Abstract
Objective
To evaluate the acceptance and preliminary efficacy of in-home telehealth delivery of problem-solving therapy (tele-PST) among depressed low-income homebound older adults in a pilot randomized control trial (RCT) designed to test its feasibility and preliminary efficacy.
Methods
121 homebound individuals who were age 50+ and scored 15+ on the 24-item Hamilton Rating Scale for Depression (HAMD) participated in the 3-arm RCT, comparing tele-PST to in-person PST and telephone support calls. Six sessions of the PST-PC (primary care) were conducted for the PST participants. For tele-PST, second through sixth sessions were conducted via Skype video call. Acceptance of tele-PST or in-person PST was measured with the 11-item, 7-point scale modified Treatment Evaluation Inventory (TEI). Mixed-effect regression analysis was used to examine the effects of treatment group, time, and the interaction term between treatment group and time on the HAMD scores.
Results
The TEI score was slightly higher among tele-PST participants than among in-person PST participants. The HAMD scores of tele-PST participants and in-person PST participants at 12-week follow-up were significantly lower than the HAMD scores of telephone support call participants, and the treatment effects were maintained at 24-week follow-up. The HAMD scores of tele-PST participants did not differ from those of in-person PST participants.
Conclusions
Despite their initial skepticism, almost all participants had extremely positive attitudes toward tele-PST at 12-week follow-up. Tele-PST also appears to be an efficacious treatment modality for depressed homebound older adults and to have significant potential to facilitate their access to treatment.
Previous randomized controlled trials (RCTs) showed the efficacy of in-home, short-term problem-solving therapy (PST) for reducing depressive symptoms among medically ill, homebound older adults.1,2 Despite its efficacy with depressed homebound older adults, in-home, in-person PST or other psychotherapy for them is likely to be cost prohibitive. Most mental health and aging-service agencies lack sufficient professional staff to deliver in-person depression interventions at older adults' homes. Travel expenses for in-person delivery are likely to create an undue burden on these providers. Moreover, one study that tested the effectiveness of providing a home delivered, therapeutic psychosocial intervention for rural older adults found that it was not unusual for interventionists to travel an hour to a participant's home for a scheduled appointment only to discover that no one was there, or that the older adult was not feeling well enough to participate in a treatment session.3
Previous studies of telepsychiatry in general, compared to face-to-face modalities, have reported overall favorable findings about reliability of clinical assessment, equivalent clinical outcomes and client satisfaction, and long-term cost effectiveness.4-8 Despite the rapid growth in telepsychiatry over the past decade, however, our literature search yielded only two studies focusing on the practice using videoconferencing link and its effectiveness with frail and disabled older adults: one on psychogeriatric assessment in Hong Kong and the other on dementia assessment in Australia.9,10 In these past practices of telepsychiatry, however, clients had to be at a site where videoconferencing equipment was set up for use by many others. Internet-based, guided self-help PST for depression has been tested with younger age persons with depression.11,12 However, we found no studies that evaluated delivery of psychosocial intervention via an interactive videoconferencing link between a therapist's office and homebound older adults' residences.
Telephone-administered psychotherapy for depression or other mental disorders has also been found to be effective and to result in lower attrition rates than in-person psychotherapy.13-16 However, videoconferencing therapy has advantages over telephone delivery of psychotherapy, as it enables therapist and client to maintain visual contact and see nonverbal behavior. Videoconferencing also allows therapist and client to show each other worksheets and other therapy aids. For isolated homebound older adults, the visual contact and interactive nature of videoconferencing are likely to be especially beneficial as they allow most of the benefits of in-person sessions.
Considering the resource constraints and high costs of in-person PST delivery and the advantages of videoconferencing over telephone delivery, home-based telehealth PST (tele-PST) may have potential to facilitate homebound older adults' access to depression treatment. With the availability of low-cost videoconferencing tools, real-time, interactive tele-PST, which allows therapists and clients most benefits of in-person sessions, holds promise as the most practical, accessible depression treatment for homebound older adults and disabled persons. The purpose of this study was to evaluate the acceptance and preliminary efficacy of in-home tele-PST (via Skype video call) among low-income homebound older-adults who participated in a pilot RCT designed to test its feasibility and preliminary signal of efficacy, compared to in-person PST and telephone support calls. We examined tele-PST acceptance among these older adults and the changes in depressive symptoms over 24 weeks.
Method
Recruitment and Participants
Depressed homebound older adults (PHQ-9 >= 10) were referred to the project by case managers at a large Meals on Wheels (MOW) and other aging-network agencies serving low-income individuals in central Texas. The sample inclusion criteria were age 50+; non-Hispanic White, Black, or Hispanic; English speaking; and a score of 15+ on the 24-item Hamilton Rating Scale for Depression (HAMD). We included those between age 50 and 64 because a higher proportion of this younger group of homebound adults than those age 65 and older suffer from depression and lack health insurance.17 The exclusion criteria were high suicide risk; dementia (assessed with the Mini-Cog18); bipolar disorder; current (12-month) or lifetime psychotic symptoms or disorder; presence of co-occurring alcohol or other addictive substance abuse; any vision or hearing impairment that would interfere with PST; and current involvement in psychotherapy. Those who had been on antidepressants more than 2 months but showed significant depressive symptoms were not excluded. Of 186 referrals received during the 24-month recruitment and enrollment period, 124 met the inclusion criteria and 121 who agreed to participation in the study were randomly assigned into three groups—tele-PST (n=43, 35%); in-person PST (n=42, 35%), and telephone support calls (n=36, 30%). Written informed consent, approved by the first author's university institutional review board, from each participant was obtained after the study procedures had been fully explained. Fourteen participants dropped out from the study before completing 6 sessions of in-person PST (n=7), tele-PST (n=5), and telephone care calls (n=2), and 5 (2 tele-PST participant; and 3 telephone care call participants) who completed all 6 sessions of intervention dropped out before 12-week follow-up. Attrition was due mostly to deteriorating health problems that resulted in hospitalization, nursing home placement, and death; however, the baseline demographic and clinical characteristics of the dropouts did not significantly differ from those who continued in the study.
Therapist Training, Supervision, and Fidelity Monitoring
The second author (MTH) trained two licensed master's-level social workers (MLM and LS) in PST and provided them ongoing clinical supervision and fidelity monitoring, with a review of the audiorecording of two sessions (the first session and one random selection between the second and the fifth) from 20% of all subjects throughout the study. All tele-PST sessions were automatically recorded using MP3 Skype Recorder software downloaded (free of charge) on the therapists' desk top computers, while all in-person PST sessions were recorded with microcasette recorders. Each therapist provided both tele-PST and in-person PST. The mean global adherence and competence rating score on the PST-PC Therapist Adherence and Competence Scale19 was 4.4 on a 6-point scale (0 = very poor to 5 = very good), with no difference between two therapists and between tele-PST and in-person PST delivery.
In-Person and Tele-PST Process and Telephone Support Calls
In this study, six 60-minute sessions of the PST-PC (primary care) version were conducted. Developed in England in the 1980s,20,21 PST-PC posits that people with deficits in problem-solving skills become vulnerable to depression because such deficits lead to ineffective coping attempts under high stress levels.22-24 Adapted in the 1990s for delivery in fast-paced U.S. primary care settings, PST-PC teaches and practices the seven steps of problem-solving in each of four to six sessions.25,26 Older-adult participants in PST reported the problem-solving therapy process to be very helpful.27 For in-person PST in the present study, all six sessions were conducted face-to-face with a therapist in the participant's home. The initial PST sessions with tele-PST participants were conducted the same way, with the therapist bringing psychoeducational materials about depression and PST worksheets for participants to use in later sessions. At the end of the first session with each tele-PST participant, the therapist provided the participant with the videoconferencing equipment and demonstrated its use for the second through sixth sessions. Telephone support calls by master's-level social workers were 30 minutes in length and designed to afford a degree of human contact to the control group. The callers were not trained in any specific psychotherapy. All baseline and follow-up assessments were done in person, and six monthly booster sessions were conducted by telephone.
Tele-PST Equipment and Internet Security
Tele-PST equipment provided to the participants included nine laptop computers, with15.6-inch high-definition (720p) LED display screen, and USB cards or modems for 3G wireless services. The Skype video call function was installed on each computer. Although the laptops had built-in microphones and speakers, each tele-PST participant also received a headset with microphone for privacy protection. Each tele-PST session began when the therapist telephoned the participant and asked him/her to turn on the computer. Only one participant, who owned a computer with Internet connection, chose to use her own computer for tele-PST sessions. Therapists used their office desktop computers.
Each laptop was configured to functionally limit the Internet and cellular network usage, minimize opportunity to make it unstable (e.g., caused by a participant accidentally hitting the keyboard buttons), and bypass log-in process. Upon boot up, the laptop automatically connected to the Internet via the wireless card/modem and auto-answered the therapist's Skype video call. This enabled people with little to no computer familiarity to easily use the video call function without manually interacting with the system. The Microsoft SteadyState application was used to remove any change a participant may have made to the laptop.
Skype is a peer-to-peer communications application, which means that computers exchange messages directly, instead of going through a third-party server. It operates behind a firewall which can help protect it from unauthorized access. Skype's encryption of communications is secure enough to prevent casual eavesdropping and for someone from impersonating a user unless the username and password are compromised.28,29 Skype on each laptop was periodically updated to benefit from the most current Skype security measures. For further Internet security, the system design allowed participants to accept video calls only from their PST therapists. For the security of Skype sessions via the therapists' desktop computers, the information security office at the first author's institution provided periodic security assessment.
Since many participants lived in neighborhoods with high property theft rates, laptop lids were engraved with university property serial numbers, and computers were attached to furniture with cable locks. All videoconferencing equipment was retrieved from tele-PST participants at their 2-week posttest and transferred to the next participants. No videoconferencing equipment was stolen.
Measures
Depressive symptoms
The 24-item HAMD consists of the GRID-HAMD-21 structured interview guide30 augmented with three additional items assessing feelings of hopelessness, helplessness, and worthlessness, with specific probes and follow-up questions developed by Moberg et al.31 According to Moberg et al., these cognitive symptoms are thought to be more sensitive to depression in older adults. We have slightly modified the scoring format of the 3 additional questions so that both frequency and intensity of these feelings can be factored in their ratings as in the case with other comparable items (e.g., depressed mood, anxiety, somatic) in the GRID-HAMD-21. The HAMD was administered at baseline and at 12-week, 24-week, and 36-week follow-ups. In this study, the baseline and 12- and 24-week follow-up HAMD scores were used.
Acceptance of tele-PST or in-person PST
At 12-week follow-up, all tele-PST or in-person PST participants were administered the 11-item, 7-point scale modified Treatment Evaluation Inventory (TEI32). The TEI has two subscales: (1) General Acceptability scale, with eight items measuring acceptability, suitability, and likely effectiveness of a treatment; likeability of the procedures used in the treatment; subject's willingness to apply the treatment to other people like him- or herself; consistency of the treatment with common sense or everyday ideas about what treatment should be; and general reaction to the treatment. (2) Negative Aspects subscale, with three items measuring undesirable side effects, discomforts, and possible risks of undergoing the treatment. A score of 44, out of the maximum possible 77, indicates moderately favorable attitudes toward the treatment. Cronbach's alphas for TEI was 0.82 for both tele-PST and in-person participants. At the time of the TEI administration or during their monthly telephone booster sessions, most participants also offered unsolicited comments about their PST experiences.
Other participant characteristics and quality of Skype connection/transmission
Participants' characteristics included sociodemographics, disability status at baseline and follow-up, and computer ownership/Internet connection. Disability status was assessed using the short-form (12-item) World Health Organization Disability Assessment Schedule (WHODAS-II33). WHODAS-II assesses disabilities without asking respondents to identify whether the problem had been caused by medical or mental health conditions. In consideration of the subjects' homebound state, the last item, “Your day to day work,” was reworded to “Your day to day work in and around the house.” With respect of tele-delivery transmission quality, immediately following each tele-PST session, the therapist noted any detailed technological problems and rated the connection and transmission quality on a 5-point scale where 1= connection was so poor that any part of the session had to be conducted via telephone, and 5 = excellent transmission (i.e., crisp audio/video). The mean transmission quality rating for each tele-PST participant was calculated by dividing five total session ratings by 5. The overall mean transmission quality rating for all tele-PST participants was calculated by taking the mean of the individual mean ratings.
Statistical Analysis
All analyses were performed using SPSS v.19 (IBM Corp, Armonk, NY). Between-group one-way ANOVA (with Bonferroni-corrected post-hoc tests), χ2 tests, and t-tests were used to assess group differences in participant characteristics. All tests of significance were two tailed with α set at 0.05. To examine the acceptance of tele-PST, the overall mean TEI scores for tele-PST and in-person PST participants were compared using independent samples t-tests. Bivariate associations between TEI scores, baseline and 12-week HAMD scores (using Pearson correlation coefficients), and other participant characteristics were also examined. Treatment effects on depression severity (HAMD score) were analyzed from an intent-to-treat approach using piecewise mixed-effects regression with random intercept model.34 Treatment group, time, and the interaction term between treatment group and time were included in the model, with group as a between-subject effect and time as a two-piece (piece 1 [time 1] = baseline to 12 weeks; piece 2 [time 2] = 12 weeks to 24 weeks) continuous within-subject variable. Variance explained in the residual was estimated using a formula from Raudenbush and Byrk.34 Standardized mean difference effect sizes, comparing tele-PST and in-person PST, respectively, with telephone support calls, were calculated following a formula presented by Lipsey and Wilson,35 in which t-values of the estimated marginal means at 12- and 24-week follow-ups were converted into effect sizes.
Results
Table 1 shows the participants' demographic and other characteristics at baseline. The participants were diverse in age, gender, and race/ethnicity, but a majority were low-income, with a high degree of medical morbidity and disability. Two-thirds met the diagnosis of major depressive disorder. No significant difference was found in age, gender, and other baseline characteristics by race/ethnicity. No significant difference was found in any baseline demographic and clinical characteristics (medical morbidity, disability, depression severity, and SCID diagnosis) among three treatment groups.
Table 1. Demographic and Clinical Characteristics of Participants at Baseline (N = 121).
| Age, mean (SD) (range: 50-89) | 65.21 (±9.22) |
|---|---|
| Age group (n, %) | |
| 50-59 | 38 (31.4) |
| 60-69 | 48 (39.7) |
| 70-79 | 24 (19.8) |
| 80-85 | 11 (9.1) |
| Gender (n, %) | |
| Male | 27 (22.3) |
| Female | 94 (77.7) |
| Race/ethnicity (n, %) | |
| Non-Hispanic White | 50 (41.3) |
| Black | 41 (33.9) |
| Hispanic | 30 (24.8) |
| Living arrangement (n, %) | |
| Living alone | 77 (63.6) |
| Not living alone | 44 (36.4) |
| Family income (n, %) | |
| <= 15,000 | 77 (63.6) |
| 15,001-25,000 | 25 (20.7) |
| 25,001-50,000 | 12 (9.9) |
| Don't know/refused | 7 (5.8) |
| Computer ownership/Internet subscription (n, %) | |
| No computer or Internet | 74 (61.2) |
| Computer only | 15 (12.5) |
| Both computer and Internet | 32 (26.4) |
| SCID diagnosis (n, %) | |
| Major Depressive disorder | 81 (67.0) |
| Depressive disorder, NOS | 35 (28.9) |
| Dystymia | 5 (4.1) |
| No. of diagnosed medical conditions, mean (SD) | 3.19 (±1.54) |
| Disability (WHODAS-II) score,1 mean (SD) (range:13-54) | 36.11 (±8.91) |
| Depression severity (HAMD score), mean (SD) (range:15-42) | 24.55 (±6.62) |
| RCT group (n, %) | |
| Tele-PST | 43 (35.5) |
| In-person PST | 42 (34.7) |
| Telephone support call | 36 (29.8) |
The possible ranges of the score are 12-60.
Treatment Acceptance
Both PST groups reported extremely high acceptance of their treatment modality, with tele-PST group reporting a slightly higher TEI scores than in-person PST group (72.14±6.64 for tele-PST and 68.08±8.27 for in-person PST; t = 2.305, df = 70, p= 0.024). The TEI scores did not differ by age, gender, race/ethnicity, income, computer/Internet ownership, baseline or 12-week HAMD scores, and transmission quality ratings. No subject had ever participated in telepsychiatry, and only two had previously used Skype video call. The overall mean rating of transmission quality (3.83±1.06) for tele-PST participants was close to “very good,” and the 50% of the participants had “very good” or “excellent” average ratings across all five tele-PST sessions (median rating = 4.2), while 6.1% of all (n = 179) tele-PST sessions had to be switched to telephone sessions because of poor transmission quality.
Nearly all participants' unsolicited comments about tele-PST were positive:
I had some discomfort with tele-PST on the first day and preferred in-person therapy, but think it was effective and recognize that this works (White female, age 75).
I enjoyed it. I looked forward to it. I loved the computer part. … I was skeptical at first, but found it worked great (White female, age 67).
I was very excited about receiving the computer and learning to use it. This was very new to me, and I am very proud of myself. This computer therapy gave me confidence to try new things, and I was able to text my granddaughter back when she sent me a text message!… I feel empowered from the therapy and am able to repeat the PST steps and feel very comfortable using them when I encounter any problem (Black female, age 84).
It [tele-PST] was great. Didn't have to go anywhere, and could do it at home. A lot of people that don't know about this that need help could really use this help (Hispanic female, age 63).
Only one tele-PST participant (White male, age 78, TEI score = 48) was displeased with tele-PST because “it did not feel real.” He was also one of the first tele-PST participants who experienced audio/video transmission glitches. These transmission problems eased as we stopped conducting tele-PST sessions during peak cell phone use periods (i.e., early afternoon hours). Another tele-PST participant stated that tele-PST did not allow her privacy protection from her prying family members, who often entered her room while she was in session. She felt that in-person PST would have given her more protection as the family members would not have walked in if the therapist had been there in person.
Group and Time Effects on Depression Severity and Effect Sizes
The results of the mixed-effects regression analysis are presented in Table 2. The main effects of group were significant for both tele-PST (t = 3.035, df = 234; p = 0.003) and in-person PST (t = 2.720; df = 237; p = 0.007), as compared to the telephone support call. The main effect of time 1 (baseline to 12 weeks) was also significant (t = 4.562, df = 204; p < 0.001), but the main effect of time 2 (12 weeks to 24 weeks) was nonsignificant (t = 1.308, df = 205; p = 0.192). Group by time 1 interaction effects were also significant (t = 2.550, df = 206; p = 0.012 for tele-PST group; t = 2.639, df = 207; p = 0.009 for in-person PST group); however, group by time 2 interaction effects were nonsignificant (t = 0.597, df = 204; p = 0.551 for tele-PST group; t = 1.196, df = 203; p = 0.233 for in-person PST group). The model pseudo-R2, calculated from comparing the full model's residual estimate to that of the intercept only model, was 0.52.
Table 2. Treatment Effects by Group, Time, and Group by Time: Mixed-Effects Regression Results.
| Variable | B | SE | 95% CI | t | df | p |
|---|---|---|---|---|---|---|
| Intercept | 19.16 | 1.26 | (16.70, 21.63) | 15.23 | 231.24 | .000 |
| Treatment group | ||||||
| Tele-PST | −5.24 | 1.73 | (−8.64, −1.84) | −3.04 | 233.56 | .003 |
| In-person PST (Telephone support call) | −4.71 | 1.73 | (−8.13, −1.30) | −2.72 | 236.82 | .007 |
| Time 1: Baseline to12 weeks | −2.87 | 0.63 | (−4.10, −1.63) | −4.56 | 203.82 | .000 |
| Time 2: 12 weeks to 24 weeks | −0.15 | 0.11 | (−0.37, 0.07) | −1.31 | 205.04 | .192 |
| Group by time | ||||||
| Tele-PST × Time 1 | −2.20 | 0.86 | (−3.90, −0.50) | −2.55 | 205.57 | .012 |
| In-person PST × Time 1 (Telephone support × Time 1) | −2.29 | 0.87 | (−3.99, −0.58) | −2.64 | 207.14 | .009 |
| Tele-PST × Time 2 | 0.09 | 0.15 | (−0.21, 0.39) | 0.60 | 203.86 | .551 |
| In-person PST × Time 2 (Telephone support × Time 2) | 0.18 | 0.15 | (−0.12, 0.48) | 1.20 | 203.08 | .233 |
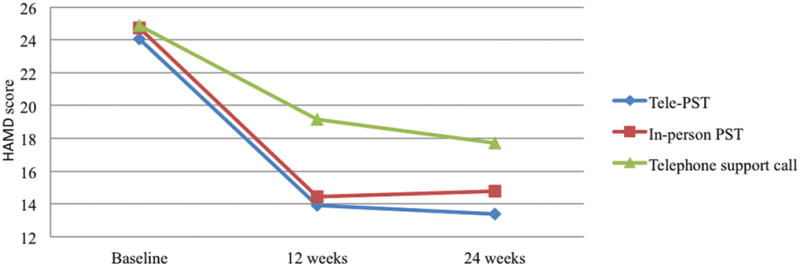
Table 3 shows that the group differences in predicted mean HAMD scores at 12-week follow-up were significant between tele-PST participants and telephone support call participants and between in-person PST participants and telephone support call participants, but they were not significant between tele-PST participants and in-person PST participants. At 24-week follow-up, the group differences remained significant between tele-PST participants and telephone support call participants, but they were marginally significant (p = 0.08) between in-person PST participants and telephone support call participants and not significant between tele-PST participants and in-person PST participants. The predicted mean HAMD scores by group and time are plotted in Figure 1. Standardized mean difference effect sizes for HAMD score changes were ESsm = 0.77 for tele-PST and ESsm = 0.70 for in-person PST at 12-week follow-up and ESsm = 0.66 for tele-PST and sm = 0.45 for in-person PST at 24-week follow-up.
Table 3. Pairwise Comparisons of Predicted Mean HAMD Scores by Group and Time.
| 12-Week Follow-Up (N = 106) | t | df | p | |
|---|---|---|---|---|
| Tele-PST vs. telephone support call | 13.92 (1.18) vs. 19.16 (1.26) | −3.03 | 233.56 | 0.003 |
| In-person PST vs. telephone support call | 14.44 (1.19) vs. 19.16 (1.26) | −2.72 | 236.81 | 0.007 |
| Tele-PST vs. in-person PST | 13.92 (1.18) vs. 14.44 (1.19) | −0.31 | 239.61 | 0.755 |
|
| ||||
| 24-Week Follow-Up (N = 96) | t | df | p | |
|
|
||||
| Tele-PST vs. telephone support call | 13.37 (1.13) vs. 17.70 (1.21) | −2.62 | 206.53 | 0.010 |
| In-person PST vs. telephone support call | 14.80 (1.12) vs. 17.70 (1.21) | −1.76 | 205.96 | 0.080 |
| Tele-PST vs. in-person PST | 13.37 (1.18) vs. 14.80 (1.12) | −0.90 | 207.56 | 0.369 |
(): Standard error.
Note: 95% CI of the predicted means at 12-week follow-up: 11.58 – 16.25 for tele-PST group; 12.09 – 16.79 for in-person PST group; and 16.68 – 21.64 for telephone support call group. 95% CI of the predicted means at 24-week follow-up: 11.14 – 15.60 for tele-PST group; 12.59 – 17.02 for in-person PST group; and 15.32 – 20.08 for telephone support call group.
Figure 1. Predicted Mean HAMD Scores by Group and Time.
Discussion
Tele-PST in this study was different from the usual office-based telepsychiatry because it enabled a therapist in an office to conduct PST sessions with individual participants in their homes via Skype video call. The study findings show that depressed homebound older adults, who were mostly low-income, racial/ethnic minorities with low-level of familiarity with technology, may have been initially skeptical or uncomfortable about tele-PST sessions. However, almost all, including most who experienced low-quality audio/video transmission early in the study, had extremely positive attitudes toward tele-PST at post-treatment. Some appear to have really enjoyed and been proud of their use of videoconferencing and to have liked its convenience.
More important, we found no significant difference between tele-PST and in-person PST participants in their treatment effects on depression severity. The results of mixed-effects regression analysis show that, although all three treatment groups experienced reduction in depressive symptom over the study period, the symptom severities were significantly lower among the participants in either delivery modality of PST than among the participants who received telephone support calls at 12-week follow-up. Since the subjects were socially isolated homebound individuals, it is not surprising that telephone support calls had positive effect. A large RCT of PST's effectiveness for older adults with major depression and executive dysfunction also found that a supportive therapy offering active listening and support focused on participants' problems and concerns had positive effect.36,37 However, the effect of either delivery modality of PST on depressive symptoms was stronger than that of telephone support calls, and the treatment gains were maintained at 24-week follow-up for the participants. Based on these results, tele-PST appears to be an efficacious treatment for depressed, low-income homebound older adults.
Since the equipment needed for videoconferencing in this study was a laptop and wireless card/modem for each participant, the cost of obtaining and installing the equipment was relatively low. Moreover, due to rapid technological advances, the equipment and transmission costs are likely to decline in the future, even in remote rural areas.38 The economical nature of the project enhances its replicability and generalizability in social service, physical health, and mental health settings in the future. Also, as increasing numbers of older adults own computers and become users of health information technology,39 they will likely become more open to telehealth delivery of mental health treatment. For aging-service providers that have been unlikely to provide their clients in-person PST due to resource constraints, tele-PST is likely to become a feasible option. Although we have occasionally experienced low-quality audio/video transmissions, the overall transmission quality was very good. Poor transmission quality will be more infrequent with the 4G/LTE mobile network carrier upgrades in the near future.
This study has the following limitations. First, because the study period was rather short (24 weeks), we were not able to examine the relationship between long-term treatment outcome and the treatment modality as well as cost analysis of tele-PST delivery versus in-person PST delivery. A community-based clinical and cost effectiveness study of tele-PST delivery to homebound older adults is the next step. Second, our sample was limited to older adults without cognitive and sensory deficits. Tele-PST for older adults with cognitive and sensory deficits, especially auditory and visual, may not be feasible as such deficits can impair the ability to interact with a therapist over a videoconference connection. This limited utility of tele–mental health delivery modality for older adults with most disabilities calls for more research on improving the quality of transmissions and incorporating special features that mimic direct human interactions in tele–mental health delivery.
Conclusions
Because of its brevity and step-by-step approach to practical, “here-and-now” problem-solving coping skills, PST is easy to deliver in person and via videoconferencing. However, in-home tele-PST had not been previously tested for acceptance by and efficacy with homebound older adults. This study found that depressed homebound older adults accept tele-PST and report extremely positive experiences with it and that tele-PST may be efficacious for disabled homebound older adults. The implication for future service delivery is that fewer home visits mean fewer resources needed for provision of PST to homebound people, and thus PST can be delivered to more of them.
Acknowledgments
This study was funded by the National Institute of Mental Health (R34 MH083872).
Footnotes
No Disclosures to Report
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ciechanowski P, Wagner E, Schmaling K, et al. Community-integrated home-based depression treatment in older adults. JAMA. 2004;29:1569–1577. doi: 10.1001/jama.291.13.1569. [DOI] [PubMed] [Google Scholar]
- 2.Gellis ZD, McGinty J, Horowitz A, et al. Problem-solving therapy for late-life depression in home care. A randomized field trial. Am J Geriat Psychiat. 2007;15:968–978. doi: 10.1097/JGP.0b013e3180cc2bd7. [DOI] [PubMed] [Google Scholar]
- 3.Kaufman AV, Scogin FR, Burgio LD, et al. Providing mental health services to older people living in rural communities. J Gerontol Soc Work. 2007;48:349–65. doi: 10.1300/j083v48n03_05. [DOI] [PubMed] [Google Scholar]
- 4.Hyler SE, Gangure DP, Batchelder ST. Can telepsychiatry replace in-person psychiatric assessment? A review and meta-analysis of comparison studies. CNS Spectr. 2005;10:403–413. doi: 10.1017/s109285290002277x. [DOI] [PubMed] [Google Scholar]
- 5.Monnier J, Knapp RG, Frueh CC. Recent advances in telepsychiatry. An updated view. Psychiat Serv. 2003;54:1604–1609. doi: 10.1176/appi.ps.54.12.1604. [DOI] [PubMed] [Google Scholar]
- 6.O'Reilly R, Bishop J, Maddox K, et al. Is telepsychiatry equivalent to face-to-face psychiatry? Results from a randomized controlled equivalence trial. Psychiat Serv. 2007;58:836–843. doi: 10.1176/ps.2007.58.6.836. [DOI] [PubMed] [Google Scholar]
- 7.Ruskin PE, Silver-Aylaian M, Kling MA, et al. Treatment outcomes in depression. Comparison of remote treatment through telepsychiatry to in-person treatment. Am J Psychiat. 2004;161:1471–1476. doi: 10.1176/appi.ajp.161.8.1471. [DOI] [PubMed] [Google Scholar]
- 8.Simpson S. Psychotherapy via videoconferencing: a review. Brit J Guid Couns. 2009;37:271–286. [Google Scholar]
- 9.Tang WK, Chiu H, Woo J, et al. Telepsychiatry in psychogeriatric service. A pilot study. Int J Geriatr Psych. 2001;16:88–931. doi: 10.1002/1099-1166(200101)16:1<88::aid-gps282>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 10.Loh PPK, Maher S, Goldswain P, et al. Diagnostic accuracy of telehealth community dementia assessments. J Am Geriatr Soc. 2005;53:2043–2044. doi: 10.1111/j.1532-5415.2005.00479_8.x. [DOI] [PubMed] [Google Scholar]
- 11.Carter JA, Buckey JC, Greenhalch L, et al. An interactive media program for managing psychosocial problems on long-duration spaceflights. Aviat Space Envir Med 2005. 2005;76:B213–B223. [PubMed] [Google Scholar]
- 12.Ünlü B, Riper H, van Straten A, et al. Guided self-help on the internet for Turkish migrants with depression: the design of a randomized controlled trial. Trials. 2010;11:101. doi: 10.1186/1745-6215-11-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohr DC, Vella L, Hart S, et al. The effect of telephone-administered psychotherapy on symptoms of depression and attrition. A meta-analysis. Clin Psychol-Sci Pr. 2008;15:243–253. doi: 10.1111/j.1468-2850.2008.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ludman EJ, Simon GE, Tutty D, et al. A randomized trial of telephone psychotherapy and pharmacotherapy for depression. Continuation and durability effect. J Consult Clin Psych. 2007;75:257–266. doi: 10.1037/0022-006X.75.2.257. [DOI] [PubMed] [Google Scholar]
- 15.Lovell K, Cox D, Haddock G, et al. Telephone administered cognitive behavior therapy for treatment of obsessive compulsive disorder. Randomized controlled non-inferiority trial. BMJ. 2006;333:883–887. doi: 10.1136/bmj.38940.355602.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simon GE, Ludman EJ, Tutty S, et al. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment. A randomized trial. JAMA. 2004;292:935–942. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- 17.Choi NG, Teeters M, Perez L, et al. Severity and correlates of depressive symptoms among recipients of Meals in Wheels: Age, gender, and racial/ethnic difference. Aging Ment Health. 2010;14:145–154. doi: 10.1080/13607860903421078. [DOI] [PubMed] [Google Scholar]
- 18.Borson S, Scanlan J, Brush M, et al. The mini-cog. A cognitive “vital signs” measure for dementia screening in multi-lingual elderly. Int J Geriatr Psych. 2000;25:1021–1027. doi: 10.1002/1099-1166(200011)15:11<1021::aid-gps234>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 19.Hegel MT, Dietrich AJ, Seville JL, et al. Training residents in problem solving treatment of depression. A pilot feasibility and impact study. Fam Med. 2004;36:204–208. [PubMed] [Google Scholar]
- 20.Catalan J, Gath DH, Anastasiades P, et al. Evaluation of a brief psychological treatment for emotional disorders in primary care. Psychol Med. 1991;21:1013–1018. doi: 10.1017/s0033291700030002. [DOI] [PubMed] [Google Scholar]
- 21.Mynors-Wallis LM, Gath DH, Lloyd-Thomas AR, et al. Randomized controlled trial comparing problem-solving treatment with amitriptyline and placebo for major depression in primary care. BMJ. 1995;310:441–445. doi: 10.1136/bmj.310.6977.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.D'Zurilla TJ, Nezu AM. A Positive Approach to Clinical Intervention. New York: Springer; 2007. Problem-Solving Therapy. [Google Scholar]
- 23.Nezu AM. Efficacy of a social problem-solving therapy approach for unipolar depression. J Consult Clin Psych. 1986;54:196–202. doi: 10.1037//0022-006x.54.2.196. [DOI] [PubMed] [Google Scholar]
- 24.Nezu AM, Nezu CM, Perri MG. Theory Research and Clinical Guidelines. New York: Wiley; 1989. Problem-Solving Therapy for Depression. [Google Scholar]
- 25.Hegel MT, Barrett JE, Cornell JE, et al. Predictors of response to problem-solving treatment of depression in primary care. Behav Ther. 2002;33:511–527. [Google Scholar]
- 26.Hegel MT, Barrett JE, Oxman TE. Training therapists in problem-solving treatment of depressive disorders in primary care. Lessons learned from the “Treatment Effectiveness Project.”. Fam Syst Health. 2000;18:423–435. [Google Scholar]
- 27.Dakin EK, Areán PA. Patient perspectives on the benefits of psychotherapy for late-life depression. Am J Geriatr Psychiatry. 2012 doi: 10.1097/JGP.0b013e331823e2fce. online publication ahead of print. [DOI] [PubMed] [Google Scholar]
- 28.Hays B. Skype: A practical security analysis. [Accessed July 25, 2009];SANS Institute. 2008 Available: www.sans.org/reading-room/whitepapers/voip/skype-pratical-security-analysis32918.
- 29.University of Texas at Austin Information Security Office. [Accessed July 25, 2009];ISO consensus paper: Skype. 2009 Jul 20; Available: http://security/utexas.educ/consensus/skype.html.
- 30.GRID-HAMD-17, GRID-HAMD-21 Structured Interview Guide. San Diego, Depression Rating Scale Standardization Team. International Society for CNS Drug Development. 2003 [Google Scholar]
- 31.Moberg PJ, Lazarus LW, Mesholam RI, et al. Comparison of the standard and structured interview guide for the Hamilton Depression Rating Scale in depressed geriatric inpatients. Am J Geriatr Psychiatry. 2001;9:35–40. [PubMed] [Google Scholar]
- 32.Landreville P, Guerette A. Psychometric properties of a modified version of the Treatment Evaluation Inventory for assessing the acceptability of treatments for geriatric depression. Can J Aging. 1998;17:414–424. [Google Scholar]
- 33.Disability Assessment Schedule: WHODAS II. Geneva, Switzerland: World Health Organization; 2000. [Google Scholar]
- 34.Raudenbush SW, Bryk AS. Hierarchical linear models: applications and data analysis methods. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- 35.Lipsey MW, Wilson DB. Practical meta-analysis: Applied social research methods series. Vol. 49. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- 36.Areán PA, Raue PJ, Mackin S, et al. Problem-solving therapy and supportive therapy in older adults with major depression and executive dysfunction. Am J Psychiat. 2010;167:1391–1398. doi: 10.1176/appi.ajp.2010.09091327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alexopoulos GS, Raue PJ, Kiosses DN, et al. Problem-solving therapy and supportive therapy in older adults with major depression and executive dysfunction: Effect on disability. Arch Gen Psychiat 2011. 2011;68:33–41. doi: 10.1001/archgenpsychiatry.2010.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yellowlees P, Shore J, Roberts L. Practice guidelines for videoconferencing-based telemental health – October 2009. American Telemedicine Association. Telemental Health Standards and Guidelines Working Group. Telemed J e-Health. 2010;16:1075–1089. doi: 10.1089/tmj.2010.0148. [DOI] [PubMed] [Google Scholar]
- 39.Choi NG. Relationship between health service use and health information technology use among older adults. Analysis of the U.S. National Health Interview Survey. J Med Internet Res. 2001;13:e33. doi: 10.2196/jmir.1753. [DOI] [PMC free article] [PubMed] [Google Scholar]


