Abstract
Study design: Systematic review.
Clinical questions: What is the effectiveness of multilevel cervical artificial disc replacement (C-ADR) compared with multilevel fusion with respect to pain and functional outcomes, and are the two procedures comparable in terms of safety? What is the effectiveness of multilevel C-ADR compared with single-level C-ADR with respect to pain and functional outcomes, and are the two procedures comparable in terms of safety?
Methods: A systematic review was undertaken for articles published up to October 2011. Electronic databases and reference lists of key articles were searched to identify studies comparing multilevel C-ADR with multilevel anterior cervical discectomy and fusion (ACDF) or comparing multilevel C-ADR with single-level C-ADR. Studies which compared these procedures in the lumbar or thoracic spine or that reported alignment outcomes only were excluded. Two independent reviewers assessed the strength of evidence using the GRADE criteria and disagreements were resolved by consensus.
Results: Two studies compared multilevel C-ADR with multilevel ACDF. While both reported improved Neck Disability Index (NDI) and Short-Form 36 (SF-36) scores after C-ADR compared with ACDF, only one study reported statistically significant results. Seven studies compared single-level C-ADR with multilevel C-ADR. Results were similar in terms of overall success, NDI and SF-36 scores, and patient satisfaction. There is discrepant information regarding rates of heterotopic ossification; dysphagia rate may be higher in multilevel C-ADR.
Conclusions: The literature suggests that outcomes are at least similar for multilevel C-ADR and ACDF and may favor C-ADR. Future studies are necessary before firm recommendations can be made favoring one treatment strategy. Multilevel C-ADR seems to have similar results to single-level C-ADR but may have higher rates of heterotopic ossification and dysphagia.
Study Rationale and Context
While the benefit of single-level C-ADR is increasingly well-described in the literature, the role of multilevel C-ADR is less clear. The purpose of this systematic review was to compare outcomes after multilevel C-ADR with those after multilevel ACDF and to evaluate whether favorable single-level C-ADR outcomes extend to multilevel surgery.
Clinical Questions
What is the effectiveness of multilevel C-ADR compared with multilevel fusion with respect to pain and functional outcomes?
What is the safety of multilevel C-ADR compared with multilevel fusion?
What is the effectiveness of multilevel C-ADR compared with single-level C-ADR with respect to pain and functional outcomes?
What is the safety of multilevel C-ADR compared with single-level C-ADR?
Materials and Methods
Study design: Systematic review.
Sampling:
Search: PubMed, Cochrane collaboration database, and National Guideline Clearinghouse databases; bibliographies of key articles.
Dates searched: January 1980–October 1, 2011.
Inclusion criteria: Studies comparing (1) multilevel C-ADR with multilevel fusion in the cervical spine; (2) multilevel C-ADR with single-level C-ADR in the cervical spine; and (3) studies published in English-language peer-reviewed journals.
Exclusion criteria: (1) Studies in the thoracic or lumbar spine; (2) disc nucleus replacement, annular reconstruction techniques, or other forms of intradiscal spacers as comparators; (3) studies reporting alignment outcomes only; and (4) case-reports.
Outcomes: Neck Disability Index (NDI), pain in the neck and arm (Visual Analog Scale [VAS]), Odom’s criteria (overall success), neurological success, Quality of Life (SF-36 Physical Component Score [PCS] and Mental Component Score [MCS]), adjacent segment disease (ASD), range of motion (ROM), return to work, analgesic use, subsequent surgeries, and complications/adverse events. Odom’s criteria classifies patients according to the following categories: (1) excellent—all preoperative symptoms relieved; abnormal findings improved; (2) good—minimal persistence of preoperative symptoms; abnormal findings unchanged or improved; (3) fair—definite relief of some preoperative symptoms; other symptoms unchanged or slightly improved; and (4) poor—symptoms and signs unchanged or exacerbated. NDI asks patients to evaluate severity of symptoms and disability in the following ten areas: pain intensity, personal care, lifting, reading, headache, concentration, work, driving, sleeping, and recreation.
Analysis: Descriptive statistics.
Details about methods can be found in the Web Appendix at www.aospine.org/ebsj
Results
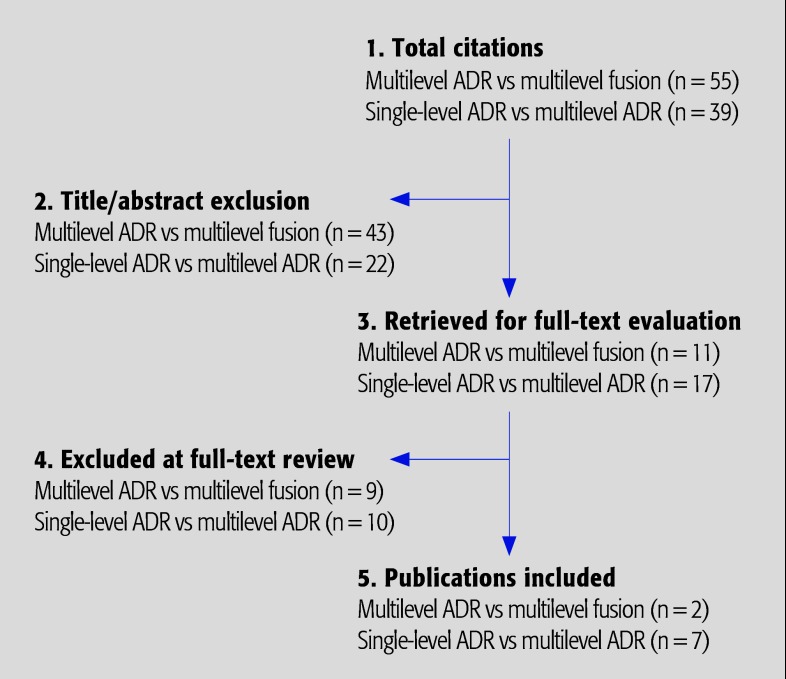
A total of nine studies were found that met the inclusion criteria (Fig. 1). Of the nine, two, a randomized controlled trial (RCT) and a prospective cohort, compared C-ADR with ACDF; and seven, four prospective and three retrospective cohorts, compared multilevel C-ADR with single-level C-ADR in the cervical spine. Further details on the class of evidence rating for these studies can be found in the Web Appendix at www.aospine.org/ebsj, but the current level of evidence available on the topic is relatively low. Demographic and study details are provided in Table 1.
Fig. 1.
Results of literature search.
Table 1. Characteristics of included studies.*.
| Author (year)/study design | CoE | Demographics | Diagnosis | Interventions | Follow-up | Funding | ||
|---|---|---|---|---|---|---|---|---|
| Studies comparing multilevel C-ADR and multilevel ACDF | ||||||||
| Cheng et al 1 (2009) RCT Single site |
II | C-ADR
|
Spondylotic myelopathy or cervical radiculopathy due to a disc herniation or stenosis | C-ADR using the Bryan disc; all procedures performed by same surgeon ACDF with iliac crest autograft; anterior cervical plating with the Orion Cervical Plate System |
2 y C-ADR: 96.8% (30/31) ACDF: 94.1% (32/34) |
NR | ||
| Kim et al 6 (2009) Prospective cohort |
III | C-ADR†
|
Symptomatic single- or 2-level cervical disc disease Radiculopathy
|
C-ADR using Bryan disc ACDF with autogenous bone using various types of anterior cervical plates (ABC, Atlantis) or stand-alone cages (Blackstone, Solis) |
C-ADR
|
NR | ||
| Studies comparing single-level C-ADR and multilevel C-ADR | ||||||||
| Coric et al 7 (2010) Prospective cohort‡ |
II | N = 57 Male: 41.5% Mean age: 46.6 y |
Symptomatic cervical radiculopathy or myelopathy | C-ADR | Follow-up: 2 y (93%; n = 53/57) |
Primary author is a consultant for Depuy Spine and Spinal Motion | ||
| Goffin et al 3 (2010)§ Retrospective cohort |
III | N = 98 Single level, n = 89
|
Radiculopathy due to: Disc herniation
Disc herniation
|
C-ADR with Bryan disc | Follow-up: 4–6 y
Multilevel: 66.7% (6/9) |
Research support and editorial assistance for this study was received from Medtronic Sofamor Danek. In addition, statistical analysis was conducted in collaboration with Medtronic. A nonstudy-related institutional grant for research and education was also received from Medtronic. Dr Lipscomb serves as a consultant for and owns stock in Medtronic. |
||
| Huppert et al 5 (2011) Prospective cohort |
III | N = 231∥ Single level, n = 175
|
DDD causing radiculopathy and/or myelopathy | Mobi-C C-ADR Single-level and multilevel procedures performed by same surgeons, using same operative procedure, during the same time interval No. of levels treated in multilevel group:
|
Single level: Mean 2.1 (1.5–2.6) y % Followed-up NR Multilevel:
|
NR | ||
| Kim et al 2 (2009) Retrospective cohort |
III | N = 52 Male: 55.8% Mean age (range): 47.2 (28–77) y Single level: n = 36 (69%) Multilevel: n = 16 (31%) |
Herniated disc: 44.2% Spondylosis: 34.6% Mixed: 15.8% OPLL: 5.8% |
Bryan C-ADR Concomitantly performed surgeries included:
|
Follow-up: mean 2.4 (1.5–3) y % Followed-up NR |
NR | ||
| Kim et al 6 (2009) Prospective cohort |
III | N = 51¶ Single level, n = 39 Male: 53.8% Mean age (range): 43.6 (24–74) y Multilevel, n = 12
|
Radiculopathy Single level: 92.3% Multilevel: 83.3% Myelopathy Single level: 7.7% Multilevel: 16.7% |
Bryan C-ADR All procedures performed by same surgeon |
Follow-up: mean 1.5 (1.1–3.3) y % Followed-up NR |
NR | ||
| Pimenta et al 4 (2007) Prospective cohort |
II | N = 140 Single level, n = 71
|
HNP
|
C-ADR using the PCM Porous Coated Motion Device Intervertebral Dynamic Disc Spacer No. of levels treated in multilevel group:
|
Follow-up: mean 2.2 (1–3.5) y Follow-up 100% |
Corporate/ industry and foundation funds were received in support of this work. One or more of the author(s) has/have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. |
||
| Tu et al 8 (2011) Retrospective cohort |
III | N = 36 Male: 58.3% Mean age (range): 46.6 (29–60) y Singlelevel, n = 20 (55.6%) Multilevel, n = 16 (44.4%) |
Disc herniation: 61.1% Spondylosis: 38.9% Radiculopathy: 50.0% Myelopathy: 13.9% Both: 19.4% Axial neck pain: 16.7% |
C-ADR using Bryan | Follow-up: mean 1.6 (range, 1–2.3) y 1 y: 100% 2 y : 69.4% (25/36) |
This study was supported by grant VGH 99-S6-001 from Taipei Veterans General Hospital. The authors report no conflict of interest. |
||
C-ADR indicates cervical artificial disc replacement; ACDF, anterior cervical discectomy and fusion; FSU, functional spinal unit; CoE, level of evidence; NR, not reported; RCT, randomized control trial; DDD, degenerative disc disease; OPLL, ossification of the posterior longitudinal ligament; HNP, herniated nucleus pulposis.
The study reported comparisons between both single-level and multilevel C-ADR and ACDF. Only 2-level cases are reported for the purpose of this article.
This study compared pooled groups of patients from three RCTs who underwent C-ADR vs ACDF (N = 98). Only the C-ADR group is reported here. Demographics are after loss to follow-up (n = 53).
Long-term follow-up results from Goffin et al3. The 98 patients included in this study agreed to participate in follow-up studies for up to 10 years; the original study had a total of 146 patients enrolled.
A total of 384 patients were enrolled in this study; a total of 231 (60.2%) have completed their 2-month follow-up evaluation and were included in the analysis.
Only the comparison between single-level and multilevel C-ADR is reported.
Multilevel C-ADR versus multilevel ACDF
Overall success
Odom’s criteria was reported by one study at 2 years with excellent or good results seen in 96.7% of multilevel C-ADR patients compared with 84.4% of multilevel ACDF patients (P = not reported).1
Function and pain (Table 2)
Table 2. Function and neck pain following multi-level C-ADR and multilevel ACDF.*.
| NDI Mean score (% change from preop) | VAS neck painMean score (% change from preop) | |||||
|---|---|---|---|---|---|---|
| C-ADR | ACDF | P | C-ADR | ACDF | P | |
| Preop | ||||||
| Cheng et al 1 (2009) | 50 | 51 | NS | 7.3 | 7.1 | NS |
| Kim et al 2(2009) | 26.4 | 26.2 | NS | 8.8 | 8.1 | NR |
| 1 year | ||||||
| Cheng et al 1 (2009) | 12 (76.0) | 18 (64.7) | .03 | 1.9 (74.0) | 2.5 (64.8) | NR |
| 2 years | ||||||
| Cheng et al 1 (2009) | 11 (78.0) | 19 (62.7) | .02 | 1.5 (79.5) | 2.6 (63.4) | .01 |
| Kim et al 2 (2009) | 7.8 (70.5) | 8.0 (69.5) | NS | 3.3 (62.5) | 3.4 (58.0) | NS |
C-ADR indicates cervical artificial disc replacement; ACDF, anterior cervical discectomy and fusion; NDI, Neck Disability Index; VAS, Visual Analog Scale; preop, preoperative; NR, not reported; and NS, not statistically significant.
One study reported outcomes at 1 year and found that multilevel C-ADR resulted in greater improvement from baseline compared with multilevel ACDF in NDI (76.0% vs 64.7%, P = .03) and VAS neck pain (74.0% vs 64.8%, P = NR) and; conversely, slightly less improvement was seen for VAS arm pain: 74.6% vs 80.6% (P = NR).1
Both studies reported greater improvement from baseline to 2 years in NDI and VAS neck pain following multilevel C-ADR vs multilevel ACDF;1,2 however, only one study1 reported that the differences were statistically significant, respectively: NDI, 78.0% vs 62.7% (P = .02) and 70.5% vs 69.5% (P = ns); VAS neck pain, 79.5% vs 63.4 (P = .01) and 62.5% vs 58.0% (P = not significant).
Quality of life
In one study, both the C-ADR and ACDF groups improved from their baseline SF-36 PCS of 35 and 34, respectively, to 49 and 46 at 1 year and 50 and 45 at 2 years; however, the C-ADR group showed a statistically greater percentage improvement at both time points over baseline compared with the ACDF group: 40.0% vs 35.3% (P = .03) and 42.9% vs 32.4% (P = .01).1
Complications
Only one study reported complications following surgery.1 One incidence of deep vein thrombosis was seen in the C-ADR group and one case of dysphagia in the ACDF group.
There were no occurrences of cerebrospinal fluid leak or hematoma in either group and no incidences of vascular or neurological complications, spontaneous fusions, device failure, or explantations in the C-ADR group.
Single-level versus multilevel C-ADR
Overall and neurological success
Odom’s criteria was reported by two studies, both of which reported similar proportions of excellent or good results between the single-level and multilevel C-ADR groups, respectively: at 4 years (88.8% [71/80] and 88.9% [8/9]) and 6 years (90.6% [48/53]) vs 100% (6/6)] in one study, and at 3 years 76% (54/71) and 85% (59/69)] in the second study.3,4
One study defined overall success as an improvement of ≥15% in NDI and absence of revision surgery; rates at 2 years were similar between the single-level (69%) and multilevel (66%) groups (follow-up numerators and denominators not reported).5
Overall neurological success was reported by one study which stated that single-level and multilevel C-ADR patients showed similar rates at 1 and 2 years, 4 years, and 6 years follow-up (no other data presented).3
Function and pain (Table 3)
Table 3. Function and neck pain following single-level and multilevel C-ADR.*.
| NDI Mean score (% change from preop) | VAS neck pain Mean score (% change from preop) | |||||
|---|---|---|---|---|---|---|
| Single | Multi | P | Single | Multi | P | |
| Preop | ||||||
| Huppert et al 5 (2011) | 51.5 | 51.4 | NS | 5.3† | 5.1† | NS |
| Kim et al 6 (2009) | 25.3 | 26.4 | NS | 8.3 | 8.8 | NS |
| Pimenta et al 4 (2007) | 48 | 44 | NS | 8.6 | 8.5 | NS |
| 1 year | ||||||
| Huppert et al 5 (2011) | 25.5 (50.5) | 30.0 (41.6) | NR | 2.1 (60.4) | 2.2 (56.8) | NR |
| Kim et al 6 (2009) | 7.6 (69.9) | 7.8 (70.5) | NS | 3.7 (55.4) | 3.3 (62.5) | NS |
| Pimenta et al 4 (2007) | 27 (43.8) | 20 (54.5) | NR | 3.3 (61.6) | 3.0 (64.7) | NR |
| 2 years | ||||||
| Huppert et al 5 (2011) | 27.3 (47.0) | 29.2 (43.2) | NS | 2.4 (54.7) | 2.4 (52.9) | NS |
| Pimenta et al 4 (2007) | 26 (45.8) | 22 (50.0) | NR | 3.0 (70.0) | 2.7 (68.2) | NR |
| 3 years | ||||||
| Pimenta et al 4 (2007) | 21 (56.3) | 11 (75.0) | NR | 4.0 (53.5) | 1.5 (82.4) | NR |
C-ADR indicates cervical artificial disc replacement; NDI, Neck Disability Index; VAS, Visual Analog Scale; preop, preoperative; NR, not reported; and NS, not statistically significant.
Pain scores from Huppert et al 5 were normalized from a VAS 100 mm scale to a VAS 10 mm scale for comparison purposes.
No significant differences were seen between single-level and multilevel C-ADR in NDI or VAS neck pain scores at 1, 2 or 3 years follow-up as reported by three studies.2,4,6
One study conducted follow-up at 4 and 6 years and reported similar NDI scores between the groups at both periods (data NR); VAS arm and neck pain scores were lower in the multilevel compared with single-level C-ADR group (data NR).3
Analgesic use at 2 years was compared between groups in one study with 32% of single-level patients compared with 53% of multilevel patients still using an analgesic (P = .03).5 This study did not define whether analgesic use referred to narcotic use only or whether it referred to use of both narcotic and non-narcotic analgesics.
One study reported a Treatment Intensity Score which takes into account analgesic medication requirements and found that overall mean improvement from baseline was 39.3% vs 54.3% in single-level and multilevel C-ADR groups, respectively (P = NR).4 This study similarly did not define whether the Treatment Intensity Score considered narcotic use only or whether use of both narcotic and non-narcotic analgesics were considered.
Quality of life (Table 4)
Table 4. Health-related quality of life following single-level and multilevel C-ADR.*.
| Study/follow-up | SF-36 PCS Mean score (% change from preop) | SF-36 MCS Mean score (% change from preop) | ||||
|---|---|---|---|---|---|---|
| Single | Multi | P | Single | Multi | P | |
| Preop | ||||||
| Goffin et al 3 (2010)† | 36.1 | 37.4 | NS | 40.1 | 35.5 | NS |
| Huppert et al 5 (2011) | 36.6 | 36.6 | NS | 35.3 | 34.3 | NS |
| 1 year | ||||||
| Goffin et al 3 (2010)† | 46.9 (29.9) | 47.0 (25.7) | NR | 50.0 (24.7) | 46.1 (29.9) | NR |
| Huppert et al 5 (2011) | 47.2 (29.0) | 45.7 (24.9) | NR | 45.9 (30.0) | 44.0 (28.3) | NR |
| 2 years | ||||||
| Goffin et al 3 (2010)‡ | 45 (24.7) | 49 (31.0) | NR | 51 (27.2) | 53 (49.3) | NR |
| Huppert et al 5 (2011) | 46.7 (27.6) | 43.9 (19.9) | NS | 46.0 (30.3) | 45.6 (32.9) | NS |
| 4 years | ||||||
| Goffin et al 3 (2010)‡ | 47 (30.2) | 52 (39.0) | NR | 52 (29.7) | 52 (46.5) | NR |
| 6 years | ||||||
| Goffin et al 3 (2010)‡ | 47 (30.2) | 51 (36.4) | NR | 52 (29.7) | 47 (32.4) | NR |
C-ADR indicates cervical artificial disc replacement; SF-36, Short-Form 36; PCS, Physical Component Score; MCS, Mental Component Score; preop, preoperative; NS, not statistically significant; and NR, not reported.
Preoperative and 1 year scores were taken from Goffin et al3 which reported short-term follow-up outcomes for the same population.
Means estimated from figures provided in the article.
No significant differences were reported between single-level and multilevel C-ADR in SF-36 PCS and MCS at 1, 2, 4, or 6 years follow-up in two studies.3,5
Patient satisfaction and return to work
One study reported that 94.2% and 94.5% of patients who underwent single-level and multilevel C-ADR, respectively, would undergo the same procedure again.5
This same study reported that at 2 years 70% of single-level C-ADR patients and 46% of multilevel C-ADR patients had returned to part-time or full-time work (P = .09) with respective mean time-to-return-to-work of 4.8 vs 7.5 months (P = .08).
Complications (Table 5)
Table 5. Complications and adverse events following single-level and multilevel C-ADR.*.
| Single level, % (n/N) | Multilevel, % (n/N) | P | Follow-up, y | |
|---|---|---|---|---|
| Reoperation | ||||
| Coric et al 7 (2010) | 5.0 (2/40) | 16.7 (2/12) | NR | 2 |
| Huppert et al 5 (2011) | 2.3 (4/175) | 3.6 (2/56) | NS | 2 |
| Pimenta et al 4 (2007) | 4.2 (3/71) | 2.9 (2/69) | NS | NR |
| Revision | ||||
| Huppert et al 5 (2011) | 0.6 (1/175) | 0 (0/56) | NS | 2 |
| Heterotopic ossification | ||||
| Any | ||||
| Huppert et al 5 (2011) | 66.7 (110/165) | 55.0 (61/111) | .02 | 2 |
| Tu et al 8 (2011) | 30.0 (6/20) | 75.0 (12/16) | .007 | 1 |
| Grade IV | ||||
| Coric et al 7 (2010) | 0 (40) | 8.3 (1/12) | NR | 2 |
| Huppert et al 5 (2011) | 10.3 (17/165) | 7.2 (8/111) | NS | 2 |
| Pimenta et al 4 (2007) | 1.4 (1/71) | 0 (0/69) | NR | NR |
| Dysphagia | ||||
| Huppert et al 5 (2011) | 4.0 (7/175) | 16.1 (9/56) | .002 | 2 |
| Device subsidence | ||||
| Huppert et al 5 (2011) | 1.1 (2/175) | 0 (5/56) | NS | 2 |
| Device migration | ||||
| Huppert et al 5 (2011) | 0.6 (1/175) | 1.8 (1/56) | NS | 2 |
| Infection | ||||
| Pimenta et al 4 (2007) | 0 (0/71) | 0 (0/69) | – | NR |
| Mortality | ||||
| Pimenta et al 4 (2007) | 0 (0/71) | 0 (0/69) | – | NR |
| Any event | ||||
| Goffin et al 3 (2010) | 66.3 (61/92) | 40.0 (4/10) | NR | 6 † |
Incidences reflect the number of patients with one or more adverse event/complication. C-ADR indicates cervical artificial disc replacement; NR, not reported; and NS, not significant.
Approximately 60% of all reported adverse events occurred 2 years after index surgery and about 15% of these events were continuations of earlier reports.
Reoperation was reported by three studies, one of which reported a lower rate at 2 years following single-level compared with multilevel C-ADR, 5.0% vs 16.7% (P = .22).7 The remaining two studies reported similar reoperation rates between the groups, 2.3% vs 3.6% and 4.2% and 2.9%, respectively.4,5
Two studies compared the rates of any grade of heterotopic ossification (HO) between groups. One study5 reported a significantly higher rate of HO at 2 years among single-level patients, 66.7% vs 55.0% following multilevel C-ADR (P = .02). Conversely, the second study8 reported a much lower rate at 1 year in those who underwent single-level C-ADR compared with multilevel, 30% vs 75% (P = .007).
A significantly lower incidence of dysphagia was reported following single-level compared with multilevel C-ADR at 2 years in one study,5 4.0% vs 16.1% (P = .002).
Rates of revision, device subsidence or migration, infection, mortality, and other complications were similar between groups.
Evidence Summary
Clinical Guidelines
No clinical guidelines were found.
Case Study
The patient is a 28-year-old man with cervical radiculopathy which affects the right C5 and bilateral C7 nerve roots. He has completed 4 months of conservative therapy including physical therapy and selective nerve root blocks and continues to have pain and bilateral triceps weakness.
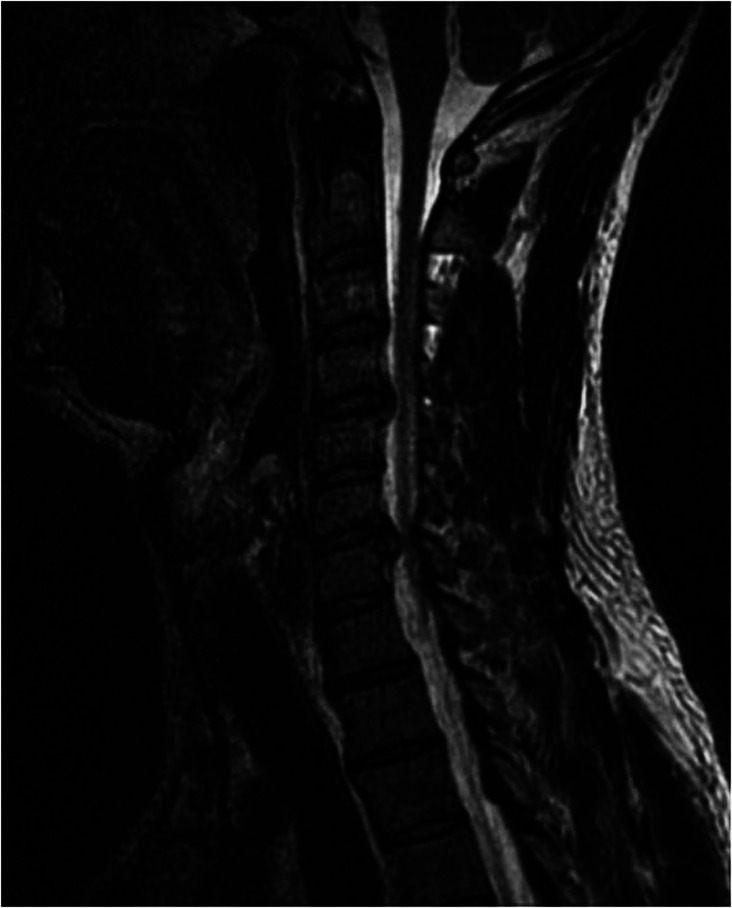
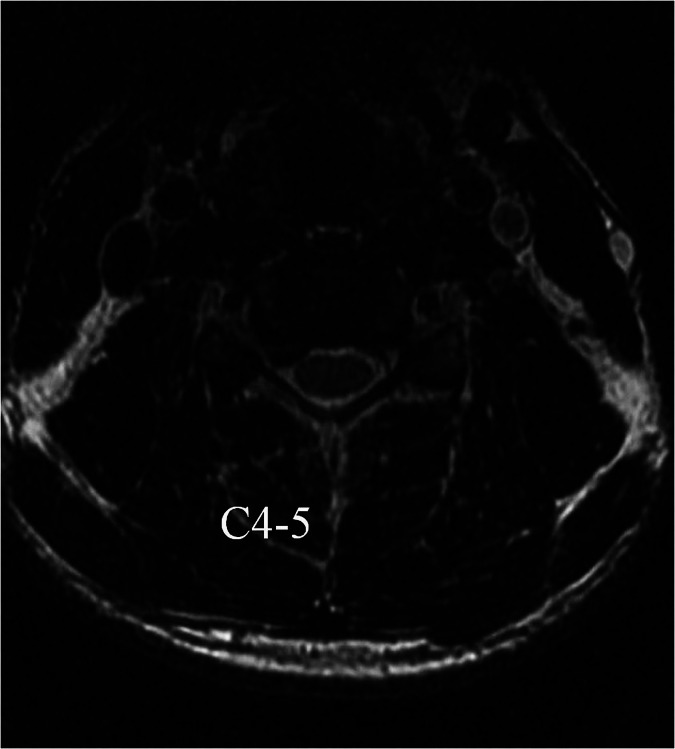
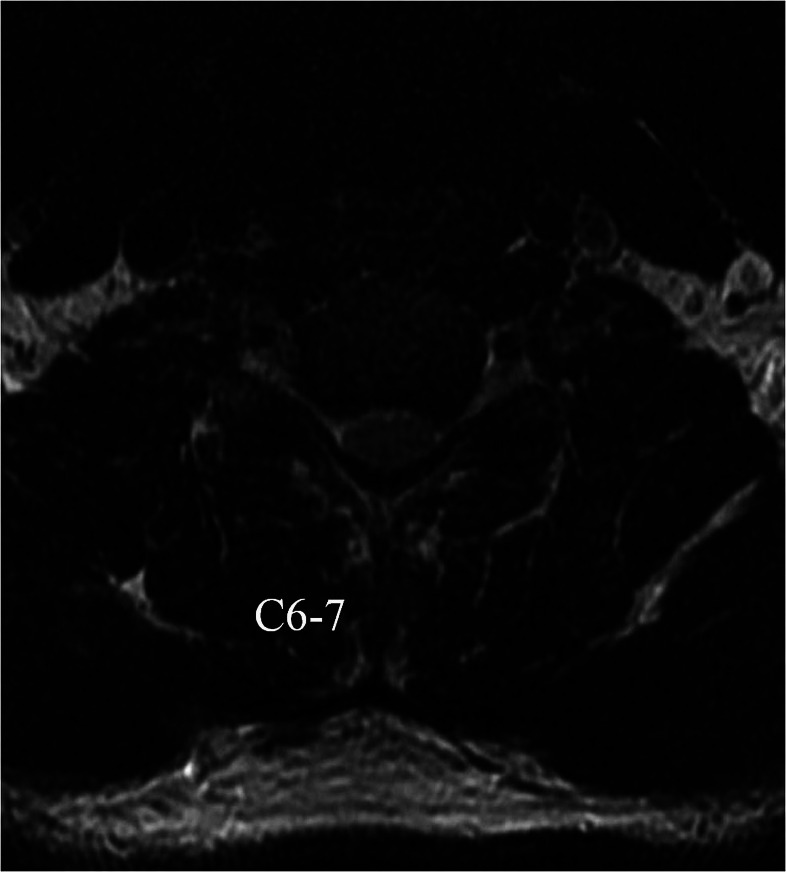
A sagittal T2-weighted MRI image is shown (Fig. 2) as are axial T2 images at C4–5 and C6–7 which demonstrate neuroforaminal stenosis on the right side at C4–5 and both sides at C6–7 (Figs. 3 and 4).
Rather than undergo noncontiguous ACDF, the patient elected to undergo noncontiguous C-ADR. Postoperatively, the patient’s upper extremity pain resolved and he remains free of pain 1 year after surgery (Figs. 5 and 6).
Fig. 2.
Midline sagittal T2 MRI image demonstrates evidence of disc herniation at C4–5 and C6–7 while the other motion segments appear relatively well-preserved.
Fig. 3.
Axial T2 MRI image at C4–5 demonstrates right-sided neuroforaminal stenosis secondary to disc herniation.
Fig. 4.
Axial T2 MRI image at C6–7 demonstrates bilateral neuroforaminal stenosis secondary to disc protrusion.
Fig. 5.
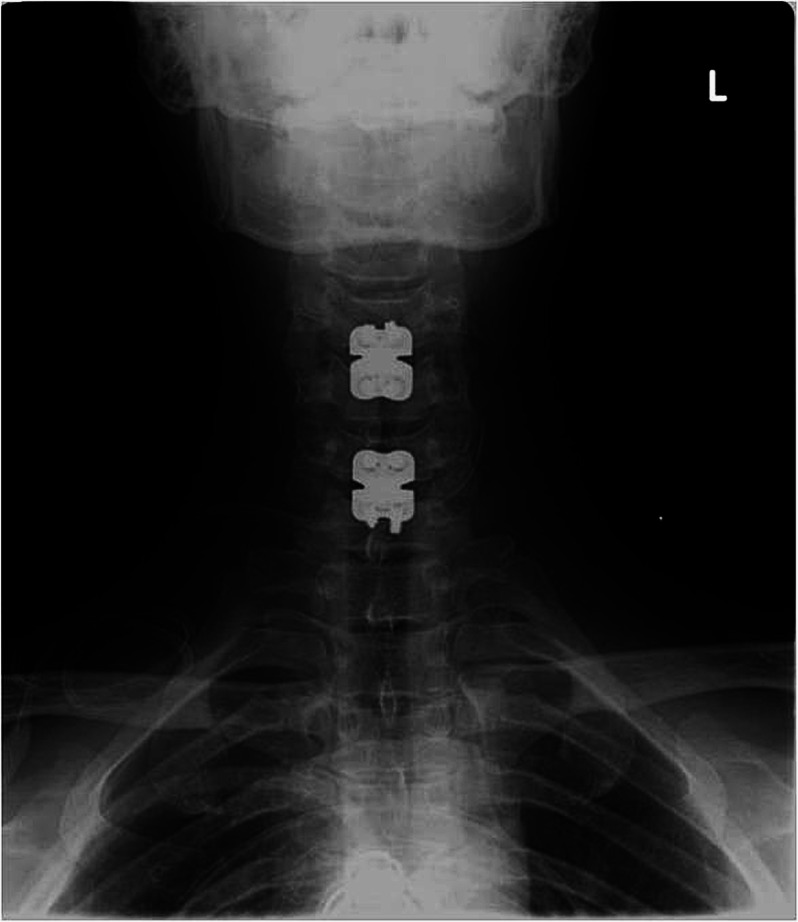
Anteroposterior postoperative x-ray demonstrates C4–5 and C6–7 disc replacements which are well-placed in midline.
Fig. 6.
Neutral lateral postoperative x-ray demonstrates C4–5 and C6–7 disc replacements.
Discussion
Multilevel C-ADR vs multilevel ACDF (Table 6)
Table 6. Multilevel C-ADR versus multilevel ACDF.
| Pain and disability | ||
|---|---|---|
| Outcomes | Strength of evidence | Conclusions/comments |
| 1. Overall success | Odom’s criteria reported by one RCT at 2 years with excellent or good results seen in a greater proportion of multilevel C-ADR patients compared with multilevel ACDF patients. | |
| 2. VAS – Neck pain |
Greater improvement in neck pain from baseline to 1 and 2 years reported by two studies following multilevel C-ADR versus multilevel ACDF; however, only one reported that the differences were statistically significant. | |
| –Arm pain | Slightly greater improvement in arm pain at 1 year after multilevel C-ADR compared with multilevel ACDF in one study. | |
| 3. NDI | Greater improvement from baseline to 1 and 2 years follow-up following multilevel C-ADR versus multilevel ACDF reported by two studies; however, only one reported that the differences were statistically significant. | |
| 4. Quality of Life | The C-ADR group showed a statistically greater percentage improvement at 1 and 2 years over baseline compared with the ACDF group as reported by one RCT. | |
| Complications | ||
|---|---|---|
| Outcomes | Strength of evidence | Conclusions/comments |
| 1. Overall complications | Only one study reported complications following surgery with no differences reported between groups. | |
Of principal clinical interest as represents potential scenario with clinical equipoise
Single study suggests outcomes significantly improved with multilevel C-ADR vs ACDF
Cannot recommend either multilevel C-ADR or ACDF on basis of single study
Single-level C-ADR vs multilevel C-ADR (Table 7)
Table 7. Single-level versus multilevel C-ADR.
| Pain and disability | ||
|---|---|---|
| Outcomes | Strength of evidence | Conclusions/comments |
| 1. Overall success | Three studies reported various measures of overall success (Odom’s criteria, neurological success, composite measure) and found no statistical differences between treatment groups across 1 to 6 years of follow-up. | |
| 1. Pain | Measured a variety of ways (VAS, analgesic use, treatment intensity score) across four studies. Inconsistent results regarding the effectiveness of one surgery to provide better pain relief over the other. |
|
| 3. NDI | No significant differences between single-level and multilevel C-ADR in NDI scores over 1 to 6 years follow-up as reported by four studies. | |
| 4. Quality of Life (SF-36 PCS and MCS) |
No significant differences were reported between single-level and multilevel C-ADR at 1, 2, 4, or 6 years follow-up in two studies. | |
| 5. Patient satisfaction | Similar numbers of patients in both treatment groups were satisfied with their treatment and would repeat the procedure as reported by one study. | |
| 6. Return to work | Greater proportion of multilevel C-ADR patients returned to part-time or full-time work and at a quicker rate than single-level C-ADR patients in one study. | |
| Complications | ||
|---|---|---|
| Outcomes | Strength of evidence | Conclusions/comments |
| 1. Reoperation | Reoperation was reported by three studies, one of which reported a lower rate at 2 years following single-level compared with multilevel C-ADR, and two studies reported similar reoperation rates between the groups. | |
| 2. Heterotopic ossification | Two studies reported conflicting results for the rate of HO between groups. | |
| 3. Other complications | A significantly lower incidence of dysphagia was reported following single-level compared with multilevel C-ADR at 2 years in one study. Rates of revision, device subsidence or migration, infection, mortality, and other complications were similar between groups. |
|
Results appear similar for functional outcome measures, success rate, and patient satisfaction
Lower return to work rate after multilevel C-ADR potentially related to greater baseline disability, longer duration of symptoms before surgery.
HO results confusing – unclear why HO would be more common after single-level surgery
Higher rates of dysphagia after multilevel C-ADR expected because length and force of retraction on the esophagus and associated swelling likely contribute to dysphagia
Strengths:
The question was reviewed systematically.
Limitations:
Few studies available to address multilevel C-ADR vs multilevel fusion.
Loss to follow-up was not reported in one study comparing multilevel C-ADR and fusion and in three studies comparing single-level vs multilevel C-ADR, possibly biasing results.
No definition of clinically meaningful improvement in VAS or NDI was provided.
Surveillance for and definitions of complications varied across studies.
Clinical relevance and impact
While there is insufficient evidence to make strong recommendations regarding the relative benefit of multilevel C-ADR vs multilevel ACDF, there conversely is no evidence suggesting that results after C-ADR are worse than after ACDF; more studies must be done to investigate whether there is a clinical role for multilevel C-ADR. More data is available to compare single-level and multilevel C-ADR; results after multilevel C-ADR appear similar to single-level C-ADR and do not demonstrate elevated reoperation or failure rates. Increase in dysphagia rate after multilevel C-ADR is to be expected compared with single-level C-ADR, a less invasive procedure. Studies with longer-term follow-up are necessary to evaluate the theoretical benefit of C-ADR in reducing ASD and to test whether results are as durable as after multilevel ACDF.
Summary and Conclusions
Although the best available literature suggests multilevel C-ADR has a slight advantage over ACDF at short-term follow-up, there is insufficient evidence to make treatment recommendations.
Multilevel C-ADR has similar results to single-level C-ADR at short-term follow-up.
Dysphagia rates are higher after multilevel C-ADR compared with single-level C-ADR.
Footnotes
No funding was received in support of this work.
References
- 1.Cheng L, Nie L, Zhang L. et al. Fusion versus Bryan Cervical Disc in two-level cervical disc disease: a prospective, randomised study. Int Orthop. 2009;33(5):1347–1351. doi: 10.1007/s00264-008-0655-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim H K, Kim M H, Cho D S. et al. Surgical outcome of cervical arthroplasty using bryan(r) J Korean Neurosurg Soc. 2009;46(6):532–537. doi: 10.3340/jkns.2009.46.6.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goffin J, Loon J van, Calenbergh F van. et al. A clinical analysis of 4- and 6-year follow-up results after cervical disc replacement surgery using the Bryan Cervical Disc Prosthesis. J Neurosurg Spine. 2010;12(3):261–269. doi: 10.3171/2009.9.SPINE09129. [DOI] [PubMed] [Google Scholar]
- 4.Pimenta L, McAfee P C, Cappuccino A. et al. Superiority of multilevel cervical arthroplasty outcomes versus single-level outcomes: 229 consecutive PCM prostheses. Spine (Phila Pa 1976) 2007;32(12):1337–1344. doi: 10.1097/BRS.0b013e318059af12. [DOI] [PubMed] [Google Scholar]
- 5.Huppert J, Beaurain J, Steib J P. et al. Comparison between single- and multi-level patients: clinical and radiological outcomes 2 years after cervical disc replacement. Eur Spine J. 2011;20(9):1417–1426. doi: 10.1007/s00586-011-1722-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim S W, Limson M A, Kim S B. et al. Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. Eur Spine J. 2009;18(2):218–231. doi: 10.1007/s00586-008-0854-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coric D, Cassis J, Carew J D. et al. Prospective study of cervical arthroplasty in 98 patients involved in 1 of 3 separate investigational device exemption studies from a single investigational site with a minimum 2-year follow-up: clinical article. J Neurosurg Spine. 2010;13(6):715–721. doi: 10.3171/2010.5.SPINE09852. [DOI] [PubMed] [Google Scholar]
- 8.Tu T H, Wu J C, Huang W C. et al. Heterotopic ossification after cervical total disc replacement: determination by CT and effects on clinical outcomes. J Neurosurg Spine. 2011;14(4):457–465. doi: 10.3171/2010.11.SPINE10444. [DOI] [PubMed] [Google Scholar]