Abstract
Objectives. We assessed the longitudinal association between housing transitions and pregnancy outcomes in a sample of public housing residents.
Methods. A cohort of 2670 Black women residing in Atlanta, Georgia, housing projects with 1 birth occurring between 1994 and 2007 was created from maternally linked longitudinal birth files and followed for subsequent births. Traditional regression and marginal structural models adjusting for time-varying confounding estimated the risk of preterm low birth weight (LBW) or small for gestational age LBW by maternal housing transition patterns.
Results. Women moving from public to private housing as a result of housing project demolition were at elevated risk for preterm LBW (risk ratio = 1.74; 95% confidence interval = 1.00–3.04) compared with women not affected by project demolition. Other non–policy-related housing transition patterns were not associated with pregnancy outcomes.
Conclusions. Further longitudinal study of housing transitions among public housing residents is needed to better understand the relationship between housing, neighborhoods, housing policy, and perinatal outcomes.
Under the auspices of Roosevelt’s New Deal in 1936, Atlanta, Georgia, led the nation by establishing Techwood Homes as the first public housing project in the United States.1 Initially envisioned as a tool for economic development, public housing evolved nationally into a critical and often criticized component of the social safety net. Although meeting demands for affordable housing, the location, design, and regulation of some high-density public housing projects in US metropolitan areas have also contributed to persistent racial residential segregation and the concentration of poverty.2,3
In 1992, Congress passed the Housing Opportunities for People Everywhere initiative to support, in part, the redevelopment and deconcentration of traditional public housing projects. Before the 1996 Summer Olympics in Atlanta, the Atlanta Housing Authority (AHA) once again led the nation by initiating a decommissioning and demolition process for 29 of Atlanta’s distressed family occupied public housing projects,4 replacing them with mixed-income housing developments and transitioning most public housing recipients to Housing Choice Vouchers (formerly Section 8) for use in the private rental market.5 Residence in high poverty neighborhoods has been associated with poor health outcomes,6,7 but it is not clear whether the voluntary or involuntary transition of individuals out of traditional housing projects results in lower poverty destination neighborhoods, and if so, whether this improves health. There are mixed findings with regards to health following voluntary residential mobility interventions such as Moving to Opportunity.8–10
The persistence of racial and economic disparities in pregnancy outcomes, including the 2 main components of infant low birth weight (LBW)—preterm birth (< 37 weeks’ gestation) and fetal growth restriction—have been widely described. Such disparities are hypothesized to exist in part because of the sensitivity of pregnancy to acute and cumulative social exposures and determinants.11–13 In particular, residential neighborhood characteristics, including violent crime, income inequality, residential segregation, and deprivation, explain some of the racial disparities in poor pregnancy outcomes.14–18 Social, behavioral, and medical risk factors for poor outcomes may interact through various pathways, including access to preconceptional primary care and perinatal care, accessibility of healthy foods and safe environments for physical activity, physiologic effects of accumulated exposure to stressors, or behavioral response (e.g., smoking) to stressors and targeted tobacco and alcohol marketing. Women residing in public housing projects generally have high health burdens19 and may be exposed to chronic stress from high crime and poverty rates. However, residence in housing project communities could also be a source of social support networks and result in access to targeted social and health services.
There are similarities in the identified risk factors for preterm birth and fetal growth restriction (commonly operationalized as small for gestational age or < 10th percentile of weight for gestational age20). However, the relative importance of hypothesized etiologic factors such as smoking, stress, and reproductive tract infection differs for each outcome. For instance, smoking, low maternal weight gain, and pregnancy-induced hypertension may be more important population drivers of small for gestational age risk, whereas inflammation or infection and chronic stress may be relatively more important for preterm birth.21 These factors could be variably influenced by housing and neighborhood characteristics, including local access to health services and healthy foods, local social networks and support, and exposure to stressful environments.
This study aims to take advantage of a unique longitudinal data set and a significant change in public housing policy to answer 2 research questions. (1) Are housing transition patterns of women ever residing in public housing projects associated with subsequent pregnancy outcomes? (2) Is housing transition resulting from public housing project decommissioning associated with subsequent pregnancy outcomes?
METHODS
A retrospective cohort of women residing in Atlanta public housing at the time of at least 1 birth were followed for subsequent births, with pregnancy outcomes contrasted across women with differing interpregnancy residential transitions.
We used maternal longitudinally linked birth data derived by the Office of Health Indicators for Planning of the Georgia Department of Public Health from all live births to Georgia residents from 1994 to 2007. Maternally linked birth files represent birth certificate information for sets of siblings or half siblings sharing a common mother. Geocoded maternal residence on each birth certificate therefore describes a partial residential history for the mother, measured at the times of sequential births. The longitudinal linkage was established using a deterministic algorithm that matched records based on equivalence on key identifying variables, including portions of the woman’s name and date of birth (Appendix A, available as a supplement to the online version of this article at http://www.ajph.org).
Combining these geocoded birth records with maps of all family-type public housing projects administered by the AHA, we identified every birth event recorded to a mother residing in AHA housing between 1994 and 2007 (a detailed description of the spatial linkage process can be obtained in Appendix B, available as a supplement to the online version of this article at http://www.ajph.org). Cohort eligibility was established with a woman’s first measured birth in traditional AHA projects (baseline birth), and then each woman was followed forward in time for all subsequent births and residences (follow-up births; Figure A, available as a supplement to the online version of this article at http://www.ajph.org). Median geocode locational error for birth records in urban Atlanta is small.22 We excluded 2% of births that did not have geocode accuracy at the street or census block level. Only 2% of the identified women were not Black, so we further restricted the cohort to Black women. There were 62 follow-up births to women residing in the new mixed-income developments that replaced AHA projects. This was an insufficient sample size to make inference about mixed-income housing, and these were excluded.
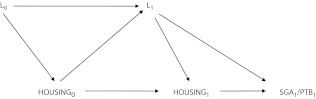
FIGURE 1—
Directed acyclic graph of possible time-varying confounding.
Note. PTB = preterm birth; SGA = small for gestational age. The exposure is housing transition measured as the housing at a baseline birth (HOUSING0) and a follow-up birth (HOUSING1). The pregnancy outcome is measured at the follow-up birth as SGA1 or PTB1. A vector of covariates (L) is also measured at baseline and follow-up. Time-varying confounding could bias effect estimates if previous exposure (HOUSING0) affected subsequent covariates (L1), making L1 both a confounder and a mediator of the housing-pregnancy outcome association.
Defining the Exposures
Our research questions focused on the effects of longitudinal housing change on subsequent pregnancy outcomes. Although the outcome of interest occurred at a single (follow-up) birth, the exposure was defined by the combination of the residence at 2 birth events (Figure A available as a supplement to the online version of this article at http://www.ajph.org). Each birth to a mother residing in AHA public housing projects was categorized as public housing. Any follow-up births where the mother did not reside in AHA projects were categorized private market housing. Many private residences are supported by Housing Choice Vouchers,23 although we could not confirm which private residents had voucher support.
The first research question concerned general housing transitions (e.g., irrespective of project closure); for a pair of birth events, the housing transition patterns could include “public–public,” “public–private,” or “private–private.” The latter category was possible because many women were followed over 3 or more pregnancies and, thus, could have the cohort-establishing public housing birth followed by 2 or more births in the private market.
The second research question concerned women whose transition out of a given public housing project was plausibly a result of the demolition of that project as part of the changing housing policy. We considered a woman “exposed” to a policy-induced transition if she had a birth while living in public housing within 1 year preceding that project’s closure date, and then had a follow-up birth while residing in a different project or in private housing.
Defining the Outcomes and Covariates
The exposure (a 2-birth sequence of housing status) and covariates were constructed from information captured at each birth from the baseline through follow-up. However, the outcomes were only captured from follow-up births. The unit of analysis was a “birth-pair” or “housing transition event” with exposure and covariates gathered from both events in the pair, but outcomes were only gathered from the latter. The outcomes were defined as preterm low birth weight (LBW; < 37 weeks' gestation, < 2500 g) and small for gestational age LBW ( < 10th percentile weight for age, < 2500 g). A small proportion of births (n = 80) were classified as both preterm LBW and small for gestational age LBW. These observations were included in each outcome because excluding them did not change results. Gestational age was assessed using last menstrual period and clinical estimates as reported on the birth certificate,24 and small for gestational age was determined using national birth weight gestational age norms.20
Individual variables assessed from each measured birth certificate included maternal age (continuous), smoking, education, parity, history of a preterm birth or small for gestational age birth, Kotelchuk index for adequacy of prenatal care,25 whether Medicaid was the payor for delivery, the length of the interpregnancy interval, and, to adjust for temporal trends, the year of birth. An indicator variable for whether the mother changed residence between 2 births was included to adjust for differential residential mobility within public or private housing categories. Census data were used to estimate tract-level proportion of households at or below the federal poverty level and proportion of tract residents who were Black.
Causal Framework for Analysis
In observational research, attempts to estimate causal effects of an exposure may be limited by several biases, including confounding, or lack of comparability in exposed and unexposed groups. Standardization and statistical regression adjusting for important confounders are common techniques to reduce confounding. However, in a longitudinal setting where both exposure and covariates can change over time, there is a possibility that a variable is simultaneously a confounder and an intermediary between a previous exposure and the outcome. For example, in Figure 1, covariates (e.g., smoking) are measured upon baseline entry into the cohort (L0), and again at subsequent follow-up births (L1). These covariates could confound the association between housing status and pregnancy outcome at a point in time. However, if past exposure (HOUSING0) leads to subsequent smoking (L1; e.g., in response to stressors or targeted neighborhood tobacco marketing), then smoking at event 1 is both a confounder of the current housing-pregnancy outcome association and a mediator of the past housing-pregnancy outcome association. Such time-varying confounding could plausibly exist for other covariates, including interpregnancy interval (because previous housing may be associated with access to and utilization of contraceptive services), utilization of prenatal care, and education. Traditional regression modeling cannot adjust for time-varying confounding, but a new class of models, marginal structural models, has been proposed as one approach to address this concern. Marginal structural models use the inverse probability of treatment as a weight to approximate groups representing counterfactual exposure transitions (e.g., longitudinal housing transition patterns) that are balanced with regards to time-varying confounder histories. The theoretical justification has been more fully described elsewhere.26,27 We adapted the approach of previous work that applied marginal structural models in longitudinal perinatal28 and social epidemiology applications29; a more detailed description of our modeling approach is available in Appendix C (available as a supplement to the online version of this article at http://www.ajph.org).
We estimated the risk ratios for the effect of housing transition patterns on each outcome (preterm LBW, small for gestational age LBW) by using Poisson regression models adjusting for measured covariates in multivariable regression models30 and marginal structural models adjusting for time-varying confounding. Sensitivity analyses restricted to women with only 1 or 2 follow-up births assessed for undue influence of women with many follow-up births. Comparison of deterministically linked and unlinked births was conducted to assess possible bias from record linkage. All models were fit using PROC GENMOD in SAS version 9.2 (SAS Institute, Cary, NC) using robust standard errors to account for repeated events within each woman and weights in marginal structural models.
RESULTS
Initial linkage of births to women ever residing in AHA projects and follow-up births yielded 5389 unique women delivering 10 609 infants. Exclusion of birth events with low-quality geocodes, multiple gestations, and non-Black mothers reduced the number of infants by 813, and the number of unique women by 209. Because the unit of analysis was a birth-pair transition, only women who had a baseline and at least 1 follow-up birth were analyzed, resulting in 4616 birth transition pairs to 2670 unique women.
Of the women, 36% contributed only 1 follow-up birth after the baseline birth event, whereas 49% contributed 2 or 3 follow-up births (Figure B available as a supplement to the online version of this article at http://www.ajph.org). The risks of preterm LBW and small for gestational age LBW were 8.6% and 6.4%, respectively (Table 1). Risk of preterm LBW was higher for adolescent mothers and mothers older than 35 years, multiparous mothers, smokers, or mothers with a history of preterm birth or small for gestational age birth. By contrast, the risk for preterm small for gestational age birth was only elevated for smoking mothers and mothers with a history of preterm birth or small for gestational age birth. Of follow-up births, 63% were paid for by Medicaid and 96% occurred to unmarried women.
TABLE 1—
Distribution of Singleton Pregnancy Outcomes by Maternal Characteristics at Time of Follow-up Birth Event: Study of the Perinatal Consequences of Changing Public Housing Policy, Atlanta, GA, 1994–2007
| PT-LBW |
SGA-LBW |
||||
| No. of Birth-Pair Transitions | % | P | % | P | |
| Total | 4616 | 8.6 | 6.4 | ||
| Age, y | < .001 | .578 | |||
| 10–17 | 140 | 10.0 | 7.9 | ||
| 18–24 | 2400 | 7.0 | 6.1 | ||
| 25–34 | 1897 | 9.3 | 6.4 | ||
| ≥ 35 | 179 | 20.7 | 8.4 | ||
| Education | .517 | .131 | |||
| No high school | 2334 | 8.0 | 6.9 | ||
| High school | 1848 | 8.9 | 5.7 | ||
| At least some college | 350 | 8.9 | 4.9 | ||
| Missing | 84 | 15.5 | 11.9 | ||
| Marital status | .423 | .729 | |||
| Married | 179 | 11.2 | 5.0 | ||
| Unmarried | 4436 | 8.5 | 6.4 | ||
| Parity | < .001 | .168 | |||
| Second or third birth | 2280 | 6.6 | 5.9 | ||
| Fourth or higher birth | 2336 | 10.4 | 6.6 | ||
| Adequacy of prenatal care (Kotelchuk index) | < .001 | .115 | |||
| Inadequate | 1292 | 8.4 | 6.5 | ||
| Intermediate | 477 | 6.5 | 5.9 | ||
| Adequate | 1253 | 3.9 | 5.0 | ||
| Adequate plus | 1190 | 13.5 | 7.3 | ||
| Missing | 404 | 11.4 | 7.9 | ||
| Interpregnancy interval | .09 | .474 | |||
| < 6 mo | 691 | 10.6 | 7.4 | ||
| ≥ 6 mo | 3899 | 8.2 | 6.2 | ||
| Missing | 26 | 3.9 | 7.7 | ||
| Smoking | < .001 | < .001 | |||
| Yes | 503 | 15.7 | 11.1 | ||
| No | 3993 | 7.5 | 5.8 | ||
| Missing | 120 | 15.0 | 6.7 | ||
| Previous preterm birth | < .001 | < .001 | |||
| Yes | 668 | 22.0 | 13.9 | ||
| No | 3948 | 6.3 | 5.1 | ||
| Payor | .002 | .813 | |||
| Medicaid | 2796 | 7.9 | 6.4 | ||
| Other | 1636 | 10.1 | 6.3 | ||
| Housing transition patternsa | .001 | .031 | |||
| Public–public | 1689 | 8.2 | 7.8 | ||
| Public–private | 1810 | 7.2 | 5.4 | ||
| Private–-public | 170 | 8.8 | 5.3 | ||
| Private–private | 947 | 11.6 | 5.9 | ||
| Policy-induced housing transitionb | .011 | .71 | |||
| Exposed | 525 | 11.8 | 8.0 | ||
| Unexposed | 1768 | 8.2 | 7.5 | ||
Note. PT-LBW = preterm low birth weight (< 37 weeks' gestation and < 2500 g); SGA-LBW = small for gestational age low birth weight (< 10th percentile weight for gestational age and < 2500 g).
Housing transition patterns between 2 consecutive births to the same woman. Public refers to residence in traditional public housing projects. Private refers to residence not in an Atlanta Housing Authority (AHA) property, presumably in the private housing market.
Subset of births could be categorized as exposed or unexposed to policy-induced housing transitions. Exposure is defined as maternal residence in an AHA public housing project within 12 months preceding demolition, followed by subsequent birth in private housing or different AHA public housing. The referent unexposed group is women with 2 consecutive births in the same AHA public housing project.
In terms of housing transitions, 37%, 39%, and 21% of births occurred to mothers with public-public, public-private, and private-private transitions, respectively. Preterm LBW occurred most frequently among women with the private-private pattern (11.6%), whereas women with the public–public pattern had the highest risk for small for gestational age LBW (7.8%). Five hundred twenty-five births followed maternal exposure to policy-induced transition out of public housing. Compared with women unexposed to policy-induced housing transition, women in this category experienced higher risk for preterm LBW (P = .011), but not small for gestational age LBW (P = .71).
Residents of public housing projects lived in tracts with high segregation (mean tract = 91.5% Black) and poverty (mean tract poverty rate = 42%). Women who transitioned from public to private market housing experienced an average 31% decrease in neighborhood poverty rate, although only a 0.1% decrease in tract percentage Black (Table A, available as a supplement to the online version of this article at http://www.ajph.org).
Multivariable regression and marginal structural model risk ratios for the effect of housing transition patterns on pregnancy outcomes are reported in Table 2. There was a consistently null association between preterm LBW and women with public-private patterns compared with public-public housing transition patterns, whereas women who had 2 consecutive births in the private market had modestly, but not significantly, elevated risk compared with public-public patterns (marginal structural model risk ratio [RR] = 1.39; 95% confidence interval [CI] = 0.90, 2.14). By contrast, for small for gestational age LBW both public–private and private–private patterns experienced lower risk than did public–public patterns, although the CIs from the marginal structural model in both cases included the null value.
TABLE 2—
Regression and Marginal Structural Model Associations of Housing Transition Patterns With Subsequent Pregnancy Outcomes: Study of the Perinatal Consequences of Changing Public Housing Policy, Atlanta, GA, 1994–2007
| Public–Private vs Public–Public, RR (95% CI) | Private–Private vs Public–Public, RR (95% CI) | |
| PT-LBW | ||
| Crude | 0.95 (0.77, 1.16) | 1.45 (1.12, 1.87) |
| Adjusted for individual factorsa | 1.02 (0.80, 1.30) | 1.25 (0.94, 1.66) |
| Adjusted for individual and area variablesb | 1.14 (0.87, 1.51) | 1.43 (1.04, 1.96) |
| Marginal structural modelc | 1.03 (0.70, 1.52) | 1.39 (0.90, 2.14) |
| SGA-LBW | ||
| Crude | 0.75 (0.59, 0.95) | 0.68 (0.49, 0.95) |
| Adjusted for individual factorsa | 0.93 (0.70, 1.24) | 0.77 (0.53,1.13) |
| Adjusted for individual and area variablesb | 0.94 (0.66, 1.33) | 0.77 (0.50, 1.18) |
| Marginal structural modelc | 1.01 (0.66, 1.55) | 0.70 (0.37, 1.33) |
Note. CI = confidence interval; PT-LBW = preterm low birth weight (< 37 weeks' gestation and < 2500 g); RR = risk ratio; SGA-LBW = small for gestational age low birth weight (< 10th percentile weight for gestational age and < 2500 g).
Adjusted for maternal age and age-squared at first measured birth, housing at first measured birth, and current maternal age, age-squared, parity, smoking, education, history of preterm or SGA birth, interpregnancy interval, adequacy of prenatal care, Medicaid status, year of birth, and indicator for whether mother moved to different tract since last birth.
Area variables include percentage of households below federal poverty level in the census tract and percentage of Black in the census tract.
Marginal structural models adjusted for time-varying confounding by the same covariates included in the traditional regression models via inverse probability of treatment weighting.
Table 3 presents model results for the second research question regarding the effect of exposure to housing policy-induced residential relocation. Women exposed compared with those unexposed to policy-induced housing transitions experienced increased risk for preterm LBW (RR = 1.74; 95% CI = 1.00, 3.04) but not small for gestational age LBW (RR = 0.69; 95% CI = 0.33, 1.24). Results from sensitivity analyses restricting to only first and second follow-up births were similar to full-sample analyses for each research question, although the effect of exposure to policy-induced transition on preterm LBW was attenuated in marginal structural models to RR of 1.35 (95% CI = 0.66, 2.75; Tables B and C, available as supplements to the online version of this article at http://www.ajph.org).
TABLE 3—
Association of Women’s Exposure to Policy-induced Housing Transition on Subsequent Pregnancy Outcomes: Study of the Perinatal Consequences of Changing Public Housing Policy, Atlanta, GA, 1994–2007
| PT-LBW, RRa (95% CI) | SGA-LBW, RRa (95% CI) | |
| Crude | 1.39 (1.04, 1.86) | 1.02 (0.70, 1.47) |
| Adjusted for individual factorsb | 1.37 (0.96, 1.95) | 1.37 (0.89, 2.11) |
| Adjusted for individual and area variablesc | 1.43 (0.99, 2.08) | 1.47 (0.91, 2.37) |
| Marginal structural modeld | 1.74 (1.00, 3.04) | 0.69 (0.33, 1.24) |
Note. CI = confidence interval; PT-LBW = preterm low birth weight (< 37 weeks' gestation and < 2500 g); RR = risk ratio; SGA-LBW = small for gestational age low birth weight (< 10th percentile weight for gestational age and < 2500 g).
RR for contrast of women exposed to housing policy change compared with those unexposed. Exposure is defined as maternal residence in an Atlanta Housing Authority (AHA) public housing project within 12 months preceding demolition, followed by subsequent birth in private housing or different AHA public housing. The referent unexposed group is women with 2 consecutive births in the same AHA public housing project.
Adjusted for maternal age and age-squared at first measured birth, housing at first measured birth, and current maternal age, age-squared, parity, smoking, education, history of preterm or SGA birth, interpregnancy interval, adequacy of prenatal care, Medicaid status, year of birth, and indicator for whether mother moved to a different tract since last birth.
Area variables include percentage of households below federal poverty level in the census tract and percentage of Black in census tract.
Marginal structural models adjusted for time-varying confounding by the same covariates included in the traditional regression models via inverse-probability of treatment weighting.
DISCUSSION
The growing recognition of the importance of structural and social determinants of population health and the role of residential place (the social and built environments) as a mechanism for differential distribution of health-related exposures suggests that greater attention needs to be paid to residential mobility and housing policy as health determinants.8 Modification of public housing policies are among the few population-based interventions available to effect neighborhood change.31 We made novel use of maternally linked vital records combined with a dramatic change in public housing policy in the city of Atlanta to test longitudinal hypotheses about the effects of mobility and housing policy on pregnancy outcomes among low-income Black women. Perhaps not surprisingly, the answers to the questions posed in this study were neither simple nor decidedly fixed because of the complex pathways by which mobility might influence perinatal health.
Preterm birth and fetal growth restriction result in substantial morbidity, mortality, and economic burdens that are disproportionately experienced by poor and African American families.11,21,32 The apparent sensitivity of pregnancy outcomes to contextual, lifecourse, and even intergenerational exposures make study of these outcomes an important model for better understanding the processes by which social experience is internalized.11,33 For example, women’s experience of chronic stress in the form of poverty, perceived discrimination, or neighborhood disorder have been associated with preterm birth and important risk factors for preterm birth, such as bacterial vaginosis.34 By contrast, the strongest predictors of fetal growth restriction are maternal smoking, pregnancy-induced hypertension, and maternal low body mass index, all factors that may be amenable to intervention in the course of prenatal care.21,35 Thus, although the 2 pregnancy outcomes have overlapping risk profiles, differences between them may be instructive.
We found no significant association of either preterm birth or small for gestational age birth with a routine (e.g., not policy-induced) transition from public to private housing compared with 2 births in public housing. However, for women who once lived in public housing but moved out, the second birth of 2 subsequent consecutive births in private-market housing was associated with increased risk for preterm LBW, but had a modestly reduced (albeit nonsignificantly) risk for small for gestational age LBW. The lower RR for small for gestational age LBW for private-private transition patterns could suggest that moving out and staying out of the projects might be associated with reduction of risk factors for fetal growth restriction, possibly through behavioral change or access to prenatal care. By contrast, for preterm birth, women with private-private patterns might experience increased risk related to loss of social support and increased stress associated with departure from public housing. The differences by housing transition pattern and by pregnancy outcome could be because of unmeasured differences among women. However, they could also reflect differences in how housing and neighborhoods influence behavior and health, and differences in the timing and chronicity of relevant exposures. For example, preconceptional exposures including social support and chronic stress might be particularly important for preterm birth.34
Different associations by pregnancy outcome persist comparing women exposed with those unexposed to the change in housing policy. For preterm LBW, but not small for gestational age preterm birth, there was a suggestion of elevated risk for women whose public housing project closed in the period between 2 births. It might be that these women were less equipped to enter the private housing market at the time of the move—even with the support of vouchers—and thus experienced greater stress, had lower social support, or were less able to access primary and prenatal medical care.
Limitations
It is also possible that the observed differences for both analyses resulted from residual confounding by unmeasured variables. Marginal structural models address time-varying confounding, which is a plausible source of bias in many social epidemiology settings in which past exposures and covariates may both mediate and confound current exposure-outcome associations. However, these models still rely on an assumption of no unmeasured confounding. It was possible, for instance, that an important risk factor differed by housing transition pattern and was not fully accounted for in our variables. For example, a woman with a criminal record for drug use might have increased risk of poor pregnancy outcomes because of ongoing drug use, and her criminal record might also limit her housing options. Other potential unmeasured factors included the reason for non–policy-induced moves (e.g., women could move because of improved economic conditions or be evicted for criminal behavior), and the effect of housing and neighborhood on fertility patterns. Although such information was not available, the restriction to a cohort of women with at least 1 birth in AHA public housing made a more homogenous sample than if other nonpublic housing recipients were included.
This study attempted to document differences in perinatal risk for women during a period of public housing change, but it was possible that this follow-up period was not adequate to fully account for the effects of housing policy. AHA projects began closing in the late 1990s, but demolition of old projects was not complete until 2010, 3 years after the end of our follow-up data. Therefore, the number of potential affected births was not fully described, and the length of time since exposure might be too short. If transition to the private housing market was initially associated with increased risk of preterm birth, it could not be determined whether these effects would persist through time, when the potentially positive impact of lower neighborhood poverty might have a larger role.
Additionally, because housing status was only measured at the time of a birth, there was imperfect measurement of the duration of exposure to any particular housing, limiting inference about the role of length of stay and outcomes. The low number of former public housing residents who moved into the new mixed-income developments means that we were unable to evaluate transition patterns including these housing units. Further follow-up and analysis to better evaluate the impact of the mixed-income developments is needed. There was also possible misclassification of housing status because of errors in geocoding and spatial linkage (Appendix B, available as a supplement to the online version of this article at http://www.ajph.org).
Finally, our internal validation of the deterministic linkage algorithm suggested high probability that the linked sets of births were true sets; however, it was also likely that additional births were incorrectly unlinked and thus did not count toward the follow-up. The primary reason for nonlinkage would be if a mother changed her surname during follow-up. However, the risk for each outcome appeared to be similar in the matched and unmatched births.
Conclusions
In summary, we found modest evidence that closure of Atlanta public housing projects was associated with increased risk of preterm LBW for women who plausibly moved as a result of project demolition. However, among women who ever lived in public housing projects, housing transitions conferred different risk depending on the pregnancy outcome of interest and the woman’s residential pattern. These findings must be interpreted with caution but demand further attention to the health impact of housing policy. Understanding residential mobility and housing policy as a means of addressing structural discrimination in the form of poverty concentration and residential segregation could lead to better interventions to reduce health disparities.
Acknowledgments
This study was supported by the Maternal and Child Health Bureau (Title V, Social Security Act), Health Resources and Services Administration, Department of Health and Human Services (grant R40 MC 17180).
The authors acknowledge Gordon Freymann of the Georgia Office of Health Indicators for Planning for providing the maternally linked data set, and Michael Rich and Moshe Haspel of the Political Science Department of Emory University for assistance in identifying the location of distressed Atlanta public housing projects. Finally, they thank Hannah Cooper of Emory University and Deirdre Oakley of Georgia State University for comments on an early draft of the article.
Human Participant Protection
This study was reviewed and approved by the institutional review board for Emory University.
References
- 1.Lapping MB. Emergence of federal public housing: Atlanta’s Techwood Project. Am J Econ Sociol. 1973;32(4):379–386 [Google Scholar]
- 2.Tegeler PD. The persistence of segregation in government housing programs. : Briggs XS, The Geography of Opportunity: Race and Housing Choice in Metropolitan America. Washington, DC: Brookings Institution Press; 2005:197–216 [Google Scholar]
- 3.Turner MA, Popkin SJ, Rawlings L. Public Housing and the Legacy of Segregation. Washington, DC: The Urban Institute Press; 2009 [Google Scholar]
- 4.Oakley D, Ruel E, Wilson GE. A choice with no options: Atlanta Public Housing residents’ lived experiences in the face of relocation. Available at: http://www2.gsu.edu/∼wwwsoc/Files/SOC/RESEARCH_public_housing_report.pdf. Accessed February 27, 2011.
- 5.Glover RL. The Atlanta blueprint: transforming public housing citywide. : Cisneros H, Engdahl L, From Despair to Hope: HOPE VI and the New Promise of Public Housing in America’s Cities. Washington, DC: Brookings Institution Press; 2009:145–167 [Google Scholar]
- 6.Kaufman JS, Dole N, Savitz DA, Herring AH. Modeling community-level effects on preterm birth. Ann Epidemiol. 2003;13(5):377–384 [DOI] [PubMed] [Google Scholar]
- 7.Pickett KE, Pearl MC. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55(2):111–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Acevedo-Garcia D, Osypuk TL, Werbel RE, Meara ER, Cutler DM, Berkman LF. Does housing mobility policy improve health? Housing Policy Debate. 2004;15(1):49–98 [Google Scholar]
- 9.Fauth RC, Leventhal T, Brooks-Gunn J. Seven years later: effects of a neighborhood mobility program on poor Black and Latino adults’ well-being. J Health Soc Behav. 2008;49(2):119–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ludwig J, Sanbonmatsu L, Gennetian Let al. Neighborhoods, obesity, and diabetes–a randomized social experiment. N Engl J Med. 2011;365(16):1509–1519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kramer MR, Hogue CR. What causes racial disparities in very preterm birth? A biosocial perspective. Epidemiol Rev. 2009;31:84–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geronimus AT. Black/white differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Soc Sci Med. 1996;42(4):589–597 [DOI] [PubMed] [Google Scholar]
- 13.Collins JW, Jr, David RJ. Urban violence and African-American pregnancy outcome: an ecologic study. Ethn Dis. 1997;7(3):184–190 [PubMed] [Google Scholar]
- 14.Messer LC, Kaufman JS, Dole N, Savitz DA, Laraia BA. Neighborhood crime, deprivation, and preterm birth. Ann Epidemiol. 2006;16(6):455–462 [DOI] [PubMed] [Google Scholar]
- 15.O’Campo P, Burke JG, Culhane Jet al. Neighborhood deprivation and preterm birth among Non-Hispanic Black and White women in eight geographic areas in the United States. Am J Epidemiol. 2008;167(2):155–163 [DOI] [PubMed] [Google Scholar]
- 16.Huynh M, Parker JD, Harper S, Pamuk E, Schoendorf KC. Contextual effect of income inequality on birth outcomes. Int J Epidemiol. 2005;34(4):888–895 [DOI] [PubMed] [Google Scholar]
- 17.Kramer MR, Cooper HL, Drews-Botsch CD, Waller LA, Hogue CR. Metropolitan isolation segregation and Black-White disparities in very preterm birth: a test of mediating pathways and variance explained. Soc Sci Med. 2010;71(12):2108–2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grady SC. Racial disparities in low birthweight and the contribution of residential segregation: a multilevel analysis. Soc Sci Med. 2006;63(12):3013–3029 [DOI] [PubMed] [Google Scholar]
- 19.Manjarrez CA, Popkin SJ, Guernsey E. Poor Health: Adding Insult to Injury for HOPE VI Families. Report No. 5 Washington, DC: Urban Institute; 2007 [Google Scholar]
- 20.Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kramer MS, Seguin L, Lydon J, Goulet L. Socio-economic disparities in pregnancy outcome: why do the poor fare so poorly? Paediatr Perinat Epidemiol. 2000;14(3):194–210 [DOI] [PubMed] [Google Scholar]
- 22.Strickland MJ, Siffel C, Gardner BR, Berzen AK, Correa A. Quantifying geocode location error using GIS methods. Environ Health. 2007;6:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oakley D, Ruel E, Reid L. Moved out to where? Initial relocation destinations of former public housing residents in Atlanta: A preliminary brief. Available at: http://www2.gsu.edu/∼wwwsoc/Files/SOC/RESEARCH_public_housing_initial_report.pdf. Accessed February 27, 2011.
- 24.Ananth CV. Menstrual versus clinical estimate of gestational age dating in the United States: temporal trends and variability in indices of perinatal outcomes. Paediatr Perinat Epidemiol. 2007;21(suppl 2):22–30 [DOI] [PubMed] [Google Scholar]
- 25.Kotelchuck M. The adequacy of prenatal care utilization index: its US distribution and association with low birthweight. Am J Public Health. 1994;84(9):1486–1489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–560 [DOI] [PubMed] [Google Scholar]
- 27.Hernán MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11(5):561–570 [DOI] [PubMed] [Google Scholar]
- 28.Bodnar LM, Davidian M, Siega-Riz AM, Tsiatis AA. Marginal structural models for analyzing causal effects of time-dependent treatments: an application in perinatal epidemiology. Am J Epidemiol. 2004;159(10):926–934 [DOI] [PubMed] [Google Scholar]
- 29.Cerdá M, Diez-Roux AV, Tchetgen ET, Gordon-Larsen P, Kiefe C. The relationship between neighborhood poverty and alcohol use: estimation by marginal structural models. Epidemiology. 2010;21(4):482–489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200 [DOI] [PubMed] [Google Scholar]
- 31.Dunn JR, Hayes MV, Hulchanski JD, Hwang SW, Potvin L. Housing as a socio-economic determinant of health: findings of a national needs, gaps and opportunities assessment. Can J Public Health. 2006;97:S11–S15 [PubMed] [Google Scholar]
- 32.Behrman RE, Butler AS, Preterm Birth: Causes, Consequences, and Prevention. Washington, DC: National Academy Press, Institute of Medicine; 2007 [PubMed] [Google Scholar]
- 33.Collins JW, Jr, Rankin KM, David RJ. African American women’s lifetime upward economic mobility and preterm birth: the effect of fetal programming. Am J Public Health. 2011;101(4):714–719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kramer MR, Hogue CR, Dunlop AL, Menon R. Preconceptional stress and racial disparities in preterm birth: sn overview. Acta Obstet Gynecol Scand. 2011;90(12):1307–1316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alexander GR, Korenbrot CC. The role of prenatal care in preventing low birth weight. Future Child. 1995;5(1):103–120 [PubMed] [Google Scholar]