Abstract
Objectives. We evaluated the impact of a diagnosis of serious mental illness on use of a primary care provider (vs the emergency department [ED]) as a source of care by people who were chronically homeless.
Methods. We used data from 750 chronically homeless adults enrolled in the 11-site Collaborative Initiative to Help End Chronic Homelessness and identified demographic and clinical characteristics independently associated with using a primary care provider rather than an ED.
Results. The factor most strongly associated with using the ED as a regular source of medical care was previous-year lack of health insurance. Despite high rates of serious mental illness, neither a diagnosis of serious mental illness nor increased severity of psychiatric symptoms was associated with such use.
Conclusions. Findings suggest that people who are chronically homeless and have chronic medical illness would be more likely to access care if they had health insurance. Individual states’ deciding not to expand Medicaid coverage will likely have a tremendous impact on the health outcomes and health care costs associated with this and other vulnerable populations.
On a typical night in 2010, approximately 650 000 people were homeless in the United States.1 Although most people are homeless for only a brief period of time, an estimated 10% have experienced chronic homelessness, defined as continuous homelessness for 1 year or more or at least 4 episodes of homelessness in the past 3 years.1 Most people experiencing chronic homelessness have chronic health problems and typically have multiple co-occurring conditions.2 Chronic homelessness has been associated with an increased risk of mortality, with reports of age-adjusted death rates of 2 to 4 times that of the general population3 and even higher mortality rates from trauma and suicide.4 Specific chronic medical conditions (HIV, liver disease, and arrhythmia) have been associated with the greatest risk of death.5
For many chronically homeless individuals, competing demands for shelter, food, and safety supersede the subjective need for primary medical care.6 This issue is of critical importance, given recent evidence that improved access to primary care reduces mortality7 and that individuals without a primary care provider (PCP) are less likely to receive recommended preventive care8 and more likely to have poor health outcomes, such as diabetic ketoacidosis9 or severe uncontrolled hypertension.10 Homeless people are less likely than domiciled individuals to use ambulatory care services,11 relying to a greater extent on emergency department (ED) visits and costly inpatient hospitalizations.12 The cost of inpatient services for people who are homeless may substantially affect the health care system because almost one quarter of homeless people in the United States report a hospitalization within the previous year.13 Homeless patients on medical and surgical services remain hospitalized longer than housed patients, resulting in substantial excess costs.14
Homeless individuals are 3 times more likely to use the ED than are nonhomeless people.15 A recent large national study of ED use demonstrated that homeless people who seek care in urban EDs come by ambulance, are more likely to lack medical insurance, and have psychiatric and substance use diagnoses than are people who are not homeless.16 Homeless individuals also appear to use the ED for routine, nonemergency medical needs,16,17 often for preventable medical problems.18
Previous research has attempted to determine rates and predictors of medical service use among homeless samples.11,19–22 The behavioral model for vulnerable populations is a conceptual model for health service use and medical outcomes of people such as those who are chronically homeless.23 This model predicts the use of health services on the basis of predisposing, enabling, and need factors and identifies the particular challenges vulnerable groups face in obtaining necessary services. This model has been applied to homeless populations, and findings from these studies have suggested that among homeless individuals, drug use increases the risk of medical hospitalization, and psychological distress (self-report of mood over the past 4 weeks) is associated with barriers to obtaining outpatient medical care.24
The impact of serious psychiatric illness and psychiatric symptom severity on engagement in primary care has not previously been specifically evaluated among chronically homeless individuals. Serious mental illness (schizophrenia or bipolar disorder) may be a more important determinant of underuse of PCPs among homeless people than are logistical barriers such as lack of insurance. Compared with the general population, people who are homeless have substantially higher rates of psychiatric and substance use disorders.25,26 Evidence has also shown that individuals with serious mental illness underuse primary care even after accounting for their medical need27 and that severity of psychiatric illness might increase the risk of frequent ED use.28 In the current study, we identified factors associated with having a regular PCP, as contrasted with relying on ED services as a usual source of care, in a national sample of chronically homeless individuals. In particular, we evaluated the impact of a diagnosis of serious mental illness and psychiatric symptom severity on having a regular source of care.
METHODS
We used data from the Collaborative Initiative to Help End Chronic Homelessness (CICH). The US Interagency Council on Homelessness implemented CICH in 2004 to provide as many as 5 years of funding from the US Departments of Housing and Urban Development, Health and Human Services, and Veterans Affairs to 11 sites to provide chronically homeless adults with permanent housing and primary health care and mental health services. Criteria for eligibility as chronically homeless were defined as “continuously homeless for one year or more or at least four episodes of homelessness in the past three years.”1(p3) The 11 communities funded through CICH included Chattanooga, TN; Chicago, IL; Columbus, OH; Denver, CO; Fort Lauderdale, FL; Los Angeles, CA; Martinez, CA; New York City, NY; Philadelphia, PA; Portland, OR; and San Francisco, CA. Each site developed a comprehensive plan to reduce the prevalence of chronic homelessness in their community through the development of sustainable, cost-effective partnerships among providers in the public and private sector. The specifics of these plans varied across communities, but each plan included strategies for providing permanent housing and provision of comprehensive primary health, mental health, and substance abuse treatment services linked to housing.29
Data Collection and Measures
After participants gave informed consent, CICH staff conducted assessments at each site through face-to-face interviews and self-report measures. Eight hundred seventy participants completed the baseline interview. Baseline data were collected between February 2004 and April 2006. All procedures were approved by the institutional review boards at the parent site and at each participating site.
Usual source of medical care.
Our indicator of participants’ usual source of medical care was determined by responses to 2 questions. Participants were asked, “Is there one health care provider or place that you usually go when you are sick or in need of advice about your health?” Participants who responded affirmatively were asked, “Where do you usually go when you are sick or need advice about your health?” Response categories were
ED,
a clinic or office in a hospital,
health clinic in the community,
a doctor’s office,
a mobile health clinic, and
other.
For the purposes of our analyses, we dichotomized responses into “ED” and “primary care” (categories 2–5). Responses of “other” were coded as missing.
Sociodemographic characteristics.
The interview conducted at the time of program entry included demographic information, specific questions about experiences of homelessness (age when first homeless, lifetime number of years of homelessness, number of days homeless in past 90 days), and questions about past incarceration and institutionalization. Staff asked participants how many days during the past 3 months they were housed in each of 9 settings, including their own apartment, room, or house and transitional housing (e.g., halfway house, residential program). Nights spent in shelters, outdoors, in vehicles, or in abandoned vehicles were classified as days homeless.
Clinical measures.
Participants self-reported medical, mental health, and substance use disorder diagnoses, which were corroborated by clinicians and administrative data. In the analyses, we used a count of chronic medical conditions to reflect burden of chronic illness. Serious mental illness was defined as a diagnosis of either schizophrenia or bipolar disorder.
Substance abuse.
We used the Addiction Severity Index, which consists of 6 items on an alcohol subscale and 13 items on a drug subscale, to document alcohol and drug use in the past month. Items were combined for a standard comparable score ranging from 0 to 1 for each subscale; higher scores reflected more serious substance use.30
Severity of psychiatric symptoms.
We included standardized validated instruments to assess the severity of psychiatric symptoms. Three subscales (16 items) of the Brief Symptom Inventory were used to measure 3 major domains of subjective distress: psychoticism, depression, and anxiety.31 Respondents rated symptoms on a scale ranging from 0 (never experience) to 4 (very often experience), and the Brief Symptom Inventory score presented is the mean value for the 3 subscales. Second, CICH staff rated 10 types of behavior (hallucinations, delusions, inappropriate behavior or speech) on an observed psychotic behavior rating scale on the basis of their observations during the baseline interviews. They rated each of these behaviors on a scale ranging from 0 (not at all) to 3 (a lot), and the total score was computed as the average score across these 10 items.32
Health status.
We used the 12-item Medical Outcomes Study Short Form to measure health-related quality of life.33 This measure has previously been validated in homeless samples.34 Scores range from 0 to 100, with a higher score reflecting higher functioning (a score of 50 represents the normal level of functioning in the general population, with each 10-point interval representing 1 standard deviation). We used both the Physical and Mental Health component subscales in these analyses.
Health insurance.
Staff also asked participants whether they had trouble paying for health care in the past year and for how much of the past year they had health insurance coverage (not at all, 3–6 months, 7–11 months, all year).
Community adjustment.
Participants were asked about their quality of life, social support network, and the extent of their integration into the community. Staff assessed participants’ subjective quality of life with 1 item asking them to rate their life on a 7-point scale ranging from 1 (terrible) to 7 (delightful).35 Social support networks were assessed by means of questions asking the number of people who would be available to help with 3 different types of assistance (short-term loan of $100, a ride to an appointment, or someone to talk with if they felt suicidal). Scores ranged from 0 to 10.36 To evaluate integration into the community, staff asked participants whether they had participated in 16 common activities during the previous 2 weeks (e.g., visit with friends, go to a grocery store, go to the theater). The number of activities was summed for a score ranging from 0 to 16, with higher scores indicating greater participation in community activities.37
Statistical Analyses
Our primary analysis involved the evaluation of the sociodemographic and clinical factors associated with having a PCP or using the ED as a regular source of care (a commonly used indicator of the lack of a PCP). Staff identified participants in each of these 2 groups on the basis of their response to the question “Where do you usually go when you are sick or need advice about your health?”
We first conducted bivariate comparisons of sociodemographic and clinical factors associated with using the ED as a regular source of care as opposed to having a PCP (community health clinic, hospital-based clinic, doctor’s office, or mobile health clinic). Next, we conducted forward stepwise logistic regression analyses to identify demographic and clinical characteristics independently associated with having a PCP. In a forward stepwise logistic regression, variables are sequentially added, and only significant variables are retained in each step until a final model is reached. Variables entered into the regression were age, race, education, age when first homeless, health insurance, lifetime number of years of homelessness, physical health status, lifetime years incarcerated, hours worked per week, total income, social support, quality of life, social integration score, number of days spent in one’s own place, number of days spent in an institution, number of days homeless, diagnosis of serious mental illness characterized by psychotic symptoms (schizophrenia or bipolar disorder), and all health, psychiatric, and substance abuse measures. All analyses were performed in SPSS version 17.0 (SPSS Inc., Chicago, IL).
RESULTS
Of the 870 participants, 750 (86%) indicated that they had a usual source of care and responded that at the time of program entry they either had a PCP or used the ED as their usual source of care. These participants’ mean age was 45.0 years. The sample was 74.1% male and 48.4% African American; 23.2% were veterans. Their mean lifetime number of years homeless was 8.2. More than half of the participants (54.4%) reported a drug use disorder. The rate of serious mental illness was high: 35.6% of the participants reported a diagnosis of either schizophrenia or bipolar disorder.
A total of 544 participants (72.5%) reported having a PCP, and 206 (27.5%) reported that they used the ED as their regular source of care. With respect to sociodemographic characteristics (Table 1), the participants who used the ED as a regular source of care were younger and had first become homeless at a younger age. A larger percentage of the ED users were male, and they had spent more days homeless and fewer days in their own place in the past 90 days (Table 1).
TABLE 1—
Characteristics of Sample Using Either a Primary Care Provider or the Emergency Department as a Usual Source of Health Care at Baseline: Collaborative Initiative to Help End Chronic Homelessness, United States, February 2004–April 2006.
| Characteristics | Usual PCP (n = 544), Mean or % | No Usual PCP—Use ED (n = 206), Mean or % | Pa |
| Demographic | |||
| Age, y | 45.5 | 43.6 | .007 |
| Male | 71.5 | 80.6 | .01 |
| Race/ethnicity | .08 | ||
| White | 40.4 | 32.2 | |
| Black | 45.4 | 56.1 | |
| Hispanic | 8.0 | 7.3 | |
| Other | 5.5 | 4.4 | |
| Marital status | .99 | ||
| Married | 0.9 | 1.0 | |
| Separated, widowed, or divorced | 75.9 | 75.7 | |
| Never married | 23.2 | 23.3 | |
| Education, y | 11.8 | 11.6 | .2 |
| Veteran | 24.3 | 20.4 | .26 |
| Social | |||
| Age first homeless, y | 32.5 | 30.0 | .01 |
| Lifetime y homeless | 8.0 | 8.5 | .32 |
| D in own place (past 90 d) | 7.3 | 3.9 | .02 |
| D in an institution (past 90 d) | 15.5 | 12.9 | .26 |
| D homeless (past 90 d) | 54.4 | 59.8 | .07 |
| Hr worked/wk (past 30 d) | 2.9 | 2.4 | .44 |
| Time in jail (lifetime) | .01 | ||
| 1 y | 27.4 | 25.4 | |
| ≤ 1 y | 37.0 | 31.6 | |
| > 1 y | 35.7 | 43.0 | |
| Social support | 1.4 | 1.5 | .1 |
| Quality of life | 4.3 | 4.2 | .2 |
| Community integration | 6.8 | 6.9 | .56 |
Note. ED = emergency department; PCP = primary care provider. The 11 communities funded through the collaborative were Chattanooga, TN; Chicago, IL; Columbus, OH; Denver, CO; Fort Lauderdale, FL; Los Angeles, CA; Martinez, CA; New York City, NY; Philadelphia, PA; Portland, OR; and San Francisco, CA. The sample size was n = 750. Percentages may not add to 100% because of rounding.
P values were determined using the χ2 or t test.
Participants who reported having a PCP had greater medical need. These participants were more likely to have a chronic medical condition and reported, on average, a greater number of chronic medical conditions and poorer physical health status. A greater percentage of participants with HIV reported having a PCP (rather than using the ED as a regular source of care; Table 2). We found no statistically significant differences between the groups with respect to psychiatric symptom severity (mean Brief Symptom Inventory), objective psychosis ratings, or the 12-item Medical Outcomes Study Short Form Mental Health component subscale. Rates of drug abuse were higher among participants who used the ED as a regular source of care.
TABLE 2—
Clinical Characteristics of Sample Using Either a Primary Care Provider or the Emergency Department as a Usual Source of Health Care at Baseline: Collaborative Initiative to Help End Chronic Homelessness, United States, February 2004–April 2006.
| Characteristic | Usual PCP (n = 544), Mean or % | No Usual PCP—Use ED (n = 206), Mean or % | Pa |
| Medical | |||
| Any medical problem, | 71.1 | 50.2 | .001 |
| No. of medical problems | 4.5 | 3.6 | .001 |
| Diabetes | 10.1 | 7.3 | .24 |
| HIV | 5.9 | 1.0 | .004 |
| Asthma or COPD | 20.9 | 21.7 | .82 |
| SF–12, PCS | 43.80 | 47.31 | .001 |
| Psychiatric | |||
| Alcohol abuse | 52.9 | 54.4 | .73 |
| Drug abuse | 52.0 | 60.7 | .03 |
| Schizophrenia | 17.8 | 18.0 | .97 |
| Posttraumatic stress disorder | 6.8 | 3.9 | .13 |
| Depression | 28.9 | 24.8 | .26 |
| Brief Symptom Inventory, 0–4 | 1.51 | 1.45 | .39 |
| SF–2, MCS | 39.29 | 38.98 | .66 |
| Observed psychosis scale, 0–3 | 0.22 | 0.23 | .32 |
| Addiction Severity Index | |||
| Alcohol | 0.12 | 0.14 | .32 |
| Drug | 0.05 | 0.06 | .11 |
| Health insurance all 12 mo of previous y | 65.5 | 31.9 | .001 |
| Past 3 mo, covered by | |||
| Medicaid | 27.0 | 24.1 | .43 |
| Medicare | 7.7 | 7.9 | .95 |
| Department of Veterans Affairs | 16.0 | 11.8 | .15 |
| State assistance | 41.1 | 18.3 | .001 |
| Private | 1.8 | 0.5 | .17 |
| Other | 3.1 | 0 | .01 |
| None | 18.8 | 43.9 | .001 |
| Trouble paying for health care in the past 3 mo | 26.3 | 47.5 | .001 |
Note. COPD = chronic obstructive pulmonary disease; ED = emergency department; PCS = mental health composite subscale; PCP = primary care provider; PCS = physical composite subscale; SF–12 = Medical Outcomes Study Short Form. The 11 communities funded through the collaborative were Chattanooga, TN; Chicago, IL; Columbus, OH; Denver, CO; Fort Lauderdale, FL; Los Angeles, CA; Martinez, CA; New York City, NY; Philadelphia, PA; Portland, OR; and San Francisco, CA.
P values were determined using the χ2 or t test.
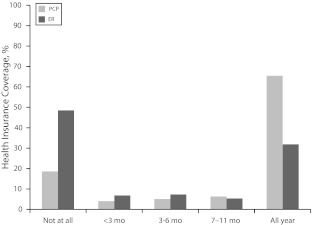
The most robust differences between the 2 groups on bivariate analyses were with respect to health insurance (Table 2, Figure 1). Participants who used the ED for a regular source of care were more likely to report having no health insurance at all in the past year (43.9% vs 18.8%, P = .001) and to have had trouble paying for health care in the past 3 months (47.5% vs 26.3%, P = .001). The greatest difference between the 2 groups with respect to type of insurance was that a higher percentage of participants with a PCP were covered by state assistance (Table 1). Not having health insurance appeared to be strongly related to having difficulty paying for health care, because more than two thirds (71.5%) of participants who had health insurance during all 12 months of the previous year reported no trouble paying for health care in the past 3 months, whereas 50.2% of patients with no health insurance at all during the past year reported trouble paying for health care in the previous 3 months (data not shown).
FIGURE 1—
Comparison of health insurance coverage in past year between participants who had a PCP (n = 544) and those who used the ED as their usual source of care (n = 206): Collaborative Initiative to Help End Chronic Homelessness, United States, February 2004–April 2006.
Note. ED = emergency department; PCP = primary care provider. The 11 communities funded through the collaborative were Chattanooga, TN; Chicago, IL; Columbus, OH; Denver, CO; Fort Lauderdale, FL; Los Angeles, CA; Martinez, CA; New York City, NY; Philadelphia, PA; Portland, OR; and San Francisco, CA. Difference significant at P < .001.
We then conducted forward stepwise multivariate logistic regression analyses to evaluate the characteristics that were independently associated with having a PCP. The logistic regression went through 7 steps before generating a final model. The final model showed that having health insurance, poorer physical health status, fewer lifetime years in jail, and more days living in either one’s own place or in an institution over the preceding 90 days were all independently and significantly associated with having a PCP (Table 3). We entered having health insurance into the first step, and it remained a significant variable throughout the stepwise analyses to the final model. Neither a diagnosis of serious mental illness (schizophrenia or bipolar disorder) nor any measure of psychiatric symptom severity was significantly associated with having a PCP at any step. We conducted an additional step to evaluate the impact of use of mental health services; this covariate was not significant and did not change the results (data not shown).
TABLE 3—
Stepwise Multivariate Logistic Regression of Characteristics Associated With Using a Primary Care Provider Rather Than the Emergency Department as a Usual Source of Care: Collaborative Initiative to Help End Chronic Homelessness, United States, February 2004–April 2006.
| Variable | B (SE) | OR (95% CI) |
| Past 90 d in | ||
| Institution | 0.01 (0.01) | 1.01 (1.01, 1.01) |
| Own place | 0.01 (0.01) | 1.01 (1.01, 1.02) |
| Social support | −0.17 (0.08) | 0.84 (0.73, 0.98) |
| Lifetime y in jail | −0.04 (0.02) | 0.96 (0.93, 0.99) |
| SF-12 PCS | −0.03 (0.01) | 0.97 (0.96, 0.99) |
| Lifetime y homeless | −0.04 (0.02) | 0.96 (0.94, 0.99) |
| Health insurance throughout previous 12 mo | 0.45 (0.05) | 1.57 (1.42, 1.74) |
Note. CI = confidence interval; OR = odds ratio; PCS = physical composite subscale; SF-12 = 12-item Medical Outcomes Study Short Form. The 11 communities funded through the collaborative were Chattanooga, TN; Chicago, IL; Columbus, OH; Denver, CO; Fort Lauderdale, FL; Los Angeles, CA; Martinez, CA; New York City, NY; Philadelphia, PA; Portland, OR; and San Francisco, CA. P values were determined using the χ2 or t test.
Participants were also asked about the major barriers to their use of outpatient medical services. The 2 main barriers reported were the inability to afford care and the prioritization of other needs above medical care, with 48% of the sample reporting that they could not afford medical care. We found no statistically significant differences with respect to reported barriers to medical care between participants with a PCP and those who used the ED as a usual source of care, although we did find a trend for participants who used the ED to report not seeking medical care because they did not think it would help (P = .09).
DISCUSSION
In this large, multisite sample of chronically homeless individuals, the factor most strongly associated with using the ED as a regular source of medical care (and not a PCP) was the lack of health insurance in the previous year. Our sample had high rates of serious mental illness (schizophrenia or bipolar disorder) even when compared with previous samples of homeless individuals,4,25,26,38 but neither a diagnosis of serious mental illness nor increased severity of symptoms on 2 measures of psychiatric symptoms was associated with using the ED as a usual source of medical care. In the current study, when participants were asked about the major barriers to their use of outpatient medical services, they identified the inability to afford care and the prioritization of other needs above medical care. Almost half of the sample reported that they could not afford medical care.
Chronically homeless individuals are a clinically complex, vulnerable population. CICH participants, as do other homeless samples, have high rates multiple chronic medical conditions along with co-occurring psychiatric and substance use disorders. Previous work by Gelberg et al.23 has suggested that among homeless individuals, having a PCP is associated with better medical outcomes. Our study extends this work and suggests that the presence of serious mental illness does not deter homeless individuals from engaging in primary care—and that the major barrier to engaging in primary care is lack of health insurance.
This finding is of critical importance, given the enormous benefits associated with having health insurance. In 2008, with limited resources to expand its Medicaid program (for 90 000 low-income adults applying for 10 000 openings), Oregon determined a lottery would be the fairest way to choose enrollees. The National Bureau of Economic Research recently examined the effects of the Oregon Medicaid lottery on access to care after approximately 1 year of insurance coverage. These investigators found that having insurance was significantly associated with better self-reported physical and mental health and far less financial distress (lower out-of-pocket medical expenditures and medical debt). Insured individuals were less likely to defer care and had increased compliance with recommended preventive care.39
Our findings suggest that chronically homeless individuals who have a significant burden of chronic medical illness would be more likely to access care if they had health insurance. Evidence of how those who are uninsured might respond once coverage becomes available has been provided by studies of novel programs that use managed care principles to shift patients away from the safety net to primary care in the community. In a study in Virginia, for example, previously uninsured individuals had fewer ED visits and inpatient admissions and more primary care visits.40 This finding has important health policy implications because a key provision of the 2010 Affordable Care Act41 is an expansion of the scope of the Medicaid program to increase the number of individuals covered by states. The original Affordable Care Act legislation requires states to extend Medicaid eligibility by 2014 to all adults within 133% of the poverty line, which is currently $11 170 for a household of 1 and $23 050 for a household of 4, or forfeit all federal Medicaid funding. This provision was weakened by the June 2012 Supreme Court decision to strike down the forfeit requirement as coercive, but the enriched federal funding (100% for 3 years, then declining to 90% in 2020) will still be available to those states that choose to expand Medicaid coverage. The original Affordable Care Act was estimated to expand Medicaid coverage for 17 million uninsured Americans40 and provide access to Medicaid for 3.7 million more individuals with severe mental illness.42
Limitations
Our study had several important limitations that must be acknowledged. First, participants were chronically homeless individuals who were enrolled in a national program to improve access to care and may not be representative of the chronically homeless population at large. Second, psychiatric diagnoses were based on self-report with corroboration from treating providers and are therefore less reliable than those based on structured psychiatric interviews. Rates of serious mental illness may possibly have been either underestimated or overestimated. Previous literature has suggested that psychiatric illness is often undiagnosed and untreated43; however, inappropriate diagnosis of bipolar disorder among CICH participants might have diluted the impact of this diagnosis on use of primary care. Third, some variables may have been excluded from the final regression model because of a limitation of stepwise regression methods. Specifically, a covariate (such as psychiatric symptom severity) may have been excluded if it was highly correlated with a covariate already identified as predictive of the dependent variable. However, examination of the correlations between either a diagnosis of serious mental illness or the 2 psychiatric symptom severity scores (Brief Symptom Inventory and Objective Psychosis Rating Scale) and the other independent covariates suggests that this explanation of the findings is not likely. Each of these 3 covariates was significantly correlated with years in jail, but not with any of the other significant covariates in the final model. These 3 covariates were also correlated with each other and with quality of life and community integration.
Finally, because the analyses were a cross-sectional evaluation of baseline data, no conclusions can be drawn about causal interactions or the impact of serious mental illness, health insurance, or engagement in primary care on medical outcomes. Most important, a high chronic medical disease burden may possibly have been the driving factor for patients to obtain both primary care and medical insurance.
Conclusions
Current health care reform efforts have focused national attention on the health needs of vulnerable populations, such as chronically homeless individuals, because they are at higher risk for morbidity and mortality. The complexity of both the clinical and the social burden experienced by chronically homeless people increases the need to identify specific targets for interventions to improve health outcomes. More aggressive attempts are needed to increase access to Medicaid and other sources of health insurance for these and other vulnerable patients. Increased access to care is intended to reduce the unnecessary use of services such as the ED and to achieve substantial cost savings. However, Medicaid expansion is not free. In the Oregon lottery, people who were newly insured had more planned hospitalizations and spent an average of $778 a year, or 25% more, on health care in the 1st year than did those who did not obtain insurance. It may take several years of insurance coverage for substantive health care savings to occur. The Supreme Court ruling gives states the flexibility not to expand their Medicaid programs (without paying the financial penalties that the Affordable Care Act called for). It remains to be seen what individual states will decide about extending Medicaid and the associated health benefits to more individuals—and whether states can see beyond the short-term monetary savings to judge Medicaid expansion by the value it offers for the money spent.
Acknowledgments
The research reported here was supported by the National Institute of Mental Health (grant K23 MH077824). The Collaborative Initiative to Help End Chronic Homelessness (CICH) Funder’s Group representing the US Departments of Housing and Urban Development, Health and Human Services, and Veterans Affairs provided essential support to and guidance for this evaluation. The CICH evaluation has been completed, and the federal government is no longer involved.
Preliminary analyses from this study were presented as a poster at the national meeting of the Academy of Psychosomatic Medicine, Chandler, AZ, November 16–20, 2011.
Note. The views presented here are those of the authors alone and do not represent the position of any federal agency or of the US Government. The authors have no conflicts of interest related to this research.
Human Participant Protection
All procedures in the CICH study were approved by the institutional review boards at the parent site and at each participating site. The analyses in this article were approved by the Human Research Protection Program of the Yale School of Medicine and the institutional review board at the VA Connecticut Healthcare System.
References
- 1. US Department of Housing and Urban Development. The 2010 Annual Homeless Assessment Report to Congress. Washington, DC: US Department of Housing and Urban Development, Office of Community Planning and Development; 2010. Available at: http://www.hudhre.info/documents/2010HomelessAssessmentReport.pdf. Accessed September 17, 2012.
- 2. Substance Abuse and Mental Health Services Administration. Blueprint for Change: Ending Chronic Homelessness for Persons With Serious Mental Illnesses and Co-occurring Substance Abuse Disorders. DHHS Pub No SMA-04-3870. Rockville, MD: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration; 2003.
- 3.Barrow SM, Herman DB, Córdova P, Struening EL. Mortality among homeless shelter residents in New York City. Am J Public Health. 1999;89(4):529–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nielsen SF, Hjorthøj CR, Erlangsen A, Nordentoft M. Psychiatric disorders and mortality among people in homeless shelters in Denmark: a nationwide register-based cohort study. Lancet. 2011;377(9784):2205–2214 [DOI] [PubMed] [Google Scholar]
- 5.Hwang SW, Lebow JM, Bierer MF, O’Connell JJ, Orav EJ, Brennan TA. Risk factors for death in homeless adults in Boston. Arch Intern Med. 1998;158(13):1454–1460 [DOI] [PubMed] [Google Scholar]
- 6.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jerant A, Fenton JJ, Franks P. Primary care attributes and mortality: a national person-level study. Ann Fam Med. 2012;10(1):34–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi L, Starfield B, Politzer R, Regan J. Primary care, self-rated health, and reductions in social disparities in health. Health Serv Res. 2002;37(3):529–550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Christakis DA, Feudtner C, Pihoker C, Connell FA. Continuity and quality of care for children with diabetes who are covered by Medicaid. Ambul Pediatr. 2001;1(2):99–103 [DOI] [PubMed] [Google Scholar]
- 10.Shea S, Misra D, Ehrlich MH, Field L, Francis CK. Predisposing factors for severe, uncontrolled hypertension in an inner-city minority population. N Engl J Med. 1992;327(11):776–781 [DOI] [PubMed] [Google Scholar]
- 11.Desai MM, Rosenheck RA, Kasprow WJ. Determinants of receipt of ambulatory medical care in a national sample of mentally ill homeless veterans. Med Care. 2003;41(2):275–287 [DOI] [PubMed] [Google Scholar]
- 12.Salit SA, Kuhn EM, Hartz AJ, Vu JM, Mosso AL. Hospitalization costs associated with homelessness in New York City. N Engl J Med. 1998;338(24):1734–1740 [DOI] [PubMed] [Google Scholar]
- 13.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200–206 [DOI] [PubMed] [Google Scholar]
- 14.Hwang SW, Weaver J, Aubry T, Hoch JS. Hospital costs and length of stay among homeless patients admitted to medical, surgical, and psychiatric services. Med Care. 2011;49(4):350–354 [DOI] [PubMed] [Google Scholar]
- 15.Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002;92(5):778–784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ku BS, Scott KC, Kertesz SG, Pitts SR. Factors associated with use of urban emergency departments by the U.S. homeless population. Public Health Rep. 2010;125(3):398–405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Han B, Wells BL. Inappropriate emergency department visits and use of the Health Care for the Homeless Program services by homeless adults in the northeastern United States. J Public Health Manag Pract. 2003;9:530–537 [DOI] [PubMed] [Google Scholar]
- 18.Kessell ER, Bhatia R, Bamberger JD, Kushel MB. Public health care utilization in a cohort of homeless adult applicants to a supportive housing program. J Urban Health. 2006;83(5):860–873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sachs-Ericsson N, Wise E, Debrody CP, Paniucki HB. Health problems and service utilization in the homeless. J Health Care Poor Underserved. 1999;10(4):443–452 [DOI] [PubMed] [Google Scholar]
- 20.Desai MM, Rosenheck RA. Unmet need for medical care among homeless adults with serious mental illness. Gen Hosp Psychiatry. 2005;27(6):418–425 [DOI] [PubMed] [Google Scholar]
- 21.Gelberg L, Linn LS, Ustaine RP, Smith MH. Health, homelessness, and poverty. A study of clinic users. Arch Intern Med. 1990;150(11):2325–2330 [PubMed] [Google Scholar]
- 22.Stein JA, Andersen RM, Koegel P, Gelberg L. Predicting health services utilization among homeless adults: a prospective analysis. J Health Care Poor Underserved. 2000;11(2):212–1230 [DOI] [PubMed] [Google Scholar]
- 23.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302 [PMC free article] [PubMed] [Google Scholar]
- 24.Stein JA, Andersen R, Gelberg L. Applying the Gelberg-Andersen behavioral model for vulnerable populations to health services utilization in homeless women. J Health Psychol. 2007;12(5):791–804 [DOI] [PubMed] [Google Scholar]
- 25.Koegel P, Burnam MA, Farr RK. The prevalence of specific psychiatric disorders among homeless individuals in the inner city of Los Angeles. Arch Gen Psychiatry. 1988;45(12):1085–1092 [DOI] [PubMed] [Google Scholar]
- 26.Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chwastiak LA, Rosenheck RA, Kazis LE. Utilization of primary care by veterans with psychiatric illness in the National Department of Veterans Affairs Health Care System. J Gen Intern Med. 2008;23(11):1835–1840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bieler G, Paroz S, Faouzi Met al. Social and medical vulnerability factors of emergency department frequent users in a universal health insurance system. Acad Emerg Med. 2012;19(1):63–68 [DOI] [PubMed] [Google Scholar]
- 29.Mares AS, Greenberg GA, Rosenheck RA. Client-level measures of services integration among chronically homeless adults. Community Ment Health J. 2008;44(5):367–376 [DOI] [PubMed] [Google Scholar]
- 30.McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic instrument for substance abuse patients: the Addiction Severity Index. J Nerv Ment Dis. 1980;168(1):26–33 [DOI] [PubMed] [Google Scholar]
- 31.Derogatis LR, Spencer N. The Brief Symptom Index: Administration, Scoring, and Procedure Manual. Baltimore, MD: Johns Hopkins University Press; 1982 [Google Scholar]
- 32.Dohrenwend B. Psychiatric Epidemiology Research Interview (PERI). New York, NY: Columbia University Social Psychiatry Unit; 1982 [Google Scholar]
- 33.Ware JE, Kosinski M, Keller SE. How to Score the SF-12 Physical and Mental Health Summary scales. 3rd ed. Lincoln, RI: Quality Metric; 1998 [Google Scholar]
- 34.Larson CO. Use of the SF-12 instrument for measuring the health of homeless persons. Health Serv Res. 2002;37(3):733–750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lehman A. A quality of life interview for the chronically mentally ill. Eval Program Plann. 1988;11(1):51–62 [Google Scholar]
- 36.Vaux A, Athanassopulou M. Social support appraisals and network resources. J Community Psychol. 1987;15(4):537–556 [Google Scholar]
- 37.Katz AH. Social adaptation in chronic illness: a study of hemophilia. Am J Public Health Nations Health. 1963;53:1666–1675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.North CS, Eyrich KM, Pollio DE, Spitznagel EL. Are rates of psychiatric disorders in the homeless population changing? Am J Public Health. 2004;94(1):103–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Finkelstein A, Taubman S, Wright Bet al. The Oregon Health Insurance Experiment: evidence from the first year. NBER Working Paper No. 17190. Cambridge, MA: National Bureau of Economic Research; 2011. Available at: http://www.nber.org/papers/w17190. Accessed September 17, 2012 [Google Scholar]
- 40.Bradley CJ, Gandhi SO, Neumark D, Garland S, Retchin SM. Lessons for coverage expansion: a Virginia primary care program for the uninsured reduced utilization and cut costs. Health Aff (Millwood). 2012;31(2):350–359 [DOI] [PubMed] [Google Scholar]
- 41. Patient Protection and Affordable Care Act, Pub. L. No. 111–148, § 3502, 124 Stat 119, 124 (2010)
- 42.Garfield RL, Zuvekas SH, Lave LR, Donohue JM. The impact of national health care reform on adults with severe mental disorders. Am J Psychiatry. 2011;168(5):486–494 [DOI] [PubMed] [Google Scholar]
- 43.Weissman MM, Leaf PJ, Tischler GLet al. Affective disorders in five United States communities. Psychol Med. 1988;18(1):141–153 [DOI] [PubMed] [Google Scholar]