Abstract
In an effort to reduce patient tobacco dependence and create healthier work environments, New York State (NYS) mandated 100% tobacco-free addiction treatment programs for state funded or certified facilities in 2008. We present the results of a longitudinal study examining how local implementation features shape clinician reactions to the regulation and influence post-regulation clinician behavior and strain. A cohort of 147 clinicians associated with 13 treatment organizations throughout NYS completed a survey prior to the passage of the regulation and again approximately 1 year post-regulation. Findings reveal that local implementation features of clinician participation in the planning for change, the provision of change-related information, and perceived organizational support predicted perceptions of change management fairness, which in turn predicted clinical practice behaviors to support smoking cessation, as well as psychological and behavioral strain. In contrast, self-efficacy for change was neither related to local implementation or clinician outcomes. Practical implications are discussed.
1. Introduction
On July 24, 2008, New York State (NYS) became the first in the nation to require all 1,419 state-funded or state-certified addiction treatment programs to be 100% tobacco-free (New York Office of Alcoholism and Substance Abuse Services [OASAS], n.d.). Far beyond other smoking bans which limit their scope to indoor smoking, this comprehensive regulation put forth by OASAS prohibited the use or possession of all tobacco products by patients, employees, volunteers, and visitors in all facilities. This includes exterior grounds and vehicles owned, leased or operated by the facility. Addiction treatment centers in NYS are also required to screen clients for tobacco use and incorporate tobacco cessation into treatment programming.
The goal of creating healthier workplaces for employees and fostering tobacco independence in clients is laudable and may yield positive effects over time such as lower rates of smoking (Williams et al., 2005) and better treatment outcomes (Baca & Yahne, 2009). However, the OASAS regulation represents a major change for substance use disorder treatment centers in NYS. Nationwide estimates are that only around 10–20% of treatment centers have policies that completely prohibit smoking (Richter et al., 2005; Knudsen et al., 2009) and only about 30% of treatment programs offer treatment for nicotine dependence (Fuller et al, 2007). In addition, the regulation impacts a large segment of the patient population; around 70% of patients seeking treatment for substance use disorders smoke (Fiore et al., 2000; McCarthy et al., 2002). Clinicians are also affected by the regulation because they must now incorporate tobacco dependence into the treatment plans of patients that use tobacco products. These are important contextual factors to consider in light of the high failure rate associated with implementing innovative practices in substance use disorder treatment (Rogers, 2002). Moreover, failure is particularly high when change is externally imposed (Bolman & Deal, 2006) as is the case with the OASAS tobacco-free regulation.
1.1 The Challenge of Treating Smoking Cessation in Substance Use Disorder Treatment
Even though national guidelines encourage clinicians to treat nicotine dependence (Fiore et al., 2000) and professional associations such as ASAM have issued policy statements to this effect, smoking cessation is not frequently included in drug treatment (Fuller et al., 2007; Gill et al., 2000; Richter et al., 2004). One reason for this is the smoking culture that exists in some drug treatment settings (McIlvain & Bobo, 2005; Reilly et al., 2006; Sees & Clark, 1993). A major contributor to this culture is the widespread use of the Alcoholics Anonymous (AA) model of treatment (White, 1998). In the AA model, individuals are taught that their first and primary responsibility is sobriety. They are advised to avoid tackling other challenges such as smoking until they are confident that they can remain sober (Bobo & Husten, 2000; Kotz, 1993). Consistent with this model, the treatment community strongly discouraged physicians and other healthcare professionals from providing smoking cessation treatment to patients until recently (McIlvain & Bobo, 2005).
1.2 Purpose of the Present Study
The present study provides a longitudinal investigation of predictors of clinician reactions to the OASAS regulation, as well as post-regulation clinician behavior and strain. As just discussed, the regulation is expected to have a substantial effect on clinicians’ work environment because center policies, procedures, and job requirements are affected by the regulation. These changes may be perceived as stressful for clinicians because some clinicians may not be adequately prepared or motivated to treat tobacco dependence. Consequently, we expect that the regulation will affect clinician behavior and strain. Examining clinician reactions is consistent with a longstanding tradition in research on organizational change (e.g., Amiot et al., 2006; Jimmieson et al., 2004; Rafferty & Griffin, 2006) and implementation science (e.g., Gotham, 2006; Klein & Sorra, 1996; Lehman et al., 2002; Simpson & Flynn, 2007), based on the recognition that ultimately it is individuals who implement change, not programs or organizations. While we focus on the implementation of the OASAS regulation from the clinician’s perspective, we will examine statistically treatment organization effects given the nested nature of our data.
1.3 What Predicts Clinician Outcomes Following the OASAS Regulation?
Organizational change is stressful and often meets with employee resistance (Eilam & Shamir, 2005; Herold et al., 2007). The same is true for the implementation of evidence-based treatments and practices (Fixsen et al., 1995; Lehman et al., 2002). This is because organizational change fundamentally alters the employer-employee relationship and creates uncertainty among employees, which is inherently stressful (Alexander, Sinclair, & Tetrick, 1995). However, the manner in which change is implemented can influence reactions, which in turn affects employee outcomes (Amiot et al., 2006; Jimmieson et al., 2004; Rafferty & Griffin, 2006). A key element often discussed in the implementation science literature is employee buy-in and support of an impending change (Fixsen et al., 1995; Klein & Sorra, 1996; Lehman et al., 2002). Likewise, the literature on workplace smoking bans discusses how the manner in which such policies are implemented can influence their success (Brighman et al., 1994; Greenberg, 1994; Kotz, 1993) and points out that highly restrictive policies are especially difficult to implement (Parry et al., 2000).
Based on this literature we examine three features of how the OASAS regulation was implemented locally as predictors of clinician reactions: (1) clinician participation in the planning for change in their treatment program (Amiot et al., 2006; Bolman & Deal, 2006; Callaly & Ayra, 2005; Cunningham et al., 2002; Rafferty & Griffin, 2006; Terry & Jimmieson, 2003; Wanberg & Banas, 2000), (2) the provision of change-related information (Gabel & Oster, 1998; Jimmieson et al., 2004; Wanberg & Banas, 2000), and (3) overall perceptions of organizational support (Amiot et al., 2006; Fugate et al., 2002; Jimmieson et al., 2004; Terry & Jimmieson, 2003). More specifically, we propose that how the change is implemented relates to clinician reactions; specifically perceptions of procedural justice and self-efficacy for change. Procedural justice refers to the perceived fairness of a decision or process (Thibaut & Walker, 1975). If change is perceived as fair, then uncertainty is reduced and a sense of control over the situation is enhanced (Thibaut & Walker, 1975). Procedural justice perceptions are shaped by the actions that are taken during the change initiative, including providing employees with voice in the change process (e.g., Brotheridge, 2003; Daly & Geyer, 1994; Kernan & Hanges, 2002), providing information about the impending change (Folger & Bies, 1989; Greenberg, 1994), and demonstrating care and concern during the change process (e.g., Greenberg, 1994). In his seminal work, Leventhal (1980) discusses how careful policy design and planning are essential in the development of fair procedures.
Self-efficacy for change may also be influenced by how the OASAS regulation is implemented at each treatment program. Because change creates uncertainty (Rafferty & Griffin, 2006), the more that employees are involved in the process, provided information about the change, and feel supported by their organization, the greater their confidence that they can cope with change. This is consistent with self-efficacy theory (Bandura, 1977) as well as research evidence that self-efficacy for change is positively related to both the provision of information (Jimmieson et al., 2004) and employee participation during the change process (Amiot et al., 2006). Taken together, this literature leads to the following predictions:
-
Hypothesis 1
Clinician perceptions of participation in the local planning for change, the provision of change-related information, and perceived organizational support will be positively related to procedural justice perceptions.
-
Hypothesis 2
Clinician perceptions of participation in the local planning for change, the provision of change-related information, and perceived organizational support will be positively related to self-efficacy for change.
In the context of the OASAS tobacco-free regulation, an important outcome is the extent to which clinicians report engaging in clinical practice behaviors that focus on treating tobacco dependence in clients. We argue that these behaviors will be more likely when clinicians believe that the change is implemented fairly and they have greater self-efficacy for the change. This prediction is supported by the finding that employees who feel more fairly treated perform better at work (Cohen-Charash & Spector, 2001). Research also indicates that self-efficacy predicts task performance (Sadri & Robertson, 1993).
We also expect that the manner in which the change is implemented will have downstream effects on clinician strain. This is because the uncertainty associated with organizational change is a workplace stressor which can induce strain (Fugate et al., 2002; Quick & Tetrick, 2003; Spector, 1998). Strain is generally classified as a psychological or behavioral reaction to a stressor (Caplan et al., 1975; Spector, 1998). Common indicators of psychological strain include attitudinal reactions to work such as reduced job satisfaction and heightened intentions to leave the organization, as well as diminished psychological well-being (e.g., burnout). Behavioral strain includes negative ways of reacting to the stressor, with a common response being the display of counterproductive work behavior; intentional employee behavior that is harmful to the organization, such as shirking job responsibilities, purposefully coming in late, and feigning sickness to get out of work (Dalal, 2005). While no research to date has examined the change to a 100% tobacco free workplace, research on other types of organizational change (e.g., downsizing, drug testing) finds that procedural justice and self-efficacy predict psychological and behavioral strain (Cropanzano et al., 2005; Fugate et al., 2002; Jimmieson et al., 2004; Konovsky & Cropanzano, 1991; Sheck & Kinicki, 2000; Tepper, 2001; Terry & Jimmieson, 2003). Therefore, we predict:
-
Hypothesis 3
As procedural justice increases, clinicians will report greater use of clinical practice behaviors to treat tobacco dependence as well as less psychological and behavioral strain.
-
Hypothesis 4
As self-efficacy for change increases, clinicians will report greater use of clinical practice behaviors to treat tobacco dependence as well as less psychological and behavioral strain.
-
Hypothesis 5
Procedural justice will mediate the relationship between implementation characteristics (participation in the planning for change, the provision of change-related information, and perceived organizational support) and clinician outcomes (use of clinical practice behaviors to treat tobacco dependence, psychological strain, and behavioral strain).
-
Hypothesis 6
Self-efficacy for change will mediate the relationship between implementation characteristics (participation in the planning for change, the provision of change-related information, and perceived organizational support) and clinician outcomes (use of clinical practice behaviors to treat tobacco dependence, psychological strain, and behavioral strain).
2. Materials and Methods
2.1 Study Design
Longitudinal data were obtained from the Managing Effective Relationships in Treatment Services (MERITS II) project. Data were collected at two points in time: approximately 1–3 months prior to the passage of the OASAS regulation and again approximately 1 year post-regulation. The project was funded by the National Institute on Drug Abuse (NIDA), in response to a program announcement focusing on health services research on practice improvement utilizing community treatment programs within NIDA’s Clinical Trials Network (CTN). At the time of initial data collection, the CTN had two New York “nodes” These are partnerships between a research center and a number of community treatment programs (CTPs). One CTN node was based in New York City, and the other on Long Island. Together, they comprised 10 eligible CTPs. Seven CTPs agreed to participate.
Because we were not able to meet our data requirements with clinicians from these two CTN nodes, recruitment was extended outside of the CTN, with the aim of assuring that we obtained a broad cross-section of treatment programs that were representative of the population of programs in existence in NYS. We reviewed available data from the 2006 SAMHSA facility locator and NSSATS database and determined that our sample of participating programs was similar to the aggregate characteristics of all NYS treatment programs in terms of having a primary focus on substance use disorders, offering detoxification services, offering methadone maintenance, having hospital inpatient services, offering short-term residential services, offering long-term residential services, operating as a halfway house, offering services for adolescents, and serving criminal justice clients (a full report is available upon request from the first author).
Paper and pencil surveys were completed by clinicians working in 31 free-standing substance use disorder treatment centers, affiliated with 13 treatment organizations throughout NYS. Fifty-two percent of these centers were in one of the five New York City boroughs and the remaining 48% were in other parts of NYS (e.g., Albany, Buffalo, Mount Kisco). To participate in the study, eligible treatment organizations had to provide substance use disorder counseling services in a community-based setting. This excluded prison-based programs, Veteran’s Health Administration programs, and driving-under-the-influence schools. Eligible clinicians had to have direct contact with patients in a therapeutic relationship (individual or group counseling sessions, or both). The data were collected on-site during normal business hours and the treatment organization was compensated for each completed survey to compensate for employee time-off-the clock. All procedures were approved by the Institutional Review Board at the University of Georgia.
2.3 Sample
Data were collected from 147 clinicians who completed surveys at time 1 and time 2. The response rate at time 1 was 69% and the response rate at time 2 was 71%. Sixty percent (60%) of the eligible time 1 participants also completed the time 2 survey. The majority of clinicians were women (57%), non-Hispanic White (59%), had no children living at home (54%), were not married (54%), and were not current smokers (85%). Overall, participants were well-educated with 50% holding at least a master degree. On average, participants were 47.58 years old (12.04), worked 36.76 (8.49) hours per week, earned $42,111 ($13, 973) per year, and worked for their center 5.80 (6.52) years. Thirty-seven percent of the clinicians were personally in recovery from substance use disorders.
2.4 Measures
All variables were measured using previously validated, multi-item measures. In the present study all measures demonstrated acceptable reliability; coefficients alpha ranged from .74 to .97 (see Table 1). Features of the implementation process and mediators were measured at time 1 and clinician outcomes were measured at time 2.
Table 1.
Means, Standard Deviations, Internal Consistencies, and Bivariate Correlations among Study Variables
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||||
| 1. Smoking Status | .15 | .36 | n/a | ||||||||||
| 2. Participation in Change | 2.62 | .85 | −.03 | .80 | |||||||||
| 3. Change-related Information | 3.35 | 1.32 | .07 | .34 | .97 | ||||||||
| 4. Perceived Organizational Support | 3.51 | .86 | −.01 | .30 | .20 | .92 | |||||||
| 5. Procedural Justice | 3.14 | .71 | −.16 | .51 | .41 | .42 | .83 | ||||||
| 6. Self-Efficacy for Change | 3.84 | .78 | −.18 | .06 | .12 | .05 | .23 | .74 | |||||
| 7. Clinical Practice Behaviors | 3.75 | .87 | .11 | .22 | .26 | .15 | .18 | −.01 | .93 | ||||
| 8. Emotional Exhaustion | 2.49 | .81 | −.07 | −.12 | −.15 | −.34 | −.22 | −.13 | −.20 | .92 | |||
| 9. Job Satisfaction | 3.89 | .68 | .14 | .18 | .34 | .28 | .23 | .20 | .32 | −.62 | .86 | ||
| 10. Turnover Intentions | 2.65 | 1.21 | .04 | −.24 | −.20 | −.41 | −.35 | −.05 | −.23 | .62 | −.45 | .92 | |
| 11. Counterproductive Work Behavior | 26.63 | 4.95 | −.02 | −.28 | −.17 | −.19 | −.20 | .08 | −.38 | .49 | −.44 | .50 | .77 |
Note. Coefficients alpha are presented on the diagonals. Smoking status coded 1 = Current smokers, 0 = Not current smokers. All correlations with an absolute value of .16 or greater are significant at p < .05.
2.4.1. Characteristics Features of the Implementation Process
Clinician participation in the local planning for change was assessed with Wanberg and Banas’ (2000) 4-item scale (e.g., “I was able to participate in decision-making regarding the implementation of changes required by this regulation”). Change-related information was measured using Jimmieson, Terry, and Callan’s (2004) 6-item scale (e.g., “Information about the regulation has been directly communicated to me”). Perceived organizational support was assessed with Eisenberger, Cummings, Armeli, and Lynch’s (1997) 8-item scale (e.g., “My treatment center cares about my opinions”). Response options for all scales ranged from 1 = strongly disagree to 5 = strongly agree.
2.4.2. Mediators
Procedural justice related to change was assessed with Greenberg’s (1994) 4-item scale, slightly modified so that it referred to the OASAS regulation (e.g., “The decision to implement the tobacco-free regulation was made in a fair manner”). Self-efficacy for change was measured using a slightly modified version of Wanberg and Banas’ (2000) orignal scale (e.g., “I have reason to believe I may not perform as well in my job following the implementation of the OASAS regulation”, reverse scored). One item was dropped from the Wanberg and Banas measure because it was double barreled and the item referent was modified from “organizational restructuring” (from the original measure) to “implementation of the OASAS regulation.” Response options for all scales ranged from 1 = strongly disagree to 5 = strongly agree.
2.4.3. Clinician Outcomes
Use of clinical practice behaviors to treat tobacco dependence assessed the extent to which clinicians routinely perform the two components of U.S. Public Health Service recommended clinical practice guideline, Treating Tobacco Use and Dependence (Fiore et al., 2000). This included five questions asking clinicians to indicate the extent to which they routinely engage in the “5 As” of treating tobacco dependence (i.e., ask clients about their tobacco use, advise tobacco users to quit, assess client willingness to quit, assist clients via brief interventions to enhance motivation to quit, arrange to follow-up with clients on their progress) and seven questions related to the use of guideline-recommended counseling to treat tobacco dependence (e.g., “Thinking about clients who are interested in quitting their tobacco use, to what extent do you personally provide them with self-help materials about smoking cessation?”). All thirteen items were averaged to represent an overall measure of clinical practice behaviors. Response options for these scales ranged from 0 = never to 5 = always.
Psychological strain was assessed with three measures. Burnout was assessed with Maslach, Jackson, and Leiter’s (1996) 9-item sub-scale for Emotional Exhaustion (e.g., “I feel emotionally drained from my work”). Job Satisfaction was assessed using Smith’s (1976) 6-item scale (e.g., “I enjoy nearly all the things I do in my job”). Turnover intentions were assessed using Adams and Beehr’s (1998) 3-item scale (e.g., “I am thinking about quitting my job and finding another in the near future”). Response options for all three stain measures ranged from 1 = strongly disagree to 5 = strongly agree. Behavioral strain was assessed with Spector, Fox, Penney, Bruursema, Goh, and Kessler’s (2006) 20-item scale measure of counterproductive work behavior(e.g., “Tried to look busy when doing nothing,” “ Taken a longer break than was allowed”). Response options for this scale ranged from 1 = never to 5 = every day.
2.4.4. Control variables
Two variables were used as statistical controls in the subsequent analyses. Because clinician smoking status might influence reactions to the OASAS regulation (e.g., clinicians who smoke may have lower self-efficacy for change and lower procedural justice perceptions), we allowed a dummy coded variable representing smoking status to covary with self-efficacy for change and procedural justice to account for these relationships. We classified clinician smoking status (0 = not current smokers; 1 = current smokers) based on two items from Etter’s (2004) scale (e.g., “Have you smoked more than 100 cigarettes in your lifetime?”; “If yes, have you smoked within the last 30 days?”). Clinicians indicating that they did not smoke more than 100 cigarettes in their lifetime, as well as those that indicated they did smoke more than 100 but none in the past 30 days, were classified as not being current smokers. Clinicians indicating that they did smoke more than 100 cigarettes in their lifetime and one or more cigarettes in the past 30 days were classified as current smokers.
One-way ANOVAs suggested that there were significant mean differences in the provision of change related information (F (12, 131) = 4.85, p < .05) and clinical practice behaviors (F (12, 125) = 2.52, p < .05) based on the organization at which counselors worked. Intraclass correlations were .24 and .11, respectively. However, the overall sample size of organizations (n=13) was not sufficient for estimating a multi-level model with organization level effects (e.g., Scherbaum & Ferreter, 2009). Thus, to hold differences due to organization location constant, nonsense coding (Cohen & Cohen, 1983) was used where a unique variable was created to represent each organization and this variable was then allowed to covary with change related information and clinical practice behaviors.
3. Results
3.1 Data Analyses
Path analysis conducted via structural equation modeling in Mplus version 5.1 (Muthén & Muthén, 2008) was used to test the study hypotheses. This method evaluates how well a proposed structural equation model, with observed variables only, explains the sample correlations among variables included in the model (Kline, 2010). We evaluated overall model fit using the chi-square statistic, the Comparative Fit Index (CFI), the root-mean-square error of approximation (RMSEA), and the standardized root mean residual (SRMR). It is recommended to only accept models with a CFI of .90 or higher (e.g., Marsh, Balla, & McDonald, 1988), with .95 or higher suggested for excellent fit (Hu & Bentler, 1999). For the RMSEA, .08 has been used to indicate mediocre fit (McCallum, Browne, & Sugawara, 1996), while .05 or lower is recommended to suggest good fit to the data (e.g., Hu & Bentler, 1999, McCallum et al, 1996). A cutoff of less than .08 is recommended for the SRMR (Hu & Bentler, 1999). Indirect effects were tested using the Delta method for calculating standard errors, as is default in Mplus.
In this study, we examined a model in which clinician involvement in change (i.e., participation in the local planning for change, change-related information, and perceived organizational support) predicted clinicians’ perceptions of procedural justice related to change and self-efficacy for change, which in turn predicted clinical practice behaviors associated with treating tobacco dependence as well as clinicians’ psychological (i.e. emotional exhaustion, turnover intentions, job satisfaction) and behavioral counterproductive work behavior) strain.
3.2 Study Results
Item-level missing data were minimal (range 0%–12%, M = 1%) and were handled with Full Information Maximum Likelihood in Mplus software, where standard errors for parameter estimates are computed using all available data without first filling in missing values (Muthén & Muthén, 2008). This is an appropriate technique for handling missing data in SEM (Enders & Bandalos, 2001) and yields unbiased estimates (Wothke, 1998). Means, standard deviations, scale reliabilities, and correlations among study variables are presented in Table 1. All implementation features and clinician outcomes were positively related to procedural justice related to change. However, self-efficacy was not correlated with any variables representing implementation features or clinician outcomes, with the exception of job satisfaction.
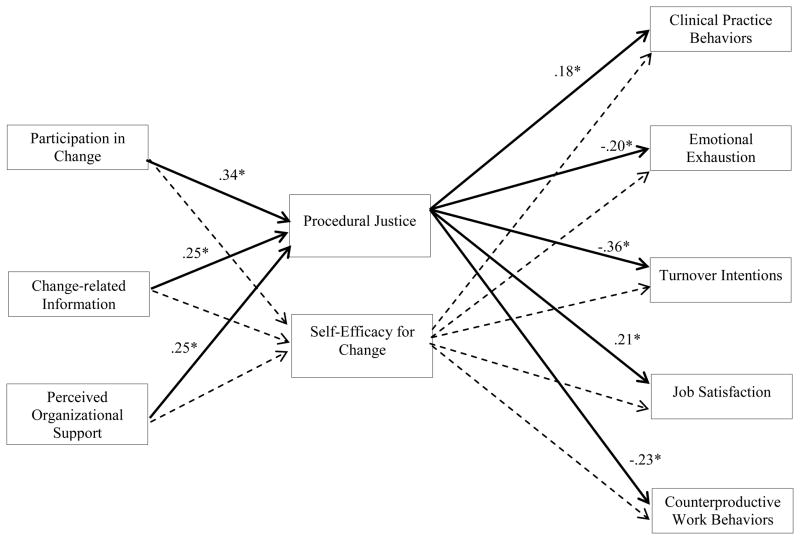
Overall model fit suggested that our hypothesized model had adequate fit to the data (χ2 (33) = 64.33; CFI = .91, RMSEA = .08, SRMR = .08). Decrements in fit can largely be attributed to non-significant parameter estimates involving self-efficacy for change. Model parameter estimates are shown in Figure 1. Standard errors associated with model parameters ranged from .07 to .09.
Figure 1. Features of the Implementation Process, Clinician Reactions, and Clinician Outcomes.
Note. * Indicates that standardized parameter estimates are significant at p < .05. Dashed lines indicate non-significant path weights.
We proposed that clinician involvement in change would predict procedural justice perceptions and self-efficacy for change. As shown in Figure 1, Hypothesis 1 was fully supported. Clinician perceptions of procedural justice were predicted by each of the change involvement variables: participation in planning for change, change-related information, and perceived organizational support. In contrast, no support was found for Hypothesis 2. Self-efficacy related to change was not predicted by participation in planning for change, change-related information, or perceived organizational support (see Figure 1).
We also proposed that stronger perceptions of procedural justice would predict greater use of clinical practice behaviors to treat tobacco dependence, less psychological strain, and less behavioral strain. Supporting Hypothesis 3 and as shown in Figure 1, perceptions of procedural justice at time 1 predicted the greater use of use of clinical practice behaviors, lower burnout, higher job satisfaction, lower turnover intentions, and less counterproductive behavior at time 2. By contrast, Hypothesis 4 was not supported; self-efficacy for change did not predict any clinician outcomes (see Figure 1).
Finally, we expected that both procedural justice (Hypothesis 5) and self-efficacy for change (Hypothesis 6) would mediate the relationship between features of the implementation process and clinician outcomes. Table 2 provides the results of the tests for these indirect effects. Full support was found for Hypothesis 5. Significant indirect effects through procedural justice were found for clinician participation in the local planning for change, change-related information, and perceived organizational support on clinician outcomes. By contrast, Hypothesis 6 was not supported; no indirect effects through self-efficacy for change were found for any of the features of the implementation process (see Table 2).
Table 2.
Summary of Indirect Effects of Features of the Implementation Process on Clinician Outcomes
| Specific Indirect Effect | via Procedural Justice | via Self-Efficacy for Change | ||
|---|---|---|---|---|
| Estimate | S.E. | Estimate | S.E. | |
| Participation in Change to | ||||
| Clinical Practice Behaviors | .06* | .03 | .00 | .01 |
| Emotional Exhaustion | −.07* | .03 | .00 | .01 |
| Job Satisfaction | .07* | .03 | .00 | .01 |
| Turnover Intentions | −.12* | .04 | .00 | .00 |
| CWBs | −.08* | .03 | .00 | .01 |
| Change Related Information to | ||||
| Clinical Practice Behaviors | .05 | .03 | −.01 | .01 |
| Emotional Exhaustion | −.05* | .03 | .01 | .01 |
| Job Satisfaction | .05* | .03 | .02 | .02 |
| Turnover Intentions | −.09* | .03 | .00 | .01 |
| CWBs | −.06* | .03 | .02 | .02 |
| Perceived Organizational Support to | ||||
| Clinical Practice Behaviors | .05* | .03 | .00 | .01 |
| Emotional Exhaustion | −.05* | .03 | .00 | .01 |
| Job Satisfaction | .06* | .03 | .00 | .01 |
| Turnover Intentions | −.10* | .03 | .00 | .00 |
| CWBs | −.06* | .03 | .00 | .01 |
Note.
significant at p < .05.
4. Discussion
The goal of the current study was to provide a longitudinal examination of predictors of clinician reactions to the NYS OASAS regulation, as well as post-regulation clinician behavior and strain. Three main conclusions can be drawn from our study. First, the manner in which the OASAS regulations were implemented locally was predictive of clinicians’ perceptions of how fairly the change was managed. Second, clinicians’ perceptions of fairness predicted clinical practice behaviors, psychological strain, and behavioral strain 1 year later. Third, counter to expectation, self-efficacy for change was not related to implementation features or clinician outcomes.
4.1 Implementation features in relation to clinician reactions and outcomes
Consistent with existing research, we found that all three implementation characteristics were related to fairness perceptions. These findings are consistent with existing research examining reactions to other types of large-scale change, such as reorganizations (e.g., Kernan & Hanges, 2002) and downsizings (e.g., Paterson & Cary, 2002). The self-interest model of procedural justice provides an explanation for these effects by noting that participation has instrumental value for employees because it may persuade managers to make decisions that are in the best interest of employees (Lind, Kanfer & Early, 1990). In the context of the OASAS regulation this has particular relevance because considerable discretion was given to local treatment providers in terms of how to implement specific regulatory components. For example, the regulation requires a written policy on how client tobacco use violations will be handled, but leaves it up to treatment programs to determine specific policies and sanctions.
Providing information about an impending change and general feeling of organizational support were also related to fairness perceptions. This is likely because in times of uncertainty, employees need information from managers and decision-makers to quell fears and reduce cynicism about how the change may negative affect them at work (Reichers, Wanous, & Austin, 1997). In addition, in the absence of communication from management employees may rely on informal sources of information to reduce uncertainty, such as rumors (Napier, Simmons, & Stratton, 1989). However, rumors are more likely to contain negative and inaccurate information (Rosnow, 1988). This can erode trust in management, particularly if rumors contain even a grain of truth (Rosnow, 1988). In support of this, Schweiger and DeNisi (1991) compared two plants on the verge of a merger and found that the employees in the plant where detailed information was provided prior to the merger reported considerably less uncertainty and more trust in management than did the other plant that received minimal information. Along these same lines, research consistently finds that perceptions of organizational support are strongly related to perceptions of fairness (for a review see Rhoades & Eisenberger, 2002). We extend this research to substance use disorder treatment and the implementation of restrictive state-mandated tobacco policies.
Unexpectedly, self-efficacy for change was unrelated to any of the implementation features shown in Figure 1. While our predictions were informed by previous research, in the context of the OASAS regulations being involved in the change process, provided information about the regulation, or supported by the organization did not relate to clinicians’ belief that they could master the skills required by the change. Perhaps the regulatory guidelines were vague enough that it was difficult for clinicians to grasp exactly how their roles would be expected to change prior to the passage of the regulation. For example, without knowing exactly what would be required to incorporate tobacco dependence into patient treatment planning, it may have been difficult for clinicians’ to gauge how successful they would likely be on the job after the regulation was passed. In addition, many of the regulatory components were not directly tied to clinicians’ core job duties. For example, many of the specific requirements dealt with having written policies in place banning tobacco use by staff, visitors, and patients. Likewise, some of the other requirements dealt with policing smoking behavior, posting signs, and making educational material available to patients. This may explain why self-efficacy for change was not affected by how the regulation was implemented. Another explanation is methodological. The self-efficacy for change measure was modified from its original form and displayed lower reliability than the other study measures. As such, the null findings may be a function of weaker psychometric properties of this measure.
In terms of predicting clinician outcomes six months after the passage of the OASAS regulations, strong support was found for the mediating role of justice perceptions. This is generally consistent with a voluminous body of research demonstrating that fairness predicts a wide range of employee outcomes, including job attitudes and behaviors (Colquitt, Colon, Wesson, Porter, & Ng, 2001). This current study adds to that literature by linking justice to clinical practice behaviors that support smoking cessation and demonstrating that justice is an explanatory mechanism for why implementation features ultimately affect clinician attitudes in the context of a state-mandated policy change on tobacco.
4.2 Practical suggestions
Several practical implications emerge from the results of this study. In light of the finding that the way in which the OASAS regulations were implemented locally relates to clinician psychological and behavioral strain, it is important to recognize the potential costly effects of clinician strain on both individuals (e.g., health problems, reduced quality of worklife) and organizations (e.g., absenteeism, reduced productivity). In addition, aspects of local implementation may influence whether clinicians engage in practice behaviors related to treating smoking cessation and, ultimately affect the quality of care for patients. The results of the present study provide concrete suggestions that managers and decision-makers can implement to reduce the negative fall-out associated with large-scale regulatory change.
While smoking bans are gaining popularity (Hammond & Gregoire, 2011), NYS is the first to implement a system-wide ban on tobacco use or possession in substance use disorder treatment facilities. The current study provides guidance for other states and programs on how to most effectively implement similar regulations. Our results suggest that when implementing similar regulations, fostering employee perceptions of fairness is critical. This can be influenced by proceeding with organizational change in a participative way that involves stakeholders in the planning related to implementation so they feel heard and supported throughout the change. Supervisors should be accessible and open to opinions from clinicians about their concerns, reconcile differences, and incorporate advice into final decisions. Timely and accurate information about the plan for change and how it will impact job responsibilities should be directly communicated to clinicians at all stages of the change process. This is particularly important to reduce uncertainty about impending change and avoid the spread of rumors that may negatively influence fairness perceptions. Finally, it is critical that clinicians feel supported by management through the change process. Creating such an environment takes sustained time and effort on the part of managers and is fostered by actively demonstrating care for clinicians’ well-being, acting supportively, and openly valuing clinicians’ contributions to the organization.
4.3 Limitations and conclusions
Although the present study provides the first empirical examination of how the NYS tobacco-free regulation was implemented locally and the downstream effects on clinician behaviors and strain, several limitations should be noted. Treatment organizations were not randomly sampled. This is because the present study was funded through a program announcement for health services research utilizing community treatment programs within the CTN. With that said the comparisons between our sample of treatment programs and the SAMHSA facility locator indicated considerable similarity in various program characteristics. Moreover, existing research finds few differences between counselors employed in CTN affiliated and non-CTN affiliated treatment programs (Knudsen, Ducharme, & Roman, 2007). Together this allays some concerns regarding generalizability.
Another potential limitation is the focus on individual-level effects, even though we know that clinicians are nested within treatment organizations. Examining clinician-level effects is consistent with the organizational change literature which argues that in order to understand the effects of change initiatives, it is essential to examine individual reactions because individuals working in the same organizational context can have very different reactions to change (e.g., Amiot et al., 2006; Jimmieson et al., 2004; Rafferty & Griffin, 2006). We chose to focus on clinicians as opposed management personnel because many of the changes dictated by the OASAS regulation are geared toward altering clinical practice (e.g., screening all patients at intake, integrating treatment for tobacco dependence into existing treatment planning) and patient behavior (e.g., forbidding patient smoking), which are likely to be implemented by clinicians on a daily basis. It is also important to note that we statistically controlled for organization-level effects in our analysis, eliminating any bias that might be introduced due to the nested nature of the data.
The present study is also limited to the examination of how the OASAS regulation affected the SUD workforce. It is also important to understand how the regulation affects other workforce outcomes, such as clinician smoking behavior and actual turnover, as well as patient outcomes such as smoking behavior after treatment, changes in overall patient census after the passage of the regulation, and patient reactions to the regulation. An internal report published by OASAS provides initial evidence that admissions remained stable after the implementation of the regulation, and that the percentages of patients who completed treatment or were referred remained relatively stable. In addition, a larger proportion of patients reported not smoking at the completion of treatment (Tesiny, Robinson, & Nottingham, 2010). This is consistent with the results of a qualitative study of clinician perceptions of the positive and negative effects of the OASAS regulation where the most frequently cited positive outcome by both counselors and clinical supervisors was reduced smoking among patients and staff (Eby, Sparks, Evans, & Selzer, 2012). However, this same study also found some perceived negative effects on patients (according to counselors and clinical supervisors), including addict behaviors (e.g., sneakiness, black market economy for cigarettes), interference with other treatment goals, and negative client reactions (e.g., anger, acting out). Clearly, more research is needed on both patient and clinician outcomes in order to gain a more comprehensive perspective on the gains and potential costs of going tobacco-free in SUD treatment. Finally, the null findings with regard to self-efficacy should be interpreted cautiously because this measure was modified from its original form. Rather than dismiss the importance of self-efficacy in effectively managing mandated regulatory change, additional research is needed using more psychometrically sound scales.
In closing, the NYS OASAS regulation aimed to reduce tobacco dependence in SUD patients and create healthier workplaces for clinicians. Understanding the important role that local implementation features have in efforts to create a work environment that facilitates the use of clinical practice behaviors to support smoking cessation in clients and reduce strain in response to organizational change has important implications for managing the change process.
Acknowledgments
This research was funded by a grant from the National Institutes of Health (R01 DA026291) awarded to Lillian T. Eby. The opinions expressed are those of the author and not the granting agency.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams GA, Beehr TA. Turnover and retirement: A comparison of their similarities and differences. Personnel Psychology. 1998;51:643–665. doi: 10.1111/j.1744-6570.1998.tb00255.x. [DOI] [Google Scholar]
- Alexander S, Sinclair RR, Tetrick LE. The role of organizational justice in defining and maintaining the employment relationship. In: Tetrick LE, Barling J, editors. Changing employment relations: Behavioral and social perspectives. Washington, DC: APA; 1995. pp. 61–89. [DOI] [Google Scholar]
- Amiot CE, Terry DJ, Jimmieson NL, Callan VJ. A longitudinal investigation of coping processes during a merger: Implications for job satisfaction and organizational identification. Journal of Management. 2006;32:552–574. doi: 10.1177/0149206306287542. [DOI] [Google Scholar]
- Baca CT, Yahne CE. Smoking cessation during substance abuse treatment: What you need to know. Journal of Substance Abuse Treatment. 2009;36:205–219. doi: 10.1016/j.jsat.2008.06.003. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295X.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bobo JK. Nicotine dependence and alcoholism epidemiology and treatment. Journal of Psychoactive Drugs. 1992;24:123–129. doi: 10.1080/02791072.1992.10471633. [DOI] [PubMed] [Google Scholar]
- Bobo JK, Husten C. Sociocultural influences on smoking and drinking. Alcohol Research & Health. 2000;24:225–232. http://www.niaaa.nih.gov/(Retrieved February 22, 2012) [PMC free article] [PubMed] [Google Scholar]
- Bolman LG, Deal TE. Reframing organizational change. In: Gallos JV, editor. Organizational development: A Jossey-Bass reader. San Francisco, CA: Jossey-Bass; 2006. pp. 447–469. [Google Scholar]
- Brigham J, Gross J, Stitzer ML, Felch LJ. Effects of a restricted work-site smoking policy on employees who smoke. American Journal of Public Health. 1994;84:773–778. doi: 10.2105/AJPH.84.5.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brotheridge CM. The role of fairness in mediating the effects of voice and justification on stress and other outcomes in a climate of organizational change. International Journal of Stress Management. 2003;10:253–268. doi: 10.1037/1072-5245.10.253. [DOI] [Google Scholar]
- Callaly T, Arya D. Organizational change management in mental health. Australian Psychiatry. 2005;13:120–123. doi: 10.1111/j.1440-1665.2005.02173.x. [DOI] [PubMed] [Google Scholar]
- Caplan RD, Cobb S, French JRP, Harrison RV, Pinneau SR. DHEW NIOSH Publication NO 75–160. Washington, DC: U.S. Government Printing Office; 1975. [Retrieved February 22, 2012]. Job demands and worker health: Main effects and occupational differences. http://babel.hathitrust.org. [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum; 1983. [Google Scholar]
- Cohen-Charash Y, Spector PE. The role of justice in organizations: A meta-analysis. Organizational Behavior and Human Decision Processes. 2001;86:278–321. doi: 10.1006/obhd.2001.2958. [DOI] [Google Scholar]
- Colquitt JA, Conlon DE, Wesson MJ, Poret C, Ng KY. Justice at the millennium: A meta-analytic review of 25 years of organizational justice research. Journal of Applied Psychology. 2001;86:425–445. doi: 10.1037//0021-9010.86.3.425. [DOI] [PubMed] [Google Scholar]
- Cropanzano R, Goldman BM, Benson L. Organizational justice. In: Barling J, Kelloway EK, Frone MR, editors. Handbook of work stress. Thousand Oaks, CA: Sage; 2005. pp. 63–87. [Google Scholar]
- Cunningham CE, Woodward CA, Shannon HS, MacIntosh J, Lendrum B, Rosenbloom D, Brown J. Readiness for organizational change: A longitudinal study of workplace, psychological and behavioural correlates. Journal of Occupational and Organizational Psychology. 2002;75:377–392. doi: 10.1348/096317902321119637. [DOI] [Google Scholar]
- Dalal RS. A meta-analysis of the relationship between organizational citizenship behavior and counterproductive work behavior. Journal of Applied Psychology. 2005;90:1241–1255. doi: 10.1037/0021-9010.90.6.1241. [DOI] [PubMed] [Google Scholar]
- Daly JP, Geyer PD. The role of fairness in implementing large-scale change: Employee evaluations of process and outcome in seven facility relocations. Journal of Organizational Behavior. 1994;15:623–638. doi: 10.1002/job.4030150706. [DOI] [Google Scholar]
- Eby LT, Sparks TE, Evans L, Selzer JA. A Qualitative Examination of the Positive and Negative Consequences Associated with Going Tobacco-free in Substance Abuse Treatment: The NY State Experience. Nicotine and Tobacco Research. 2012 doi: 10.1093/ntr/nts027. (available on line March, 13, 2012) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eilam G, Shamir B. Organizational change and self-concept threats. Journal of Applied Behavioral Science. 2005;41:399–421. doi: 10.1177/0021886305280865. [DOI] [Google Scholar]
- Eisenberger R, Cummings J, Armeli S, Lynch P. Perceived organizational support, discretionary treatment, and job satisfaction. Journal of Applied Psychology. 1997;82:812–820. doi: 10.1037//0021-9010.82.5.812. [DOI] [PubMed] [Google Scholar]
- Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling: A Multidisciplinary Journal. 2001;8(3):430–457. doi: 10.1207/S15328007SEM0803_5. [DOI] [Google Scholar]
- Etter J. Associations between smoking prevalence, stages of change, cigarette consumption, and quit attempts across the United States. Preventative Medicine. 2004;38:369–373. doi: 10.1016/j.ypmed.2003.11.006. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Bailey WC, Cohen SJ. Treating tobacco use and dependency: Clinical practice guidelines. Rockville, MD: U.S. Department of Health and Human Services; 2000. [Google Scholar]
- Fixsen DL, Naoom SF, Blasé KA, Friedman RM, Wallace F. Implementation research: A synthesis of the literature. Tampa, FL: University of South Florida; 1995. [Google Scholar]
- Folger R, Bies RJ. Managerial responsibilities and procedural justice. Employee Responsibilities and Rights Journal. 1989;2:79–89. doi: 10.1007/BF01384939. [DOI] [Google Scholar]
- Fugate M, Kinicki AJ, Scheck CL. Coping with an organizational merger over four stages. Personnel Psychology. 2002;55:905–928. doi: 10.1111/j.1744-6570.2002.tb00134.x. [DOI] [Google Scholar]
- Fuller BE, Guydish J, Tsoh J, Reid MS, Resnick M, Zammarelli L, Ziedonis DM, Sears C, McCarty D. Attitudes toward the integration of smoking cessation treatment into drug abuse clinics. Journal of Substance Abuse Treatment. 2007;32:53–60. doi: 10.1016/j.sat.2006.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabel S, Oster GD. Mental health providers confronting organizational change: Process, problems, and strategies. Psychiatry. 1998;61:302–316. doi: 10.1080/00332747.1998.11024842. www.ncbi.nlm.nih.gov(Retrieved February 22, 2012) [DOI] [PubMed] [Google Scholar]
- Gill BS, Bennett DL, Abu-Salha M, Fore-Arcand L. Addiction professionals’ attitudes regarding treatment of nicotine dependence. Journal of Substance Abuse Treatment. 2000;19:317–318. doi: 10.1016/S0740-5472(00)00106-9. [DOI] [PubMed] [Google Scholar]
- Gotham HJ. Advancing the implementation of evidence-based practices into clinical practice: How do we get there from here? Professional Psychology: Research and Practice. 2006;32:606–613. doi: 10.1037/0735-7028.37.6.606. [DOI] [Google Scholar]
- Greenberg J. Using socially fair treatment to promote acceptance of a work site smoking ban. Journal of Applied Psychology. 1994;79:288–297. doi: 10.1037//0021-9010.79.2.288. [DOI] [PubMed] [Google Scholar]
- Hammond GC, Gregoire T. Breaking ground in treating tobacco dependence at a women’s treatment center. Journal of Social Work Practice in the Addictions. 2011;11:1–16. doi: 10.1080/1533256X.2011.544606. [DOI] [Google Scholar]
- Herold DM, Fedor DB, Caldwell SD. Beyond change management: A multilevel investigation of contextual and personal influences on employee’ commitment to change. Journal of Applied Psychology. 2007;92:942–951. doi: 10.1037/0021-9010.92.4.942. [DOI] [PubMed] [Google Scholar]
- Hu LH, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424–453. doi: 10.1037//1082-989X.3.4.424. [DOI] [Google Scholar]
- Jimmieson NL, Terry DJ, Callan VJ. A longitudinal study of employee adaptation to organizational change: The role of change-related information and change-related self-efficacy. Journal of Occupational Health Psychology. 2004;9:11–27. doi: 10.1037/1076-8998.9.1.11. [DOI] [PubMed] [Google Scholar]
- Kernan MC, Hanges PJ. Survivor reactions to reorganization: Antecedents and consequences of procedural, interpersonal, and informational justice. Journal of Applied Psychology. 2002;87:16–928. doi: 10.1037//0021-9010.87.5.916. [DOI] [PubMed] [Google Scholar]
- Klein KJ, Sorra JS. The challenge of innovation implementation. Academy of Management Review. 1996;21:1055–1080. doi: 10.2307/259164. [DOI] [Google Scholar]
- Kline RB. Principles and Practice of Structural Equation Modeling. 3. New York, NY: The Guilford Press; 2010. [Google Scholar]
- Knudsen H, Ducharme L, Roman PM. Research participation and turnover intention: An exploratory analysis of substance abuse counselors. Journal of Substance Abuse Treatment. 2007;33:211–217. doi: 10.1016/j.jsat.2006.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen HK, Roman PM, Johnson AJ. Preliminary analyses from NIDA Grant R01DA020757, Smoking Cessation Practices in Community Treatment Programs. University of Georgia; 2009. http://cdar.uky.edu (Retrieved February 22, 2012) [Google Scholar]
- Konovsky MS, Cropanzano R. Perceived fairness and employee drug testing as a predictor of employee attitudes and performance. Journal of Applied Psychology. 1991;76:698–707. doi: 10.1037//0021-9010.76.5.698. [DOI] [PubMed] [Google Scholar]
- Kotz MM. A smoke-free chemical dependency unit: The Cleveland Clinic experience. Journal of Substance Abuse Treatment. 1993;10:125–131. doi: 10.1016/0740-5472(93)90036-2. [DOI] [PubMed] [Google Scholar]
- Lehman WEK, Greener JM, Simpson DD. Assessing organizational readiness for change. Journal of Substance Abuse. 2002;22:197–209. doi: 10.1016/S0740-5472(02)00233-7. [DOI] [PubMed] [Google Scholar]
- Leventhal GS. What should be done with equity theory? New approaches to the study of fairness in social relationships. In: Gergen K, Greenberg M, Willis R, editors. Social exchange: Advances in theory and research. New York: Plenum; 1980. pp. 27–55. [DOI] [Google Scholar]
- Lind EA, Kanfer R, Early PC. Voice, control, and procedural justice: Instrumental and noninstrumental concerns in fairness judgments. Journal of Personality and Social Psychology. 1990;59:952–959. doi: 10.1037//0021-9010.87.5.916. [DOI] [Google Scholar]
- Marsh HW, Balla JR, McDonald RP. Goodness-of-fit indexes in confirmatory factor analysis: The effect of sample size. Psychological Bulletin. 1988;103:391–410. doi: 10.1037/0033-2909.103.3.391. [DOI] [Google Scholar]
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory manual. Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1:130–149. doi: 10.1037/1082-989X.1.2.130. [DOI] [Google Scholar]
- McCarthy WJ, Zhou Y, Hser YL, Collins C. To smoke or not to smoke: Impact on disability, quality of life, and illicit drug use in baseline polydrug users. Journal of Addictive Diseases. 2002;21:35–54. doi: 10.1300/J069v21n02_04. [DOI] [PubMed] [Google Scholar]
- McIIvain HE, Bobo JK. Tobacco cessation with patients recovering from alcohol and other substance abuse. Primary Care: Clinics in Office Practice. 2005;26:671–689. doi: 10.1016/S0095-4543(05)70123-8. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 5. Los Angeles, CA: Muthén & Muthén; 1998–2008. [Google Scholar]
- Napier NK, Simmons G, Stratton K. Communication during a merger: Experience of two banks. Human Resource Planning. 1989;12:105–122. http://www.hrps.org/(Retrieved February 20, 2012) [Google Scholar]
- New York Office of Alcoholism and Substance Abuse Services. Tobacco-free services Title 14 NYCRR part 856. n.d Retrieved from http://www.oasas.ny.gov/tobacco/providers/reg856.cfm.
- Parry O, Platt S, Thomson C. Out of sight, out of mind: Workplace smoking bans and the relocation of smoking at work. Health Promotion International. 2000;15:125–133. doi: 10.1093/heapro/15.2.125. [DOI] [Google Scholar]
- Paterson JM, Green A, Cary J. The measurement of organizational justice in organizational change programmes: A reliability, validity and context sensitivity assessment. Journal of Occupational and Organizational Psychology. 2002;75:393–408. doi: 10.1348/096317902321119565. [DOI] [Google Scholar]
- Quick JC, Tetrick LE. Handbook of occupational health psychology. Washington, DC: APA; 2003. [DOI] [Google Scholar]
- Rafferty AE, Griffin MA. Perceptions of organizational change: A stress and coping perspective. Journal of Applied Psychology. 2006;91:1154–1162. doi: 10.1037/0021-9010.91.5.1154. [DOI] [PubMed] [Google Scholar]
- Reichers AE, Wanous JP, Austin JT. Understanding and managing cynicism about organizational change. Academy of Management Executive. 1997;11:48–59. doi: 10.5465/AME.1997.9707100659. [DOI] [Google Scholar]
- Reilly P, Murphy L, Alderton D. Challenging the smoking culture within a mental health service supportively. International Journal of Mental Health Nursing. 2006;15:272–278. doi: 10.1111/j.1447-0349.2006.00434.x. [DOI] [PubMed] [Google Scholar]
- Rhoades L, Eisenberger R. Perceived organizational support: A review of the literature. Journal of Applied Psychology. 2002;87:698–714. doi: 10.1037//0021-9010.87.4.698. [DOI] [PubMed] [Google Scholar]
- Richter KP, Choi WS, McCool RM, Harris KJ, Ahluwalia JS. Smoking cessation services in the U.S. methadone maintenance facilities. Psychiatric Services. 2004;55:1258–1264. doi: 10.1176/appi.ps.55.11.1258. [DOI] [PubMed] [Google Scholar]
- Richter KP, Choi WS, Alford DP. Smoking policies in U.S. outpatient drug treatment facilities. Nicotine and Tobacco Research. 2005;7:475–480. doi: 10.1080/14622200500144956. [DOI] [PubMed] [Google Scholar]
- Rogers EM. Diffusion of preventive innovations. Addictive Behaviors. 2002;27:989–993. doi: 10.1016/S0306-4603(02)00300-3. [DOI] [PubMed] [Google Scholar]
- Rosnow RL. Rumor as communication: A contextualist approach. Journal of Communication. 1988;38:12–28. doi: 10.1111/j.1460-2466.1988.tb02033.x. [DOI] [Google Scholar]
- Sadri G, Robertson IT. Self-efficacy and work-related behavior: A review and meta-analysis. Applied psychology: An international review. 1993;42:139–152. doi: 10.1111/j.1464-0597.1993.tb00728.x. [DOI] [Google Scholar]
- Sheck CL, Kinicki A. Identifying the antecedents of coping with an organizational acquisition: A structural assessment. Journal of Organizational Behavior. 2000;21:627–648. http://www.wiley.com/WileyCDA/WileyTitle/productCd-JOB.html (retrieved February 20, 2012) [Google Scholar]
- Scherbaum CA, Ferreter JM. Estimating statistical power and required sample sizes for organizational research using multilevel modeling. Organizational Research Methods. 2009;12:347–367. 0.1177/1094428107308906. [Google Scholar]
- Schweiger DM, DeNisi AS. Communicating with employees following a merger: A longitudinal field experiment. Academy of Management Journal. 1991;34:110–135. doi: 10.2307/256304. [DOI] [Google Scholar]
- Sees KL, Clark HW. When to begin smoking cessation in substance abusers. Journal of Substance Abuse Treatment. 1993;10:189–195. doi: 10.1016/0740-5472(93)90044-3. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Flynn PM. Moving innovations into treatment: A stage-based approach to program change. Journal of Substance Abuse. 2007;33:111–129. doi: 10.1016/j.jsat.2006.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JF. Index of organizational reactions (IOR) JSAS Catalog of Selected Documents in Psychology. 1976;6(1265):54. http://www.eric.ed.gov. (Retrieved February 22, 2012) [Google Scholar]
- Spector PE. A control theory of the job stress process. In: Cooper CL, editor. Theories of organizational stress. London: Oxford University Press; 1998. pp. 153–169. [Google Scholar]
- Spector PE, Fox S, Penney LM, Bruursema K, Goh A, Kessler S. The dimensionality of counterproductive behavior: Are all counterproductive behaviors created equal? Journal of Vocational Behavior. 2006;68:446–460. doi: 10.1016/j.jvb.2005.10.005. [DOI] [Google Scholar]
- Tesiny EP, Robbinson J, Nottingham WT. Tobacco regulation impact report. New York Office of Alcoholism & Substance Abuse Services, Addiction Services for Prevention, Treatment, and Recovery; Albany, NY: Nov, 2010. http://www.oasas.ny.gov/hps/evaluation/documents/Part856Impact-2010.pdf (Retrieved February 22, 2012) [Google Scholar]
- Tepper BJ. Health consequences of organizational injustice: Tests of main and interactive effects. Organizational Behavior and Human Decision Processes. 2001;86:97–215. doi: 10.1006/obhd.2001.2951. [DOI] [Google Scholar]
- Terry DJ, Jimmieson NL. A stress and coping approach to organizational change: Evidence from Three Field Studies. Australian Psychologist. 2003;38:92–101. doi: 10.1080/00050060310001707097. [DOI] [Google Scholar]
- Thibaut J, Walker L. Procedural justice: A psychological analysis. Hillsdale, NJ: Erlbaum; 1975. [Google Scholar]
- Wanberg CR, Banas JT. Predictors and outcomes of openness to change in a reorganizing workplace. Journal of Applied Psychology. 2000;85:132–142. doi: 10.1037//0021-9010.85.1.132. [DOI] [PubMed] [Google Scholar]
- White WL. Slaying the dragon: The history of addiction treatment and recovery in America. Chestnut Health Systems; 1998. [Google Scholar]
- Williams JM, Foulds J, Dwyer M, Order-Connors B, Springer M, Gaddle P, et al. The integration of tobacco dependence treatment and tobacco-free standards into residential addictions treatment in New Jersey. Journal of Substance Abuse Treatment. 2005;28:331–340. doi: 10.1016/j.jsat.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Wothke W. Longitudinal and multi-group modeling with missing data. In: Little TD, Schnabel KU, Baumert J, editors. Modeling longitudinal and multiple group data: Practical issues, applied approaches and specific examples. Mahwah, NJ: Lawrence Erlbaum Publishers; 1998. [Google Scholar]