Abstract
Osteoarthritis (OA) is one of the most frequently occurring musculoskeletal diseases, posing a significant public health problem due to its impact on pain and disability. Traditional risk factors fail to account for all of the risk observed for OA outcomes. In recent years, our view of disease causation has broadened to include health risks that are created by an individual’s socioeconomic circumstances. Early research into social determinants has focused on social position and explored factors related to the individual such as education, income and occupation. Results from these investigations suggest that low education attainment and nonprofessional occupation are associated with poorer arthritis outcomes. More recently, research has expanded to examine how one’s neighborhood socioeconomic environment may be relevant to OA outcomes. This narrative review proposes a framework to help guide our understanding of how social context may interact with pathophysiological processes and individual-level variables to influence health outcomes in those living with OA.
Keywords: osteoarthritis, sociall determinant, socioeconomic status
Despite the growing capacity of societies to extend life and prevent disease, the disparities in health between and within countries remain ubiquitous and vexing [1–4]. Historically, society has attributed disparities in health and disease to the medical sector. While access to medical care is certainly relevant to one’s health, the literature over the past 15–20 years on the social and environmental influences on people’s health has invariably shown that socioeconomically disadvantaged populations experience worse health outcomes than more affluent populations [5–7]. The disproportionate burden of illness experienced by these populations is a result of structural inequalities reflected in the unequal distribution of power and income, globally and nationally [8,9].
In 1998, the W HO published Social Determinants of Health-The Solid Facts [201], a booklet that presented policy makers, researchers and practitioners with a more holistic approach to views on health that acknowledged the impact of the social environment on health, as represented by social inequalities in health. In 2001, the WHO approved the International Classification of Functioning, Disability and Health (ICF), a framework that synthesizes the medical model of disability with the social model of disability. The ICF conceptual model of disability is innovative in that it recognizes disability as a complex phenomenon that includes the interaction of an individual with features of the social and environmental context [202]. With the creation of the WHO Commission on Social Determinants in 2005, views of disease causation have continued to expand to include discourse on health risks that are created and maintained by the social context above and beyond individual risk factors [10–12].
Early research related to social determinants and health disparities focused on social position and explored downstream determinants primarily related to the individual, such as mechanisms of human biology and the clinical issues of how people cope with disease and disability. Increasingly, research findings have focused on the broader view of upstream determinants related to the community, such as place of residence, work environment or wider social and economic policies of society [10–12].
It is important to focus on social determinants and osteoarthritis (OA) outcomes to advance our understanding of how social context affects health outcomes, particularly in older adults who may experience multiple chronic conditions. OA is one of the most frequently occurring musculoskeletal diseases in western nations, posing a significant public health problem due to its impact on pain, disability and older adults [13–16,203]. Despite the rise in literature on the impact of environment on physical and mental health and functioning of individuals [17–19], the majority of studies have not focused on older adults with OA who may be particularly vulnerable to barriers in their surrounding social and physical environments [20,21]. With the aging of the population worldwide, the prevalence of OA is expected to increase and is likely to result in substantial economic costs for health-care systems. As noted in the recent Institute of Medicine report, Living Well with Chronic Illness: A Call for Public Health Action, although the health of Americans is better now than any other time in history, the gains are not shared by all members of our society [22].
Studies on risk factors of OA have focused on variables at the individual level (e.g., BMI, older age and female gender); however, even after controlling for these individual factors, variation in arthritis prevalence is not completely explained. Evidence exists linking lower levels of individual socioeconomic status (SES) and poorer health outcomes in many diseases [23–27], including arthritis [28–31]. Recent data suggest that the social context (i.e., factors in society that cannot be directly measured at the individual level), or socioeconomic environment of an individual’s neighborhood may be relevant to arthritis prevalence and health outcomes as well. Although studies have focused on how community contexts interact with individual characteristics for individuals with rheumatoid arthritis (R A), systemic lupus erythematosus and self-reported arthritis [32–38], far fewer studies have investigated this relationship with populations of individuals with OA [22,39,40].
Prior research has demonstrated a strong association between SES and numerous health outcomes and several frameworks currently exist that explain the relationship between social determinants and poor health outcomes [41,204]. The most common dimensions used in research as proxies for SES include educational attainment, occupation and income or wealth. We recognize that SES is a complex phenomenon and that there are numerous dimensions of SES that are not captured by these factors; however, it is not within the scope of this paper to discuss this at length. While these measures are interrelated and often combined because they reflect aspects underlying socioeconomic stratification, it remains critical to decompose these measures individually to better understand the specific mechanisms and pathways through which these factors impact specific health outcomes at different stages of the life course, in various populations. Whereas occupation is widely used as a proxy indicator for occupational exposure, social standing, or social networks, education can capture knowledge-related assets of an individual [42] that may affect an individual’s problem-solving abilities or influence values [43]. Within the life course framework, educational attainment can also be a reflection of one’s early life circumstances [44]. Income and wealth are likely to influence health primarily through the transformation of money and assets into health enhancing environments, commodities and services [45], whereby increased income provides access to additional, or higher quality health-promoting resources.
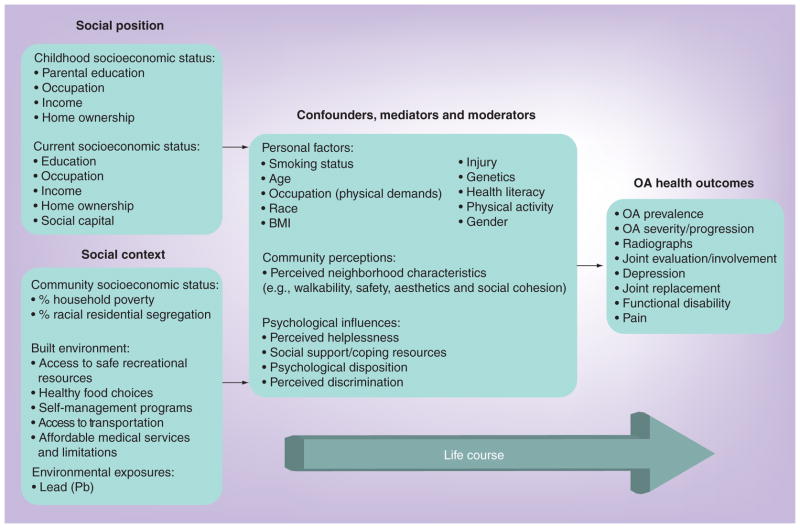
In this narrative review, we apply these general concepts and propose an OA-specific framework to help guide our understanding of how social context and social position may interact with pathophysiological processes and individual-level variables to influence health outcomes in those living with OA (Figure 1). Recognizing that social context has not been extensively researched in OA, our proposed schematic is based on previous models for other chronic diseases and what current research findings in other rheumatologic diseases have demonstrated [22,30,31,38,40,46–49]. We summarize the current literature on research about OA and social determinants including discussion of current measures of social context, social position, and potential mediators and moderators between social determinants and OA outcomes. Our review closes by focusing on future directions and identifying conceptual and methodological limitations in our current knowledge about social determinants and OA, which will contribute to the framework and further elucidate our understanding of the mechanisms of the health–environment relationship.
Figure 1. The relationships between social position, social context and osteoarthritis outcomes.
OA: Osteoarthritis.
OA: definitions & outcomes
Definition of OA
Studies report different measurements of OA. While some studies may use self-reported OA based on questionnaires, radiographic definitions of OA are more common. Studies that measure self-reported arthritis often use the response to a question such as “Have you ever been told by a doctor or nurse that you have any of the following long-term health conditions?”, listing OA as one of the conditions to which respondents are asked to indicate ‘yes’ or ‘no’ [38]. Radiographic definitions are often based on the Kellgren-Lawrence (K-L) scale, which assesses radiographic features of OA such as joint space narrowing and osteophyte development [50,51]. Typically, individuals who score 2 or above on the K-L scale are considered as having radiographic knee OA [50]. Symptomatic OA is defined as the combination of radiographic evidence of OA and self-reported pain in the same joint. Although OA can in theory exist in any joint in the body, it most commonly affects the weight bearing joints such as the hips and knees, but can also frequently affect the hands, feet and spine [52]. In this review, all studies have reported radiographic or symptomatic OA unless otherwise noted.
OA health outcomes
In addition to measuring the prevalence of OA in the general population and assessing severity and progression of OA through radiographs and joint evaluation, recent research has examined physical and psychosocial health outcomes of individuals living with OA (Figure 1). Arthritis is both a leading cause of disability [13] and a frequent source of chronic pain among older adults [53]. Joint change and destruction can often lead to the need for joint replacement surgery [53]. Depressive symptoms are also common among people living with chronic arthritis pain [54,55] and previous studies show that individuals with OA often report an overall lower health-related quality of life [56].
Measures of social determinants
There are several dimensions to measuring social position and social context as they relate to populations with OA (Figure 1). Similar concepts are often composite measures that are aggregated differently depending on the population of interest, or unique aspects of the country of research. In addition to measuring social position and social context, our model also includes a number of mediators, moderators and common confounders, through which social position and social context could affect OA health outcomes. While many aspects of social position and social context can be difficult or impossible to change, understanding mediators and moderators in these associations can provide more easily modifiable opportunities for public health interventions to improve health outcomes.
Social position, compositional effects & individual level measures of SES
Compositional attributes of SES are measured at the individual level and have commonly included variables such as occupation type (professional/managerial versus nonprofessional/nonmanagerial) or occupational grade ranking in Europe, level of educational attainment, income (both individual and household), home ownership, and social class (Figure 1) [57]. Education and occupation tend to be two of the most readily attainable variables. Several studies have examined the relationship between formal education level and rheumatic disease outcomes, particularly in RA [58–64] and to a lesser degree in OA [65,66].
Educational attainment
Lower levels of educational attainment have frequently been associated with the increased prevalence, morbidity and mortality of many chronic diseases [67]. Although it is often used as a proxy for SES, in comparison to income and occupation, educational attainment is unlikely to be changed by disease. Educational attainment has been measured as a continuous variable by the number of years of schooling in studies [65,68]. However, as relatively few individuals in developed countries have received no formal education, or only elementary school education [69], studies often dichotomize levels of schooling at <12 and ≥12 years to represent less than high school or completion of high school and postsecondary education, respectively [22,66,69].
Occupation
In the USA, several studies have measured occupation type based on US census classifications, with self-reported job titles grouped into one of seven occupational groups [22,70] (farming, forestry or fishing; management or professional; fabrication or manual labor; precision production, crafting and repair; service; technology, sales or administration; and military) [205]. These occupational groups are often then classified as nonmanagerial or managerial. The term managerial is intended to imply occupations that tend to include office work, lower physical demand, more control over the pace of one’s work and higher SES, based on census group descriptions.
In other studies measuring occupational classification with arthritis, workers have also been grouped according to the 2000 Standard Occupational Codes in four major occupational groups: white-collar, service, farm and blue-collar [71,72]. Similarly, in Britain, social class quintiles have been used in OA research [73] and are linked to operational categories of the National Statistics Socio-Economic Classif ication (NS-SEC) including: I: higher managerial, administrative and professional occupations; II: managerial and technical occupations; IIIN: skilled occupation-nonmanual; IIIM: skilled occupations-manual; IV: partly skilled occupations; and V: unskilled occupations [74]. Low social class is defined by the residents in households with an economically active head of household in social class IV or V, as a proportion of all residents in households [75]. In a study of prevalence of self-report arthritis in Quebec, researchers measured occupation using the Pineo Porter-McRoberts [76] socioeconomic classification of occupation scale with a total of 16 occupational categories distinguished by their shared attributes in the labor force. Researchers trichotomized these categories into skilled, and semi-skilled or lower scores [77].
Income
Far fewer studies have included income as a measure of SES; Hawker and colleagues created a dichotomized variable of annual household income of ≤$20,000 (Canadian) versus >$20,000 and also created a composite education/income variable to explore the confluence of low educational attainment and low income [69]. The differences in health outcomes by these compositional measures could reflect relatively direct health benefits of having more economic resources (e.g., better nutrition or housing) or unmeasured behavioral psychology variables [78]. The majority of studies examining social position and OA outcomes have focused on an individual’s current SES. The income of one’s parents in addition to an individual’s own income in adulthood can influence health outcomes (Figure 1) [79,80]. To our knowledge, no studies have examined associations of childhood SES, such as parental education, occupation, income or homeownership with the prevalence of OA or OA health outcomes.
Contextual effects & multilevel modeling: individual & community level variables
Social context can be defined as the “social and cultural forces that shape people’s day-to-day experiences and that directly and indirectly affect health and behavior” [81]. Aspects of one’s environment can be either health-promoting or health-damaging [57]. The socioeconomic context of communities may affect characteristics of the environment of communities to which all residents are exposed, regardless of their social position. The complex nature of social context can be described in terms of both physical and social components, as well as their objective (i.e., actual) or subjective (i.e., perceived qualities) and their scale or immediacy to individuals and groups [82].
Community SES
In an Australian study examining the variation in rates of hip and knee joint replacement, SES was derived from the Index of Disadvantage [83]. This index is an area-based measure that represents the average level of disadvantage across a geographical area (i.e., Statistical Local Area) [84] and is a composite of the income, educational attainment, levels of public sector housing, unemployment and jobs in relatively less skilled occupations. These areas are classified into quintiles where 1 indicates an area with significantly disadvantaged households and quintile 5 represents the least disadvantaged households. Another Australian study, examining the association between SES and utilization of primary total hip replacements used postcodes and residential addresses of each subject and matched them to corresponding ABS Census Collection Districts (i.e., 250 households.) [85]. These reference data were then used to determine the Socio Economic Indexes for Areas (SEIFA) value from the census and then the Index of Relative Socioeconomic Disadvantage (IRSD) was applied.
The Townsend Deprivation Score (TDS) is a similar measure of deprivation, which uses census data to enumerate district (i.e., 450 people in 200 households) or ward (i.e., 5500 people in 2400 households) levels and provide a composite score based upon [86]:
The percentage of homes that are not owner-occupied;
The percentage of economically active residents who are unemployed;
The percentage of households that do not have access to a car;
The percentage of households with more than one person per room.
In the USA, studies have used census data to calculate the household poverty rate at the block-group level (i.e., 600–3000 people) [22,40,87], which is the percentage of households with income below the poverty level, as defined by US Census Bureau poverty thresholds. Participants’ physical addresses are geocoded, linked to a block-group identification number, and then used to extract aggregate census information. Poverty level variables can then be categorized, for example, into tertiles: low, medium and high. In studies of self-reported arthritis in Canada, provincial and regional level measures, such as families in a region with low income have been used [46].
Built environment
Previous studies that have examined features of the neighborhood environment have used modified versions of the Home and Community Environment Instrument (HACE) [88], a self-report measure that examines how different environmental domains influence levels of participation, an instrument that has both construct validity and reliability [88]. In studies of individuals with OA, features of the neighborhood environment have examined community mobility barriers (i.e., uneven sidewalks or other walking areas; parks and walking areas that are easy to get to and easy to use; safe parks or walking areas; places to sit and rest at bus stops, in parks, or in other places where people walk; curbs with curb cuts) and transportation facilitators (i.e., public transportation close to home; public transportation with adaptations for people who are limited in their daily activities; and adequate handicap parking, able to drive, have a car available to you at your home) [89,90]. Scores are summed and dichotomized into low barriers (0–1 barrier) and high barriers (2–5 barriers) and high facilitators (4–5 facilitators) and low facilitators (0–3 facilitators), respectively.
While many studies have seen moderate associations between certain occupational activities (e.g., kneeling, squatting and climbing) and the increased risk of knee OA as a result of increased biomechanical loads on the knee joint [91–93], far fewer studies have examined associations of OA with organizational characteristics and policies in the work environment. In one such study, Chen and colleagues asked study participants about work accommodations (i.e., opportunities to switch to physically less demanding jobs; availability for part-time work for people needing reduced time), and benefits (i.e., paid sick leave, short-term or long-term disability payment) [70].
Environmental exposures
Regional differences in OA prevalence may be an indication of physical environmental factors contributing to health outcomes. Early studies suggest that whole blood lead levels are associated with radiographic knee OA [94].
Life course
The life course approach is particularly relevant in understanding the long-term effects of both social position and social context on chronic diseases. Life course measures encompass the aforementioned factors while explicitly including the variable of time, which allows researchers to study disease outcomes across generations and at the individual level beginning from gestation and through childhood, adolescence, young adulthood, middle-age and senescence [95]. Several proposed theoretical models that explain the influence of life course on disease risk may include critical or sensitive periods, which state that exposures during a specific window of time may have long-lasting effects that increase disease risk [96].
While life course is difficult to assess in practice, with most studies measuring life course SES at only two or three time points, there is suggestion that the impact of childhood SES on health decreases over time in adults [97]. Other life course models propose that effects accumulate over the life course, such that increased duration or number of exposures are compounded over time, leading to increased health risk in later years [10]. Although methodological challenges exist in creating summary measures, combinations of the aforementioned indicators (e.g., educational attainment, environmental exposures, occupation type among others) in OA studies would allow researchers to better understand the trajectory and development of OA for an individual over time.
Potential confounders, mediators & moderators between social determinants & OA outcomes
Our model also includes commonly related personal risk factors associated with OA (Figure 1), including smoking status [98], older age [99], female gender [100], occupation-tasks [101–103], BMI (i.e., obesity) [104,105], injury [100], genetics [106,107], race [105] and physical activity [108]. Many of these personal risk factors are also associated with one’s current social position [109]. Although race is not considered a social determinant of health, we have included it in the personal factors in our framework and discussion as it is highly correlated with social position, and a large body of research in OA has explored race as an effect modifier [110–113]. In addition to the more commonly associated risk factors for OA, our figure also includes more proximal mediator and moderators, such as community perceptions and several dimensions of psychological influences (i.e., perceived helplessness, social support/coping resources, psychological disposition, perceived discrimination and/or catastrophizing), that previous research in other rheumatologic conditions or emerging literature in OA have demonstrated to be associated with health outcomes. Including these sets of factors provides for a more transparent relationship to be made linking social determinants to health outcomes, but also allows us to identify areas for public health or behavioral interventions.
While we acknowledge that it is important to recognize individual risk factors associated with OA prevalence and health outcomes, the WHO ICF model also recognizes that attributes beyond an individual affect outcomes. Thus our model of OA health outcomes includes both external, environmental factors, which we refer to as the social context, and internal, personal factors, which are included in our measures of social position and mediators and moderators (Figure 1). This integrated biopsychosocial approach allows us to understand the mechanisms through which distal factors can affect more modifiable, proximal determinants of OA health outcomes.
Studies of social determinants & OA outcomes
Social position & outcomes in knee & hip OA
Significant associations between radiographic and symptomatic knee OA and low educational attainment in the National Health and Nutrition Examination Survey has been reported by Hannan and colleagues [65]. Symptomatic knee pain and self-reported OA remained significantly associated with educational attainment (Table 1), even after adjustment for the risk factors of age, race, BMI, knee injury and occupation. The association between educational attainment and radiographic OA no longer remained significant among women after adjustment for risk factors. A later study of the Johnston County Osteoarthritis Project [66], revealed gender differences as well, such that for men, associations of low educational attainment with radiographic knee OA were explained by age and race, while for women, the association of radiographic OA and low educational attainment persisted after adjusting for smoking status, alcohol use, occupation, knee injury and obesity. Similar to Hannan and colleagues, this study found that symptomatic knee OA was more prevalent in both men and women with limited educational attainment. Significant associations between education and OA of the hip were also noted in the Johnston County Osteoarthritis Study [114].
Table 1.
Studies measuring social position and osteoarthritis health outcomes.
| Study (year) | Type of OA | Social position or social context | Data source/population | Health outcomes | Covariates measured (personal factors) | Outcome | Country | Ref. |
|---|---|---|---|---|---|---|---|---|
| Hannan et al. (1992) | Knee OA radiographs, symptomatic knee pain, self-report arthritis at any site | Educational attainment | National Health and Nutrition Examination Survey | Prevalence of OA | Age, knee injury, race, obesity, occupation | Low educational attainment associated with a high prevalence of knee OA in both men and women, according to all three definitions, known risk factors explain association between educational attainment, although risk factor contributions differ by gender | USA | [65] |
| Hawker et al. (2002) | Self-reported hip and knee OA followed by clinical and radiographic examinations | Educational attainment, income | Mail, telephone survey of persons aged 55 years and older | Potential need for and willingness to consider hip and knee arthroplasty | Age, sex, region of residence | Less education and lower income independently associated with greater likelihood of having potential need for arthroplasty; individuals with less education and/or lower income more likely to have potential unmet need for arthroplasty | Canada | [69] |
| Peters et al. (2005) | Self-reported hip and knee OA, followed by clinical examination | Social class, employment status (self and partner) | Somerset and Avon Survey of Health, community-based, age–sex stratified survey registered in 40 general practices | Change in severity of pain and disability | Sex, age group, BMI, marital status, comorbidities, healthcare utilization | Those reporting greater knee or hip pain had more pain and worse function at follow-up; comorbidities, lower social class, hypertension and higher BMI was associated with greater deterioration | UK | [73] |
| Juhakoski et al. (2008) | Hip OA | Educational level | Rehabilitation clinic in a Finnish Hospital | Self-reported pain and self-reported disease-specific physical function | Age, sex, depression, life satisfaction, smoking, years of sporting activities, radiologic score, BMI, comorbidities, duration of knee pain | Educational level, comorbidities, and BMI significant factors for self-reported pain and physical functioning; no direct relationship with pain and psychological factors detected | Finland | [68] |
| Callahan et al. (2010) | Unilateral and bilateral radiographic and symptomatic knee OA | Educational attainment: number of years of formal education, dichotomized at 12 years | Johnston County Osteoarthritis Project, (NC, USA), African–American and Caucasian men and women aged ≥45 years in rural NC (USA) | Presence of radiographic and symptomatic knee OA | Age, race, gender, smoking status, alcohol use, history of previous knee injury, BMI, occupational characteristics, hormone replacement therapy | Association of low educational attainment with radiographic knee OA explained by age and race, but association with symptomatic knee OA remains after adjustment for covariates; with women, association of low educational attainment with all four knee OA outcomes remain after adjustment; association not explained by current HRT use | USA | [66] |
HRT: Hormone replacement therapy; OA: Osteoarthritis.
Few studies have examined associations between educational attainment and other OA outcomes, such as disability and pain, in hip OA. In a Finnish study conducted in a clinical setting, educational level was identified as a significant factor for self-reported pain and physical function in participants with hip OA [68]. The EUROHIP consortium [115] reported that greater severity of pain, stiffness and physical function symptoms, as measured by the Western Ontario and McMaster Universities (WOMAC) Arthritis Index, was associated with lower levels of educational attainment in a population of patients with hip radiographic OA who were seeking hip replacements. In a study conducted with patients of the Dresden Hip Surgery Registry [116], significant differences in mean gain in WOMAC scores indicated better scores with increasing levels of educational attainment when comparing those who finished school after 12 years to those who ended their education after 8 years; however, beyond 12 years of educational attainment, no significant differences in WOMAC scores were seen. Similar findings were seen in a community-based sample, whereby WOMAC scores were significantly associated with low educational attainment and nonmanagerial occupation in radiographic and symptomatic hip OA, and disability was significantly associated with low educational attainment [22]. Although associations remained even when all SES variables (e.g., educational attainment, occupation and community poverty) were in the model, they were significantly diminished.
A community-based prospective observational study of hip and knee OA conducted in the UK confirmed that individuals in lower social classes were more likely to experience greater deterioration with more severe knee and hip pain and disability at follow-up, while another study conducted in Canada found that individuals with lower levels of educational attainment or lower income were more likely to have potential unmet need for arthroplasty [69].
International studies examining SES and total joint replacement (TJR) have been mixed, but some have demonstrated an association. TJR is a cost-effective elective procedure that is used in severe cases of OA [117]. SES, particularly less education and lower income have been shown to be independently associated with a greater likelihood of having the potential need for TJR [69]. However, those with low SES are less likely to receive a consultation for their OA or TJR [118,119]. Despite having more severe arthritis [69], those with lower SES are often recommended for TJR less frequently [120]. It has been suggested that this may be due to physicians’ perceptions of patients with low SES, which has been shown to be associated with beliefs about abilities, behavioral tendencies and role demands [121]. Further affecting the rates of TJR among those with lower SES is their willingness to consider receiving the procedure. Lower SES, particularly less education, may affect perceived risks of those with lower SES [122] and subsequently influence willingness to receive TJR [123]. Thus, rates of receiving TJR have been consistently associated with SES worldwide, with low rates of TJR amongst those with lower SES in Australia [85], Europe [118,124,125], Canada [119,126] and the USA [127–129]. Furthermore, SES has been associated with higher risk of acute adverse medical events and worse outcomes [124,130,131]. Although SES may play some role in joint replacement, research has shown that the procedure is a complex relationship that involves patient-related factors and issues surrounding equitable access to healthcare service [127].
Social context & outcomes in knee & hip OA
Community SES
To our knowledge, only one study has examined associations of individual level SES and community level SES on the prevalence of radiographic and symptomatic knee OA [40]. This study confirmed previous findings in rheumatology research that neighborhoods have an independent effect on outcomes in arthritis [30,31,46]; independent associations were noted between neighborhoods with higher rates of household poverty and outcomes of knee radiographic OA, bilateral knee radiographic OA and symptomatic knee OA in the Johnston County Osteoarthritis Project (Table 2) [40]. A recent multilevel Australian study using self-report measures of arthritis also found independent associations of neighborhood disadvantage with prevalence of arthritis such that residents of the most disadvantaged neighborhoods were 42% more likely than those in the least disadvantaged neighborhoods to self-report arthritis [38]. Although individual characteristics, such as BMI, educational attainment, and occupation type, have been linked to the risk and prevalence of OA, they do not explain all the variance seen across different geographic regions. Thus, it will be of continued importance to understand how community characteristics (e.g., access to physical activity resources, environmental exposures), beyond poverty, may be linked to the prevalence of disease.
Table 2.
Studies measuring social context and osteoarthritis health outcomes.
| Study (year) | Type of OA | Social position or social context | Data source/population | Health outcomes | Covariates measured (personal factors) | Outcome | Country | Ref. |
|---|---|---|---|---|---|---|---|---|
| Cookson et al. (2007) | Total hip replacement | Townsend deprivation score | Hospital episode statistics, English National Health Service | Elective total hip replacement | Not available | Socioeconomic small area inequality in use of total hip replacement fell between 1991 and 2001 | England | [133] |
| Dixon et al. (2011) | Hip and knee joint | Community socioeconomic status from the Index of Disadvantage, geographic locality, birthplace | National hospital morbidity database | Primary hip or knee joint replacement | Indigenous status, age, gender | Rates of joint replacement were significantly lower in people living in the most disadvantaged and remote areas, people born outside Australia, and indigenous peoples, however knee replacement rates were higher in the most advantaged than in the least disadvantaged areas; hip and knee replacements higher in regional areas than in major cities | Australia | [83] |
| White et al. (2010) | Incident and symptomatic knee OA | Individual environment features | Multicenter osteoarthritis study-knee pain and disability subcohort | Disability in daily activities | Knee pain, functional limitation, comorbidities, BMI, age, gender, educational attainment, ethnicity and study site | Older adults whose neighborhoods did not have parks and walking areas less frequently engaged in a regular fitness program, and in social activities | USA | [90] |
| Chen et al. (2007) | Knee OA | Work-related organizational | Johnston County Osteoarthritis Project, (NC, USA) African–American and Caucasian men and women aged ≥45 years in rural NC (USA) | Prevalence of knee OA | Sociodemographic features, lifestyle factors, knee injuries, BMI, other workplace characteristics | Individuals employed in workplaces offering better policies had significantly less knee symptoms | USA | [70] |
| Nelson et al. (2011) | Radiographic and symptomatic knee OA | Environmental exposure | Johnston County Osteoarthritis Project, (NC, USA), African–American and Caucasian men and women aged ≥45 years in rural NC (USA) | Prevalence and severity of knee OA | Age, race, sex, BMI, smoking, alcohol drinking | Increasing levels of blood lead are statistically significantly associated with radiographic knee OA | USA | [94] |
| Callahan et al. (2011) | Tibiofemoral knee OA | Educational attainment, occupation, community poverty | Johnston County Osteoarthritis Project, (NC, USA), African–American and Caucasian men and women aged ≥45 years in rural NC (USA) | Presence of radiographic and symptomatic knee OA | Age, gender, race, BMI, current smoking status, knee injury and occupational activity score | Low educational attainment was significantly associated with radiographic OA, bilateral OA and symptomatic OA; occupation had no significant independent association beyond educational attainment and community poverty | USA | [40] |
| Knight et al. (2011) | Radiographic and symptomatic hip OA | Educational attainment, occupation type, community poverty | Johnston County Osteoarthritis Project, (NC, USA), African–American and Caucasian men and women aged ≥45 years in rural NC (USA) | Pain and disability | Age, gender, race, BMI, presence of knee symptoms | Pain and disability significantly associated with low educational attainment in radiographic and symptomatic OA; disability additionally associated with and nonmanagerial occupation | USA | [22] |
| Brennan et al. (2012) | Hip OA | Relative Index of Socioeconomic Disadvantage | Australian Orthopaedic Association National Joint Replacement Registry data among residents of the Barwon Statistical Division of Victoria (Australia) | Primary total hip replacement | Age, sex | Rates of total hip replacement are greater for both the most disadvantaged and least disadvantaged groups | Australia | [85] |
| Wills et al. (2012) | Knee OA | BMI across life | British birth cohort of 3035 men and women | Risk of midlife knee OA | Occupation type, activity level at the age of 36 years | Prolonged exposure to high BMI throughout adulthood associated with the highest risk for knee OA with no additional risk conferred from adolescence | UK | [141] |
OA: Osteoarthritis.
The relationship between community-level SES and several OA outcomes has also been examined in the Johnston County Osteoarthritis Project. One study investigating SES factors associated with hip OA found that living in a community with high household poverty rate (>25%) was associated with radiographic hip OA [114]. In another investigation, although Knight and colleagues did not find any association between community poverty and disability among those with radiographic hip OA [22] after adjusting for education and occupation, they did find that individuals with radiographic OA of the knee who lived in areas with poverty rates higher than 25% had higher total WOMAC scores when compared with those living in areas with poverty rates lower than 12%. This association remained strong when other sociodemographic factors were considered [132].
In addition to studying associations with prevalence and physical health outcomes, several studies suggest that social context may contribute to the variations in the utilization of knee and hip replacements (Table 2). Although a 2007 study by Cookson and colleagues in England found that socioeconomic small area inequality in total hip replacement decreased from 1991 and 2001 [133], a recent Australian study reported by Dixon and colleagues noted significant variations in rates of hip and knee joint replacements by community SES [83]. People living in the most disadvantaged and remote areas had more knee, but less hip replacements compared with those who lived in the least advantaged areas. Researchers posit that this variation in knee as compared with hip replacement procedures may result from a greater proportion of individuals from disadvantaged areas being engaged in occupations that involve kneeling, heavy lifting and combined kneeling/squatting and lifting, all of which are known risk factors for knee OA [134].
Built environment
While census and administrative data can be used to capture objective aspects of communities (e.g., poverty rates), descriptive, qualitative data describing an older adult’s community environment (e.g., safe walking areas and even sidewalks) may provide more insight on how neighborhood features may promote mobility or allow adults to remain engaged in daily activities. Older adults often report mobility barriers resulting from features in their community environment [135], however, fewer studies have examined the association of the community environment with disability (Table 2) [136]. Understanding qualitative aspects of the built environment as health enhancing or as perceived barriers to older adults provides information to policy makers that can allow them to more effectively allocate resources at the community level to promote quality of life, enhance mobility and reduce disability in the lives of older adults, particularly those living with OA. A study conducted with a knee pain and disability subcohort of the Multicenter Osteoarthritis Study revealed that walking areas, handicapped parking and public transportation were important features of the neighborhood that affected health outcomes of older adults with functional limitations such that the absence of parks was associated with more reports of disability with social and recreational activities and the presence of handicapped parking was associated with less disability for social, leisure and work role activities [90].
In addition to considerations of neighborhood-level features that may affect health outcomes of those living with OA, the prevalence of knee OA has been examined in conjunction with workplace policies. It was found that individuals employed in workplaces offering better policies (e.g., work accommodations and benefits such as paid sick leave and long-term disability payment) had significantly less knee symptoms compared with those with fewer workplace policies, taking into account age, race, sex, SES, BMI, smoking habit, prior knee injury, frequencies of occupational physical activities, or occupational group [70].
Access to affordable medical services and interventions and access to quality healthcare can be an important determinant of health outcomes in OA [137]. Previous research has shown that among individuals with hip and knee OA, those with lower levels of educational attainment were less likely to receive advice on exercise [138]. A systematic review of evidence on the effectiveness of interventions to improve healthcare quality for disadvantaged populations with OA noted that while several arthritis self-management interventions target disadvantaged populations with OA, there is a dearth of literature on how well these programs work compared with more advantaged population to reduce disparities in care [139].
Environmental exposures
There is strong, consistent evidence in the USA that shows that there is a disproportionate burden of risk to suboptimal unhealthy environmental conditions for those with low SES [140]. Early studies on environmental exposure and OA have suggested that increasing levels of whole blood lead exposure is associated with small but significant increases in the prevalence and severity of radiographic knee OA [94]. It is currently unclear whether or not this association is explained by a direct toxic effect of lead on joint tissues or through an indirect mechanism, however this preliminary research suggests that features of the environment, such as environmental exposure to this toxicant may play some role in mobility and disability in knee OA.
Life course
Although there are no current studies that have examined composition and context over the life course, there is evidence to suggest that BMI, an important risk factor for OA, may have unique effects across the life course. Researchers in the UK examined the relationship between lifetime BMI and midlife knee OA in a population-based British cohort of 3035 men and women with knee OA [141], comparing outcomes of prolonged exposure to high BMI to high BMI at a particular period. Wills and colleagues found that prolonged exposure to high BMI throughout adulthood had a greater influence on the risk of knee OA [141]. Analyses supported an accumulation model of risk indicating that having a high BMI in earlier stages of life was not independently associated with knee OA above and beyond BMI in adulthood. Earlier findings by Macfarlane and colleagues on the association between BMI throughout the life course and adult knee pain found that while association with adult obesity is strongest, associations of high BMI at the age of 11 years was associated with increased risk of knee pain at the age of 45 years [142].
Recent research on life course SES and RA found that patients with R A reported lower childhood SES compared with noncases, with cumulative effects across multiple measures, such as household education, food insecurity and young maternal age [143]. Another study conducted in southern Sweden with patients in an outpatient clinic and private rheumatology clinics assessed perinatal characteristics in relation to the risk of adult RA. High birth weight, initiation of breast feeding during inpatient care after delivery, and paternal occupation were associated with OA indicating that characteristics of the perinatal period may be relevant to the pathogenesis of RA [144]. These findings on the impact of life course BMI and OA and previous research on life course SES and RA suggest that it will also be important to examine social position and social context across the life course in OA health outcomes.
Potential mediators & moderators
Social position and social context most likely affect health outcomes indirectly through other factors such as personal lifestyle, demographic characteristics as well as community perceptions and psychological influences (Figure 1). As social position and aspects of the community are more difficult to intervene upon or impossible to change in adulthood, it is critical to identify and better understand modifiable risk factors, which may be more amenable to intervention in order to eliminate disparities in the prevalence of OA and improve health outcomes of those with OA. As we have previously noted common risk factors associated with OA prevalence, this section will highlight other potential mediators and moderators (Table 3).
Table 3.
Studies measuring mediating or moderating effects and osteoarthritis outcomes.
| Study (year) | Type of OA | Independent variables | Data source/population | Health outcomes | Covariates measured | Outcome | Country | Ref. |
|---|---|---|---|---|---|---|---|---|
| Sandmark et al. (2000) | Knee OA | Job titles and exposure to physical load in occupational work, housework and leisure-time activities | Men and women who had prosthetic surgery due to primary tibiofemoral OA | Development of knee OA leading to prosthetic surgery | Age, BMI, sports, for women: hormone substitution | Among men there was an association between lifting at work, squatting or knee bending, kneeling and jumping with knee OA | Sweden | [146] |
| Allen et al. (2010) | Knee and hip OA | Ten occupational tasks and lifetime exposure to jobs that require spending >50% of their time doing five specific tasks | Johnston County Osteoarthritis Project (NC, USA), African–American and Caucasian men and women aged ≥45 years in rural NC (USA) | Presence of knee and hip OA | Age, race, gender, BMI, prior knee or hip injury, smoking | Radiographic hip and knee OA not significantly associated with any occupational tasks; specific activities associated with symptomatic knee and hip OA; exposure to a greater number of physically demanding occupational tasks at the longest job was associated with greater odds of symptomatic knee and hip OA | USA | [102] |
| Andersen et al. (2012) | Knee and hip OA | Occupations with heavy workload (i.e., farming, construction, healthcare work) | National patient register data on the Danish working population from 1981 to 2006 followed-up for hip and knee OA during 1996–2006 | Increased risk of OA, particularly for women | Age, personal income, personal unemployment, previous knee injury | Male floor layers and bricklayers and male and female healthcare assistants had the highest risk of knee OA; farmers had the highest risk of hip OA; generally, risk increased with cumulative years in the occupation | Denmark | [150] |
| Keysor et al. (2010) | Incident and symptomatic knee OA | Community mobility barriers, transportation facilitators | Multicenter Osteoarthritis Study Knee Pain and Disability subcohort | Disability: DAL and DAF, prevalence of barriers | Age, gender, race, educational attainment, comorbidity, BMI, knee pain, functional limitation and study site | People who reported more transportation facilitators reported less disability, whereas a greater presence of transportation facilitators was not associated with DAF | USA | [89] |
| Martin et al. (2011) | Hip and knee OA | Participant identified community factors | Johnston County Osteoarthritis Project (NC, USA), African–American and Caucasian men and women aged ≥45 years in rural NC (USA) | Facilitators/barriers to OA self-management | Not applicable | Individuals use local recreational facilities, senior centers, shopping centers, religious organizations, medical providers, pharmacies, and their social network for OA management; built environmental characteristics both facilitate and hinder use of community resources for OA management | USA | [39] |
| Ethgen et al. (2004) | Knee and hip OA | Social support | Patients with consecutive hip and knee OA attending an outpatient physical rehabilitation and rheumatology clinic of University Hospital of Liege in Belgium | Health-related quality of life | Age, sex, BMI, number of comorbid conditions, SES, site of survey completion, severity of OA | Greater social companionship transactions associated with higher physical functioning, general health, mental health, social functioning and vitality | Belgium | [166] |
| Kee (2003) | OA | Sociodemographic characteristics (age, race, education, income), psychosocial factors, health promotion practices and social support, health status and pain | Older adults | Psychological equilibrium, physical function | Not available | Hardiness, pain and social support were significant contributors to psychological status and physical function | USA | [168] |
| Rapp et al. (2000) | Knee OA | Pain coping skills | Older adults | Self-reported disability, walking disability | Demographic variables, BMI, medical comorbidities, history of fractures, vision and hearing impairment | Pain coping was significantly associated with disability and distance walked. Less catastrophic thinking and prayer was associated with less disability and better physical function | USA | [171] |
| Keefe et al. (2000) | Knee OA | Gender, catastrophizing | Patients with OA | Pain, pain behavior, physical disability | Age, ethnic background, income, education level, number of years since OA diagnosis, generalized or localized OA, disability and financial compensation or not | Significant difference in pain, pain behavior, and physical disability in men and women, mediated by catastrophizing | USA | [172] |
| Hausmann et al. (2011) | OA | Past perceived discrimination, classism | African–American and white patients treated for OA by orthopedic surgeons in two Veteran Affairs facilities | Affective tone of patient–provider communication | Race, age, annual income, highest educational attainment, whether patient had been seen in the orthopedic clinic previously, quality of life | Perceived racism and classism were reported by more African–American patients than by white patients. High levels of perceived racism among African–American patients was associated with less positive nonverbal affect | USA | [174] |
DAF: Daily activity frequency; DAL: Daily activity limitation; OA: Osteoarthritis; SES: Socioeconomic status.
Personal factors
Occupational tasks
Specific occupational tasks related to radiographic OA and symptomatic OA have not been consistent across studies [145,146]. However, research has consistently shown a strong, positive relationship between work involving knee bending and knee OA in men [147]. Specific occupations however, such as farming, have shown moderate associations with radiographic and symptomatic OA [148], particularly for those who have ten or more years in agricultural work [149]. Far fewer studies have examined the associations of specific occupational tasks with OA of the hip. However, research suggests that prolonged standing at work and heavy lifting increase the risk of degenerative hip disease for farmers [149]. Recent research by Allen and colleagues demonstrated an association between occupational tasks and knee OA (Table 3) [102]. Four specific tasks were associated with symptomatic hip OA: lifting >10 lbs, bending/twisting/reaching, crawling, doing heavy work while standing, as well as the cumulative number of tasks. Additionally, there was an association of lifetime exposure to jobs involving specific occupational tasks with radiographic knee OA, but not radiographic hip OA. However, a Danish study using register data of the whole Danish working population confirmed that occupations with heavy physical workload were associated with a high risk for both hip and knee OA in men and women separately, with risks increasing with cumulative years in occupation (Table 3) [150].
Health literacy
Although health literacy has not yet been explored as a mediator or effect modifier in OA health outcomes, it has been associated with poorer health outcomes in other common chronic diseases [151], such as diabetes [152] and RA [153], as well as in the functional health status among older adults [154]. Swearingen and colleagues analyzed the literacy of 194 consecutive patients at an academic rheumatology clinic using the Rapid Estimate of Adult Literacy in Medicine (REALM) and an ‘Arthritis-Adapted’ REALM (A-REALM) [155]. This study found that more than 10% of patients living with R A for an average of 11 years could not read ‘cartilage’, ‘diagnosis’, ‘rheumatologist’, or ‘symptom’, highlighting the potential for literacy-associated barriers in socioeconomic disparities in rheumatologic health.
Community perceptions
Understanding qualitative aspects of the built environment as health enhancing or as perceived barriers to older adults provides information to policymakers that can allow them to more effectively allocate resources at the community level to promote the quality of life, enhance mobility and reduce disability in the lives of older adults, particularly those living with OA.
Despite the vast body of research that links features of the built environment to physical activity [156–159], research on environmental features as they relate to disabled individuals living with OA, is relatively recent. Keysor and colleagues confirmed the hypothesis that people who reported more mobility barriers and fewer facilitators in the community perceived more limitation in their daily activities [89]. A recent qualitative study with six focus groups in Johnston County (NC, USA), identified community resources and environmental characteristics that are facilitators or barriers to OA disease management [39]. Using the Corbin and Strauss chronic illness trajectory framework, the study divided emergent community resources into three self-management tasks: medical and behavioral management, role management and emotional management. Local area senior and civic centers, a local health facility and aquatics center, community parks and religious organizations were viewed as community resources that promoted physical activity. Social support networks were also used for self-management and to facilitate the completion of daily tasks. The positive benefits of socializing contributed to emotional management of OA. Focus group participants also discussed environmental features in their neighborhood as barriers and facilitators for OA management. Although short distances between residences and community resources promoted physical activity, the availability and quality of lighting, sidewalks and level surfaces could limit one’s ability to engage in physical activity [39]. However, although Martin and colleagues’ research revealed older adults’ recognition of existing neighborhood barriers, Keysor and colleagues found no association with the way people perceived how often daily activities were performed; while features in the neighborhood may make involvement in daily activities difficult, older adults with functional limitations are able to adapt (Table 3) [89].
Psychological influences
Perceived helplessness
Previous research in other rheumatologic conditions has demonstrated an association with helplessness and outcomes [59,160,161]. Early research by Callahan and colleagues confirmed that helplessness mediated a component of the association between formal education level and mortality over 5 years in patients with RA [59]. A recent investigation of patients in the Norfolk Arthritis Registry examined the cross-sectional relationship between SES, learned helplessness, and disease outcome in patients with inflammatory polyarthritis [160]. Camacho and colleagues found that patients with the lowest SES had significantly worse health outcomes compared with patients with the highest SES, a relationship that appeared to be mediated by learned helplessness [160].
Social support/coping resources
An extensive body of research has demonstrated the positive health benefits of social support acting as an appropriate buffer against psychological distress caused by disease [162], particularly for older adult populations [163,164] and in other chronic diseases [165]. In OA, social support has been associated with higher physical functioning, general health, mental health, social functioning and vitality [166–168]. In combination with hardiness and pain, social support accounted for 53 and 54% of the variance in psychological status and physical function, respectively, in older adults with OA [166].
Additional psychosocial factors may explain the variation in self-reports of and disability of those who have OA. Catastrophizing has been conceptualized as both a coping response [169] and a cognitive process in which individuals perceive catastrophic threat, harm or consequences from a stressor (e.g., pain or disability), including negative self-statements and negative predictions about the future. In combination with learned helplessness, Keefe and colleagues demonstrated that levels of catastrophizing were inversely associated with reports of knee pain, disability and psychological distress [170], extending previous research on pain, coping and self-reported disability in older adults [171]. Recent research also found that gender differences in reporting of pain, pain behavior and physical disability were mediated by catastrophizing, even after controlling for depression [172]. A separate study showed that at the end of a 10-week skills intervention focused on providing pain coping skills among older OA patients, the skills training group reported significantly lower levels of pain and psychological disability than the control group [173]. Even at a 6-month follow-up, low catastrophizing scores were associated with better health outcomes.
Perceived discrimination
There is little research on perceived discrimination as it affects OA outcomes. In a recent study by Hausman and associates that examined the impact of perceived discrimination on patient-provider communication, African–Americans reported greater levels of perceived racism and classism [174]. Although Hausman et al. studied patient–provider communication as the outcome, there is reason to believe that the mechanisms of discrimination operate through complex pathways that could ultimately affect both the prevalence of OA in populations, and other OA health outcomes. Additional research is needed to identify the causal pathway through which perceived discrimination can produce negative mental health and induce physiological stress responses.
Conclusion
This article reviews the impact of social determinants on OA outcomes and proposes an OA-specific framework that synthesizes a medical model with a social model of disability. Our narrative review highlights several important components of this topic, including discussion on the current methods of measurement of social determinants at both the individual (i.e., occupation type, educational attainment and/or income) and contextual level (i.e., community-level measures of SES, the built environment and/or environmental exposure), while also identifying potential mediators and moderators that may affect OA health outcomes.
Educational attainment is one of the most investigated measures of social determinants. It has been found to be associated with prevalence of knee and hip OA, as well as markers of disease severity and progression among those with knee and hip OA, including disability, pain and physical function. Other dimensions of social position can be captured through occupation type or measures of income, but vary from study to study, and country to country.
Research on contextual measures of social determinants has demonstrated that living in areas with high community poverty rates is associated with higher rates of self-reported arthritis and higher prevalence of radiographic knee and hip OA and increased disability among those with knee OA. More qualitative, descriptive approaches to capturing contextual environment have included studies on features of the built environment, community perceptions and workplace policies that can be viewed as facilitators or barriers to OA self-management.
We recognize that the mediating, moderating and confounding factors included in our schematic are not an exhaustive list. However, in our review of the literature, we created three categories to reflect conceptual distinctions, including personal factors, community perceptions and psychological influences. As the body of research on social determinants in OA continues to expand, and the measurement of concepts becomes more precise, we expect that additional factors will be added to the model and the mechanisms explaining the relationship between social determinants and OA health outcomes to be better explicated.
Future perspective
In reviewing the existing literature on social determinants of OA, it is important to identify gaps in the literature and areas in need of future research in order to reach out to decision-makers and guide the development of health promoting policies that reduce the disparities seen in OA and other chronic diseases. Our paper has identified several factors of interest and provided rationale as to how they may potentially affect OA health outcomes, most of which have largely been unexplored. These include: social cohesion/social capital, environmental exposure, neighborhood environment (perceived and actual), health literacy, perceived discrimination; and life course. We encourage researchers to consider our proposed schematic in their future studies and develop their research around these factors to help build and strengthen our understanding of the complex causal linkages that underlie disparities in OA health outcomes.
While there is strong evidence for individual SES/compositional effects on prevalence and outcomes of OA, most studies have focused primarily on educational attainment and occupation type. The inclusion of more studies examining the association of income or wealth might provide more understanding on the conversion of assets and money into health-enhancing commodities, environments and services. Measurement of social phenomena and other aggregate constructs in social determinants at both the individual level and particularly at the group level remain underdeveloped [175]. Definitions of occupation type, community poverty and deprivation often vary from study to study and country to country. Thus, we encourage continued conceptualization in the development of valid measures that would allow for the comparison of data across countries and improvement in methodological approaches and study designs that can better capture dimensions of social position and social context. In particular, additional research is needed to determine if aggregate-level measures of SES are providing accurate estimations of individual SES as well as determining if there are specific populations where SES measures should be measured contextually or individually.
More research, particularly multilevel modeling, is needed. Although there is evidence linking social context and individual SES in other chronic conditions, there is little research regarding how community contexts can interact with individual-level characteristics in OA. Using the ICF conceptual model of disability as a framework for research in OA requires adequate consideration of the complex relationship of individuals within their social and environmental context [202]. In particular, greater use of multilevel models in OA and determinants research will better allow us to understand how populations interact with aggregate phenomena (i.e., community poverty) and change over time.
With a growing aging population, and one that lives longer, the life course perspective will allow researchers to understand trends within chronic diseases and understand trajectories of illness over time. Currently, no studies have explored the role of social determinants across the life course and OA.
Although radiographic assessment of OA is considered the gold standard, some studies on OA still use self-report as their measure of disease. A movement towards radiographic, clinical assessment as compared with self-report is needed to improve accuracy and comparability between studies. Additionally, there has been a large focus on OA of the knee and hip. More research is needed to assess the effects of social determinants on other types of OA, including the hands, spine and feet.
With the exception of the Johnston County Osteoarthritis Study, which has enrolled a sizeable number of African–Americans, most research investigating the effect of social determinants on OA outcomes has focused primarily on Caucasian populations. Future research needs to be carried out to determine whether OA outcomes have similar associations with SES among different racial and ethnic groups/settings, different cultures, developing countries and older adults. In closing, it is of continued importance to focus on social determinants and OA outcomes in order to advance our understanding of how social context affects health outcomes. Identifying potential mediators, such as social support or psychological disposition, which are proximal to OA health outcomes, may provide public health practitioners with more accessible opportunities to develop health interventions to improve the quality of life of those living with OA. However, we emphasize that only through understanding the mechanisms of distal, social determinants can we expect to truly affect the structural inequalities that underlie the disproportionate burden of illness.
Executive summary.
Overview
Early research related to social determinants and health disparities focused on social position and explored downstream determinants primarily related to the individual, such as mechanisms of human biology and the clinical issues of how people cope with disease and disability. Over the past 15–20 years, our view of disease causation has broadened to include discourse on the health risks that are created and maintained by the social context above and beyond individual risk factors.
This review proposes a framework to help guide our understanding of how social context may interact with pathophysiological processes and individual-level variables to influence health outcomes in those living with osteoarthritis (OA). Our schematic is based on previous models for chronic disease and what current research findings in other rheumatologic diseases have demonstrated.
We summarize the current literature on research on OA and social determinants, focus on future directions for research, and identify conceptual and methodological limitations in our current knowledge about social determinants and OA.
Social determinants & OA outcomes
Education and occupation are the compositional measures of socioeconomic status (SES) that have been examined most extensively in OA.
Low educational attainment and/or having a nonmanagerial/nonprofessional occupation have been demonstrated to be associated with increased OA prevalence and morbidity (poor health outcomes), after adjusting for other known risk factors (gender, BMI, injury, and age).
In the limited studies to date, social context (percentage of the neighborhood living in poverty) has been shown to be associated with OA outcomes, independent of individual measures of SES.
Conclusion & future perspective
Due to the complex nature of community variables often referred to as social context, better and more consistent definitions of this measure need to be developed.
-
Research on the effects of social determinants on OA outcomes has focused primarily on education and occupation type. Definitions of SES need to be expanded to include other measures that will address methodological issues in defining social determinants, including:
Social cohesion/social capital
Environmental exposure
Neighborhood factors (actual and perceived)
Health literacy
Perceived discrimination
Life course
Income
Most research investigating the effect of social determinants on OA outcomes has focused primarily on Caucasian populations. Future research needs to be carried out to determine if OA outcomes have similar associations with SES among different racial and ethnic groups/settings, different cultures, developing countries and older adults.
Footnotes
For reprint orders, please contact: reprints@futuremedicine.com
Financial & competing interests disclosure
The authors would like to acknowledge the support received for their research on social determinants and osteoarthritis from the National Institute of Arthritis and Musculoskeletal Skin Diseases (NIAMS) grant numbers RO1-AR-053-989-01, 5-P60-AR-30701 and 5-P60-AR49465. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
• of interest
•• of considerable interest
- 1.Pickett K, Wilkinson R. The Spirit Level: Why Greater Equality Makes Societies Stronger. Bloomsbury Press; NY, USA: 2009. [Google Scholar]
- 2.Evans T, Whitehead M, Diderichsen F, Bhuiya A, Wirth M. In: Challenging Inequities in Health: From Ethics to Action. Evans T, Whitehead M, Diderichen F, Bhuiya A, Wirth M, editors. Oxford University Press; Oxford, UK: 2001. [Google Scholar]
- 3.Marmot M, Wilkinson RG. Social Determinants of Health. Oxford University Press; Oxford, UK: 1999. [Google Scholar]
- 4.Wilkinson RG. Unhealthy Societies: The Afflictions of Inequality. Routledge; NY, USA: 1996. [Google Scholar]
- 5.Dalstra JA, Kunst AE, Borrell C, et al. Socioeconomic differences in the prevalence of common chronic diseases: an overview of eight European countries. Int J Epidemiol. 2005;34(2):316–326. doi: 10.1093/ije/dyh386. [DOI] [PubMed] [Google Scholar]
- 6.Huisman M, Kunst AE, Bopp M, et al. Educational inequalities in cause-specific mortality in middle-aged and older men and women in eight western European populations. Lancet. 2005;365(9458):493–500. doi: 10.1016/S0140-6736(05)17867-2. [DOI] [PubMed] [Google Scholar]
- 7.Kunst AE, Bos V, Lahelma E, et al. Trends in socioeconomic inequalities in self-assessed health in 10 European countries. Int J Epidemiol. 2005;34(2):295–305. doi: 10.1093/ije/dyh342. [DOI] [PubMed] [Google Scholar]
- 8.Subramanian S, Kawachi I. Income inequality and health: what have we learned so far? Epidemiol Rev. 2004;26(1):78–91. doi: 10.1093/epirev/mxh003. [DOI] [PubMed] [Google Scholar]
- 9.Wilkinson RG, Pickett KE. Income inequality and population health: a review and explanation of the evidence. Soc Sci Med. 2006;62(7):1768–1784. doi: 10.1016/j.socscimed.2005.08.036. [DOI] [PubMed] [Google Scholar]
- 10.Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31(2):285–293. [PubMed] [Google Scholar]
- 11.Frohlich KL, Corin E, Potvin L. A theoretical proposal for the relationship between context and disease. Soc Health Illness. 2001;23(6):776–797. [Google Scholar]
- 12.Adler NE, Stewart J. The biology of disadvantage: socioeconomic status and health. Ann NY Acad Sci. 2010;1186:1–275. doi: 10.1111/j.1749-6632.2009.05385.x. [DOI] [PubMed] [Google Scholar]
- 13.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murphy L, Schwartz TA, Helmick CG, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. 2008;59(9):1207–1213. doi: 10.1002/art.24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lubar D, White PH, Callahan LF, et al. A national public health agenda for osteoarthritis 2010. Semin Arthritis Rheum. 2011;39(5):323–326. doi: 10.1016/j.semarthrit.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 16.Murphy LB, Hootman JM, Langmaid GA, Brady TJ, Al E. Prevalence of doctor-diagnosed arthritis and arthritis-attributable effects among Hispanic adults, by Hispanic subgroup – United States, 2002, 2003, 2006, and 2009. MMWR. 2011;60(6):167–171. [PubMed] [Google Scholar]
- 17.Yen IH, Syme SL. The social environment and health: a discussion of the epidemiological literature. Annu Rev Public Health. 1999;20:287–308. doi: 10.1146/annurev.publhealth.20.1.287. [DOI] [PubMed] [Google Scholar]
- 18.Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Commun Health. 2001;55(2):111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glass TA, Balfour JL. Neighborhoods, aging and functional limitations. In: Kawachi I, Berkman LF, editors. Neighborhoods and Health. Oxford University Press; NY, USA: 2003. pp. 303–334. [Google Scholar]
- 20.Robert SA, Li LW. Age variation in the relationship between community socioeconomic status and adult health. Res Aging. 2001;23(2):234–259. [Google Scholar]
- 21.Wahl H-W, Lang FF. Aging in context across the adult life course: integrating physical and social environmental research perspectives. Ann Rev Gerontol Geriatr. 2003;23:1–33. [Google Scholar]
- 22•.Knight JB, Callahan LF, Luong MLN, et al. The association of disability and pain with individual and community socioeconomic status in people with hip osteoarthritis. Open Rheumatol J. 2011;5:51–58. doi: 10.2174/1874312901105010051. Confirms the association between individual-level socioeconomic status measures of education and occupation with disability and pain in those with hip osteoarthritis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adler NE, Marmot M, McEwen BS, Steyaert J. Socioeconomic status and health in industrial nations: social, psychological, and biological pathways. Ann N Y Acad Sci. 1999;1186:1–4. [PubMed] [Google Scholar]
- 24.House JS, Williams DR. Understanding and reducing socioeconomic and racial/ethnic disparities in health. In: Smedley BD, Syme SL, editors. Promoting Health: Intervention Strategies from Social and Behavioral Research. National Academy Press; DC, USA: 2000. [Google Scholar]
- 25.Taylor SE, Repetti RL, Seeman T. Health psychology: what is an unhealthy environment and how does it get under the skin? Annu Rev Psychol. 1997;48:411–447. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- 26.Mackenbach JP, Howden-Chapman P. New perspectives on socioeconomic inequalities in health. Perspect Bio Med. 2003;46:428–444. doi: 10.1353/pbm.2003.0039. [DOI] [PubMed] [Google Scholar]
- 27.Marmot M. Epidemiology of socioeconomic status and health: are determinants within countries the same as between countries? Ann NY Acad Sci. 1999;896:16–29. doi: 10.1111/j.1749-6632.1999.tb08102.x. [DOI] [PubMed] [Google Scholar]
- 28.Jordan JM, Callahan LF. Community and environmental factors and arthritis outcomes. N C Med J. 2007;68(6):439–443. [PubMed] [Google Scholar]
- 29.Callahan LF, Shreffler J, Mielenz T, et al. Health-related quality of life in adults from 17 family practice clinics in North Carolina. Preven Chronic Dis. 2009;6(1):A05. [PMC free article] [PubMed] [Google Scholar]
- 30.Callahan LF, Shreffler J, Mielenz T, et al. Arthritis in the family practice setting: associations with education and community poverty. Arthritis Care Res. 2008;59(7):1002–1008. doi: 10.1002/art.23834. [DOI] [PubMed] [Google Scholar]
- 31.Callahan LF, Martin KR, Shreffler J, et al. Independent and combined influence of homeownership, occupation, education, income, and community poverty on physical health in persons with arthritis. Arthritis Care Res. 2011;63(5):643–653. doi: 10.1002/acr.20428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harrison MJ, Tricker KJ, Davies L, et al. The relationship between social deprivation, disease outcome measures, and response to treatment in patients with stable, longstanding rheumatoid arthritis. J Rheumatol. 2005;32(12):2330–2336. [PubMed] [Google Scholar]
- 33.Margaretten M, Barton J, Julian L, et al. Socioeconomic determinants of disability and depression in patients with with rheumatoid arthritis. Arthritis Care Res. 2011;63:240–246. doi: 10.1002/acr.20345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liao KP, Alfredsson L, Karlson EW. Environmental influences on risk for rheumatoid arthritis. Curr Opin Rheumatol. 2009;21(3):279–283. doi: 10.1097/BOR.0b013e32832a2e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martin KR, Schoster B, Shreffler J, Meier A, Callahan LF. Perceived barriers to physical activity among North Carolinians with arthritis: findings from a mixed-methodology approach. N C Med J. 2007;68(6):404–412. [PubMed] [Google Scholar]
- 36.Martin KR, Shreffler J, Schoster B, Callahan LF. Associations of perceived neighborhood environment on health status outcomes in persons with arthritis. Arthritis Care Res. 2010;62(11):1602–1611. doi: 10.1002/acr.20267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trupin LS, Tonner MC, Yazdany J, et al. The role of neighborhood and individual socioeconomic status in outcomes of systemic lupus erythematosus. J Rheumatol. 2008;35(9):1782–1788. [PMC free article] [PubMed] [Google Scholar]
- 38.Brennan S, Turrell G. Neighborhood disadvantage, individual-level socioeconomic position, and self-reported chronic arthritis: a cross-sectional multilevel study. Arthritis Care Res. 2012;64(5):721–728. doi: 10.1002/acr.21590. [DOI] [PubMed] [Google Scholar]
- 39•.Martin KR, Schoster B, Woodard JC, Callahan LF. What community resources do older community-dwelling adults use to manage their osteoarthritis? A formative examination. J Appl Gerontol. 2011 doi: 10.1177/0733464810397613. (Epub ahead of print). Qualitative study that explores community resources for osteoarthritis self-management. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40•.Callahan LF, Cleveland RJ, Shreffler J, et al. Associations of educational attainment, occupation and community poverty with knee osteoarthritis in the Johnston County (North Carolina) osteoarthritis project. Arthritis Res Ther. 2011;13(5):R169. doi: 10.1186/ar3492. Population-based study that examines community and individual-level socioeconomic status indicators with the presence of knee osteoarthritis after adjusting for known risk factors. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.WHO. Environment and Health Risks: a Review of the Influence and Effects of Social Inequalities. WHO; Geneva, Switzerland: 2010. pp. 1–262. [Google Scholar]
- 42.Lynch JW, Kaplan GA. Socioeconomic position. In: Berkman L, Kawachi I, editors. Social Epidemiology. Oxford University Press; Oxford, UK: 2000. pp. 13–35. [Google Scholar]
- 43.Liberatos P, Link BG, Kelsey JL. The measurement of social class in epidemiology. Epidemiol Rev. 1988;10(1):87–121. doi: 10.1093/oxfordjournals.epirev.a036030. [DOI] [PubMed] [Google Scholar]
- 44.Beebe-Dimmer J, Lynch JW, Turrell G, Lustgarten S, Raghunathan T, Kaplan GA. Childhood and adult socioeconomic conditions and 31-year mortality risk in women. Am J Epidemiol. 2004;159(5):481–490. doi: 10.1093/aje/kwh057. [DOI] [PubMed] [Google Scholar]
- 45.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Smith GD. Indicators of socioeconomic position (part 1) J Epidemiol Commun Health. 2006;60(1):7–12. doi: 10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cañizares M, Power JD, Perruccio AV, Badley EM. Association of regional racial/cultural context and socioeconomic status with arthritis in the population: a multilevel analysis. Arthritis Care Res. 2008;59(3):399–407. doi: 10.1002/art.23316. [DOI] [PubMed] [Google Scholar]
- 47.Brown AF, Ang A, Pebley AR. The relationship between neighborhood characteristics and self-rated health for adults with chronic conditions. Am J Public Health. 2007;97(5):926–932. doi: 10.2105/AJPH.2005.069443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Freedman VA, Grafova IB, Rogowski J. Neighborhoods and chronic disease onset in later life. Am J Public Health. 2011;101(1):79. doi: 10.2105/AJPH.2009.178640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Menec VH, Shooshtari S, Nowicki S, Fournier S. Does the relationship between neighborhood socioeconomic status and health outcomes persist into very old age? A population-based study. J Aging Health. 2010;22(1):27–47. doi: 10.1177/0898264309349029. [DOI] [PubMed] [Google Scholar]
- 50.Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kellgren JH, Lawrence JS, editors. The Epidemiology of Chronic Rheumatism, Atlas of Standard Radiographs. Blackwell Scientific; Oxford, UK: 1963. p. 2. [Google Scholar]
- 52.Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 53.Felson DT, Zhang Y. An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum. 1998;41(8):1343–1355. doi: 10.1002/1529-0131(199808)41:8<1343::AID-ART3>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 54.Bookwala J, Harralson TL, Parmelee PA. Effects of pain on functioning and well-being in older adults with osteoarthritis of the knee. Psychol Aging. 2003;18(4):844–850. doi: 10.1037/0882-7974.18.4.844. [DOI] [PubMed] [Google Scholar]
- 55.Creamer P, Lethbridge-Cejku M, Hochberg M. Determinants of pain severity in knee osteoarthritis: effect of demographic and psychosocial variables using 3 pain measures. J Rheumatol. 1999;26(8):1785–1792. [PubMed] [Google Scholar]
- 56.Burckhardt CS. The impact of arthritis on quality of life. Nurs Res. 1985;34(1):11–16. [PubMed] [Google Scholar]
- 57.Oakes JM, Kaufman JS. In: Methods in Social Epidemiology. Oakes JM, Kaufman JS, editors. Wiley; CA, USA: 2006. [Google Scholar]
- 58.Pincus T, Callahan LF. Formal education as a marker for increased mortality and morbidity in rheumatoid arthritis. J Chronic Dis. 1985;38(12):973–984. doi: 10.1016/0021-9681(85)90095-5. [DOI] [PubMed] [Google Scholar]
- 59.Callahan LF, Cordray DS, Wells G, Pincus T. Formal education and five-year mortality in rheumatoid arthritis: mediation by helplessness scale scores. Arthritis Rheum. 1996;9(6):463–472. doi: 10.1002/art.1790090608. [DOI] [PubMed] [Google Scholar]
- 60.Callahan LF, Pincus T. Formal education level as a significant marker of clinical status in rheumatoid arthritis. Arthritis Rheum. 1988;31(11):1346–1357. doi: 10.1002/art.1780311102. [DOI] [PubMed] [Google Scholar]
- 61.Jacobi CE, Mol GD, Boshuizen HC, Rupp I, Dinant HJ, Van Den Bos GA. Impact of socioeconomic status on the course of rheumatoid arthritis and on related use of health care services. Arthritis Rheum. 2003;49(4):567–573. doi: 10.1002/art.11200. [DOI] [PubMed] [Google Scholar]
- 62.Bengtsson C, Nordmark B, Klareskog L, Lundberg I, Alfredsson L. Socioeconomic status and the risk of developing rheumatoid arthritis: results from the Swedish EIRA study. Ann Rheum Dis. 2005;64(11):1588–1594. doi: 10.1136/ard.2004.031666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pedersen M, Jacobsen S, Klarlund M, Frisch M. Socioeconomic status and risk of rheumatoid arthritis: a Danish case-control study. J Rheumatol. 2006;33(6):1069–1074. [PubMed] [Google Scholar]
- 64.Leigh JP, Fries JF. Education level and rheumatoid arthritis: evidence from five data centers. J Rheumatol. 1991;18(1):24–34. [PubMed] [Google Scholar]
- 65.Hannan MT, Anderson JJ, Pincus T, Felson DT. Educational attainment and osteoarthritis: differential associations with radiographic changes and symptom reporting. J Clin Epidemiol. 1992;45(2):139–147. doi: 10.1016/0895-4356(92)90006-9. [DOI] [PubMed] [Google Scholar]
- 66.Callahan L, Shreffler J, Siaton B, et al. Limited educational attainment and radiographic and symptomatic knee osteoarthritis: a cross-sectional analysis using data from the Johnston County (North Carolina) Osteoarthritis Project. Arthritis Res Ther. 2010;12(2):R46. doi: 10.1186/ar2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.IOM (Institute of Medicine) Living Well with Chronic Illness: A Call for Public Health Action. The National Academies Press; Washington, DC, USA: 2012. [Google Scholar]
- 68•.Juhakoski R, Tenhonen S, Anttonen T, Kauppinen T, Arokoski JP. Factors affecting self-reported pain and physical function in patients with hip osteoarthritis. Arch Phys Med Rehabil. 2008;89(6):1066–1073. doi: 10.1016/j.apmr.2007.10.036. Finnish study confirming educational level and life satisaction as significant factors for self-reported pain and physical functioning in those with hip osteoarthritis. [DOI] [PubMed] [Google Scholar]
- 69.Hawker GA, Wright JG, Glazier RH, et al. The effect of education and income on need and willingness to undergo total joint arthroplasty. Arthritis Rheum. 2002;46(12):3331–3339. doi: 10.1002/art.10682. [DOI] [PubMed] [Google Scholar]
- 70.Chen JC, Linnan L, Callahan LF, Yelin EH, Renner JB, Jordan JM. Workplace policies and prevalence of knee osteoarthritis: the Johnston County Osteoarthritis Project. Occup Environ Med. 2007;64(12):798–805. doi: 10.1136/oem.2006.030148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Krieger N, Barbeau EM, Soobader MJ. Class matters: US versus UK measures of occupational disparities in access to health services and health status in the 2000 US National Health Interview Survey. Int J Health Ser. 2005;35(2):213–236. doi: 10.2190/JKRE-AH92-EDV8-VHYC. [DOI] [PubMed] [Google Scholar]
- 72.Caban-Martinez AJ, Lee DJ, Fleming LE, et al. Arthritis, occupational class, and the aging US workforce. Am J Public Health. 2011;101(9):1729–1734. doi: 10.2105/AJPH.2011.300173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Peters TJ, Sanders C, Dieppe P, Donovan J. Factors associated with change in pain and disability over time: a community-based prospective observational study of hip and knee osteoarthritis. Br J General Pract. 2005;55(512):205–211. [PMC free article] [PubMed] [Google Scholar]
- 74.Chandola T, Jenkinson C. The new UK national statistics socio-economic classification (NS-SEC); investigating social class differences in self-reported health status. J Public Health. 2000;22(2):182–190. doi: 10.1093/pubmed/22.2.182. [DOI] [PubMed] [Google Scholar]
- 75.Morgan O, Baker A. Measuring deprivation in England and Wales using 2001 Carstairs scores. Health Stat Q. 2006;31:28–33. [PubMed] [Google Scholar]
- 76.Pineo PC, Porter J, McRoberts HA. The 1971 census and the socioeconomic classification of occupations. Can Rev Sociol Anthropol. 1977;14:91–102. [Google Scholar]
- 77.Wang PP, Badley EM. Consistent low prevalence of arthritis in Quebec: findings from a provincial variation study in Canada based on several canadian population health surveys. J Rheumatol. 2003;30(1):126–131. [PubMed] [Google Scholar]
- 78.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- 79.Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical channges and interdisciplinary perspectives. Int J Epidemiol. 2002;34(2):481–482. [PubMed] [Google Scholar]
- 80.Lynch J, Due P, Muntaner C, Smith GD. Social capital – is it a good investment strategy for public health? J Epidemiol Commun Health. 2000;54(6):404–408. doi: 10.1136/jech.54.6.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pasick RJ, Burke NJ. A critical review of theory in breast cancer screening promotion across cultures. Ann Rev Public Health. 2008;29:351–368. doi: 10.1146/annurev.publhealth.29.020907.143420. [DOI] [PubMed] [Google Scholar]
- 82.Burke NJ, Joseph G, Pasick RJ, Barker JC. Theorizing social context: rethinking behavioral theory. Health Educ Behav. 2009;36(Suppl 5):S55–S70. doi: 10.1177/1090198109335338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dixon T, Urquhart DM, Berry P, et al. Variation in rates of hip and knee joint replacement in Australia based on socioeconomic status, geographical locality, birthplace and indigenous status. ANZ J Surg. 2011;81:26–31. doi: 10.1111/j.1445-2197.2010.05485.x. [DOI] [PubMed] [Google Scholar]
- 84.Trewin D. Statistical Geography Volume 1-Australian Standard Geographical Classification (ASGC) Australian Bureau of Statistics; Canberra, Australia: [Google Scholar]
- 85.Brennan SL, Stanford T, Wluka AE, et al. Cross-sectional analysis of association between socioeconomic status and utilization of primary total hip joint replacements 2006–7: Australian Orthopaedic Association National Joint Replacement Registry. BMC Musculoskelet Disord. 2012;13(1):63. doi: 10.1186/1471-2474-13-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Townsend P. Deprivation. J Soc Pol. 1987;16(2):125–146. [Google Scholar]
- 87.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian S, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (US) J Epidemiol Commun Health. 2003;57(3):186–199. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Keysor J, Jette A, Haley S. Development of the home and community environment (HACE) instrument. J Rehabil Med. 2005;37(1):37–44. doi: 10.1080/16501970410014830. [DOI] [PubMed] [Google Scholar]
- 89•.Keysor JJ, Jette AM, Lavalley MP, et al. Community environmental factors are associated with disability in older adults with functional limitations: the MOST study. J Gerontol Series A Biol Sci Med Sci. 2010;65(4):393. doi: 10.1093/gerona/glp182. New evidence addressing the environment–disability link in community-dwelling adults with symptomatic knee osteoarthritis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90•.White DK, Jette AM, Felson DT, et al. Are features of the neighborhood environment associated with disability in older adults? Disabil Rehabil. 2010;32(8):639–645. doi: 10.3109/09638280903254547. Exploratory study confirming that features of the environment are associated with disability in older adults. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Manninen P, Heliovaara M, Riihimaki H, Suomalainen O. Physical workload and the risk of severe knee osteoarthritis. Scand J Work Environ Health. 2002;28(1):25–32. doi: 10.5271/sjweh.643. [DOI] [PubMed] [Google Scholar]
- 92.Coggon D, Croft P, Kellingray S, Barrett D, Mclaren M, Cooper C. Occupational physical activities and osteoarthritis of the knee. Arthritis Rheum. 2000;43(7):1443–1449. doi: 10.1002/1529-0131(200007)43:7<1443::AID-ANR5>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 93.Vrezas I, Elsner G, Bolm-Audorff U, Abolmaali N, Seidler A. Case-control study of knee osteoarthritis and lifestyle factors considering their interaction with physical workload. Int Arch Occupat Environ Health. 2010;83(3):291–300. doi: 10.1007/s00420-009-0486-6. [DOI] [PubMed] [Google Scholar]
- 94.Nelson AE, Shi XA, Schwartz TA, et al. Whole blood lead levels are associated with radiographic and symptomatic knee osteoarthritis: a cross-sectional analysis in the Johnston County Osteoarthritis Project. Arthritis Res Ther. 2011;13(2):R37. doi: 10.1186/ar3270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Smith GD, Lynch J. Life course approaches to socioeconomic differentials in health. Life Course Approach Chronic Dis Epidemiol. 2004;2:77–115. [Google Scholar]
- 96.Kuh D, Ben-Shlomo Y. A Life Course Approach Chronic Disease Epidemiology. Vol. 2. Oxford University Press; USA: 2004. [Google Scholar]
- 97.Power C, Hertzman C. Social and biological pathways linking early life and adult disease. Br Med Bull. 1997;53(1):210–221. doi: 10.1093/oxfordjournals.bmb.a011601. [DOI] [PubMed] [Google Scholar]
- 98.Felson DT, Anderson JJ, Naimark A, Hannan MT, Kannel WB, Meenan RF. Does smoking protect against osteoarthritis? Arthritis Rheum. 1989;32(2):166–172. doi: 10.1002/anr.1780320209. [DOI] [PubMed] [Google Scholar]
- 99.Felson DT, Zhang Y, Hannan MT, et al. Risk factors for incident radiographic knee osteoarthritis in the elderly The Framingham Study. Arthritis Rheum. 1997;40(4):728–733. doi: 10.1002/art.1780400420. [DOI] [PubMed] [Google Scholar]
- 100.Blagojevic M, Jinks C, Jeffery A, Jordan K. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2010;18(1):24–33. doi: 10.1016/j.joca.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 101.Holte HH, Tambs K, Bjerkedal T. Manual work as predictor for disability pensioning with osteoarthritis among the employed in Norway 1971–1990. Int J Epidemiol. 2000;29(3):487–494. [PubMed] [Google Scholar]
- 102.Allen KD, Chen JC, Callahan LF, et al. Associations of occupational tasks with knee and hip osteoarthritis: the Johnston County Osteoarthritis Project. J Rheumatol. 2010;37(4):842–850. doi: 10.3899/jrheum.090302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Klussmann A, Gebhardt H, Nübling M, et al. Research article Individual and occupational risk factors for knee osteoarthritis: results of a case-control study in Germany. Arthritis Res Ther. 2010;12(3):R88. doi: 10.1186/ar3015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kellgren J, Lawrence J. Osteo-arthrosis and disk degeneration in an urban population. Ann Rheum Dis. 1958;17(4):388–397. doi: 10.1136/ard.17.4.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first national Health and Nutrition Examination Survey (HANES I) Am J Epidemiol. 1988;128(1):179–189. doi: 10.1093/oxfordjournals.aje.a114939. [DOI] [PubMed] [Google Scholar]
- 106.Pollard T, Batra R, Judge A, et al. Genetic predisposition to the presence and 5-year clinical progression of hip osteoarthritis. Osteoarthritis Cartilage. 2012;20(5):368–375. doi: 10.1016/j.joca.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 107.Spector TD, Cicuttini F, Baker J, Loughlin J, Hart D. Genetic influences on osteoarthritis in women: a twin study. BMJ. 1996;312(7036):940–943. doi: 10.1136/bmj.312.7036.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cheng Y, Macera CA, Davis DR, Ainsworth BE, Troped PJ, Blair SN. Physical activity and self-reported, physician-diagnosed osteoarthritis: is physical activity a risk factor? J Clin Epidemiol. 2000;53(3):315–322. doi: 10.1016/s0895-4356(99)00168-7. [DOI] [PubMed] [Google Scholar]
- 109.Berkman LF, Kawachi I. Social Epidemiology. Oxford University Press; NY, USA: 2000. [Google Scholar]
- 110.Jordan JM, Helmick CG, Renner JB, et al. Prevalence of hip symptoms and radiographic and symptomatic hip osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2009;36(4):809–815. doi: 10.3899/jrheum.080677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Braga L, Renner J, Schwartz T, et al. Differences in radiographic features of knee osteoarthritis in African–Americans and Caucasians: the Johnston County Osteoarthritis Project. Osteoarthritis Cartilage. 2009;17(12):1554–1561. doi: 10.1016/j.joca.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Allen KD, Helmick CG, Schwartz TA, Devellis RF, Renner JB, Jordan JM. Racial differences in self-reported pain and function among individuals with radiographic hip and knee osteoarthritis: the Johnston County Osteoarthritis Project. Osteoarthritis Cartilage. 2009;17(9):1132–1136. doi: 10.1016/j.joca.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Nelson AE, Braga L, Renner JB, et al. Characterization of individual radiographic features of hip osteoarthritis in African American and White women and men: the Johnston County Osteoarthritis Project. Arthritis Care Res. 2010;62(2):190–197. doi: 10.1002/acr.20067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Callahan LF, Shreffler J, Schwartz TA, Schoster B, Renner JB, Jordan JM. Associations between education, occupation and community poverty with hip osteoarthritis. Osteoarthritis Cartilage. 2009;17(11):S367. [Google Scholar]
- 115.Dieppe P, Judge A, Williams S, et al. Variations in the pre-operative status of patients coming to primary hip replacement for osteoarthritis in European orthopaedic centres. BMC Musculoskelet Disord. 2009;10(1):19. doi: 10.1186/1471-2474-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Schafer T, Krummenauer F, Mettelsiefen J, Kirschner S, Gunther KP. Social, educational, and occupational predictors of total hip replacement outcome. Osteoarthritis Cartilage. 2010;18(8):1036–1042. doi: 10.1016/j.joca.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 117.Chang RW, Pellisier JM, Hazen GB. A cost–effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996;275(11):858–865. [PubMed] [Google Scholar]
- 118.Chaturvedi N, Ben-Shlomo Y. From the surgery to the surgeon: does deprivation influence consultation and operation rates? Br J Gen Pract. 1995;45(392):127–131. [PMC free article] [PubMed] [Google Scholar]
- 119.Rahman MM, Kopec JA, Sayre EC, et al. Effect of sociodemographic factors on surgical consultations and hip or knee replacements among patients with osteoarthritis in British Columbia, Canada. J Rheumatol. 2011;38(3):503–509. doi: 10.3899/jrheum.100456. [DOI] [PubMed] [Google Scholar]
- 120.Ellis H, Bucholz R. Disparity of care in total hip arthroplasty. Curr Opin Ortho. 2007;18(1):2–7. [Google Scholar]
- 121.Van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc Sci Med. 2000;50(6):813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 122.Hawker GA, Wright JG, Badley EM, Coyte PC. Perceptions of, and willingness to consider, total joint arthroplasty in a population-based cohort of individuals with disabling hip and knee arthritis. Arthritis Rheum. 2004;51(4):635–641. doi: 10.1002/art.20524. [DOI] [PubMed] [Google Scholar]
- 123.Hawker GA. Who, when, and why total joint replacement surgery? The patient’s perspective. Curr Opin Rheumatol. 2006;18(5):526–530. doi: 10.1097/01.bor.0000240367.62583.51. [DOI] [PubMed] [Google Scholar]
- 124.Agabiti N, Picciotto S, Cesaroni G, et al. The influence of socioeconomic status on utilization and outcomes of elective total hip replacement: a multicity population-based longitudinal study. Int J Qual Health Care. 2007;19(1):37–44. doi: 10.1093/intqhc/mzl065. [DOI] [PubMed] [Google Scholar]
- 125.Judge A, Welton NJ, Sandhu J, Ben-Shlomo Y. Geographical variation in the provision of elective primary hip and knee replacement: the role of socio-demographic, hospital and distance variables. J Public Health (Oxf) 2009;31(3):413–422. doi: 10.1093/pubmed/fdp061. [DOI] [PubMed] [Google Scholar]
- 126.Hawker GA, Guan J, Croxford R, et al. A prospective population-based study of the predictors of undergoing total joint arthroplasty. Arthritis Rheum. 2006;54(10):3212–3220. doi: 10.1002/art.22146. [DOI] [PubMed] [Google Scholar]
- 127.Escalante A, Espinosa-Morales R, Del Rincon I, Arroyo RA, Older SA. Recipients of hip replacement for arthritis are less likely to be Hispanic, independent of access to health care and socioeconomic status. Arthritis Rheum. 2000;43(2):390–399. doi: 10.1002/1529-0131(200002)43:2<390::AID-ANR20>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 128.Hanchate AD, Zhang Y, Felson DT, Ash AS. Exploring the determinants of racial and ethnic disparities in total knee arthroplasty: health insurance, income, and assets. Med Care. 2008;46(5):481–488. doi: 10.1097/MLR.0b013e3181621e9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Melzer D, Guralnik JM, Brock D. Prevalence and distribution of hip and knee joint replacements and hip implants in older Americans by the end of life. Aging Clin Exp Res. 2003;15(1):60–66. doi: 10.1007/BF03324481. [DOI] [PubMed] [Google Scholar]
- 130.Ang DC, Ibrahim SA, Burant CJ, Kwoh CK. Is there a difference in the perception of symptoms between african americans and whites with osteoarthritis? J Rheum. 2003;30(6):1305–1310. [PubMed] [Google Scholar]
- 131.Mahomed NN, Barrett J, Katz JN, Baron JA, Wright J, Losina E. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am. 2005;87(6):1222–1228. doi: 10.2106/JBJS.D.02546. [DOI] [PubMed] [Google Scholar]
- 132.Callahan LF, Knight J, Shreffler J, Schoster B, Renner J, Jordan JM. Disability and knee osteoarthritis: associations with individual and community socioeconomic status. Arthritis Rheum. 2010;62(10):S1463. [Google Scholar]
- 133.Cookson R, Dusheiko M, Hardman G. Socioeconomic inequality in small area use of elective total hip replacement in the English National Health Service in 1991 and 2001. J Health Serv Res Policy. 2007;12(Suppl 1):S10–S17. doi: 10.1258/135581907780318365. [DOI] [PubMed] [Google Scholar]
- 134.Jensen LK. Knee osteoarthritis: influence of work involving heavy lifting, kneeling, climbing stairs or ladders, or kneeling/squatting combined with heavy lifting. Occup Environ Med. 2008;65(2):72. doi: 10.1136/oem.2007.032466. [DOI] [PubMed] [Google Scholar]
- 135.Shumway-Cook A, Patla A, Stewart A, Ferrucci L, Ciol MA, Guralnik JM. Environmental components of mobility disability in community-living older persons. J Am Geriatr Soc. 2003;51(3):393–398. doi: 10.1046/j.1532-5415.2003.51114.x. [DOI] [PubMed] [Google Scholar]
- 136.Haak M, Fänge A, Horstmann V, Iwarsson S. Two dimensions of participation in very old age and their relations to home and neighborhood environments. Am J Occu Ther. 2008;62(1):77–86. doi: 10.5014/ajot.62.1.77. [DOI] [PubMed] [Google Scholar]
- 137.Marmot M, Friel S, Bell R, Houweling TA, Taylor S Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 138.Li LC, Sayre EC, Kopec JA, Esdaile JM, Bar S, Cibere J. Quality of non-pharmacological care for people with osteoarthritis in the community. J Rheumatol. 2011;38(10):2230–2237. doi: 10.3899/jrheum.110264. [DOI] [PubMed] [Google Scholar]
- 139.Borkhoff CM, Wieland ML, Myasoedova E, et al. Reaching those most in need: a scoping review of interventions to improve health care quality for disadvantaged populations with osteoarthritis. Arthritis Care Res. 2011;63(1):39–52. doi: 10.1002/acr.20349. [DOI] [PubMed] [Google Scholar]
- 140.Evans GW, Kantrowitz E. Socioeconomic status and health: the potential role of environmental risk exposure. Ann Rev Public Health. 2002;23(1):303–331. doi: 10.1146/annurev.publhealth.23.112001.112349. [DOI] [PubMed] [Google Scholar]
- 141• •.Wills AK, Black S, Cooper R, et al. Life course body mass index and risk of knee osteoarthritis at the age of 53 years: evidence from the 1946 British birth cohort study. Ann Rheum Dis. 2012;71(5):655–660. doi: 10.1136/ard.2011.154021. A prospective longitudinal study that provides insight on the lifecourse approach and confirms that osteoarthritis risk accumulates from prolonged exposure to high BMI throughout adulthood. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Macfarlane GJ, De Silva V, Jones GT. The relationship between body mass index across the life course and knee pain in adulthood: results from the 1958 birth cohort study. Rheumatology. 2011;50(12):2251–2256. doi: 10.1093/rheumatology/ker276. [DOI] [PubMed] [Google Scholar]
- 143.Parks CG, D’Aloisio AA, Deroo LA, et al. Childhood socioeconomic factors and perinatal characteristics influence development of rheumatoid arthritis in adulthood. Ann Rheum Dis. 2012 doi: 10.1136/annrheumdis-2011-201083. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Jacobsson LTH, Jacobsson ME, Askling J, Knowler WC. Perinatal characteristics and risk of rheumatoid arthritis. BMJ. 2003;326(7398):1068–1069. doi: 10.1136/bmj.326.7398.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Felson D, Hannan M, Naimark A, et al. Occupational physical demands, knee bending, and knee osteoarthritis: results from the Framingham Study. J Rheumatol. 1991;18(10):1587–1592. [PubMed] [Google Scholar]
- 146.Sandmark H, Hogstedt C, Vingard E. Primary osteoarthrosis of the knee in men and women as a result of lifelong physical load from work. Scand J Work Environ Health. 2000;26(1):20–25. doi: 10.5271/sjweh.505. [DOI] [PubMed] [Google Scholar]
- 147.Maetzel A, Mäkelä M, Hawker G, Bombardier C. Osteoarthritis of the hip and knee and mechanical occupational exposure – a systematic overview of the evidence. J Rheumatol. 1997;24(8):1599. [PubMed] [Google Scholar]
- 148.Croft P, Coggon D, Cruddas M, Cooper C. Osteoarthritis of the hip: an occupational disease in farmers. Br Med J. 1992;304(6837):1269–1272. doi: 10.1136/bmj.304.6837.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Croft P, Cooper C, Wickham C, Coggon D. Osteoarthritis of the hip and occupational activity. Scand J Work Environ Health. 1992;18(1):59–63. doi: 10.5271/sjweh.1608. [DOI] [PubMed] [Google Scholar]
- 150.Andersen S, Thygesen LC, Davidsen M, Helweg-Larsen K. Cumulative years in occupation and the risk of hip or knee osteoarthritis in men and women: a register-based follow-up study. Occu Environ Med. 2012;69(5):325–330. doi: 10.1136/oemed-2011-100033. [DOI] [PubMed] [Google Scholar]
- 151.Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes. J General Int Med. 2004;19(12):1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 153.Gordon MM, Hampson R, Capell H, Madhok R. Illiteracy in rheumatoid arthritis patients as determined by the Rapid Estimate of Adult Literacy in Medicine (REALM) score. Rheumatology. 2002;41(7):750–754. doi: 10.1093/rheumatology/41.7.750. [DOI] [PubMed] [Google Scholar]
- 154.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Internal Med. 2005;165(17):1946–1952. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 155.Swearingen CJ, McCollum L, Daltroy LH, Pincus T, Dewalt DA, Davis TC. Screening for low literacy in a rheumatology setting: more than 10% of patients cannot read ‘cartilage,’ ‘diagnosis,’ ‘rheumatologist,’ or ‘symptom’. J Clin Rheumatol. 2010;16(8):359–364. doi: 10.1097/RHU.0b013e3181fe8ab1. [DOI] [PubMed] [Google Scholar]
- 156.Handy SL, Boarnet MG, Ewing R, Killingsworth RE. How the built environment affects physical activity: views from urban planning. Am J Prevent Med. 2002;23(2):64–73. doi: 10.1016/s0749-3797(02)00475-0. [DOI] [PubMed] [Google Scholar]
- 157.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117(2):417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 158.Berke EM, Koepsell TD, Moudon AV, Hoskins RE, Larson EB. Association of the built environment with physical activity and obesity in older persons. Am J Public Health. 2007;97(3):486–492. doi: 10.2105/AJPH.2006.085837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Mcginn AP, Evenson KR, Herring AH, Huston SL, Rodriguez DA. Exploring associations between physical activity and perceived and objective measures of the built environment. J Urban Health. 2007;84(2):162–184. doi: 10.1007/s11524-006-9136-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Camacho E, Verstappen S, Symmons D. The association between socioeconomic status, learned helplessness, and disease outcome in patients with inflammatory polyarthritis. Arthritis Care Res. 2012 doi: 10.1002/acr.21677. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Smith TW, Peck JR, Ward JR. Helplessness and depression in rheumatoid arthritis. Health Psychol. 1990;9(4):377–389. doi: 10.1037//0278-6133.9.4.377. [DOI] [PubMed] [Google Scholar]
- 162.Sarason IG, Levine HM, Basham RB, Sarason BR. Assessing social support: the social support questionnaire. J Personal Soc Psychol. 1983;44(1):127–139. [Google Scholar]
- 163.Pinquart M, Sörensen S. Influences of socioeconomic status, social network, and competence on subjective well-being in later life: a meta-analysis. Psychol Aging. 2000;15(2):187–224. doi: 10.1037//0882-7974.15.2.187. [DOI] [PubMed] [Google Scholar]
- 164.Michael YL, Colditz GA, Coakley E, Kawachi I. Health behaviors, social networks, and healthy aging: cross-sectional evidence from the Nurses’ Health Study. Qual Life Res. 1999;8(8):711–722. doi: 10.1023/a:1008949428041. [DOI] [PubMed] [Google Scholar]
- 165.Bosworth H, Siegler I, Olsen M, et al. Social support and quality of life in patients with coronary artery disease. Qual Life Res. 2000;9(7):829–839. doi: 10.1023/a:1008960308011. [DOI] [PubMed] [Google Scholar]
- 166.Ethgen O, Vanparijs P, Delhalle S, Rosant S, Bruyère O, Reginster JY. Social support and health-related quality of life in hip and knee osteoarthritis. Qual Life Res. 2004;13(2):321–330. doi: 10.1023/B:QURE.0000018492.40262.d1. [DOI] [PubMed] [Google Scholar]
- 167.Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48(12):3359–3370. doi: 10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- 168.Kee C. Older adults with osteoarthritis. Psychological status and physical function. J Gerontol Nurs. 2003;29(1):26–34. doi: 10.3928/0098-9134-20031201-07. [DOI] [PubMed] [Google Scholar]
- 169.Keefe FJ, Lefebvre JC, Smith SJ. Catastrophizing research: avoiding conceptual errors and maintaining a balanced perspective. Pain Forum. 1999;8:176–180. [Google Scholar]
- 170.Keefe FJ, Caldwell DS, Queen KT, et al. Pain coping strategies in osteoarthritis patients. J Consul Clin Psychol. 1987;55(2):208. doi: 10.1037//0022-006x.55.2.208. [DOI] [PubMed] [Google Scholar]
- 171.Rapp SR, Rejeski WJ, Miller ME. Physical function among older adults with knee pain: the role of pain coping skills. Arthritis Care Res. 2000;13(5):270–279. doi: 10.1002/1529-0131(200010)13:5<270::aid-anr5>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 172.Keefe FJ, Lefebvre JC, Egert JR, Affleck G, Sullivan MJ, Caldwell DS. The relationship of gender to pain, pain behavior, and disability in osteoarthritis patients: the role of catastrophizing. Pain. 2000;87(3):325–334. doi: 10.1016/S0304-3959(00)00296-7. [DOI] [PubMed] [Google Scholar]
- 173.Keefe FJ, Caldwell DS, Williams DA, et al. Pain coping skills training in the management of osteoarthritic knee pain-II: follow-up results. Behav Ther. 1990;21(4):435–447. [Google Scholar]
- 174.Hausmann LRM, Hannon MJ, Kresevic DM, Hanusa BH, Kwoh CK, Ibrahim SA. Impact of perceived discrimination in healthcare on patient-provider communication. Med Care. 2011;49(7):626–633. doi: 10.1097/MLR.0b013e318215d93c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Daly MC, Duncan GJ, McDonough P, Williams DR. Optimal indicators of socioeconomic status for health research. Am J Public Health. 2002;92(7):1151–1157. doi: 10.2105/ajph.92.7.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
Websites
- 201.Wilkinson RG, Marmot M. Social determinants of health: the solid facts. World Health Organization; 2003. www.euro.who.int/__data/assets/pdf_file/0005/98438/e81384.pdf. [Google Scholar]
- 202.World Health Organization: towards a common language for functioning, disability and health: ICF. World Health Organisation; 2002. www.who.int/classifications/icf/training/icfbeginnersguide.pdf. [Google Scholar]
- 203.Arthritis Foundation. Osteoarthritis Summit 2012 Agenda. Arthritis Foundation; Atlanta, GA: 2012. www.arthritis.org/osteoarthritis-agenda/ [Google Scholar]
- 204.Solar O, Irwin A. A conceptual framework for action on the social determinants of health. 2007 www.who.int/sdhconference/resources/conceptualframeworkforactiononsdh_eng.pdf.
- 205.Census of population and housing: summary social, economic, and housing characteristics. 1993 www.census.gov/population/www/censusdata/90pubs/cph-5.html.