Abstract
Objectives. We assessed shifts in patterns of mortality during a hot weather event in greater Vancouver, British Columbia.
Methods. We used a case-only analysis to compare characteristics of individuals who died during the hottest week of 2009 with those who died (1) during earlier summer weeks in 2009 and (2) during the same calendar weeks in the summers of 2001 through 2008.
Results. Compared with the 8 previous weeks of 2009, odds of mortality during the summer’s hottest week were highest in the 65 to 74 years age category, compared with the 85 years and older category (odds ratio [OR] = 1.47; 95% confidence interval [CI] = 1.06, 2.03). The number of deaths at home increased over deaths in hospitals or institutions (OR = 1.43; 95% CI = 1.10, 1.86). Densely populated administrative health areas were more affected.
Conclusions. A shift toward deaths at home suggests that in-home–based protective measures should be part of planning for hot weather events in greater Vancouver. Targeting should be considered for those aged 65 to 74 years. The case-only approach is quick and easy to apply and can provide useful information about localized, time-limited events.
Climate change has heightened public health interest in the epidemiology of death associated with very high temperatures. Although recent heat waves affecting Chicago, Illinois,1,2 and Paris, France,3,4 have been studied, other hot weather events have passed largely unreported.5,6 In this article, we show that rapid assessment of impacts and risk factors can be facilitated by methods that use easily accessed administrative health data to compare groups of decedents.
Case-only analyses were originally used to study gene–environment interactions7,8 but have recently been applied to assess the effects of weather and air pollution on mortality.9 Case-only analyses have been used to examine sensitivity to extreme temperatures across multiple cities over lengthy study periods10,11 but have not been applied to specific hot weather events in defined geographic regions. Benefits of the case-only design include simplification of data analysis and reduction in model complexity.9
During summer 2009, Vancouver, British Columbia, and its surrounding suburban and semirural areas (i.e., greater Vancouver) experienced an atypically hot weather event. The maximum (and minimum) temperatures at Vancouver International Airport were 30.9°C (19.6°C) on July 28, 34.0°C (20.2°C) on July 29, and 34.4°C (22.4°C) on July 30, all under clear skies with an average relative humidity of 57%. By comparison, the 10-year (1999–2008) average of maximum (and minimum) daily temperature for July 28 to 30 was 21.9°C (14.1°C), with an average relative humidity of 68%. Within days of the onset of the hot weather event, British Columbia’s rapid mortality surveillance system indicated that deaths among residents of greater Vancouver had increased by around 40% for the period through August 2. The objective of this case-only analysis was to examine whether patterns of mortality in greater Vancouver shifted during this hot weather event by comparing characteristics of the individuals who died during the hottest calendar week with those of the individuals who died during 3 comparison periods.
METHODS
Complete nonnominal mortality records were obtained from the British Columbia Vital Statistics Agency for the summers of 2001 though 2009. These records included all deaths occurring in the greater Vancouver area. From each mortality record, we extracted
date of death,
underlying cause of death,
age,
sex,
place of death (at home, in a hospital, in a residential institution, or in another location), and
administrative health area (AHA) of residence (an indicator of geographic location).
Place of death was available only for 2008 and 2009. Cause of death was coded according to the International Classification of Diseases, 10th Revision.
The daily mean, maximum, and minimum temperatures measured at Vancouver International Airport were downloaded for the same period from the Environment Canada archives. The hottest calendar week of summer 2009 (referred to hereinafter as the hot weather event) was identified as July 27 through August 2 by calculating 7-day running averages of the maximum temperature measurements. Averages of the mean and minimum temperatures likewise identified the same week. We selected a 1-week period to avoid biasing the results with the day-of-the-week effect.12 Three comparison periods were chosen: (1) the 8 weeks before the hot weather event in 2009, (2) the same calendar weeks as the hot weather event for the summers of 2001 through 2008, and (3) the same calendar weeks as the hot weather event for the summers of 2005 through 2008, a period closer in time to the 2009 hot weather event although with half as many comparison days. Daily 24-hour concentrations of ozone and particulate matter less than 2.5 microns in aerodynamic diameter were downloaded from the British Columbia Ministry of Environment archives for the summers of 2001 though 2009.
We assessed patterns of mortality during the hot weather event using logistic regression, as described in the literature on case-only analyses.9,11 In brief, the characteristic of interest was set as the response variable and the hot weather event was treated as a predictive covariate, with a value of 1 for death during the event and 0 for death during the comparison period (Equation 1). The characteristics we considered were
age category (< 65, 65–74, and 75–84 years compared with ≥85 years),
sex (male compared with female),
death at home (compared with death at another location),
AHA with a population density of more than 1000 people per square kilometer (compared with ≤ 1000 people/km2),
AHA with more than 40% of people older than 65 years living alone (compared with AHA with ≤ 40%), and
AHA with more than 20% of residents below the low-income cutoff (compared with AHA with ≤ 20%).
The cutpoints for characteristics 4, 5, and 6 were chosen at natural breaks in the spatial distributions.13 We adjusted regression coefficients for age and sex when appropriate. All statistical analyses were done in R (R Foundation for Statistical Computing, Vienna, Austria).
 |
To further investigate changes in spatial patterns of mortality, we mapped by AHA the difference in mortality rates between the hot weather event and the 8 weeks before the hot weather event.
RESULTS
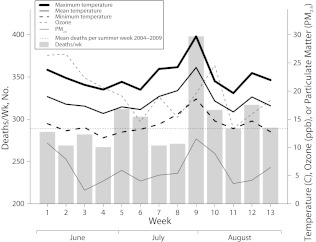
There were 398 nonaccidental deaths during the hot weather event (July 27–August 2, 2009), compared with an average of 290 (±41.9) deaths for all summer weeks in 2001 though 2009 (Figure 1). Causes of death are reported in Table 1. Although numbers were small, the proportion of deaths with heat-specific International Classification of Diseases, 10th Revision, codes as the primary cause was higher during the hot weather event than during the comparison periods (Fisher exact P < .05). The proportion of deaths resulting from respiratory causes was also higher during the hot weather event than during the 2009 and the 2001 through 2008 comparison periods (Fisher exact P = .36 and .09, respectively).
FIGURE 1—
Weekly (Sunday through Saturday) mortality compared with temperatures, ozone, and particulate matter measured at Vancouver International Airport: greater Vancouver, BC; summer 2009.
Note. ppb = parts per billion; PM2.5 = particulate matter < 2.5 μ in aerodynamic diameter.
TABLE 1—
Distribution of Deaths by Primary Cause for the Hot Weather Event and the 3 Comparison Periods: Vancouver, BC; Summer 2009, Summers 2001–2008, and Summers 2005–2008
| Cause of Deatha | 2009 Hot Weather Event | 8 Previous Weeks, Summer 2009 | 8 Same Weeks, Summers 2001–2008 | 4 Same Weeks, Summers 2005–2008 |
| All nonaccidental, No. | 398 | 2258 | 2582 | 1070 |
| Heat (×30), % | 1.00 | 0.04 | 0.15 | 0 |
| Respiratory (J00—J99), % | 13.1 | 11.2 | 9.9 | 9.6 |
| Cardiovascular (I00—I99), % | 27.9 | 29.4 | 32.0 | 32.0 |
Primary cause of death was determined using International Classification of Diseases, 10th Revision.
Regression results are reported in Table 2. Compared with the 8 previous weeks, risk of mortality during the hot weather event was highest in the 65 to 74 years age category compared with the 85 years and older category (odds ratio [OR] = 1.47; 95% confidence interval [CI] = 1.06, 2.03) and higher in the younger than 65 years category (OR = 1.10; 95% CI = 0.82, 1.49). Men were at higher risk than were women (OR = 1.12; 95% CI = 0.90, 1.39). The number of deaths outside of institutions (i.e., at home or another location) was higher than that of deaths in hospitals or other care facilities (OR = 1.43; 95% CI = 1.10, 1.86). When we compared the 2009 hot weather event with the same calendar weeks of the previous 8 summers (2001–2008), the age effects disappeared. However, comparison with the same calendar weeks of the previous 4 summers (2005–2008) once again showed that the highest risk was in the 65 to 74 years age category (OR = 1.35; 95% CI = 0.94, 1.93). Adjustment for daily concentrations of ozone and particulate matter had minimal effect on the regression results (not shown).
TABLE 2—
Logistic Regression Results for the Case-Only Models: Vancouver, BC; Summer 2009, Summers 2001–2008, and Summers 2005–2008
| Characteristic | Comparison Group | 8 Previous Weeks, Summer 2009, OR (95% CI) | 8 Same Weeks, Summers 2001–2008, OR (95% CI) | 4 Same Weeks, Summers 2005–2008, OR (95% CI) |
| Age, y | ||||
| < 65 | ≥ 85 | 1.10 (0.82, 1.49) | 0.95 (0.70, 1.29) | 0.99 (0.71, 1.38) |
| 65–74 | ≥ 85 | 1.47* (1.06, 2.03) | 1.03 (0.75, 1.42) | 1.35 (0.94, 1.93) |
| 75–84 | ≥ 85 | 1.02 (0.76, 1.36) | 0.88 (0.66, 1.17) | 0.97 (0.71, 1.32) |
| Male | Female | 1.12 (0.90, 1.39) | 1.09 (0.88, 1.36) | 1.08 (0.85, 1.37) |
| Died outside institutiona | Died in institution | 1.43* (1.10, 1.86) | 1.42 (0.94, 2.14)b | 1.42 (0.94, 2.14)b |
| > 1000 people/km2 | ≤ 1000 people/km2 | 1.26* (1.02, 1.58) | 1.32* (1.06, 1.65) | 1.43* (1.13, 1.82) |
| > 40% of people aged ≥ 65 y living alone | ≤ 40% of people aged ≥ 65 y living alone | 1.23 (0.88, 1.72) | 1.07 (0.77, 1.49) | 1.12 (0.78, 1.61) |
| > 20% under LICOc | ≤ 20% under LICO | 1.17 (0.94, 1.45) | 1.23* (1.00, 1.52) | 1.34* (1.07, 1.70) |
Note. CI = confidence interval; LICO = low-income cutoff; OR = odds ratio. All models adjusted for age and sex when appropriate.
Institutions include hospitals and care residences.
Data available for 2008 only.
The before-tax low income cut-off as defined by Statistics Canada.14
*α = 0.05.
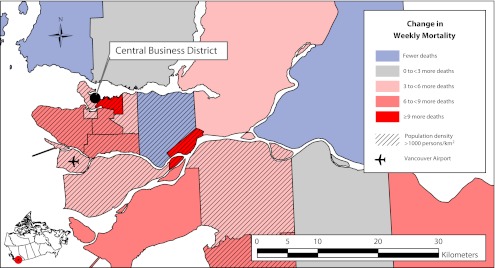
Differences in mortality rates during the hot weather event compared with the previous summer weeks varied considerably across AHAs (Figure 2). When we used a case-only analysis to compare the 11 administrative areas with a population density of more than 1000 people per square kilometer with the 10 less densely populated areas, the resulting OR was 1.26 (95% CI = 1.02, 1.58) for the 2009 comparison period. We found smaller differences when administrative areas were dichotomized on the basis of the population percentage below Canada’s low-income cutoff, or the percentage of persons aged 65 years or older living alone (Table 2).
FIGURE 2—
Change in the mortality rate (number of deaths/100 000 person weeks) between the hot weather event and previous summer weeks: Vancouver, BC; 2009.
Note. Black borders indicate the administrative health areas in greater Vancouver.
Source. Map from the British Columbia Ministry of Health and population data from the Census of Canada.
DISCUSSION
Although conditions during the 2009 hot weather event were unusual for greater Vancouver, temperatures were far lower than the thresholds at which mortality has been shown to increase in southern cities or in those with more continental climates.15,16 Although absolute numbers were small, descriptive summaries showed an increase in deaths with International Classification of Diseases, 10th Revision, codes specific to heat during the hot weather event compared with the earlier summer weeks in 2009 and the same calendar weeks in 2001 through 2008. The number of respiratory deaths also increased, which is consistent with reports of heat events in Europe,17,18 Asia,19 and North America.20
Hot weather events elsewhere have been investigated using episode analysis, in which during-event deaths are compared with historic rates and rate ratios are calculated over demographic or geographic strata.21 This alternative case-only design assumes constancy of denominators and allows the effect of multiple risk factors to be assessed simultaneously. It is easy and quick, and its results can inform the elaboration of hypotheses for case-control studies based on the same case series. The application of alternate previous-year comparisons demonstrates that caution needs be applied in selecting comparison periods. In our analyses, the increased odds of dying among people aged 65 to 74 years relative to the oldest age stratum disappeared when we used a comparison period of 2001 through 2008 but were apparent when the period was limited to 2005 through 2008. In Vancouver, the proportion of senior citizens older than 85 years rose from 11.5% to 14.0% between 2001 and 2009, thus increasing the number of expected deaths in the reference group and thereby lessening odds ratios when the 2009 heat episode was compared with much earlier periods. In fact, the odds ratio increased for every year that was removed from the comparison (not shown).
Case-only analyses showed an increase in deaths at home during the hot weather event, possibly reflecting the rapid demise associated with exposure to extreme heat.22,23 A similar increase occurred during the 2003 Paris heat wave, for which risk factors for at-home death included living alone, chronic diseases, lack of mobility, sleeping on the top floor, limited thermal insulation, and higher temperatures around the decedent’s residence. Using residential cooling was found to be protective.24,25 These factors may partially explain our observation that those living in more densely populated and less advantaged AHAs were more likely to die during the greater Vancouver hot weather event. Excess mortality in cities compared with rural areas affected by regional heat events has been reported elsewhere,26 as has a mortality shift toward a densely populated urban core27 or to peripheral areas of social and economic disadvantage.23
Advanced age has been identified as a major risk factor for mortality during hot weather events.21 However, we found that mortality risk was higher for the 65 to 74 years age group compared with the 85 years and older age group. During the 1995 Chicago heat wave, the highest relative risk of death was found for people aged 55 to 64 years and those aged 85 years and older.2 Relative mortality was highest among people aged 85 years and older in the 2003 French heat event.3 We have no comparative demographic or case-specific measures to suggest why people aged 65 to 74 years were relatively more affected than older cohorts in Vancouver.
Case-only methods allow public health questions to be addressed with speed and ease but are limited by the restriction that all study participants experienced the same outcome (death, in this case), with their selection into the case or comparison group being made by some other characteristic (time period of death, in this case). As such, the results presented here cannot provide conclusive evidence about risk factors for death itself, only about risk factors for death during the hot weather period as opposed to death during other periods. Alternate, more intensive studies using case-control or cohort designs would be needed to assess individual risk factors for increased mortality during hot weather events.
Because climate, weather, urban structure, and demography differ between cities and because cities change over time, the assessment of recent heat episodes in specific locales informs public health agencies about how best to prepare for future events. The results of the current work have been valuable in allocating resources and targeting public health messaging to vulnerable groups for future hot weather events in greater Vancouver.
Acknowledgments
We thank the British Columbia Vital Statistics Agency for making surveillance data available to the British Columbia Centre for Disease Control.
This article was previously presented at the 20th Annual John K. Friesen Conference; May 25–26, 2011; Vancouver, British Columbia.
Human Participant Protection
No approval was required for this study, which was conducted as part of routine environmental health surveillance at the British Columbia Centre for Disease Control.
References
- 1.Semenza JC, Rubin CH, Falter KHet al. Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med. 1996;335(2):84–90 [DOI] [PubMed] [Google Scholar]
- 2.Whitman S, Good G, Donoghue E, Benbow N, Shou W, Mou S. Mortality in Chicago attributed to the July 1995 heat wave. Am J Public Health. 1997;87(9):1515–1518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fouillet A, Rey G, Laurent Fet al. Excess mortality related to the August 2003 heat wave in France. Int Arch Occup Environ Health. 2006;80(1):16–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vandentorren S, Suzan F, Medina Set al. Mortality in 13 French cities during the August 2003 heat wave. Am J Public Health. 2004;94(9):1518–1520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kosatsky T, Henry B, King N. How Montreal and Toronto (Canada) deal with summertime heat. : Kirch W, Menne B, Bertollini R, Extreme Weather Events and Public Health Responses. Berlin: Springer; 2005:167–171 [Google Scholar]
- 6.Rey G, Jougla E, Fouillet Aet al. The impact of major heat waves on all-cause and cause-specific mortality in France from 1971 to 2003. Int Arch Occup Environ Health. 2007;80(7):615–626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khoury MJ, Flanders WD. Nontraditional epidemiologic approaches in the analysis of gene-environment interaction: case-control studies with no controls! Am J Epidemiol. 1996;144(3):207–213 [DOI] [PubMed] [Google Scholar]
- 8.Piegorsch WW, Weinberg CR, Taylor JA. Non-hierarchical logistic models and case-only designs for assessing susceptibility in population-based case-control studies. Stat Med. 1994;13(2):153–162 [DOI] [PubMed] [Google Scholar]
- 9.Armstrong BG. Fixed factors that modify the effects of time-varying factors: applying the case-only approach. Epidemiology. 2003;14(4):467–472 [DOI] [PubMed] [Google Scholar]
- 10.Medina-Ramón M, Zanobetti A, Cavanagh DP, Schwartz J. Extreme temperatures and mortality: assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ Health Perspect. 2006;114(9):1331–1336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schwartz J. Who is sensitive to extremes of temperature?: a case-only analysis. Epidemiology. 2005;16(1):67–72 [DOI] [PubMed] [Google Scholar]
- 12.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345(9):663–668 [DOI] [PubMed] [Google Scholar]
- 13.Jenks GF. The data model concept in statistical mapping. International Yearbook of Cartography. 1967;7:186–190 [Google Scholar]
- 14.Statistics Canada definition of the low income cut-off (before tax) Available at: http://www12.statcan.ca/census-recensement/2006/ref/dict/fam020-eng.cfm. Accessed December 2, 2010.
- 15.Baccini M, Biggeri A, Accetta Get al. Heat effects on mortality in 15 European cities. Epidemiology. 2008;19(5):711–719 [DOI] [PubMed] [Google Scholar]
- 16.Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155:80–87 [DOI] [PubMed] [Google Scholar]
- 17.D’Ippoliti D, Michelozzi P, Marino Cet al. The impact of heat waves on mortality in 9 European cities: results from the EuroHEAT project. Environ Health. 2010;9:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huynen MM, Martens P, Schram D, Weijenberg MP, Kunst AE. The impact of heat waves and cold spells on mortality rates in the Dutch population. Environ Health Perspect. 2001;109(5):463–470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang W, Kan H, Kovats S. The impact of the 2003 heat wave on mortality in Shanghai, China. Sci Total Environ. 2010;408(11):2418–2420 [DOI] [PubMed] [Google Scholar]
- 20.Braga AL, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect. 2002;110(9):859–863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kovats RS, Hajat S. Heat stress and public health: a critical review. Annu Rev Public Health. 2008;29:41–55 [DOI] [PubMed] [Google Scholar]
- 22.Bouchama A, Knochel J. Heat stroke. N Engl J Med. 2002;346(25):1978–1988 [DOI] [PubMed] [Google Scholar]
- 23.Jones T, Liang A, Kilbourne Eet al. Morbidity and mortality associated with the July 1980 heat wave in St Louis and Kansas City, Mo. JAMA. 1982;247(24):3327–3331 [PubMed] [Google Scholar]
- 24.Canouï-Poitrine F, Cadot E, Spira A. Excess deaths during the August 2003 heat wave in Paris, France. Rev Epidemiol Sante Publique. 2006;54(2):127–135 [DOI] [PubMed] [Google Scholar]
- 25.Vandentorren S, Bretin P, Zeghnoun Aet al. August 2003 heat wave in France: risk factors for death of elderly people living at home. Eur J Public Health. 2006;16(6):583–591 [DOI] [PubMed] [Google Scholar]
- 26.Ramlow JM, Kuller LH. Effects of the summer heat wave of 1988 on daily mortality in Allegheny County, PA. Public Health Rep. 1990;105(3):283–289 [PMC free article] [PubMed] [Google Scholar]
- 27.Henschel A, Burton L, Margolies L, Smith J. An analysis of the heat deaths in St. Louis during July, 1966. Am J Public Health Nations Health. 1969;59(12):2232–2242 [DOI] [PMC free article] [PubMed] [Google Scholar]