Abstract
PURPOSE
To understand if Hispanics report health differently than other racial/ethnic groups after controlling for demographics and risk factors for poor health.
METHODS
The sample (n=5,502) included 3,201 women, 1,767 black, 1,859 white and 1,876 Hispanic subjects from the Boston Area Community Health Survey, a population-based survey of English and Spanish-speaking residents of Boston, Massachusetts, United States, age 30–79 in 2002–05. Multiple logistic regression was used to examine the association between race/ethnicity (including interview language for Hispanics) and fair/poor self-reported health (F/P SRH) adjusting for gender, age, socioeconomic status (SES), depression, nativity, and comorbidities.
RESULTS
Compared to whites, Hispanics interviewed in Spanish were seven times as likely to report F/P SRH (Odds Ratio = 7.7, 95% confidence interval 4.9, 12.2) after adjusting for potential confounders and Hispanics interviewed in English were twice as likely. In analyses stratified by depression and nativity, we observed stronger associations with Hispanic ethnicity in immigrants and non-depressed individuals interviewed in Spanish.
CONCLUSIONS
Increased odds of F/P SRH persisted in the Hispanic group even when accounting for interview language and controlling for SES, age, depression, and nativity, with language of interview mitigating the association. These findings have methodologic implications for epidemiologists using SRH across diverse populations.
MeSH Headings: Hispanic Americans, self-reported, health status, comorbidity
INTRODUCTION
Self-reported health (SRH) is a ubiquitous measure used across the spectrum of health research from clinical to epidemiologic studies. Its wide acceptance as a useful tool for assessing health is due to its ability to predict mortality (1–4) and morbidity (4) and its ease of use as a single question measure. Yet there is also evidence of significant variability in SRH across racial and ethnic groups (5–10). Specifically, Hispanic populations have repeatedly shown a tendency to report worse SRH compared to other racial/ethnic groups (6, 11). Various characteristics have been shown to affect this phenomenon including language, immigration, and acculturation (6, 12–18). Many prior studies focused on racial/ethnic differences in SRH have focused on older subjects, have limited comorbid assessments to a single condition, or have focused on two racial groups. Very few assessments of SRH have focused on number of health conditions (9, 15) to provide additional control for SRH disparities. Furthermore, most studies have used national data, which include predominantly Mexican populations, thus limiting the generalizability of Hispanic results.
The objective of the current analysis was to understand if Hispanics report health differently than other racial/ethnic groups after controlling for interview language and risk factors for poor health, such as age, socioeconomic status (SES), nativity, depression and number of comorbidities. The Boston Area Community Health (BACH) Survey provided a unique opportunity to assess this question in a diverse Hispanic population with representation from five Hispanic subgroups, as well as to compare Hispanics with both black and white individuals.
METHODS
The BACH Survey is a population-based, epidemiologic cohort study conducted among 5,502 men and women aged 30 to 79 residing in Boston, Massachusetts. A multistage, stratified cluster sampling design was used to recruit approximately equal numbers of persons in pre-specified groups defined according to age (30–39, 40–49, 50–59, 60–79), race/ethnicity (black, Hispanic, white) and gender. This analysis used baseline data collected from April 2002 to June 2005 during two-hour, in-person interviews conducted by bilingual interviewers. Interviews were completed for 63.3% of eligible persons, with a resulting study sample of 2,301 men and 3,201 women, and 1,767 black, 1,876 Hispanic and 1,859 white subjects. The Hispanic sample is predominantly Puerto Rican (N=601), Dominican (N=521), Central American (N=336), and South American (N=247). All subjects provided written informed consent and the protocols and procedures were approved by New England Research Institutes’ Institutional Review Board (19).
SRH was assessed using the general health question of the 12-Item Short Form Health Survey (SF-12) version 1 (20): “In general, would you say your health is” excellent, very good, good, fair, or poor. Responses were dichotomized into fair/poor versus good/very good/excellent.
Racial/ethnic groups were mutually exclusive and were based on self-report as black, white or Hispanic (21). If a participant identified as Hispanic and any other race, s/he was included only in the Hispanic group. Among Hispanics only, race/ethnicity was further defined by language of interview: Hispanics interviewed in Spanish (HIS) and Hispanics interviewed in English (HIE). It was infeasible to categorize white and black participants by language of interview as more than 99% were interviewed in English. Nativity was based on location of birth (US vs. not US). SES categories of low, middle, high were created using standardized income (assessed in $5,000 increments up to $10,000 and $10,000 increments up to $100,000) and education variables (assessed as total number of years of school completed) for the Northeastern US (22). Marital status was classified as married/living with a partner, single (never married), or other. Depression was defined as reporting at least five of the eight symptoms in the Center for Epidemiologic Studies Depression Scale (CES-D) (23).
Comorbidities were assessed by the question “Have you ever been told by a health care provider that you have or had…?” Conditions of interest (arthritis, asthma, chronic lung disease, diabetes (type 1 and 2), high blood pressure, and myocardial infarction [MI]) were selected based on their potential impact on quality of life, chronicity, prevalence in the overall sample (see Table 1), and proportion currently receiving treatment for that condition (range: 36% to 80%). All of these conditions have either been shown to negatively impact SRH (24–26); or have been used commonly in other studies assessing SRH in patient populations (9, 27, 28). We used a variable based on number of comorbidities in this analysis. We do not presume that each of these conditions has the same impact on perception of health, but believe that these conditions, especially in combination, would greatly impact perceived health. In some analyses, the number of conditions was dichotomized as 0–3, and 4+ based on observed differences by race/ethnicity at this cutpoint.
Table 1.
Patient Characteristics by Race/Ethnicity*
| Independent Variable | Percent of Respondents Within Category | Overall (N = 5,502) | p-value | ||
|---|---|---|---|---|---|
| Black (N = 1,767) | Hispanic (N = 1,876) | White (N = 1,859) | |||
| Self-Reported Health | < 0.001 | ||||
| Fair/Poor | 20.7 | 33.9 | 10.7 | 16.5 | |
| Excellent/Very Good/Good | 79.3 | 66.1 | 89.3 | 83.5 | |
|
| |||||
| Nativity | < 0.001 | ||||
|
| |||||
| US-born | 78.6 | 14.5 | 90.1 | 77.0 | |
| Foreign-born | 21.4 | 85.5 | 9.9 | 23.0 | |
|
| |||||
| Language of interview | < 0.001 | ||||
|
| |||||
| English | 99.7 | 35.0 | 99.8 | 91.2 | |
| Spanish | 0.3 | 65.0 | 0.2 | 8.8 | |
|
| |||||
| SES | < 0.001 | ||||
|
| |||||
| Low | 41.1 | 61.1 | 14.0 | 27.6 | |
| Medium | 49.5 | 30.6 | 49.7 | 47.1 | |
| High | 9.4 | 8.3 | 36.3 | 25.3 | |
|
| |||||
| Marital Status | < 0.001 | ||||
|
| |||||
| Married/Living with Partner | 39.0 | 53.9 | 54.2 | 50.0 | |
| Single, Never Married | 33.0 | 19.4 | 27.5 | 27.9 | |
| Other | 28.1 | 26.7 | 18.3 | 22.1 | |
|
| |||||
| Gender | 0.08 | ||||
|
| |||||
| Male | 44.4 | 47.0 | 49.7 | 47.9 | |
| Female | 55.6 | 53.0 | 50.3 | 52.1 | |
|
| |||||
| Age Group | < 0.001 | ||||
|
| |||||
| 30–39 | 33.2 | 44.7 | 34.0 | 35.2 | |
| 40–49 | 27.9 | 28.2 | 23.1 | 25.1 | |
| 50–59 | 19.8 | 15.4 | 18.0 | 18.1 | |
| 60–69 | 11.7 | 7.7 | 14.8 | 13.1 | |
| 70–79 | 7.3 | 3.9 | 10.1 | 8.5 | |
|
| |||||
| Depression Status | < 0.001 | ||||
|
| |||||
| Yes | 21.1 | 27.1 | 13.1 | 17.1 | |
| No | 78.9 | 72.9 | 86.9 | 82.9 | |
|
| |||||
| Comorbidity Category | 0.642 | ||||
|
| |||||
| 0–3 | 96.7 | 97.1 | 97.4 | 97.2 | |
| 4+ | 3.3 | 2.9 | 2.6 | 2.8 | |
|
| |||||
| Comorbidity Prevalence | |||||
|
| |||||
| Arthritis | 24.9 | 18.3 | 23.9 | 23.5 | 0.002 |
| Asthma | 19.3 | 17.0 | 15.4 | 16.7 | 0.112 |
| Chronic lung disease | 5.6 | 6.7 | 7.4 | 6.8 | 0.262 |
| Diabetes (Type 1 or 2) | 12.8 | 11.5 | 7.5 | 9.4 | < 0.001 |
| High blood pressure | 36.6 | 24.8 | 23.6 | 27.3 | < 0.001 |
| Myocardial infarction | 4.3 | 3.0 | 3.5 | 3.7 | 0.360 |
These data were weighted to the population of Boston as described in the methods section.
Univariate logistic regression models predicting the odds of F/P SRH were initially fit to establish the associations between each covariate and outcome (not shown). Multiple logistic regression (MLR) models estimating the association between race/ethnicity and dichotomous SRH were then built using a manual backward selection-type procedure. To fit parsimonious models, only variables statistically significant (P<0.05) in Wald F tests of each covariate (not accounting for multiple comparisons) were retained. We estimated separate associations for Hispanics interviewed in English and Spanish because of evidence of an effect of interview language on SRH. We examined variation in the results by covariates that we hypothesized would modify the association between race/ethnicity and SRH, including nativity and depression, through simple two-way interaction models. Significant interactions with race/ethnicity were further examined via stratified analyses. Estimates of the odds ratios (ORs) and corresponding 95% confidence intervals (CIs) are reported. Although all covariates had 1% or fewer missing observations (with the exception of income which was missing for 4%, 11%, and 3% of black, Hispanic, and white subjects respectively) multiple imputation was used to impute the missing values. Sampling weights were used to produce estimates representative of the black, Hispanic, and white Boston, MA population between the ages of 30 and 79 years (based on Boston census population in 2000). Sampling weights account for oversampling of particular age and racial/ethnic groups as well as participant non-response, and therefore all percentages reported are weighted values. Statistical analyses were conducted using SAS version 9.2 (SAS Institute, Cary, NC,) and SUDAAN version 10.0.1 (Research Triangle Institute, Research Triangle Park, NC).
RESULTS
Overall, 16.5% of the population reported F/P SRH, 23.0% were foreign-born, 8.8% were interviewed in Spanish, 27.6% had low SES, 50.0% were married or living with a partner, 52.1% were female, 60.3% were under 50 years old, 17.1% met the definition for current depression, and 2.8% reported four or more of the selected comorbidities (Table 1). All characteristics except gender and the number of comorbidities were significantly different by racial/ethnic group. Independent pairwise comparisons (not shown) confirmed that the proportion of Hispanics in each of the following covariate subgroups was significantly higher than for black or white subjects: F/P SRH, foreign-born, Spanish language of interview, low SES, age less than 40 years, and current depression. Hispanic subjects, however, were no more likely to report ≥4 comorbidities than blacks or whites.
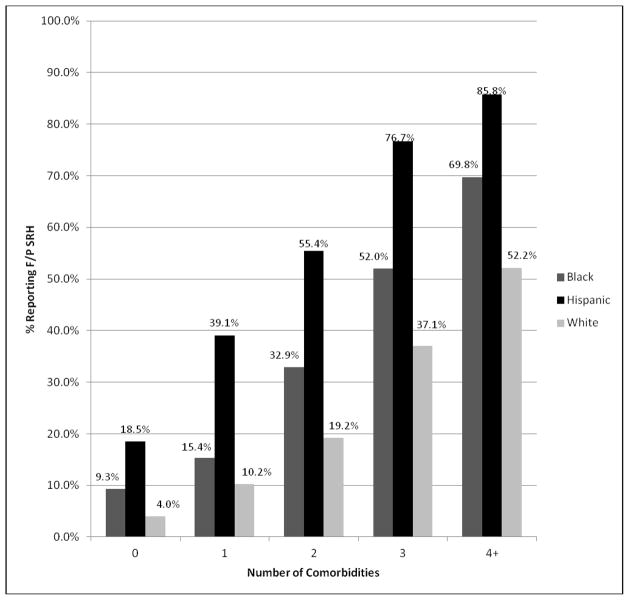
For all race/ethnic groups, the proportion reporting F/P SRH increased with increasing number of comorbidities (Figure 1). For any given number of comorbidities, black and Hispanic subjects reported F/P SRH more often than white subjects. Of the three groups, Hispanic subjects consistently reported the highest levels of F/P SRH at every level of comorbidity, with the largest differences observed between Hispanic and white subjects. The most striking difference appears in those reporting 3 comorbidities: 76.7% of Hispanic subjects reported F/P SRH compared to 52.0% of black subjects and 37.1% of white subjects. As the differences were statistically significant for subjects reporting 0–3 but not ≥ 4 comorbidities, we dichotomized the number of cormorbidities based on significance.
Figure 1. Fair/Poor SRH by Race/ethnicity and Number of Major Comorbidities.
Differences are significant at the p =<0.5 for number of comorbidities 0, 1, 2, 3.
The main model (Table 2) includes all covariates considered except for marital status and gender, which were not significantly associated with reporting F/P SRH. After adjustment for other variables included in the model, black race/ethnicity (OR=1.74, 95% CI 1.31, 2.29) and Hispanic race/ethnicity interviewed in either language (HIE OR=2.33, 95% CI 1.41, 3.83; HIS OR=7.74, 95% CI 4.89, 12.24) were associated with reporting F/P SRH, compared with whites.
Table 2.
Multiple Logistic Regression Analysis of Fair/Poor Self-Reported Health Status
| Independent Variable | Odds Ratio (N = 5,502) | ||
|---|---|---|---|
| Estimate | Lower 95% | Upper 95% | |
| Race/Ethnicity/Language* | |||
|
| |||
| Black | 1.74 | 1.31 | 2.29 |
| Hispanic - English | 2.33 | 1.41 | 3.83 |
| Hispanic - Spanish | 7.74 | 4.89 | 12.24 |
| White (Reference) | 1.00 | ||
|
| |||
| Nativity | |||
|
| |||
| US-born | 1.71 | 1.21 | 2.43 |
| Foreign-born (Reference) | 1.00 | ||
|
| |||
| SES | |||
|
| |||
| Low | 2.73 | 1.78 | 4.17 |
| Medium | 1.34 | 0.89 | 2.04 |
| High (Reference) | 1.00 | ||
|
| |||
| Age Group | |||
|
| |||
| 70–79 | 6.07 | 3.82 | 9.65 |
| 60–69 | 5.04 | 3.20 | 7.93 |
| 50–59 | 4.14 | 2.77 | 6.18 |
| 40–49 | 3.13 | 2.10 | 4.67 |
| 30–39 (Reference) | 1.00 | ||
|
| |||
| Depression Status | |||
|
| |||
| Yes | 5.39 | 4.16 | 6.97 |
| No (Reference) | 1.00 | ||
|
| |||
| Comorbidity Category | |||
|
| |||
| 4+ | 3.85 | 2.22 | 6.69 |
| 0–3 (Reference) | 1.00 | ||
Language of interview for Hispanics
Subjects who were US-born (OR=1.71, 95% CI 1.21, 2.43) were more likely to report F/P SRH than foreign-born respondents. Only the low SES category was associated with F/P SRH (OR=2.73, 95% CI 1.78, 4.17). Subjects classified as depressed had one of the strongest associations with F/P SRH (OR=5.39, 95% CI 4.16, 6.97) compared to those not depressed. Reporting ≥4 comorbidities was also strongly associated with F/P SRH (OR=3.85, 95% CI 2.22, 6.69). A secondary model treating comorbidity category as a 5-level variable (0, 1, 2, 3, 4+) yielded estimates for that did not differ appreciably from the dichotomized results (not shown).
Interactions between race/ethnicity and each covariate in Table 2 were tested. We observed significant interactions between race and nativity (P<0.04) and race and depression status (P=0.01), but no evidence of a three-way interaction between race, nativity, and depression (P=0.46). While most covariates positively associated with reporting F/P SRH remained significant for both US-born and foreign-born subjects, the magnitude of the association differed by nativity (Table 3). Specifically, this model showed a stronger association among Hispanics interviewed in Spanish vs. English in foreign-born subjects. In the US-born population, subjects with black race and HIS were more likely to have F/P SRH.
Table 3.
Multiple Logistic Regression Analysis of Fair/Poor Self-Reported Health Status, Stratified by Nativity
| Independent Variable | US-born (N=3,267) | Foreign-born (N=2,235) | ||||
|---|---|---|---|---|---|---|
| OR | Lower 95% | Upper 95% | OR | Lower 95% | Upper 95% | |
| Race/Ethnicity/Language | ||||||
|
| ||||||
| Black | 1.83 | 1.34 | 2.49 | 1.12 | 0.56 | 2.25 |
| Hispanic - English | 1.97 | 0.89 | 4.35 | 2.40 | 1.08 | 5.34 |
| Hispanic - Spanish | 3.32 | 1.16 | 9.51 | 7.09 | 3.75 | 13.37 |
| White (Reference) | 1.00 | 1.00 | ||||
|
| ||||||
| SES | ||||||
|
| ||||||
| Low | 2.82 | 1.77 | 4.49 | 2.31 | 0.88 | 6.05 |
| Medium | 1.33 | 0.84 | 2.11 | 1.32 | 0.50 | 3.51 |
| High (Reference) | 1.00 | 1.00 | ||||
|
| ||||||
| Age Group | ||||||
|
| ||||||
| 70–79 | 6.19 | 3.45 | 11.10 | 6.87 | 3.07 | 15.39 |
| 60–69 | 5.17 | 2.91 | 9.18 | 5.14 | 2.78 | 9.50 |
| 50–59 | 4.27 | 2.47 | 7.38 | 4.02 | 2.40 | 6.71 |
| 40–49 | 3.47 | 1.98 | 6.07 | 2.51 | 1.58 | 3.99 |
| 30–39 (Reference) | 1.00 | 1.00 | ||||
|
| ||||||
| Depression Status | ||||||
|
| ||||||
| Yes | 6.14 | 4.42 | 8.51 | 3.87 | 2.69 | 5.56 |
| No (Reference) | 1.00 | 1.00 | ||||
|
| ||||||
| Comorbidity Category | ||||||
|
| ||||||
| 4+ | 3.58 | 1.87 | 6.84 | 5.65 | 2.35 | 13.57 |
| 0–3 (Reference) | 1.00 | 1.00 | ||||
Language of interview for Hispanics
The results among non-depressed individuals (Table 4) were similar to those for all subjects combined. In contrast, within the depressed group, only HIS, age and ≥4 comorbidities remained significantly associated with F/P SRH. While HIS remained associated with F/P SRH in both the depressed and non-depressed, the association was stronger in non-depressed.
Table 4.
Multiple Logistic Regression Analysis of Fair/Poor Self-Reported Health Status, Stratified by Depression Status
| Independent Variable | Depressed (N=1,220) | Not Depressed (N=4,282) | ||||
|---|---|---|---|---|---|---|
| OR | Lower 95% | Upper 95% | OR | Lower 95% | Upper 95% | |
| Race/Ethnicity/Language* | ||||||
|
| ||||||
| Black | 1.17 | 0.69 | 1.99 | 2.16 | 1.53 | 3.05 |
| Hispanic - English | 1.41 | 0.68 | 2.95 | 3.52 | 1.92 | 6.46 |
| Hispanic - Spanish | 4.37 | 2.02 | 9.43 | 10.49 | 5.92 | 18.59 |
| White (Reference) | 1.00 | 1.00 | ||||
|
| ||||||
| Nativity | ||||||
|
| ||||||
| US-born | 1.62 | 0.95 | 2.77 | 1.79 | 1.15 | 2.76 |
| Foreign-born (Reference) | 1.00 | 1.00 | ||||
|
| ||||||
| SES | ||||||
|
| ||||||
| Low | 1.39 | 0.51 | 3.79 | 3.36 | 2.07 | 5.44 |
| Medium | 0.93 | 0.33 | 2.61 | 1.40 | 0.86 | 2.28 |
| High (Reference) | 1.00 | 1.00 | ||||
|
| ||||||
| Age Group | ||||||
|
| ||||||
| 70–79 | 6.19 | 2.36 | 16.22 | 6.26 | 3.98 | 9.82 |
| 60–69 | 2.96 | 1.31 | 6.66 | 6.14 | 3.94 | 9.57 |
| 50–59 | 4.67 | 2.32 | 9.43 | 3.85 | 2.55 | 5.82 |
| 40–49 | 3.26 | 1.57 | 6.79 | 3.10 | 2.10 | 4.57 |
| 30–39 (Reference) | 1.00 | 1.00 | ||||
|
| ||||||
| Comorbidity Category | ||||||
|
| ||||||
| 4+ | 2.91 | 1.26 | 6.71 | 4.91 | 2.48 | 9.73 |
| 0–3 (Reference) | 1.00 | 1.00 | ||||
Language of interview for Hispanics
Given the heterogeneity of the Hispanic population, we tested the main model (without language) with each of the five Hispanic subgroups represented in the study sample and found that each subgroup was more likely to report F/P SRH than white respondents (not shown). In a second analysis among Hispanics only, the main model, tested on the five Hispanic subgroups, (referent=South American) found that no subgroup had a significant OR for F/P SRH compared to the referent group (not shown). A final Hispanic-only model included each of the five subgroups and language as a separate variable in the MLR analysis (Table 5). In this model, Puerto Rican ethnicity, Spanish interview, age, depression and 4 or more comorbidities are associated with F/P SRH. SES and nativity no longer predicted F/P SRH in any of these analyses.
Table 5.
Multiple Logistic Regression Analysis of Fair/Poor Self-Reported Health Status with Differentiated Hispanic Subgroups
| Independent Variable | Odds Ratio (N=1,876) | ||
|---|---|---|---|
| Estimate | Lower 95% | Upper 95% | |
| Race/Ethnicity | |||
|
| |||
| Puerto Rican | 2.10 | 1.02 | 4.33 |
| Central American | 1.80 | 0.87 | 3.74 |
| Dominican | 1.65 | 0.84 | 3.25 |
| Other Hispanic | 2.95 | 1.00 | 8.69 |
| South American (Reference) | 1.00 | ||
|
| |||
| Nativity | |||
|
| |||
| US-born | 0.98 | 0.47 | 2.07 |
| Foreign-born (Reference) | 1.00 | ||
|
| |||
| Language of Interview | |||
|
| |||
| Spanish | 3.11 | 1.83 | 5.30 |
| English | 1.00 | ||
|
| |||
| SES | |||
|
| |||
| Low | 3.02 | 0.71 | 12.82 |
| Medium | 1.51 | 0.35 | 6.60 |
| High (Reference) | 1.00 | ||
|
| |||
| Age Group | |||
|
| |||
| 70–79 | 3.55 | 1.17 | 10.76 |
| 60–69 | 4.89 | 2.66 | 8.99 |
| 50–59 | 3.67 | 2.27 | 5.92 |
| 40–49 | 2.45 | 1.53 | 3.94 |
| 30–39 (Reference) | 1.00 | ||
|
| |||
| Depression Status | |||
|
| |||
| Yes | 2.89 | 1.98 | 4.22 |
| No (Reference) | 1.00 | ||
|
| |||
| Comorbidity Category | |||
|
| |||
| 4+ | 6.21 | 2.40 | 16.03 |
| 0–3 (Reference) | 1.00 | ||
DISCUSSION
The primary importance of this analysis is that it adds to the scarce literature on SRH disparities that include in-depth analysis of number of comorbidities and language of interview. Furthermore, it complements these few existing studies by including under-represented Hispanic subpopulations and a wide age range. A notable finding of our analysis is that even after adjustment for the presence of ≥4 comorbidities, Hispanic subjects were 2–8 times more likely to report F/P SRH compared to white subjects, depending on the language of interview.
This analysis identified several factors that increased the odds of reporting F/P SRH: black or Hispanic race/ethnicity (interviewed in either language), being born in the US, low SES, increasing age, depressive symptoms, and presence of ≥4 comorbidities. Even after accounting for these covariates, black and Hispanic subjects remained more likely to report F/P SRH than white subjects, with stronger associations for the Hispanic groups, especially those interviewed in Spanish. While there were differences between each Hispanic subgroup and the white reference group, no significant differences between the Hispanic subgroups were identified. When focusing on the Hispanic population, language of interview remained strongly associated with F/P SRH while SES, nativity and Hispanic subgroup were not associated with F/P SRH (with the exception of the Puerto Rican subgroup).
Stratified analyses suggested that depression and being US-born modify the influence of Hispanic ethnicity on F/P SRH for those interviewed in Spanish. For US-born or depressed subjects, Hispanic ethnicity was not associated with F/P SRH for those Hispanics interviewed in English. In analyses stratified by nativity, Hispanic ethnicity was strongly associated with F/P SRH in foreign-born subjects. This result differs from other studies that found that foreign-born Hispanics either reported better SRH (15) or had lower odds of reporting F/P SRH (12) in comparison to their US-born counterparts. Those studies were based on nationally representative data sets (Current Population Survey and National Health Interview Surveys) and nationally Mexicans comprise the majority of the Hispanic population. The BACH dataset is predominantly Dominican and Puerto Rican and our findings are consistent with Jerant et al.’s study which reported that US-born Dominicans expressed better mental health status than their foreign-born counterparts, and US-born Puerto Ricans expressed better physical health status than their foreign-born counterparts (16). Being US-born may reduce the differences in SRH between certain Hispanic populations and other US-born groups, which is consistent with other studies that have shown that acculturation appeared to reduce differences in SRH reporting (12, 17). In contrast, we found the opposite for black subjects, where the odds of reporting F/P SRH were stronger only among US-born subjects. These findings indicate that nativity may have a different influence on black versus Hispanic populations in relation to SRH.
One potential explanation for the observed disparity in SRH is a ‘cut-point shift’, which occurs when a group or population defines the response scale differently than another population. This concept has been postulated to explain differences in SRH by age (24), gender (29), and SES (2). It may be useful to test this concept in relation to SRH differences between Hispanic and non-Hispanic populations. We were unable to test this in the BACH sample because the data are predominantly self-reported, whereas this type of analysis requires objective measures of physical function such as vision, hearing and walking tests (2, 24).
Another explanation for the strong association of Spanish interview and F/P SRH could be the inherent meaning of response options. Many studies group SRH responses into positive responses (“Excellent”, “Very Good” and “Good”) vs. negative responses (“Fair” and “Poor”), thus putting the threshold for positive or negative health between “Good” and “Fair”. The inherent meaning of the words used for these response options may be different between Hispanic and non-Hispanic populations, possibly due to language, culture or both (30). Viruell-Fuentes et al. (31) found, similar to our analysis, that accounting for language of interview reduced the disparity in F/P SRH reporting, with Hispanics who were interviewed in Spanish more likely to report fair health than those interviewed in English.
The location of the SRH question has also been shown to affect reporting in Spanish speaking women. Lee and Grant (32) found that placement of the SRH question after reviewing comorbidities was associated with decreased reporting of F/P SRH in Spanish language interviews but not in English language interviews. In BACH the question on SRH is asked prior to reviewing health conditions. We were unable to examine whether placement of the question affected reporting F/P SRH because all interviews, regardless of language, asked the question at the same point in the interview.
A potential limitation of the analysis was the number of comorbidities was based on self-reported diagnoses, rather than review of medical records and the agreement between self-reported diagnoses and medical records varies by condition (33–35). Given that this analysis included several comorbidities and does not assess SRH by type of condition but rather by number of conditions, this limitation was expected to have minimal effect on the interpretation of the findings. The selection of comorbidities for this analysis was consistent with similar published analyses and was based on perceived impact on SRH. While this analysis assumed that the conditions selected would negatively impact SRH, the selection may influence the results in unknown directions. We tested the impact of history of cancer on the main model and found that it did not predict F/P SRH nor did its inclusion significantly change the odds of reporting F/P SRH (not shown). The cross-sectional nature of our analysis may be considered a limitation, as it is impossible to determine the temporal relationship between SRH and the impact of preexisting conditions or other factors such as nativity, age, etc. However, in this analysis we were interested in the current factors impacting SRH, rather than anything related to incidence where a prospective design would be more suitable.
Our ability to produce findings generalizable to Boston, MA (19), is a strength because of the scarcity of studies assessing SRH in a northeast Hispanic population. The US Hispanic population is incredibly diverse in regard to country of origin and its composition varies regionally across the nation. It has been noted that this heterogeneity must be taken into account whenever assessing Hispanic health (16, 36). Our analysis is unique in that it included a diverse group of Hispanics, with significant representation of Puerto Rican and Dominican populations, who are less often the focus of research on SRH.
CONCLUSION
In summary, we found that even when accounting for the number of major comorbidities, depression status, language of interview, and demographic variables, black and Hispanic racial/ethnic groups were more likely to report F/P SRH than whites, with the association strongest in Hispanics, and especially in those Hispanics interviewed in Spanish. The association of race/ethnicity on SRH was also found to differ by depression and nativity. The difference in magnitude of the association of Hispanic ethnicity and F/P SRH compared to white when stratified by interview language suggests that language must be considered in any assessment of SRH among Hispanics. Even when accounting for interview language and controlling for comorbidity, the persistent F/P SRH disparity between Hispanic and other racial/ethnic groups indicates that great care should be taken when comparing SRH across these populations. The predictive power of SRH may be different across populations, particularly in the case of Hispanics where the high proportion of F/P responses does not indicate a population burdened with illness and doomed to death (37). Further research on the predictive power of SRH and cut-point shifts across racial/ethnic populations may lead to a better understanding and more accurate utilization of this health assessment tool.
Acknowledgments
The project described was supported by Award Number U01DK056842 from the National Institute Of Diabetes And Digestive And Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute Of Diabetes And Digestive And Kidney Diseases or the National Institutes of Health.
We would like to acknowledge the technical support given to this paper by Ms. Deborah Brander.
LIST OF ABBREVIATIONS AND ACRONYMS
- BACH
Boston Area Community Health Survey
- CES-D
Center for Epidemiologic Studies Depression Scale
- CI
Confidence interval
- F/P SRH
Fair/Poor Self-reported health
- HIE
Hispanics Interviewed in English
- HIS
Hispanics Interviewed in Spanish
- MLR
Multiple Logistic Regression, OR, Odds ratio
- SES
Socioeconomic Status
- SRH
Self-reported health
- US
United States
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.McGee DL, Liao Y, Cao G, Cooper RS. Self-reported health status and mortality in a multiethnic US cohort. Am J Epidemiol. 1999;149(1):41–6. doi: 10.1093/oxfordjournals.aje.a009725. [DOI] [PubMed] [Google Scholar]
- 2.Dowd JB, Zajacova A. Does the predictive power of self-rated health for subsequent mortality risk vary by socioeconomic status in the US? Int J Epidemiol. 2007;36(6):1214–21. doi: 10.1093/ije/dym214. [DOI] [PubMed] [Google Scholar]
- 3.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- 4.Idler EL, Russell LB, Davis D. Survival, functional limitations, and self-rated health in the NHANES I Epidemiologic Follow-up Study, 1992. First National Health and Nutrition Examination Survey. Am J Epidemiol. 2000;152(9):874–83. doi: 10.1093/aje/152.9.874. [DOI] [PubMed] [Google Scholar]
- 5.Shetterly SM, Baxter J, Mason LD, Hamman RF. Self-rated health among Hispanic vs non-Hispanic white adults: the San Luis Valley Health and Aging Study. Am J Public Health. 1996;86(12):1798–801. doi: 10.2105/ajph.86.12.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Borrell LN, Dallo FJ. Self-rated health and race among Hispanic and non-Hispanic adults. J Immigr Minor Health. 2008;10(3):229–38. doi: 10.1007/s10903-007-9074-6. [DOI] [PubMed] [Google Scholar]
- 7.Banerjee D, Perry M, Tran D, Arafat R. Self-reported health, functional status and chronic disease in community dwelling older adults: untangling the role of demographics. J Community Health. 2010;35(2):135–41. doi: 10.1007/s10900-009-9208-y. [DOI] [PubMed] [Google Scholar]
- 8.Spencer SM, Schulz R, Rooks RN, Albert SM, Thorpe RJ, Jr, Brenes GA, et al. Racial differences in self-rated health at similar levels of physical functioning: an examination of health pessimism in the health, aging, and body composition study. J Gerontol B Psychol Sci Soc Sci. 2009;64(1):87–94. doi: 10.1093/geronb/gbn007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang J, Quinones AR, Bennett JM, Ye W, Xu X, Shaw BA, et al. Evolving Self-Rated Health in Middle and Old Age: How Does it Differ Across Black, Hispanic, and White Americans? J Aging Health. 2010;22(1):3–26. doi: 10.1177/0898264309348877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi L, Green LH, Kazakova S. Primary care experience and racial disparities in self-reported health status. J Am Board Fam Pract. 2004;17(6):443–52. doi: 10.3122/jabfm.17.6.443. [DOI] [PubMed] [Google Scholar]
- 11.Lorraine PJ, Hammock RL, Blanton JM. Predictors of self-rated health status among Texas residents. Prev Chronic Dis. 2005;2(4):A12. [PMC free article] [PubMed] [Google Scholar]
- 12.Acevedo-Garcia D, Bates LM, Osypuk TL, McArdle N. The effect of immigrant generation and duration on self-rated health among US adults 2003–2007. Soc Sci Med. 2010;71(6):1161–72. doi: 10.1016/j.socscimed.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 13.Bzostek S, Goldman N, Pebley A. Why do Hispanics in the USA report poor health? Soc Sci Med. 2007;65(5):990–1003. doi: 10.1016/j.socscimed.2007.04.028. [DOI] [PubMed] [Google Scholar]
- 14.Franzini L, Fernandez-Esquer ME. The association of subjective social status and health in low-income Mexican-origin individuals in Texas. Soc Sci Med. 2006;63(3):788–804. doi: 10.1016/j.socscimed.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 15.Huh J, Prause JA, Dooley CD. The impact of nativity on chronic diseases, self-rated health and comorbidity status of Asian and Hispanic immigrants. J Immigr Minor Health. 2008;10(2):103–18. doi: 10.1007/s10903-007-9065-7. [DOI] [PubMed] [Google Scholar]
- 16.Jerant A, Arellanes R, Franks P. Health status among US Hispanics: ethnic variation, nativity, and language moderation. Med Care. 2008;46(7):709–17. doi: 10.1097/MLR.0b013e3181789431. [DOI] [PubMed] [Google Scholar]
- 17.Johnson KL, Carroll JF, Fulda KG, Cardarelli K, Cardarelli R. Acculturation and self-reported health among Hispanics using a socio-behavioral model: the North Texas Healthy Heart Study. BMC Public Health. 2010;10:53. doi: 10.1186/1471-2458-10-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mulvaney-Day NE, Alegria M, Sribney W. Social cohesion, social support, and health among Latinos in the United States. Soc Sci Med. 2007;64(2):477–95. doi: 10.1016/j.socscimed.2006.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McKinlay JB, Link CL. Measuring the urologic iceberg: design and implementation of the Boston Area Community Health (BACH) Survey. Eur Urol. 2007;52(2):389–96. doi: 10.1016/j.eururo.2007.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Executive Office of the President of the United States: Office of Management and Budget. Federal Register Notice: Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity [Web page] Executive Office of the President of the United States: Office of Management and Budget; 1997. [updated 1997; cited 2008 January 25]; October 30, 1997:[Available from: http://www.whitehouse.gov/omb/fedreg/1997standards.html. [Google Scholar]
- 22.Green LW. Manual for scoring socioeconomic status for research on health behavior. Public Health Rep. 1970;85(9):815–27. [PMC free article] [PubMed] [Google Scholar]
- 23.Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. Int Psychogeriatr. 1999;11(2):139–48. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- 24.Tsai J, Ford ES, Li C, Zhao G, Balluz LS. Physical activity and optimal self-rated health of adults with and without diabetes. BMC Public Health. 10:365. doi: 10.1186/1471-2458-10-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arif AA, Rohrer JE, Delclos GL. A population-based study of asthma, quality of life, and occupation among elderly Hispanic and non-Hispanic whites: a cross-sectional investigation. BMC Public Health. 2005;5:97. doi: 10.1186/1471-2458-5-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Katz P, Morris A, Gregorich S, Yazdany J, Eisner M, Yelin E, et al. Valued life activity disability played a significant role in self-rated health among adults with chronic health conditions. J Clin Epidemiol. 2009;62(2):158–66. doi: 10.1016/j.jclinepi.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martinez DJ, Kasl SV, Gill TM, Barry LC. Longitudinal association between self-rated health and timed gait among older persons. J Gerontol B Psychol Sci Soc Sci. 65(6):715–9. doi: 10.1093/geronb/gbp115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller TR, Wolinsky FD. Self-rated health trajectories and mortality among older adults. J Gerontol B Psychol Sci Soc Sci. 2007;62(1):S22–7. doi: 10.1093/geronb/62.1.s22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lindeboom M, van Doorslaer E. Cut-point shift and index shift in self-reported health. J Health Econ. 2004;23(6):1083–99. doi: 10.1016/j.jhealeco.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 30.Angel R, Guarnaccia PJ. Mind, body, and culture: somatization among Hispanics. Soc Sci Med. 1989;28(12):1229–38. doi: 10.1016/0277-9536(89)90341-9. [DOI] [PubMed] [Google Scholar]
- 31.Viruell-Fuentes EA, Morenoff JD, Williams DR, House JS. Language of interview, self-rated health, and the other Latino health puzzle. Am J Public Health. 101(7):1306–13. doi: 10.2105/AJPH.2009.175455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee S, Grant D. The effect of question order on self-rated general health status in a multilingual survey context. Am J Epidemiol. 2009;169(12):1525–30. doi: 10.1093/aje/kwp070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bergmann MM, Byers T, Freedman DS, Mokdad A. Validity of self-reported diagnoses leading to hospitalization: a comparison of self-reports with hospital records in a prospective study of American adults. Am J Epidemiol. 1998;147(10):969–77. doi: 10.1093/oxfordjournals.aje.a009387. [DOI] [PubMed] [Google Scholar]
- 34.Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57(10):1096–103. doi: 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 35.St Sauver JL, Hagen PT, Cha SS, Bagniewski SM, Mandrekar JN, Curoe AM, et al. Agreement between patient reports of cardiovascular disease and patient medical records. Mayo Clin Proc. 2005;80(2):203–10. doi: 10.4065/80.2.203. [DOI] [PubMed] [Google Scholar]
- 36.Weinick RM, Jacobs EA, Stone LC, Ortega AN, Burstin H. Hispanic healthcare disparities: challenging the myth of a monolithic Hispanic population. Med Care. 2004;42(4):313–20. doi: 10.1097/01.mlr.0000118705.27241.7c. [DOI] [PubMed] [Google Scholar]
- 37.Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41(3):385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]