC, Patterson V, Scott RE. Reducing your carbon footprint: how telemedicine helps. BMJ. 2007;335(7629):1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yellowlees PM, Chorba K, Burke Parish Met al. Telemedicine can make healthcare greener. Telemed J E Health. 2010;16(2):229–232 [DOI] [PubMed] [Google Scholar]
- 61.Patterson V. Teleneurology. J Telemed Telecare. 2005;11(2):55–59 [DOI] [PubMed] [Google Scholar]
- 62.Smith AC, Kimble RM, O’Brien A, Mill J, Wootton R. A telepaediatric burns service and the potential travel savings for families living in regional Australia. J Telemed Telecare. 2007;13(suppl 3):76–79 [Google Scholar]
- 63.Roberts I, Godlee F. Reducing the carbon footprint of medical conferences. BMJ. 2007;334(7589):324–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Crane J, Caldwell B. Another inconvenient truth? BMJ. 2006;333:1256 [Google Scholar]
- 65.Callister MEJ, Griffiths MJD. The carbon footprint of the American Thoracic Society meeting. Am J Respir Crit Care. 2007;175(4):417. [DOI] [PubMed] [Google Scholar]
- 66.Hudson S. Carbon emissions. ANZ J Surg. 2008;78(12):1137. [DOI] [PubMed] [Google Scholar]
- 67. Organization for Economic Co-operation and Development. OECD Health Data 2010. Available at: http://www.oecd.org/health. Accessed March 5, 2011.
- 68.Huijbregts MAJ, Rombouts LJA, Hellweg Set al. Is cumulative fossil energy demand a useful indicator for the environmental performance of products? Environ Sci Technol. 2006;40(3):641–648 [DOI] [PubMed] [Google Scholar]
- 69.Inventory of U.S. Greenhouse Gas Emissions and Sinks: 1990–2009. Washington, DC: Environmental Protection Agency; 2011 [Google Scholar]
- 70.U.K. Climate Change Sustainable Development Indicator: 2009 Greenhouse Gas Emissions, Final Figures. London: United Kingdom Department of Energy and Climate Change; 2011 [Google Scholar]
- 71. Climate Change 2007: Synthesis Report—Summary for Policymakers. Geneva, Switzerland: Intergovernmental Panel on Climate Change; 2007.
- 72.Department of Climate Change Australia’s National Greenhouse Accounts. Canberra: Commonwealth of Australia; 2009 [Google Scholar]
- 73.Nichols A, Richardson J. Climate change, health and sustainability: a brief survey of primary care trusts in the south west of England. Perspect Public Health. 2011;131(2):82–84 [DOI] [PubMed] [Google Scholar]
- 74.Hawkins SC. The green machine. Development of a high-efficiency, low-pollution EMS response vehicle. JEMS. 2008;33(7):108–120 [DOI] [PubMed] [Google Scholar]
- 75.Bailey DM. Energy contingency planning for health facilities: conference report. Public Health Rep. 1980;95(1):58–61 [PMC free article] [PubMed] [Google Scholar]
- 76.Clark GB, Kline B. Impact of oil shortage on plastic medical supplies. Public Health Rep. 1981;96(2):111–115 [PMC free article] [PubMed] [Google Scholar]