Abstract
Background:
This article examines the value of morbidity and mortality (M&M) conferences, and the multiple factors that contribute to their efficacy. Physicians’ morbidity and mortality conferences (M&MCs) focus on education by reviewing individual adverse events (AE), M&M. Alternatively, Quality Assurance (QA) conferences better examine system-wide issues (e.g., the role institutions play) in attaining or maintaining acceptable levels of patient care. Other issues examined in this review include: whether prospective vs. retrospective M&M data collection are more accurate, and how most states offer ‘nondiscovery’ of M&M proceedings.
Methods:
Most studies emphasize the educational role of M&MCs, and differentiate their role from QA. Studies comparing the accuracy of prospective vs. retrospective collection of M&M data were reviewed along with the medicolegal issues surrounding the protection of M&M data (‘nondiscovery’).
Results:
Multiple review articles emphasized that QA conferences typically identify system-wide failures (e.g., hospital policies) while M&MCs focus on physicians’ AE/morbidity/mortality. Additionally, the prospective collection of M&M data proved to be more accurate than retrospective analysis. Finally, most states protect M&M confidentiality (‘nondisclosure’); a glaring exception is Florida, ‘The Sunshine State,’ that allows ‘full disclosure.’
Conclusion:
This study reviews how M&MCs, differentiated from QA meetings, and educate physicians. It also documents how prospective collection of M&M data is more accurate than retrospective analysis. Additionally, it documents how in most states, medicolegal protections against discovery are in place, with Florida, the ‘Sunshine State’ remaining a glaring exception.
Keywords: Attendance revival, conferences, medicolegal requirements, morbidity, mortality, spinal surgery
INTRODUCTION
In surgical and other departments, morbidity and mortality (M&M) conferences are critical for the ongoing education of physicians, resident, nurses, physician assistants, and other adjunctive health care personnel. They provide an invaluable forum for ‘cross talk’ between disciplines, and facilitate the coalescence of cumulative learning and experiences. Their aim is to both maintain and improve the quality of patient care, by enabling physicians and colleagues to acknowledge adverse events (AE)/medical errors that result in morbidity or mortality; such recognition should limit/eliminate some of these events in the future.
This review was undertaken to reassess the value and function (e.g., running of, participation in) of morbidity and mortality conferences (M&MCs). M&MCs aims/functions differ from Quality Assurance (QA) and nursing ‘Best Practice’ conferences, as M&M review individuals’ AE/complications, morbidity, and mortality, and serve to educate physicians, residents, nurses, and other healthcare personnel directly involved in patient care. One basic premise is that greater recognition of prior mistakes offers the opportunity, in the future, to avoid them, and thus, improve patient care. Additionally, the literature regarding whether M&M data are more accurately recorded prospectively vs. retrieved retrospectively was assessed, along with a brief evaluation of the medicolegal provisions in different states for protection (‘nondiscovery’ vs. ‘full discovery’) of M&M proceedings.
MATERIALS AND METHODS
Defining quality assurance
QA Conferences do not share the same goals as M&MCs. Hospitals set up QA programs to routinely evaluate the quality of medical and/or nursing care, and to document that sufficient measures are taken to attain the best result, while avoiding ‘unanticipated’ complications. QA measures are typically system-wide rather that physician specific. QA addresses issues like those raised by the Institute of Medicine (IOM) study that documented that between 44,000 and 98,000 in-hospital deaths occur/year secondary to ‘faulty systems, process, and conditions,’ not just human error.[17] Alternatively, M&M are directed at discerning physician specific medical/surgical AE/morbidity, mortality, and educating, through shared ‘open discussion’ how to avoid these complications in the future.
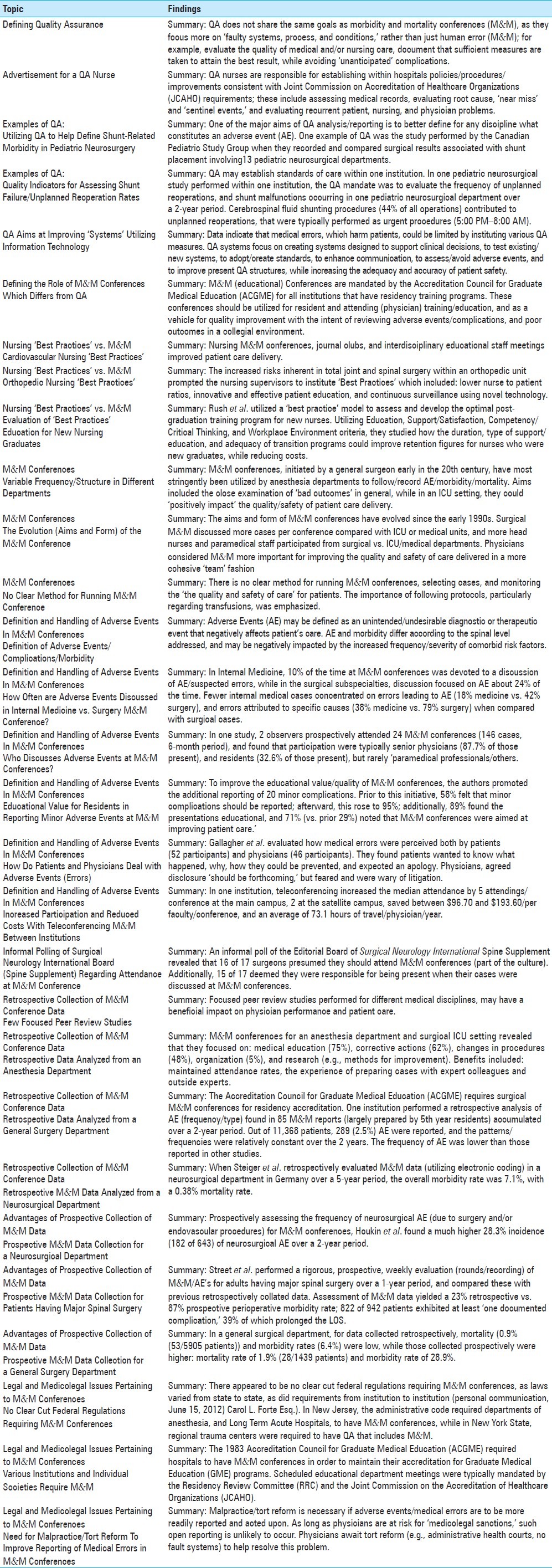
Summary: QA does not share the same goals as M&MCs, as they focus more on ‘faulty systems, process, and conditions,’ rather than just human error (M&M); for example, evaluate the quality of medical and/or nursing care, document that sufficient measures are taken to attain the best result, while avoiding ‘unanticipated’ complications [Tables 1 and 2].
Table 1.
Results of questionnaire regarding morbidity mortality conferences
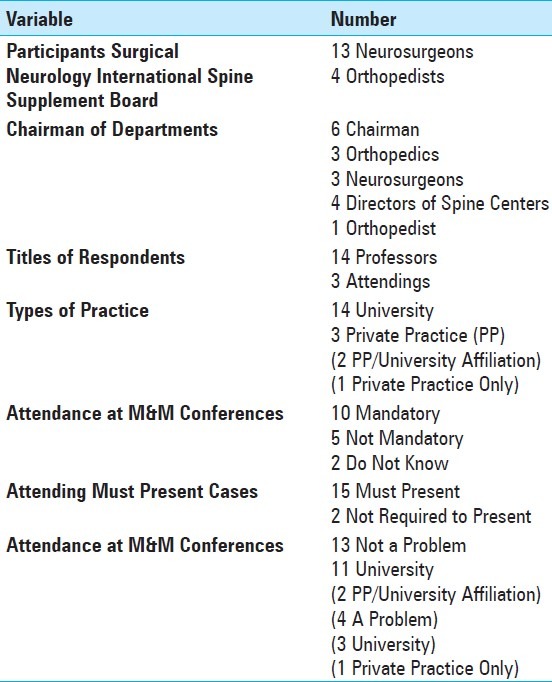
Table 2.
Summary of Topics and Findings
Advertisement for a Quality Assurance nurse
This advertisement for a QA nurse (www.co.monterey.ca.us/personnel/documents/) at the Natividad Medical Center (NMC) in California summarizes the multiple factors that comprise the typical QA nurse's job description. They must be registered nurses with ‘at least 3-5 years experience in process improvement.’ Their multiple responsibilities include: design and implementation of QA policies/procedures/improvements consistent with Joint Commission on Accreditation of Healthcare Organizations (JCAHO) requirements, assess patients medical records using QA criteria (make recommendations for physician peer review), investigate root cause, ‘near miss’ and ‘sentinel events,’ review state regulations/policies, educate staff regarding these policies, evaluate ‘recurrent patient problems,’ and finally ‘participate in nursing and physician staff meetings for information gathering and consultation.’
Summary: QA nurses are responsible for establishing within hospitals policies/procedures/improvements consistent with JCAHO requirements; these include assessing medical records, evaluating root cause, ‘near miss’ and ‘sentinel events,’ and evaluating recurrent patient/nursing/physician problems [Table 2].
Examples of Quality Assurance: Utilizing Quality Assurance to help define shunt-related morbidity in pediatric neurosurgery
One of the major aims of QA analysis/reporting is to better define, for any discipline, what constitutes an AE. In the field of pediatric neurosurgery, Drake et al. utilized data collected by the Canadian Pediatric Neurosurgery Study Group, from 13 Canadian pediatric neurosurgical departments, to accurately record and compare surgical results associated with shunt placement.[5] They more clearly defined ‘adverse events’ (utilizing data from randomized trials, prospective series, and the literature) attributed to shunt placement/shunt failure: obstruction/malfunction, infections (shunt/wound infections), and postoperative neurological deficits. They applied their expanded definition of shunt failure to M&M data collection within their society, allowing for better comparisons of data between sites, and to ‘allow significant variations in outcomes to be identified and acted upon.’
Summary: One of the major aims of QA analysis/reporting is to better define for any discipline what constitutes an AE. One example of QA was the study performed by the Canadian Pediatric Study Group when they recorded and compared surgical results associated with shunt placement involving 13 pediatric neurosurgical departments [Table 2].
Examples of Quality Assurance: Quality indicators for assessing shunt failure/unplanned reoperation rates
QA may be utilized to establish standards of care within or between institutions. For example, Mukerji et al. looked at the frequency of unplanned reoperations in pediatric neurosurgery in one institution in order to establish a quality indicator for dealing with, as it turned out, shunt malfunction.[20] The authors evaluated the frequency of unplanned reoperations in a pediatric neurosurgery practice over a 2-year period at one institution. The plan was to use ‘unplanned reoperations as a quality indicator.’ Operating room logs and hospital records were retrospectively assessed (January 2008-January 2010). The definition of unplanned reoperations, provided by the Society of British Neurological Surgeons included: (an) unscheduled secondary procedure required for a complication resulting directly or indirectly from the index operation or as an unscheduled return to the operating theater for the same condition.[20] Routine elective cases were those scheduled within working hours (8:00 A.M.-5:00 P.M.). Emergency elective procedures were dealt with on the emergency schedule but were performed ‘within working hours.’ Urgent procedures were performed from 5:00 P.M. to 8:00 A.M. (out of hours). Out of the total of 410 operations, 28% were ‘unplanned reoperations,’ which were typically performed on the 9th postoperative day. Cerebrospinal fluid (CSF) shunting procedures (constituting overall 44% of all operations) most significantly contributed to unplanned reoperations, which were usually performed as urgent procedures. At 30 days, the unplanned reoperation rate was 17% (32% urgent cases). Of interest, ‘trainees’ performed 52% of the urgent operations. The authors concluded that CSF shunting procedures correlated with a high-unplanned reoperation rate (procedure specific), and this high failure rate could be utilized as a ‘quality indicator’ in a future ‘prospective multicenter study.’
Summary: QA may establish standards of care within one institution. In one pediatric neurosurgical study performed within one institution, the QA mandate was to evaluate the frequency of unplanned reoperations/shunt malfunction occurring in one pediatric neurosurgical department over a 2-year period. CSF shunting procedures (44% of all operations) contributed to unplanned reoperations, which were typically performed as urgent procedures (5:00 PM-8:00 AM) [Table 2].
Quality Assurance aims at improving ‘systems’ utilizing information technology
Data indicate that medical errors, which harm patients, could be limited by instituting various QA measures. In Bates et al. study, they noted that optimizing information technology should improve care, and ‘make general and specific recommendations regarding error reduction through the use of information technology.’[2] QA aims included: ‘creating systems designed to support clinical decisions, to test existing/new systems, to adopt/create standards, to enhance communication, to assess/avoid AE, to improve present QA structures, and to improve regulations for vendors.’[2] QA measures have included new order-entry systems, computerized prescribing/bar code utilization, and ways of utilizing ‘modern electronic systems to communicate key pieces of asynchronous data such as markedly abnormal laboratory values.’ In short, their focus was to streamline/simplify patient care, while increasing the adequacy and accuracy of patient safety.
Summary: Data indicate that medical errors, which harm patients, could be limited by instituting various QA measures. Therefore, QA systems focus on creating systems designed to support clinical decisions, to test existing/new systems, to adopt/create standards, to enhance communication, to assess/avoid AE, and to improve present QA structures, while increasing the adequacy and accuracy of patient safety [Table 2].
Defining the role of morbidity and mortality conferences which differs from Quality Assurance
Kravet et al. clearly noted that ‘M&MCs are an Accreditation Council for Graduate Medical Education (ACGME) mandated educational series that occur regularly at all institutions that have residency training programs.’[16] They emphasized that the educational value was ‘immense’ so long as the review of AE/complications, and poor outcomes occurred where ‘education’ rather than ‘culpability’ were emphasized.
M&MCs should focus in a collegial environment on how physicians, residents, physician assistants, nurses, and other adjunctive health care providers (typically within a department/institute), evaluate who, what, when, how, and why AE (AE)/morbidity or mortality occurred, and how to avoid these complications in the future. Liu noted that one of the roles of M&MCs was to equip resident physicians to deal with errors in an educational forum aimed at improving ‘health care delivery and patient safety.’[17] Orlander et al. similarly noted how M&MCs should focus ‘on the tradition of self-analysis and critical thinking in a manner that is productive for all participants.’[21] Mezrich further commented that M&M may vary from ‘heated adversarial affairs seen in traditional surgery departments, to more passive versions often seen in radiology departments.’[18] He emphasized how they can be utilized for resident and attending (physician) training/education, and as a ‘vehicle for quality improvement’ (e.g., including legal considerations).[18]
Summary: M&M (educational) Conferences are mandated by the ACGME for all institutions that have residency training programs. These conferences should be utilized for resident and attending (physician) training/education, and as a ‘vehicle for quality improvement with the intent or reviewing of AE/complications, and poor outcomes in a collegial environment’[Table 2].
Nursing ‘best practices’ vs. morbidity and mortality
‘Best Practices’ conferences, nursing's equivalent to combined QA and M&MCs, utilize a collegial/collaborative environment to foster better patient care.
Cardiovascular nursing ‘best practices’
When Staveski et al. evaluated how to implement ‘best practices’ to a nursing peer review system in a cardiovascular intensive care unit (ICU), they found that ‘regular cycles of nursing M&MCs, a journal club, and interdisciplinary educational sessions in staff meetings,’ resulted in practice changes and ‘improved patient care delivery.’[26]
Summary: Nursing M&MCs, journal clubs, and interdisciplinary educational staff meetings improved patient care delivery [Table 2].
Orthopedic nursing ‘best practices’
Esoga and Seidl assessed ‘best practices’ for orthopedic patients.[7] First, they acknowledged the increased risks inherent in the total joint, and spinal operations performed in orthopedic patients. A major problem was that they were typically admitted to general acute care surgical units without adequate monitoring or sufficient staffing ratios to handle these patients; in the event of a complication, they were often transferred to telemetry where care usually differed from the ‘orthopedic care pathway.’ In this study, the authors (both senior nurses/directors) initiated best care practices, which led to improvement in outcomes. These included: ‘lower nurse to patient ratios, innovative and effective patient education, and continuous surveillance using novel technology in an orthopaedic unit.’
Summary: The increased risks inherent in total joint and spinal surgery within an orthopedic unit prompted the nursing supervisors to institute ‘Best Practices’ which included: lower nurse to patient ratios, innovative and effective patient education, and continuous surveillance using novel technology [Table 2].
Evaluation of ‘best practices’ education for new nursing graduates
Rush et al. utilized a ‘best practice’ model to assess and develop the optimal postgraduation training program for new nurses.[24] Utilizing multiple databases, 47 articles were identified, which met the inclusion criteria for evaluating programs developed to train new nurses. The following criteria were central to the assessment; ‘Education (preregistration and practice), Support/Satisfaction, Competency and Critical Thinking, and Workplace Environment.’[24] The duration, type of support/education, adequacy of transition programs ‘resulted in improved new graduate nurse retention and cost benefits.’ The authors concluded that the development of formal postgraduate transition programs increased not only retention, but also improved competency. They additionally recommended providing technical/practical skills, having well-trained preceptors available for the first 6 to 9 months, and also looked at attitudinal factors/collegiality, noting that they ‘should strive to ensure clinical units with healthy work environments.’
Summary: Rush et al. utilized a ‘best practice’ model to assess and develop the optimal postgraduation training program for new nurses. Utilizing Education, Support/Satisfaction, Competency/Critical Thinking, and Workplace Environment criteria, they studied how the duration, type of support/education, and adequacy of transition programs could improve retention for nurses who were new graduates, while reducing costs [Table 2].
MORBIDITY AND MORTALITY CONFERENCES
Variable frequency/structure in different departments
Liu et al. noted that although M&MCs were begun by a general surgeon in the early 20th century, anesthesia departments have most stringently utilized M&MCs to follow/record AE.[17] Orlander et al. also corroborated that these conferences are aimed to ‘improve practice through the examination of medical errors and bad outcomes,’ are held primarily in departments of anesthesia and surgery, but on a very ‘limited’ basis for internal medicine.[21]
Fassier et al. examined the impact of M&MCs when utilized in an ICU to help monitor quality/safety of patient care delivery. They utilized Medline to search for appropriate select studies, and found that they were ‘recent and scarce.’[10] Nevertheless, although marked variations in study designs were identified, they unequivocally concluded that the institution of M&M clearly had a ‘positive impact’ on outcomes/safety/quality of care in the ICU stetting.
Summary: M&MCs, initiated by a general surgeon early in the 20th century, have most stringently been utilized by anesthesia departments to follow/record AE/morbidity/mortality. Aims included the close examination of ‘bad outcomes’ in general, while in an ICU setting, they could ‘positively impact’ the quality/safety of patient care delivery [Table 2].
The evolution (aims and form) of the morbidity and mortality conference
The aims and form of M&MCs have evolved over the past two decades. In Sellier et al. study, they assessed the ‘format and progression’ of M&MCs, starting with the early 1990s.[25] The study employed 189 questionnaires/interviews of department heads regarding past M&MCs, along with analysis of M&M reports; 105 (55.6%) were answered. They found that the format of M&MCs markedly varied between different departments. For instance, surgical M&M discussed more cases per conference vs. ICUs or medical units.[25] Overall, compared with data from 1998, more head nurses (70.4% (surgical) vs. 27.3% (ICU/medical) and more paramedical staff (63.0% vs. 18.2%) came to conferences. Additionally, the import of M&MCs was highlighted: ‘Physicians considered M&MCs important for improving service quality, patient safety, and enhancing team cohesion.’[25]
Summary: The aims and form of M&MCs have evolved since the early 1990s. Surgical M&M discussed more cases per conference compared with ICU or medical units, and more head nurses and paramedical staff participated from surgical vs. ICU/medical departments. Additionally, physicians considered M&M more important for improving the quality and safety of care delivered in a more cohesive ‘team’ fashion [Table 2].
No clear method for running morbidity and mortality conference
Francois et al. noted that there was no clear method for running M&MCs, selecting cases, and monitoring the ‘the quality and safety of care’ for patients.[11] Observing that the M&MC ‘is one of the keystones in the evaluation of quality of care,’ they went on to discuss how/why a 16-year-old with chronic anemia mistakenly received the wrong ‘second unit’ of blood in transfusion (resulting in hemolysis). This constituted a failure to follow the ‘transfusion protocol,’ while ‘poor working conditions of nurses, linked to inadequate staff in relation to the activity’ also contributed to this AE.
Summary: Often, there is no clear method for running M&MCs, selecting cases, and monitoring the ‘the quality and safety of care’ for patients. The importance of following protocols, particularly regarding transfusions, was emphasized [Table 2].
DEFINITION AND HANDLING OF ADVERSE EVENTS IN M&M CONFERENCES
Definition of adverse events/complications/morbidity
Dekutoski et al. evaluated ‘electronic and federal databases’ (1990-2008) for spinal surgery, and defined AE as: ‘an unintended and undesirable diagnostic or therapeutic event that may impact the patient's care.’[4] They also observed that mortality rates for cervical and lumbar surgery were <1%, but varied from 0.3% to 7% for thoracic surgery. Furthermore, AE varied according to the spinal level; cervical AE 5-19%, thoracic AE 7-18%, and lumbar AE 4-14%. They also recommended that patients’ attendant comorbid risk factors should be carefully considered as contributors to AE in the overall analysis of outcomes.
Summary: AE may be defined as an unintended/undesirable diagnostic or therapeutic event that negatively affects patient's care. AE and mortality differ according to the spinal level addressed, and may be negatively impacted by the increased frequency/severity of comorbid risk factors [Table 2].
How often are adverse events discussed in internal medicine vs. surgery morbidity and mortality conference?
How often are AE discussed in M&MCs involving different subspecialty residency training programs?[17] Out of 295 directors of residency training programs in Internal Medicine, 90% ran M&MCs, but only about 10% of the time was devoted to a discussion of AE/suspected errors. In contrast, in the surgical subspecialties, discussion focused on AE approximately 24% of the time.
Pierluissi et al., utilizing trained physician observers, prospectively evaluated how frequently AE were discussed during 100 internal medicine case presentations vs. 232 surgical cases.[23] Although internal medicine cases were discussed, on average, 3 times longer than surgical cases, there was less overall discussion, and fewer discussions of AE: 37% medicine vs. 72% surgery. Furthermore, fewer internal medical vs. surgical cases concentrated on errors leading to AE; 18% for medicine vs. 42% for surgery. Errors were also attributed to specific causes in 38% of medicine vs. 79% of surgery-related cases.
Summary: In Internal Medicine, 10% of the time at M&MCs was devoted to a discussion of AE/suspected errors, while in the surgical subspecialties, discussion focused on AE about 24% of the time. Fewer internal medical cases concentrated on errors leading to AE (18% medicine vs. 42% surgery), and errors attributed to specific causes (38% medicine vs. 79% surgery) when compared with surgical cases [Table 2].
Who discusses adverse events at morbidity and mortality conferences?
In Bal et al. series, 2 observers prospectively attended 24 M&MCs involving 146 cases over a 6-month period (2007 to 2008).[1] They focused on the structure, discussions, decisions, and actions of these conferences, along with their impact on quality improvement. Participation primarily involved senior physicians (87.7% of those present), and to a lesser degree residents (32.6% of those present), but rarely ‘paramedical professionals and other attendees.’ Notably, these percentages varied for different departments. Although AE were reviewed in 91% of cases, only 10% offered ‘a structured method’ to address these issues. Similarly, ‘although a large number of decisions for quality improvement were declared, fewer actions were planned with a timeline.’
Summary: In one study, 2 observers prospectively attended 24 M&MCs (146 cases, 6-month period), and found that participation were typically senior physicians (87.7% of those present), and residents (32.6% of those present), but rarely ‘paramedical professionals/others [Table 2].
Educational value for residents in reporting minor adverse events at morbidity and mortality
Thomas et al. reassessed the value of reporting minor complications that were typically overlooked at M&MCs, offering the new hypothesis that these seemingly insignificant factors do in fact impact patient outcomes.[29] To improve the quality of M&MCs, the authors focused on defining and then reporting 20 minor complications (chosen by surgeons) to determine whether this enhanced the ‘educational value’ of the conferences. Once a month, a junior resident chose 1 out of the 20 complications, and gave a 10-minute presentation at the M&MC. Faculty and residents were then polled regarding the educational value of the M&MCs before and after implementation of this short-review series. Prior to presenting these short reviews, only 58% felt that minor complications should be reported; afterward, this jumped to 95%. Additionally, 89% thought the presentations were of educational value, and 71% (vs. prior 29%) noted that these reviews helped emphasize that M&MCs were aimed at improving patient care. They concluded, these short reviews of selected minor complications should be incorporated into the M&M format.
Summary: To improve the educational value/quality of M&MCs, the authors promoted the additional reporting of 20 minor complications. Prior to this initiative, 58% felt that minor complications should be reported; afterward, this rose to 95%; additionally, 89% found the presentations educational, and 71% (vs. prior 29%) noted that M&MCs were aimed at improving patient care [Table 2].
How do patients and physicians deal with adverse events (errors)
Gallagher et al. evaluated how medical errors were perceived both by patients (52 participants) and physicians (46 participants).[12] They found that following medical errors or AE’s, patients wanted to know what happened, why, how they could be prevented, and expected an apology. Although physicians agreed that disclosure should be forthcoming, their fear of litigation warranted ‘careful wording’ of such statements. Furthermore, it was noted that if physicians were ‘upset,’ little emotional support was ‘available’
Summary: Gallagher et al. evaluated how medical errors were perceived both by patients (52 participants) and physicians (46 participants). They found patients wanted to know what happened, why, how they could be prevented, and expected an apology. Physicians, agreed disclosure should be forthcoming, but were wary and feared litigation [Table 2].
Increased participation and reduced costs with teleconferencing morbidity and mortality between institutions
Falcone et al. retrospectively analyzed the utility (e.g., enhanced faculty attendance) and cost savings of teleconferencing M&MCs between 2 healthcare campuses.[9] In 2010, 186 conferences were held at the main campus, while 68 were at satellite sites; and involved a total of 236 Continuing Medical Education (CME) hours. Teleconferencing increased the median total attendance by 5 attending physicians/per conference at the main campus, and two at the satellite campus. Additionally, the estimated cost savings/per faculty was between $96.70 and $193.60 per conference, and an average savings of 73.1 hours for physician travel time annually.
Summary: In one institution, teleconferencing increased the median attendance by 5 attendings/conference at the main campus, 2 at the satellite campus, saved between $96.70 and $193.60/per faculty/conference, and an average of 73.1 hours of physician travel time annually [Table 2].
Informal polling of surgical neurology international board (spine supplement) regarding attendance at morbidity and mortality conference
Seventeen members of the board of Surgical Neurology International Spine Supplement answered an informal questionnaire regarding attendance at M&MCs [Table 1].[6] There were 4 orthopedists and 13 neurosurgeons; 6 were past or present Chairs of Departments (3 of Orthopedics, and 3 of Neurosurgery), and 4 were Directors of Spine Sections. Fourteen were in university practices (12 professors, 1 associate professor, and 1 assistant professor), while 3 were in private practice (2 professors affiliated with universities, and 1 attending physician in private practice). Attendance at M&MCs was mandatory in 10 cases, 5 were not mandatory, and in 2 did not know. While 16 of 17 surgeons assumed they should attend M&MCs (part of the culture), 15 of 17 agreed that they were responsible for presenting or being present when their cases were discussed. The one surgeon who disagreed with both requirements was a spine surgeon in Florida, the Sunshine State, which allows for ‘full discovery’ of M&M proceedings.
Summary: An informal poll of the Editorial Board of Surgical Neurology International Spine Supplement revealed that 16 of 17 surgeons presumed they should attend M&MCs (part of the culture). Additionally, 15 of 17 deemed they were responsible for being present when their cases were discussed at M&MCs [Table 2].
RETROSPECTIVE COLLECTION OF MORBIDITY AND MORTALITY CONFERENCE DATA
Few focused peer review studies
Focused peer review (FPR) studies, if applicable to different medical disciplines, may have a beneficial impact on physician performance and patient care. One example was the Hussain et al. study, performed in a radiology department, where the peer-review process was included ‘misdiagnoses from all sources’ and used ‘FPR in faculty accountability and management.’[14] Radiologists reviewed 12 cases per month for the study, while additional errors and misdiagnoses were scrutinized. The FPR documents were assessed by the chairman, were presented at monthly M&MCs, and resulted in ‘no action to termination.’ This study involved 1646 cases out of 300,000 studies reviewed by 31 radiologists. Ultimately, ‘16 FPRs were completed; 5 (31%) from routine peer review and 11 (69%) from clinically reported errors.’ The authors concluded ‘FPR can effectively contribute to the surveillance and management of faculty performance for improved patient care.’
Summary: FPR studies performed for different medical disciplines may have a beneficial impact on physician performance and patient care [Table 2].
Retrospective data analyzed from an anesthesia department
While retrospectively evaluating M&MCs data from an anesthesia department and surgical ICU setting, Baumann et al. noted that meetings focused on ‘medical education (75%), corrective actions (62%), changes in procedures (48%), organization (5%), and research (e.g., methods for improvement).’[3] All deaths or ‘near deaths in the operating room,’ and other instructive cases were also included. During the study, benefits included the maintenance of M&M attendance rates, the experience of preparing cases for the conference with ‘expert colleagues,’ and the ‘participation of external morbidity mortality committee (MMC) experts.
Summary: M&MCs for an anesthesia department and surgical ICU setting revealed that they focused on: medical education (75%), corrective actions (62%), changes in procedures (48%), organization (5%), and research (e.g., methods for improvement). Benefits included: maintained attendance rates, the experience of preparing cases with ‘expert colleagues,’ and outside experts [Table 2].
Retrospective data analyzed from a general surgery department
In Falcone et al. study, ‘The ACGME core competency of practice-based learning and improvement was assessed with surgical M&MC.’[8] Retrospectively analyzing M&M reports prepared predominantly by 5th year general surgery residents, they evaluated the number of AE that occurred vs. those published in the literature. Their hypothesis was that ‘reporting patterns and incidence rates will remain constant over time.’ Over a 2-year period, 85 M&M reports were evaluated regarding how residents reported AE, their frequency and type. Of 11,368 patients, 289 (2.5%) experienced AE; this was a lower number than reported in other studies. Of interest, the frequencies of AE were consistent for residents at the postgraduate year 2, 4, and 5 levels for all services. Notably, 522 major AE were reported for 461 patients, and they included; mortality (24.1%), hematologic/vascular (16.7%), and gastrointestinal (16.1%). They concluded that reports of AE were consistent/stable within this 2-year period, and provided a valuable experience for the 5th year residents.
Summary: The ACGME requires surgical M&MCs for accreditation. One institution performed a retrospective analysis of AE (frequency/type) found in 85 M&M reports (largely prepared by 5th year residents) accumulated over a 2-year period. Out of 11,368 patients, 289 (2.5%) AE were reported, and the patterns/frequencies were relatively constant over the 2 years. However, the frequency of AE was lower than those reported in other studies [Table 2].
Retrospective morbidity and mortality data analyzed from a neurosurgical department
When Steiger et al. retrospectively evaluated M&M data (utilizing electronic coding) in a neurosurgical department in Germany over a 5-year period, the overall morbidity rate was 7.1% (surgical/medical morbidity), and the mortality rate directly related to surgery was 0.38%.[27] Leading causes for morbidity included: new neurological deficits (25%), postoperative hemorrhages (23%), and second operations attributed to incomplete first procedures (14%). Although the authors accepted the conferences as a teaching tool, they found no clear-cut impact on quality improvement.
Summary: When Steiger et al. retrospectively evaluated M&M data (utilizing electronic coding) in a neurosurgical department in Germany over a 5-year period, the overall morbidity rate was 7.1%, with a 0.38% mortality rate [Table 2].
ADVANTAGES OF PROSPECTIVE COLLECTION OF MORBIDITY AND MORTALITY DATA
Prospective morbidity and mortality data collection for a neurosurgical department
Houkin et al. prospectively assessed how neurosurgical AE (unexpected vs. anticipated complications) due to surgery and/or endovascular procedures were discussed in M&MCs.[13] Prospective assessment resulted in a much higher 28.3% incidence (182 of 643) of neurosurgical AE over 2 years.[13] Of these, 90.7% (165) were ‘closely related to procedures,’ 68.7% (125) were considered ‘predictable,’ and just 6 (3.3%) were thought to be ‘avoidable’; of note only 2 (1.1%) of these latter 6 were attributed to ‘error.’
Summary: Prospectively assessing the frequency of neurosurgical AE (due to surgery and/or endovascular procedures) for M&MCs, Houkin et al. found a much higher 28.3% incidence (182 of 643) of neurosurgical AE over a 2-year period [Table 2].
Prospective morbidity and mortality data collection for patients having major spinal surgery
Street et al. performed a rigorous, prospective, weekly evaluation (rounds/recording) of M&M/AE's for adults having major spinal surgery over a 1-year period, and compared these with previous retrospectively collated data.[28] Morbidities were defined as major or minor medical or surgical complications, particularly those impacting length of stay (LOS), along with ‘unplanned second surgeries during the index admission, wound infections requiring reoperation, and readmissions during the same calendar year.’[28] Assessment of M&M data yielded a 23% retrospective vs. 87% prospective perioperative morbidity rate; 822 of 942 patients exhibited at least one complication, which prolonged the LOS in 39% of patients. There were 14 mortalities, while intraoperative surgical morbidity/complications occurred in 10.5% of patients; these included a 4.5% incidence of durotomies (unintended), a 1.9% incidence of malpositioned instrumentation warranting secondary surgery, and a 2.2% frequency of blood loss exceeding 2 L. Postoperative complications in 73.5% of patients included; ‘wound complications, 13.5%; delirium, 8%; pneumonia, 7%; neuropathic pain, 5%; dysphagia, 4.5%, and neurological deterioration, 3%’ among others.[28] The authors’ concluded that prospective rather than retrospective assessment of morbidity/mortality for complex spine surgery revealed higher AE than anticipated, and noted ‘ the true complexity of spine surgery may be greatly underestimated.’
Summary: Street et al. performed a rigorous, prospective, weekly evaluation (rounds/recording) of M&M/AE's for adults having major spinal surgery over a 1-year period, and compared these with previous retrospectively collated data. Assessment of M&M data yielded a 23% retrospective vs. 87% prospective perioperative morbidity rate; 822 of 942 patients exhibited at least ‘one documented complication,’ 39% of which prolonged the LOS [Table 2].
Prospective morbidity and mortality data collection for a general surgery department
For a general surgical department, Hutter et al. similarly compared the accuracy of retrospectively vs. prospectively collected M&M data collated by a nurse reviewer from the American College of Surgeons-National Surgical Quality Improvement Program (ACS-NSQIP).’[15] For data collected retrospectively, 0.9% mortality and 6.4% morbidity rates were low, while those collected prospectively were higher, revealing a 1.9% mortality rate, and 28.9% morbidity rate. The authors concluded that retrospective M&M data analysis markedly underreported in-hospital/post-discharge complications and deaths vs. ACS-NSQIP. The retrospective method typically missed 1 of 2 deaths and 3 of 4 AE at Massachusetts General Hospital (Boston, MA, Dept of Surgery). To address this shortcoming, they recommended adopting an internet/web-based reporting system utilizing the ACS-NSQIP platform to ‘to automate, facilitate, and standardize data on surgical morbidity and mortality.’[15]
Summary: In a general surgical department, for data collected retrospectively, mortality (0.9%) (53/5905 patients) and morbidity rates (6.4%) were low, while those collected prospectively were higher: mortality rate of 1.9% (28/1439 patients) and morbidity rate of 28.9% recommending ACS-NSQIP platform [Table 2].
LEGAL AND MEDICOLEGAL ISSUES PERTAINING TO MORBIDITY AND MORTALITY CONFERENCES
No clear cut federal regulations requiring morbidity and mortality conferences
’There appeared to be no clear cut federal regulations requiring M&MCs, as laws varied state by state, as did requirements from institution to institution (personal communication, June 15, 2012: Carol L. Forte, Esq.). Although there were references in various state administrative codes to M&M reviews, Assessment of the Code of Federal Regulations yielded no specific requirement for hospitals to hold M&MCs. In New Jersey, however, the administrative code required departments of anesthesia, and Long Term Acute Hospitals, to have M&MCs. (Notably, the phrase ‘long term acute hospitals’ sounds like a contradiction, but it has a specific definition.) In New York State there was a requirement that regional trauma centers have an organized QA program that includes M&M review, but there were no further specifications in the statute as to what it should consist of.
Summary: There appeared to be no clear cut federal regulations requiring M&MCs, as laws vary from state to state, as did requirements from institution to institution (Personal communication, June 15,2012, Carol L. Forte, Esq.). In New Jersey, the administrative code required departments of anesthesia, and Long Term Acute Hospitals, to have M&MCs, while in New York State, regional trauma centers were required to have QA that included M&M [Table 2].
Various institutions and individual societies require morbidity and mortality
’Various institutions and individual societies require M&MCs. (Personal communication, June 15, 2012, Carol L. Forte. Esq.)’ For example, the Massachusetts Medical Society has a document on line that does require regularly scheduled conferences to maintain the hospital's accreditation. In addition, Emory University Medical School (Atlanta, Georgia, USA) also requires that the Department of Obstetrics and Gynecology have scheduled M&MCs. Although no specific Joint Commission National Quality Core Measures or JCAHO requirements could be found, the 1983 ACGME required hospitals to have M&MCs in order to maintain their accreditation for Graduate Medical Education (GME) programs. For example, mandatory for residency training programs (Personal Communication, June 15, 2012, Carol Forte Esq.).[17]
A prior chairman of a neurosurgical department in the state of New Jersey wrote ‘scheduled educational department meetings were mandated by the Residency Review Committee (RRC) for neurosurgery and the JCAHO. Both required M&MCs at any university (department with resident-training) hospital. (Personal communication, May 10, 2012, George Jacobs, M.D.).
Summary: The 1983 ACGME required hospitals to have M&MCs in order to maintain their accreditation for GME programs. Scheduled educational department meetings were typically mandated by the RRC and the JCAHO [Table 2].
Need for malpractice/tort reform to improve reporting of medical errors in morbidity and mortality conferences
Patrick et al. focused on the need for malpractice/tort reform if reporting of medical errors or ‘near misses’ is to improve.[22] Among the multiple barriers to reporting are the physicians who consider themselves at risk for ‘sanctions, malpractice claims, and unpredictable compensation of injured patients.’ They noted that the Patient Safety and Quality Improvement Action (2005) recommended, as a form of tort reform, the development of ‘administrative health courts’ promoting ‘no fault insurance’ programs to deal with AE/claims.
Miller supported ‘compensation measures’ to deal with birth injuries in Virginia and Florida.[19] By reducing the number of claims and cost of premiums, and focusing on resolving disputes with greater ‘transparency and disclosure,’ patients would receive more reasonable and appropriate compensation, while patient safety could also be improved.
Summary: Malpractice/tort reform is necessary if AE/medical errors are to be more readily reported and acted upon. As long as physicians are at risk for ‘medicolegal sanctions,’ such open reporting is unlikely to occur. Physicians anxiously await tort reform (e.g., administrative health courts, no fault systems) to help resolve this problem [Table 2].
CONCLUSION
Most agree that holding M&MCs to review AE/morbidity/mortality educates attending physicians, residents, nurses, physician assistants, and other adjunctive personnel. Learning from mistakes, helps prevent them from being repeated in the future. Participation in M&MCs should remain a vibrant part of the culture aimed at the common good: improving the safety and care of our patients. The QA process, aimed at correcting system-wide failures, supplements but does not supplant the value of M&MCs that focus on individual shortcomings and their impact on AE and M&M.
Other findings included documenting that prospective collection of M&M data vs. retrospective analyses more accurately identified perioperative/postoperative complications (AE/morbidity/mortality).
Unfortunately, as long as physicians perceive their continued medicolegal susceptibility and vulnerability to suits, even with ‘nondiscovery’ clauses protecting most M&M proceedings in the majority of states, our ability to better educate will remain hampered, limiting our capability and culpability to ‘right the wrongs.’ M&MCs must continue to offer a forum for frank discussion of complications and solutions between physicians (medical/surgical) and adjunctive personnel in a ‘protected’ environment. Medicolegal concerns should not be an ‘excuse’ for failing to attend M&MCs, as most universities require 75-100% attendance. Noteably, almost all institutions ‘hold cases over’ if the involved physician is not at M&M when his/her case is presented. Most critically, if physicians do not attend M&MCs, they fail to educate themselves and others, while also imparting the message to their staff and patients that they simply ‘do not care’ or do not assume responsibility for what has occurred.
Footnotes
Disclaimer: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. No funds were received in support of this article.
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2012/3/6/377/103872
REFERENCES
- 1.Bal G, Sellier E, Tchouda SD, Francois P. Improving quality of care and patient safety through morbidity and mortality conferences. J Healthc Qual. 2012 Apr 24; doi: 10.1111/j.1945-1474.2011.00203.x. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 2.Bates DW, Cohen M, Leape LL, Overhage JM, Shabot MM, Sheridan T. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc. 2001;8:299–308. doi: 10.1136/jamia.2001.0080299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baumann A, Cuignet-Royer E, Bouaziz H, Borgo J, Claudot F, Torrens J, et al. Morbidity and mortality conferences in anaesthesia and intensive care: experience feedback from Nancy university hospital. Ann Fr Anesth Reanim. 2011;30:888–93. doi: 10.1016/j.annfar.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 4.Dekutoski MB, Norvell DC, Dettori JR, Fehlings MG, Chapman JR. Surgeon perceptions and reported complications in spine surgery. Spine (Phila Pa 1976) 2010;35(9 Suppl):S9–S21. doi: 10.1097/BRS.0b013e3181d830de. [DOI] [PubMed] [Google Scholar]
- 5.Drake JM, Singhal A, Kulkarni AV, Deveber G, Cochrane DD. The Canadian Pediatric Neurosurgery Study Group.Consensus definitions of complications for accurate recording and comparisons of surgical outcomes in pediatric neurosurgery. J Neurosurg Pediatr. 2012;10:89–95. doi: 10.3171/2012.3.PEDS11233. [DOI] [PubMed] [Google Scholar]
- 6.Epstein NE. Editorial: Are morbidity and mortality conferences DNR (Do Not Resuscitate) or can they be revived? .Surg Neurol Int Sept. 2012;3:114. doi: 10.4103/2152-7806.101804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Esoga PI, Seidl KL. Best practices in orthopaedic inpatient care. Orthop Nurs. 2012;31:236–40. doi: 10.1097/NOR.0b013e31825dfe23. [DOI] [PubMed] [Google Scholar]
- 8.Falcone JL, Lee KK, Billiar TR, Hamad GG. Practice-based learning and improvement: a two-year experience with the reporting of morbidity and mortality cases by general surgery residents. J Surg Educ. 2012;69:385–92. doi: 10.1016/j.jsurg.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Falcone JL, Watson AR. Surgical Morbidity and Mortality Conference using teleconferencing allows for increased faculty participation and moderation from satellite campuses and saves costs. J Surg Educ. 2012;69:58–62. doi: 10.1016/j.jsurg.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 10.Fassier T, Favre H, Piriou V. How to assess the impact of morbimortality conferences on healthcare quality and safety in ICU? Ann Fr Anesth Reanim. 2012;31:609–16. doi: 10.1016/j.annfar.2012.04.025. [DOI] [PubMed] [Google Scholar]
- 11.François P, Sellier E, Pouzol P, Bal G, Labarère J. Mortality and morbidity conference: A tool for quality and safety of care continuous improvement. Transfus Clin Biol. 2011;18:43–8. doi: 10.1016/j.tracli.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Gallagher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. Patients’ and physicians’ attitudes regarding the disclosure of medical errors. JAMA. 2003;289:1001–7. doi: 10.1001/jama.289.8.1001. [DOI] [PubMed] [Google Scholar]
- 13.Houkin K, Baba T, Minamida Y, Nonaka T, Koyanagi I, Iiboshi S. Quantitative analysis of adverse events in neurosurgery. Neurosurgery. 2009;65:587–94; discussion 594. doi: 10.1227/01.NEU.0000350860.59902.68. [DOI] [PubMed] [Google Scholar]
- 14.Hussain S, Hussain JS, Karam A, Vijayaraghavan G. Focused peer review: the end game of peer review. J Am Coll Radiol. 2012;9:430–3.e1. doi: 10.1016/j.jacr.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 15.Hutter MM, Rowell KS, Devaney LA, Sokal SM, Warshaw AL, et al. Identification of surgical complications and deaths: an assessment of the traditional surgical morbidity and mortality conference compared with the American College of Surgeons-National Surgical Quality Improvement Program. J Am Coll Surg. 2006;203:618–24. doi: 10.1016/j.jamcollsurg.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Kravet SJ, Howell E, Wright SM. Morbidity and mortality conference, grand rounds, and the ACGME's core competencies. J Gen Intern Med. 2006;21:1192–4. doi: 10.1111/j.1525-1497.2006.00523.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu M. Medicine and Society: Error in Medicine: The Role of the Morbidity & Mortality Conference.Virtual Mentor. Ethics J Am Med Assoc. 2005;7:4. doi: 10.1001/virtualmentor.2005.7.4.msoc1-0504. [DOI] [PubMed] [Google Scholar]
- 18.Mezrich JL. Putting the heat back into radiology morbidity and mortality conferences. J Am Coll Radiol. 2011;8:638–41. doi: 10.1016/j.jacr.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 19.Miller LA. Health courts: an alternative to traditional tort law. J Perinat Neonatal Nurs. 2011;25:99–102. doi: 10.1097/JPN.0b013e318215926e. [DOI] [PubMed] [Google Scholar]
- 20.Mukerji N, Jenkins A, Nicholson C, Mitchell P. Unplanned reoperation rates in pediatric neurosurgery: a single center experience and proposed use as a quality indicator. J Neurosurg Pediatr. 2012;9:665–9. doi: 10.3171/2012.2.PEDS11305. [DOI] [PubMed] [Google Scholar]
- 21.Orlander JD, Barber TW, Fincke BG. The morbidity and mortality conference: the delicate nature of learning from error. Acad Med. 2002;77:1001–6. doi: 10.1097/00001888-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Paterick ZR, Paterick BB, Waterhouse BE, Paterick TE. The challenges to transparency in reporting medical errors. J Patient Saf. 2009;5:205–9. doi: 10.1097/PTS.0b013e3181be2a88. [DOI] [PubMed] [Google Scholar]
- 23.Pierluissi E, Fischer MA, Campbell AR, Landefeld CS. Discussion of medical errors in morbidity and mortality conferences. JAMA. 2003;290:2838–42. doi: 10.1001/jama.290.21.2838. [DOI] [PubMed] [Google Scholar]
- 24.Rush KL, Adamack M, Gordon J, Lilly M, Janke R. Best practices of formal new graduate nurse transition programs: An integrative review. Int J Nurs Stud. 2012 Jul 11; doi: 10.1016/j.ijnurstu.2012.06.009. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 25.Sellier E, David-Tchouda S, Bal G, François P. Morbidity and mortality conferences: their place in quality assessments. Int J Health Care Qual Assur. 2012;25:189–96. doi: 10.1108/09526861211210411. [DOI] [PubMed] [Google Scholar]
- 26.Staveski S, Leong K, Graham K, Pu L, Roth S. Nursing mortality and morbidity and journal club cycles: paving the way for nursing autonomy, patient safety, and evidence-based practice. AACN Adv Crit Care. 2012;23:133–41. doi: 10.1097/NCI.0b013e3182424ce7. [DOI] [PubMed] [Google Scholar]
- 27.Steiger HJ, Stummer W, Hänggi D. Can systematic analysis of morbidity and mortality reduce complication rates in neurosurgery? Acta Neurochir (Wien) 2010;152:2013–9. doi: 10.1007/s00701-010-0822-3. [DOI] [PubMed] [Google Scholar]
- 28.Street JT, Lenehan BJ, DiPaola CP, Boyd MD, Kwon BK, Paquette SJ, et al. Morbidity and mortality of major adult spinal surgery.A prospective cohort analysis of 942 consecutive patients. Spine J. 2012;12:22–34. doi: 10.1016/j.spinee.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 29.Thomas MK, McDonald RJ, Foley EF, Weber SM. Educational value of morbidity and mortality (M&M) conferences: are minor complications important? J Surg Educ. 2012;69:326–9. doi: 10.1016/j.jsurg.2011.11.010. [DOI] [PubMed] [Google Scholar]


