Abstract
Gastrointestinal stromal tumors (GIST) are rare mesenchymal smooth muscle sarcomas that can arise anywhere within the gastrointestinal tract. Sporadic mutations within the tyrosine kinase receptors of the interstitial cells of Cajal have been identified as the key molecular step in GIST carcinogenesis. Although many patients are asymptomatic, the most common associated symptoms include: abdominal pain, dyspepsia, gastric outlet obstruction, and anorexia. Rarely, GIST can perforate causing life-threatening hemoperitoneum. Most are ultimately diagnosed on cross-sectional imaging studies (i.e., computed tomography and/or magnetic resonance imaging in combination with upper endoscopy. Endoscopic ultrasonographic localization of these tumors within the smooth muscle layer and acquisition of neoplastic spindle cells harboring mutations in the c-KIT gene is pathognomonic. Curative treatment requires a complete gross resection of the tumor. Both open and minimally invasive operations have been shown to reduce recurrence rates and improve long-term survival. While there is considerable debate over whether GIST can be benign neoplasms, we believe that all GIST have malignant potential, but vary in their propensity to recur after resection and metastasize to distant organ sites. Prognostic factors include location, size (i.e., > 5 cm), grade (> 5-10 mitoses per 50 high power fields and specific mutational events that are still being defined. Adjuvant therapy with tyrosine kinase inhibitors, such as imatinib mesylate, has been shown to reduce the risk of recurrence after one year of therapy. Treatment of locally-advanced or borderline resectable gastric GIST with neoadjuvant imatinib has been shown to induce regression in a minority of patients and stabilization in the majority of cases. This treatment strategy potentially reduces the need for more extensive surgical resections and increases the number of patients eligible for curative therapy. The modern surgical treatment of gastric GIST combines the novel use of targeted therapy and aggressive minimally invasive surgical procedures to provide effective treatment for this lethal, but rare gastrointestinal malignancy.
Keywords: Gastrointestinal stromal tumors, Laparoscopic resections of gastrointestinal stromal tumors, Imatinib mesylate, Gastrectomy
INTRODUCTION
Gastrointestinal stromal tumors (GIST) are rare mesenchymal tumors that occur throughout the smooth muscle layer of the gastrointestinal (GI) tract[1]. GIST represent less than 1% of all GI tract malignancies. The most common location of these tumors is the stomach (70%), small bowel (20%-30%), small intestine and colon/rectum (10%). Uncommonly, they can arise within the greater omentum, esophagus, appendix, and gallbladder. Most cases are sporadic, and affect men slightly more frequently than women (54% vs 46%)[2]. The annual incidence in the United States has remained stable at 3000 to 4000 cases per year. The world-wide age-adjusted annual incidence rates range from 6.8 to 14.5 cases per million and vary between countries of origin. The median age at diagnosis is 58 years of age, but GIST have been reported in newborns and adolescents[3]. GIST can range in size from several millimeters to over 30 cm in diameter. Tumor diameter appears to significantly influence biologic behavior, as small GIST may remain indolent for many years and large, “massive” GIST have higher rates of recurrence and associated metastases[2].
Historically, smooth muscle sarcomas were classified as leiomyosarcomas[4]. The development of malignant GIST requires the transformation of the interstitial cells of Cajal, pacemakers of the GI tract, to a malignant phenotype through activating or gain of function mutations in the c-KIT proto-oncogene[5]. GIST are spindle cell neoplasms that usually retain the ultrastructural characteristics of smooth muscle cells, but have immunohistochemical staining for c-KIT, CD-34, smooth muscle actin, desmin and S-100[6]. Approximately 70% of GIST are spindle cell type neoplasms; the minority are epithelioid (20%) or mixed cell type (10%)[7]. Hirota et al[5] first described the novel mutation in the KIT tyrosine kinase receptor gene in 1998. Since this landmark discovery, most “leiomyosarcomas” have been reclassified as GIST. KIT is located on chromosome 4q11-q12 and functions as a transmembrane receptor for its ligand, stem cell factor. In the non-cancerous state, this ligand binds to the extracellular portion of the receptor to induce homodimerization and downstream activation of its cell-signaling pathways[8]. Wild-type c-KIT normally regulates cellular differentiation, growth, and survival. Approximately 80%-90% of GIST harbor mutations in the KIT genome. Mutations in the platelet-derived growth factor receptor (PDGFRα) occur in 5%-10% of c-KIT-wild type GIST. DOG1 mutations may help identify GIST with wild type c-KIT and PDGFR[9]. Mutated KIT receptors induce ligand-independent, unregulated activation of the downstream cell signaling pathways which collectively results in a loss of normal cell adhesion, differentiation, and proliferation to promote tumorigenesis. Exon 11 mutations in the KIT gene cause constitutively activated receptors leading to unregulated autophosphorylation of the intracytoplasmic tyrosine kinases[10]. KIT mutations in exons 9, 13, 17 are less common and have been associated with more aggressive tumor behavior.
Biologically, gastric GIST tumors grow locally within the stomach (intra- or extraluminal expansion) and eventually obtain the capability to metastasize via hematogenous routes to the solid viscera (liver, small bowel, lungs) and peritoneal cavity. Tumors can also spread along the smooth muscle planes within the stomach or can rupture into the peritoneal cavity causing sarcomatosis. Complete surgical resection is thought to be the only curative treatment for GIST. The recent use of cytostatic agents, such as imatinib mesylate, in patients with metastatic disease has been associated with durable recurrence-free survival[11]. This important observation suggests that overall survival may not be the most important endpoint to consider when making treatment decisions. Radical gastrectomy is seldom required for extirpation of these tumors[3]. In contradistinction to gastric adenocarcinoma, where it is essential to obtain at least five-centimeter proximal and distal margins, GIST tumors can be effectively treated by a complete gross resection of the tumor[1]. Given the infrequency of lymphatic metastases, regional lymphadenectomy is not indicated. Minimally-invasive operations are now frequently used to treat gastric GIST. Retrospective series suggest that these techniques may reduce perioperative stress and are associated with lower rates of postoperative complications, shorter hospital stays and equivalent recurrence rates (Table 1)[12-16].
Table 1.
Summary of large-series (> 35 cases) of minimally-invasive resections for gastric gastrointestinal stromal tumor
| Ref. | Location | MIS/GIST | Proximal tumors n (%) | Size (cm) | Operative time (min) | Complications n (%) | Conversion to open surgery n (%) | LOS (d) | R0 resection rate | Intermediate/high risk GIST n (%) | Recurrence rate n (%) | Median F/U (mo)(range) |
| Sasaki et al[16] | Japan | 451/37 | 6 (13) | 3.2 (1.6-7.4) | 100 (30-240) | 1 (2) | 1 (2) | NR | 100 | 9 (24) | 0 | 74 (1-81) |
| Sexton et al[14] | Germany | 112/61 | 7 (11) | 3.8 (± 1.8) | 151.9 (± 67.3) | 10 (16.4) | 1 (2) | 3.9 (± 2.2) | 98 | 15 (25) | 3 (5) | 15 (0-103) |
| Wilhelm et al[15] | Germany | 93/633 | 36 (39) | 2.6 (0.3-6.5) | 90.7 | 7 (7.5) | 6 (6.5) | 7.3 | 100 | 8 (13) | 0 | 40 (2-99) |
| Otani et al[13] | Japan | 60 | 36 (60) | 3.6 (1.8-15.0) | 141/1884 | NR | 0 | 7.2 | 1002 | 17 (28) | 2 (3) | 53 |
| Novitsky et al[12] | NC | 50 | 17 (34) | 4.4 (± 2.0) | 135 (± 56) | 4 (8) | 0 | 3.8 (± 1.6) | 100 | 14 (28) | 4 (8) | 36 (4-84) |
| Total (for GIST) | 271 | 102 (38) | 8 (3) | 63 (23) | 9 (3) |
Forty-five laparoscopic operations and 37 confirmed gastrointestinal stromal tumors (GIST);
no positive margins, but one patient had a laparoscopic resection in the setting of distant metastatic disease;
ninty-three consecutive patients, including 62 GIST; there was 1 laparascopic-assisted endoscopic resection, 55 laparoscopic wedge resections, and 34 transgastric resections;
the mean operative time was 141 for laparoscopic operations and 188 min for laparoscopy-assisted operations. NC: North Carolina; n: Number of patients in each series; MIS: Minimally invasive operations; Proximal tumors: GIST at gastroesophageal junction or within gastric cardia; Size: Median pathologic tumor size; Complications: Surgical morbidity; LOS: Length of hospital stay; NR: Not reported; R0 resection: Gross and microscopically-negative margins; F/U: Follow-up.
EPIDEMIOLOGY AND DIAGNOSIS
Miettinen et al[3] published the largest retrospective series of gastric GIST that reviews 1869 cases seen at the Armed Forces Institute of Pathology from 1970-1996. The vast majority of cases occurred in patients over 40 years of age and the median tumor diameter was 6 cm (range: 0.5-4.4 cm). Most gastric GIST had spindle-cell or epithelioid differentiation.Over 90% of these neoplasms had mutations in the c-KIT gene; PDGFR mutations were more frequently identified in epitheliod tumors. The metastatic potential of these tumors strongly correlated with their size and rate of mitotic activity. Unfavorable prognostic factors included proximal tumors (gastric cardia and gastroesophageal junction), the presence of coagulative necrosis, ulceration, and invasion deep to the mucosal layer.
Most GIST are incidentally diagnosed during evaluations for nonspecific GI symptoms, such as pain, nausea and vomiting, and weight loss[2]. Tumor hemorrhage commonly occurs when large tumors develop an ischemic, punctate ulcer (Figure 1A). Usually, the bleeding can be temporized using endoscopic sclerotherapy or electrosurgical coagulation techniques. Seldom is it necessary to take patients urgently for surgical resection with intractable hemorrhage (Figure 1B and C). Often these patients can be stabilized with medical and endoscopic therapy and have elective operations to extirpate these tumors. Intraperitoneal tumor rupture with hemoperitoneum and tumor dissemination is a difficult clinical problem that is associated with a significant risk of intraperitoneal sarcomatosis.
Figure 1.
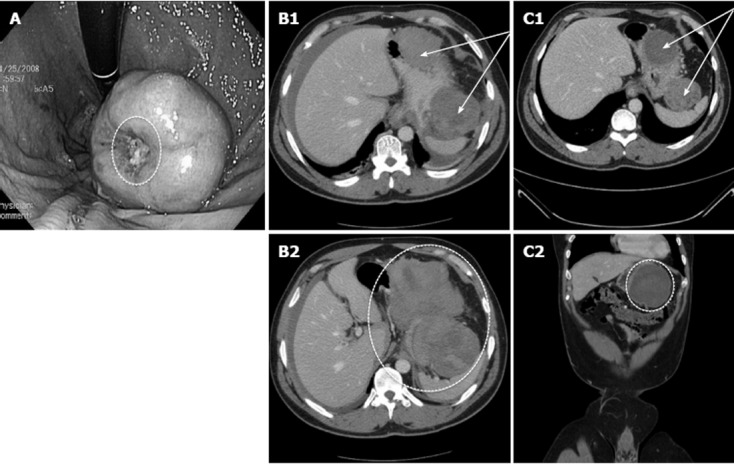
Clinical images of complicated gastrointestinal stromal tumors. A: Large intraluminal gastric gastrointestinal stromal tumors (GIST) with punctate central ulceration. The bleeding ulcer was treated endoscopically with sclerotherapy and electrocautery (cauterized tissue; white oval). The patient had an interval resection electively without additional hemorrhage from the tumor; B: Acute presentation of a patient with a ruptured gastric GIST with hemoperitoneum. These images represent contrast-enhanced computed tomography (CT) scan from a patient with a large extraluminal gastric GIST along the greater curvature of the stomach. B1 demonstrates axial CT images of the bi-lobed tumor with irregular borders (arrows); B2 shows additional axial images at the caudal extent of gastric tumor with layering of blood in the splenic recess (oval). He was diagnosed with hemoperitoneum and was resuscitated with packed red blood cells, fresh frozen plasma, and platelets; the patient was on antiplatelet therapy at the time of admission. He stabilized and had an upper endoscopy/ultrasonography for tissue diagnosis and to plan definitive treatment; C: Ruptured gastric GIST following conservative management. Contrast-enhanced CT images following a six-week period of conservative management of the patient with ruptured gastric GIST. C1 demonstrates the more organized bi-lobed tumor with distinct borders (arrows); C2 shows coronal images of the organized hemorrhagic component within the splenic recess after a period of observation (oval). Ultimately this patient had an interval open subtotal gastrectomy for a high-grade GIST.
Computed tomography (CT) scanning is the most widely used and effective staging modality[2]. Multiple-row detector can localize the tumor within the stomach and remains a very sensitive technique to detect distant metastasis (at least ≥ 1 mm in diameter) within the liver or lungs; small volume intraperitoneal disease is often only detected on diagnostic laparoscopy and is responsible for the reported 10%-15% of false negative rate with dynamic CT. Magnetic resonance imaging (MRI) is an acceptable alternative to CT for patients with renal dysfunction or in whom the risk of cumulative ionizing radiation may be prohibitive. Positron emission tomography (PET) remains an experimental test that may be useful in confirming distant metastatic disease and determining the response to neoadjuvant targeted therapy. PET scans usually indicate tumor responsiveness to imatinib mesylate within days to weeks of induction therapy.
Upper endoscopy (EGD) with ultrasonography (EUS) is an essential diagnostic modality to acquire tissue for diagnosis, usually by fine needle aspiration (FNA) or core-needle biopsy (Figure 2). In addition, EUS is accurate in determining the depth of penetration and origin of these neoplasms and also allows one to potentially consider a hybrid endoscopy/laparoscopic resection[17]. The published National Comprehensive Cancer Network (NCCN) guidelines outline the recommended principles of tissue sampling for GIST (http://www.nccn.org). Since most GIST are soft, fragile, well-encapsulated tumors, indiscriminate biopsies increase the risk of tumoral hemorrhage and rupture. This is associated with higher rates of tumor recurrence and/or intraperitoneal dissemination. The decision to perform a preoperative or pretreatment biopsy should be individualized and only performed when the results of the sampling would definitively influence the choice of treatment[18]. Biopsy is mandatory for all locally-advanced gastric GIST that will be treated with pre-resection neoadjuvant targeted therapy. Careful review of the acquired tissue by experienced GI histopathologists and use of comprehensive immunohistochemical staining for c-KIT and other markers is essential to confirm the diagnosis. Given the accuracy and real time localization of these tumors, EUS-guided biopsy is generally preferable to CT- or ultrasound-guided FNA biopsy techniques[2,19].
Figure 2.
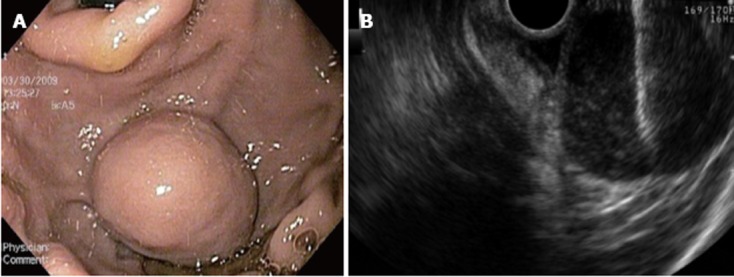
Endoscopy ultrasound images with fine needle aspiration biopsy. A: A 3 cm × 3 cm submucosal intraluminal mass within the gastric cardia; B: This Endoscopy ultrasound image shows the fine needle aspiration biopsy needle (horizontal white line in upper right corner of image) puncturing the submucosal gastric gastrointestinal stromal tumors.
EGD/EUS can identify the key anatomic relationships of the tumor to the gastric wall layers. GIST at the gastroesophageal junction (Figure 3), pylorus and along the posterior wall of the stomach represent unique surgical challenges and influence the required operation. EGD can also effectively be used to treat tumor hemorrhage and avoid the need for urgent gastric operations. EUS can determine the depth of penetration through the layers of the gastric wall and potentially identify tumors that can be extirpated using endoscopic resection techniques. Only intragastric GIST that arise from the superficial circular muscular layer or muscularis mucosa can be removed with endoscopic enucleation[20]. These procedures are technically demanding and require considerable experience and skill. Some of these cases take place in the endoscopy suites, but are often coordinated with surgical specialists to assist with the management of hemorrhage or gastric perforation. Often these resections are best performed in surgical operating rooms using laparoscopic-assisted techniques with an experienced surgeon present for the operation.
Figure 3.
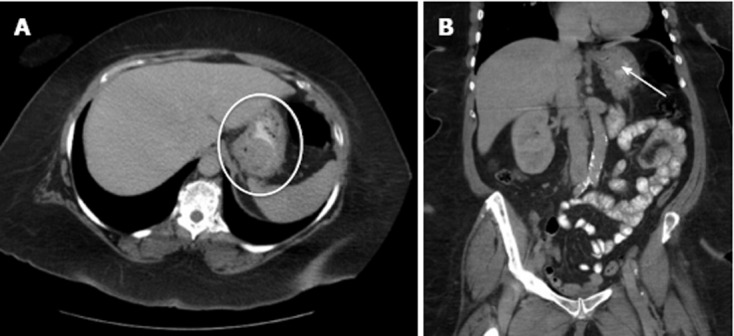
Gastroesophageal junction gastrointestinal stromal tumors. A: An axial computed tomography image of a gastric gastrointestinal stromal tumor (white oval) located along the posterior wall of the gastroesophageal junction (GEJ); B: Coronal images of the tumor (white arrow) show its proximity to the GEJ.
SURGICAL TREATMENT
Surgical treatment of gastric GIST is the only known curative therapy[1]. It is essential to completely remove the entire tumor without violating the capsule of the mass. Tumor spillage or hemorrhage is associated with high locoregional recurrence rates and/or development of peritoneal sarcomatosis[18]. Given the rarity of lymphatic dissemination, regional lymphadenectomy is not routinely performed. Since these tumors originate from the muscular layer of the gastric wall, enucleation is an option, but may be associated with higher recurrence rates unless the intramuscular pedicle can be clearly identified. Standard operations include both “open” and minimally invasive operations. Wedge or a “full-thickness” partial gastrectomy is an effective strategy for tumors that are located along the lesser or greater curvature of the stomach[21]. Posteriorly-based gastric GIST often require transgastric resections through an anterior longitudinal gastrotomy; the tumor is everted and its pedicle divided with a linear stapling device[22]. Anatomic gastrectomy (i.e., subtotal or total gastrectomy) is reserved for large tumors that involve a significant portion of the stomach. Endoscopic-assisted, laparoscopic gastric resections are cutting-edge operations that combine precise intraoperative localization of these tumors with gastric-volume preservation techniques.
NCCN guidelines suggest that small (< 1 cm) gastric GIST without high-risk endoscopic ultrasonographic features (i.e., irregular borders, cystic spaces, ulceration, echogenic foci and heterogeneity) may be followed with close endoscopic surveillance at 6-12 mo intervals (http://www.nccn.org). In the absence of biopsy-proven metastatic disease, patients with an acceptable performance status and GIST confined to the stomach should undergo complete surgical resection. In patients with marginally resectable tumors or in cases that GIST are potentially resectable, but the need for concomitant en bloc organ resection or total gastrectomy is likely, consideration should be given to neoadjuvant treatment with imatinib mesylate to cytoreduce or “downstage” tumors so that a less morbid or less extensive operation can be considered in the future (Figure 4)[23-25].
Figure 4.
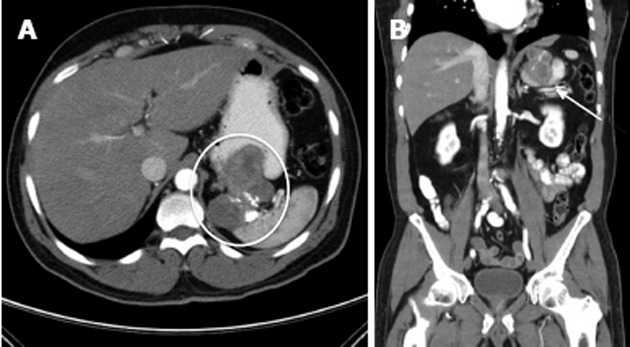
Locally-advanced gastric gastrointestinal stromal tumors. A: Representative contrast-enhanced computed tomography images show a large, proximal gastric gastrointestinal stromal tumors that invades into the splenic hilum (oval); B: On the coronal images the arrow indicates a heterogeneous mass invading into the spleen with areas of viable tumor and necrotic areas represented by calcifications.
Multiple single institutions highlight the increased use of laparoscopic or minimally-invasive operations for gastric GIST[12-16]. Resection techniques include: (1) laparoscopic transgastric resections; (2) laparoscopic full-thickness or “wedge” resections; (3) laparoscopic extramucosal enucleation; and (4) combined laparoscopic, endoscopic resections[26]. The five largest published reports of laparoscopy resections for gastric GIST are summarized in Table 1[12-16]. Most of these retrospective series include non-GIST, benign submucosal tumors (leiomyomas). Although a formal meta-analysis was not performed given the small number of patients, general trends are evident. It appears that minimally-invasive operations for gastric GIST have been successfully used to treat patients with large tumors in difficult locations (i.e., proximal stomach and gastroesophageal junction). The data also suggest reasonable operative times, acceptable complication rates, and few conversions to open operations. Since none of the series had strict criteria for postoperative discharge to home, the reported postoperative length of stay is difficult to interpret, but was shorter than historic controls for open operations. Importantly, despite nearly one-third of the patients having intermediate to high-risk lesions, nearly 100% were completely removed and did not recur after 1-4 years of follow-up[12-16]. We urge caution in broadly extrapolating these results to all patients with gastric GIST; most series had relatively short follow-up, involved a considerable selection bias, and most operations were performed by surgeons with considerable experience with these techniques[27]. Our institutional experience with laparoscopic resection of GIST suggest that these techniques are both feasible and effective treatment for tumors less than eight centimeters in diameter. We advocate using a multidisciplinary approach with combined surgical oncology and minimally-invasive specialists to estimate the biologic behavior and determine the optimal method of resection. Cutting-edge modifications include the use of robot-assisted laparoscopic resections[28], natural orifice surgery[29], gasless laparoscopic resections[30], single-port techniques[31,32], and novel methods of removing posteriorly based tumors[26]. One report described an experimental transgastric technique that utilized the retractable, metal-rimmed EndoCatch bags to elevate posterior wall GIST to facilitate laparoscopic stapled transection of the tumor pedicle[33].
OUTCOMES AFTER SURGICAL RESECTION OF GASTRIC GIST
Since GISTs are rare neoplasms that demonstrate a spectrum of biologic behavior, outcomes following surgical resection are difficult to ascertain. Recurrence free survival appears dependent on tumor size, location, and mitotic rate[6,34]. Prior to the use of imatinib mesylate as an adjuvant treatment following complete resection of gastric GIST, several large, retrospective reports suggest local recurrence rates as high as 40% and five-year survival rates as ranging between 40%-90%[1,35-38]. Dematteo et al[1] published a series of 200 patients with GIST in 2000; more than half of these patients had gastric GIST. In the 93 patients with primary GIST, 80 (86%) had a complete resection with a median disease-specific survival of 54%. Fujimoto et al[36] reported a series of 140 patients that had curative operations for gastric GIST. The five- and ten-year overall survival rates for the 129 patients with “curative” operations were 93% and 88%, respectively. Independent predictors of poor prognosis included male patients [hazard ratio (HR) = 0.469, P = 0.013], tumor size greater than or equal to 10 cm (HR = 20.98, P = 0.001), a mitotic index of 10+ (HR = 45.95, P < 0001), and epithelioid cell histologic component (HR = 5.32, P = 0.014). Models to estimate the risk of recurrence have been created from large, retrospective data set of patients with verified GIST[6,34]. Size (> 10 cm) and mitotic rates greater than five per 50 high-powered fields are the most significant variables that predict malignant behavior.
Conventional chemo- and radiation therapy are historically ineffective adjuvant treatments for GIST and do not significantly improve survival in patients with recurrent, metastatic or unresectable primary tumors[18]. The evolution of targeted therapy has dramatically altered outcomes for patients with advanced GIST. Imatinib mesylate is an orally bioavailable, selective molecular inhibitor of cellular tyrosine kinases. First used to treat Philadelphia chromosome-positive chronic myelogenous leukemia, imatinib inhibits tyrosine receptor kinases such as PDGFR and KIT[39]. The Federal Drug Administration (FDA) approved imatinib mesylate for use in patients with metastatic GIST in 2002. The American College of Surgeons Oncology Group (ACOSOG) phase II non-randomized Z9000 trial examined the use of adjuvant imatinib for one-year following complete resection of high-risk GIST (> 10 cm tumors or ruptured GIST). Imatinib-use was associated with decreased recurrence rates (vs historic controls)[40]. The ACOSOG Z9001 was a randomized, double-blind, placebo-controlled, multicenter trial that conclusively showed a statistically significant reduction in the risk of recurrence with one-year of adjuvant imatinib mesylate therapy (400 mg daily dose; HR = 0.35, range: 0.22-0.53, P < 0.0001)[41]. Seven hundred and thirteen patients with completely resected c-KIT positive GIST (greater than 3 cm) were randomized in an intention to treat analysis. At a median follow-up of 19.7 mo, the study was halted when it became evident that only 30 (8%) of patients in the imatinib group and 70 (20%) in the placebo arm had recurrent disease identified. Further maturation of this data is necessary to determine whether the adjuvant treatment improves overall survival in treated patients.
The FDA approved imatinib mesylate in 2008 as adjuvant therapy following complete resection of GIST for all patients without restrictions on time (to initiate therapy) or histopathologic criteria. The European Medicines Agency approved adjuvant imatinib in 2009 for adult patients with resected c-KIT-positive GIST at significant risk of relapse of disease. At least one year of postoperative imatinib mesylate therapy (400 mg daily) is now considered the standard of care for tumors greater than 3 cm with high-risk features (> 5-10 mitoses/50 high power field) per the results of ACOSOG Z9001[2]. Several postoperative models of risk assessment have been used to estimate the likelihood of recurrence for patients who do not meet the aforementioned criteria[6,34]. The optimal duration of imatinib and long-term survival benefit remains the subject of several ongoing randomized, controlled international cooperative group trials and industry-sponsored studies. Current protocols include the recently completed EORTC 62024 trial that randomized 900 patients with completed resected intermediate- and high-risk GIST to receive either two years of adjuvant imatinib mesylate vs observation. The primary endpoint of the EORTC trial was overall survival, so the final results will require approximately ten years for complete analysis. The Scandinavian Sarcoma Group phase II trial, (SSGXVII; one vs three years of adjuvant imatinib mesylate) and the non-randomized Novartis Pharmaceutical Trial (NCT00867113; five years of adjuvant imatinib) were both designed to test extended use of adjuvant imatinib mesylate following complete resection. Patients at a higher risk of recurrence may justify indefinite use of adjuvant therapy. Three recent cooperative group trials using imatinib in patients with locally-advanced, unresectable or metastatic GIST have suggested that the KIT mutation genotype may have prognostic value to estimate the duration of response and optimal dose of imatinib mesylate[10,42,43]. Patients in these trials with exon 11-mutations had better treatment outcomes (improved tumor response, progression-free survival, and overall survival) when compared to patients with KIT exon 9-mutants and wild-type patients. At the American Society of Clinical Oncology annual meeting in 2010, it was reported that only deletions (all types) in the KIT exon 11 gene was associated with an increased risk of recurrence[44]. Heinrich et al[43] also reported that GIST with KIT exon 9-mutations had higher tumor response rates to neoadjuvant imatinib mesylate with daily doses of 800 mg (vs 400 mg).
POST-OPERATIVE SURVEILLANCE
NCCN guidelines suggest that following complete resection of gastric GIST; patients should be followed with comprehensive history and physical examinations every 3-6 mo for 5 years, then annually (http://www.nccn.org). Abdominal/pelvic contrast enhanced CT scans were recommended every 3-6 mo for at least three to five years postoperatively. Given the risk of renal insufficiency with iodinated contrast and the cumulative ionizing radiation exposure with frequent CT scans, we believe that less intensive surveillance programs should be advocated. MRI remains an acceptable alternative for suitable patients and avoids the deleterious radiation exposure that is associated with serial CT scans. It is reasonable to consider an EGD at one-year after resection to rule out a local or anastomotic recurrence. Less frequent surveillance programs have been suggested for small (< 2 cm), low-risk tumors. Patients on investigational adjuvant protocols routinely are scanned more frequently to determine the efficacy of treatment.
NEOADJUVANT TREATMENT OF LOCALLY-ADVANCED GASTRIC GIST
Locally-advanced “unresectable” or borderline-resectable gastric GIST are often treated with neoadjuvant imatinib mesylate therapy prior to surgical resection (Figure 5)[45]. Theoretically, the use of preoperative imatinib may “downstage” or substantially cytoreduce GIST preoperatively and diminish the need for concomitant, en bloc organ resections. Over the past five years, there have been several small, single-institution; retrospective reports documenting outcomes following neoadjuvant treatment of borderline or locally-advanced GIST (Table 2)[25,44,46-51]. Approximately 75% of these highly selected patients with “unresectable” GIST were subsequently treated with R0/R1 resections. The duration of neoadjuvant therapy and best method of detecting maximal treatment effect have been the subject of two recent phase II trials[52,53]. The RTOG 0132/ACRIN 6665 cooperative group trial prospectively administered “neoadjuvant” imatinib mesylate (600 mg/d) for eight weeks to patients with both potentially resectable (n = 30) and recurrent/metastatic GIST (n = 22)[53]. The majority of patients had disease stabilization; only 12% had a partial tumor response to therapy. Patients were resected with minimal morbidity and given an additional two years of adjuvant therapy. The patients without metastatic disease had estimated two-year progression-free and overall-survival rates of 83% and 93%, respectively. McAuliffe et al[52] randomized 19 patients with locally-advanced GIST to receive “nanoneoadjuvant” imatinib therapy; subjects were given 600 mg/d for 3 d, 5 d or 7 d prior to surgical resection. Seventeen of 19 patients had a subsequent resection without significant morbidity and were given two years of adjuvant therapy. Approximately 30% of these patients had an objective radiologic response to imatinib (CT/PET) and 12% of the resected tumors had an increase in apoptosis by terminal deoxynucleotidyl transferase- mediated dUTP-biotin nick end labeling assay. These studies provide the proof of principle that neoadjuvant imatinib mesylate may be a safe and effective method of treating patients with locally-advanced GIST.
Figure 5.
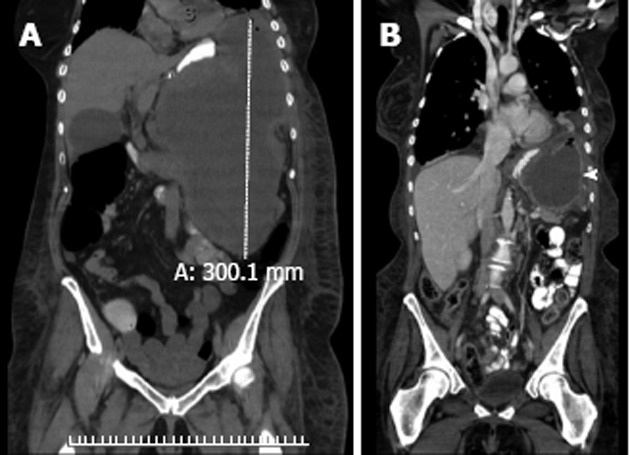
Neoadjuvant treatment of a locally-advanced gastrointestinal stromal tumors with imatinib mesylate. A: This woman presented with abdominal pain and fullness. A computed tomography (CT) scan identified a massive (> 30 cm), homogeneous tumor in the gastric fundus that was exophytic and extending caudally towards the pelvic inlet; B: After tissue diagnosis confirmed a gastric gastrointestinal stromal tumor (GIST), the patient was treated with six months of low-dose imatinib mesylate (400 mg/d) until a maximal response was achieved. The coronal views of this interval CT scan demonstrated a much smaller, well-encapsulated, homogenous tumor (solid white arrowhead). She had a radical resection of the gastric GIST and was free of disease until 24 mo when she developed a metastatic lesion in the left lateral segment of the liver. Following complete metastectomy, she was treated with several targeted tyrosine kinase inhibitors until she ultimately succumbed from her metastatic disease 19 mo from her second operation and 43 mo from her initial operation.
Table 2.
Summary of retrospective single-institutional experience with surgical resection of metastatic gastrointestinal stromal tumor after treatment with imatinib mesylate n (%)
| Ref. | Number of patients | R0/R1 resections |
| Sym et al[47] | 24 | 15 (62) |
| DeMatteo et al[25] | 49 | 39 (80) |
| Gronchi et al[48] | 38 | 31 (82) |
| Raut et al[49] | 69 | 57 (83) |
| Rutkowski et al[51] | 24 | 22 (92) |
| Bonvalot et al[46] | 22 | 15 (68) |
| Andtbacka et al[50] | 46 | 22 (48) |
| Totals | 272 | 201 (74) |
R0/R1 resections: Complete gross removal of the gastrointestinal stromal tumor with/without negative microscopic margins.
CONCLUSION
Gastric GIST are rare neoplasms that have traditionally required complete surgical resection to achieve cure. Both traditional and minimally invasive gastric resections can be used to remove these tumors with minimal morbidity and excellent perioperative outcomes. The revolutionary use of specific, molecularly-targeted therapies, such as imatinib mesylate, reduces the frequency of disease recurrence when used as an adjuvant following complete resection. Neoadjuvant treatment with these agents appears to stabilize disease in the majority of patients and may reduce the extent of surgical resection required for subsequent complete tumor removal. Importantly, tyrosine kinase inhibitors likely extend the progression-free survival of most patients with GIST. The optimal sequencing of therapies and incorporation of predictive genomic data highlight future challenges in this disease.
ACKNOWLEDGMENTS
The authors would like to thank Roberta Carden for proofreading and editing this manuscript.
Footnotes
Peer reviewer: Yasuhiro Kodera, Professor, Department of Surgery II, Nagoya University Graduate School of Medicine, 65 Tsurumai-cho, Showa-ku, Nagoya 4668550, Japan
S- Editor Gou SX L- Editor A E- Editor Xiong L
References
- 1.Dematteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000;231:51–58. doi: 10.1097/00000658-200001000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Demetri GD, von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, Pisters PW, Raut CP, Riedel RF, Schuetze S, et al. NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw. 2010;8 Suppl 2:S1–41; quiz S42-44. doi: 10.6004/jnccn.2010.0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miettinen M, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol. 2005;29:52–68. doi: 10.1097/01.pas.0000146010.92933.de. [DOI] [PubMed] [Google Scholar]
- 4.Nishida T, Nakamura J, Taniguchi M, Hirota S, Ito T, Kitamura Y, Matsuda H. Clinicopathological features of gastric stromal tumors. J Exp Clin Cancer Res. 2000;19:417–425. [PubMed] [Google Scholar]
- 5.Hirota S, Isozaki K, Moriyama Y, Hashimoto K, Nishida T, Ishiguro S, Kawano K, Hanada M, Kurata A, Takeda M, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577–580. doi: 10.1126/science.279.5350.577. [DOI] [PubMed] [Google Scholar]
- 6.Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Miettinen M, O’Leary TJ, Remotti H, Rubin BP, et al. Diagnosis of gastrointestinal stromal tumors: A consensus approach. Hum Pathol. 2002;33:459–465. doi: 10.1053/hupa.2002.123545. [DOI] [PubMed] [Google Scholar]
- 7.Thomas RM, Sobin LH. Gastrointestinal cancer. Cancer. 1995;75:154–170. doi: 10.1002/1097-0142(19950101)75:1+<154::aid-cncr2820751305>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 8.Duensing A, Medeiros F, McConarty B, Joseph NE, Panigrahy D, Singer S, Fletcher CD, Demetri GD, Fletcher JA. Mechanisms of oncogenic KIT signal transduction in primary gastrointestinal stromal tumors (GISTs) Oncogene. 2004;23:3999–4006. doi: 10.1038/sj.onc.1207525. [DOI] [PubMed] [Google Scholar]
- 9.West RB, Corless CL, Chen X, Rubin BP, Subramanian S, Montgomery K, Zhu S, Ball CA, Nielsen TO, Patel R, et al. The novel marker, DOG1, is expressed ubiquitously in gastrointestinal stromal tumors irrespective of KIT or PDGFRA mutation status. Am J Pathol. 2004;165:107–113. doi: 10.1016/S0002-9440(10)63279-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heinrich MC, Corless CL, Demetri GD, Blanke CD, von Mehren M, Joensuu H, McGreevey LS, Chen CJ, Van den Abbeele AD, Druker BJ, et al. Kinase mutations and imatinib response in patients with metastatic gastrointestinal stromal tumor. J Clin Oncol. 2003;21:4342–4349. doi: 10.1200/JCO.2003.04.190. [DOI] [PubMed] [Google Scholar]
- 11.Demetri GD. Targeting c-kit mutations in solid tumors: scientific rationale and novel therapeutic options. Semin Oncol. 2001;28:19–26. [PubMed] [Google Scholar]
- 12.Novitsky YW, Kercher KW, Sing RF, Heniford BT. Long-term outcomes of laparoscopic resection of gastric gastrointestinal stromal tumors. Ann Surg. 2006;243:738–745; discussion 745-747. doi: 10.1097/01.sla.0000219739.11758.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Otani Y, Furukawa T, Yoshida M, Saikawa Y, Wada N, Ueda M, Kubota T, Mukai M, Kameyama K, Sugino Y, et al. Operative indications for relatively small (2-5 cm) gastrointestinal stromal tumor of the stomach based on analysis of 60 operated cases. Surgery. 2006;139:484–492. doi: 10.1016/j.surg.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 14.Sexton JA, Pierce RA, Halpin VJ, Eagon JC, Hawkins WG, Linehan DC, Brunt LM, Frisella MM, Matthews BD. Laparoscopic gastric resection for gastrointestinal stromal tumors. Surg Endosc. 2008;22:2583–2587. doi: 10.1007/s00464-008-9807-1. [DOI] [PubMed] [Google Scholar]
- 15.Wilhelm D, von Delius S, Burian M, Schneider A, Frimberger E, Meining A, Feussner H. Simultaneous use of laparoscopy and endoscopy for minimally invasive resection of gastric subepithelial masses - analysis of 93 interventions. World J Surg. 2008;32:1021–1028. doi: 10.1007/s00268-008-9492-1. [DOI] [PubMed] [Google Scholar]
- 16.Sasaki A, Koeda K, Obuchi T, Nakajima J, Nishizuka S, Terashima M, Wakabayashi G. Tailored laparoscopic resection for suspected gastric gastrointestinal stromal tumors. Surgery. 2010;147:516–520. doi: 10.1016/j.surg.2009.10.035. [DOI] [PubMed] [Google Scholar]
- 17.Davila RE, Faigel DO. GI stromal tumors. Gastrointest Endosc. 2003;58:80–88. doi: 10.1067/mge.2003.317. [DOI] [PubMed] [Google Scholar]
- 18.Gold JS, Dematteo RP. Combined surgical and molecular therapy: the gastrointestinal stromal tumor model. Ann Surg. 2006;244:176–184. doi: 10.1097/01.sla.0000218080.94145.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gu M, Ghafari S, Nguyen PT, Lin F. Cytologic diagnosis of gastrointestinal stromal tumors of the stomach by endoscopic ultrasound-guided fine-needle aspiration biopsy: cytomorphologic and immunohistochemical study of 12 cases. Diagn Cytopathol. 2001;25:343–350. doi: 10.1002/dc.10003. [DOI] [PubMed] [Google Scholar]
- 20.Ludwig K, Weiner R, Bernhardt J. [Minimally invasive resections of gastric tumors] Chirurg. 2003;74:632–637. doi: 10.1007/s00104-002-0570-x. [DOI] [PubMed] [Google Scholar]
- 21.Cueto J, Vázquez-Frias JA, Castañeda-Leeder P, Baquera-Heredia J, Weber-Sánchez A. Laparoscopic-assisted resection of a bleeding gastrointestinal stromal tumor. JSLS. 1999;3:225–228. [PMC free article] [PubMed] [Google Scholar]
- 22.Morinaga N, Sano A, Katayama K, Suzuki K, Kamisaka K, Asao T, Kuwano H. Laparoscopic transgastric tumor-everting resection of the gastric submucosal tumor located near the esophagogastric junction. Surg Laparosc Endosc Percutan Tech. 2004;14:344–348. doi: 10.1097/01.sle.0000148467.33437.c4. [DOI] [PubMed] [Google Scholar]
- 23.Demetri GD. Identification and treatment of chemoresistant inoperable or metastatic GIST: experience with the selective tyrosine kinase inhibitor imatinib mesylate (STI571) Eur J Cancer. 2002;38 Suppl 5:S52–S59. doi: 10.1016/s0959-8049(02)80603-7. [DOI] [PubMed] [Google Scholar]
- 24.Dematteo RP, Heinrich MC, El-Rifai WM, Demetri G. Clinical management of gastrointestinal stromal tumors: before and after STI-571. Hum Pathol. 2002;33:466–477. doi: 10.1053/hupa.2002.124122. [DOI] [PubMed] [Google Scholar]
- 25.DeMatteo RP, Maki RG, Singer S, Gonen M, Brennan MF, Antonescu CR. Results of tyrosine kinase inhibitor therapy followed by surgical resection for metastatic gastrointestinal stromal tumor. Ann Surg. 2007;245:347–352. doi: 10.1097/01.sla.0000236630.93587.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schubert D, Kuhn R, Nestler G, Kahl S, Ebert MP, Malfertheiner P, Lippert H, Pross M. Laparoscopic-endoscopic rendezvous resection of upper gastrointestinal tumors. Dig Dis. 2005;23:106–112. doi: 10.1159/000088591. [DOI] [PubMed] [Google Scholar]
- 27.Roggin KK, Posner M. What is the long-term safety and efficacy of laparoscopic resection for gastric gastrointestinal stromal tumors? Nat Clin Pract Gastroenterol Hepatol. 2007;4:76–77. doi: 10.1038/ncpgasthep0686. [DOI] [PubMed] [Google Scholar]
- 28.Buchs NC, Bucher P, Pugin F, Hagen ME, Morel P. Robot-assisted oncologic resection for large gastric gastrointestinal stromal tumor: a preliminary case series. J Laparoendosc Adv Surg Tech A. 2010;20:411–415. doi: 10.1089/lap.2009.0385. [DOI] [PubMed] [Google Scholar]
- 29.Nakajima K, Nishida T, Takahashi T, Souma Y, Hara J, Yamada T, Yoshio T, Tsutsui T, Yokoi T, Mori M, et al. Partial gastrectomy using natural orifice translumenal endoscopic surgery (NOTES) for gastric submucosal tumors: early experience in humans. Surg Endosc. 2009;23:2650–2655. doi: 10.1007/s00464-009-0474-7. [DOI] [PubMed] [Google Scholar]
- 30.Wu JM, Yang CY, Wang MY, Wu MH, Lin MT. Gasless laparoscopy-assisted versus open resection for gastrointestinal stromal tumors of the upper stomach: preliminary results. J Laparoendosc Adv Surg Tech A. 2010;20:725–729. doi: 10.1089/lap.2010.0231. [DOI] [PubMed] [Google Scholar]
- 31.Henckens T, Van de Putte D, Van Renterghem K, Ceelen W, Pattyn P, Van Nieuwenhove Y. Laparoendoscopic single-site gastrectomy for a gastric GIST using double-bended instruments. J Laparoendosc Adv Surg Tech A. 2010;20:469–471. doi: 10.1089/lap.2009.0391. [DOI] [PubMed] [Google Scholar]
- 32.Hirano Y, Watanabe T, Uchida T, Yoshida S, Kato H, Hosokawa O. Laparoendoscopic single site partial resection of the stomach for gastrointestinal stromal tumor. Surg Laparosc Endosc Percutan Tech. 2010;20:262–264. doi: 10.1097/SLE.0b013e3181e36a5b. [DOI] [PubMed] [Google Scholar]
- 33.Warsi AA, Peyser PM. Laparoscopic resection of gastric GIST and benign gastric tumours: evolution of a new technique. Surg Endosc. 2010;24:72–78. doi: 10.1007/s00464-009-0561-9. [DOI] [PubMed] [Google Scholar]
- 34.Dematteo RP, Gold JS, Saran L, Gönen M, Liau KH, Maki RG, Singer S, Besmer P, Brennan MF, Antonescu CR. Tumor mitotic rate, size, and location independently predict recurrence after resection of primary gastrointestinal stromal tumor (GIST) Cancer. 2008;112:608–615. doi: 10.1002/cncr.23199. [DOI] [PubMed] [Google Scholar]
- 35.Crosby JA, Catton CN, Davis A, Couture J, O’Sullivan B, Kandel R, Swallow CJ. Malignant gastrointestinal stromal tumors of the small intestine: a review of 50 cases from a prospective database. Ann Surg Oncol. 2001;8:50–59. doi: 10.1007/s10434-001-0050-4. [DOI] [PubMed] [Google Scholar]
- 36.Fujimoto Y, Nakanishi Y, Yoshimura K, Shimoda T. Clinicopathologic study of primary malignant gastrointestinal stromal tumor of the stomach, with special reference to prognostic factors: analysis of results in 140 surgically resected patients. Gastric Cancer. 2003;6:39–48. doi: 10.1007/s101200300005. [DOI] [PubMed] [Google Scholar]
- 37.Pierie JP, Choudry U, Muzikansky A, Yeap BY, Souba WW, Ott MJ. The effect of surgery and grade on outcome of gastrointestinal stromal tumors. Arch Surg. 2001;136:383–389. doi: 10.1001/archsurg.136.4.383. [DOI] [PubMed] [Google Scholar]
- 38.Langer C, Gunawan B, Schüler P, Huber W, Füzesi L, Becker H. Prognostic factors influencing surgical management and outcome of gastrointestinal stromal tumours. Br J Surg. 2003;90:332–339. doi: 10.1002/bjs.4046. [DOI] [PubMed] [Google Scholar]
- 39.Demetri GD, von Mehren M, Blanke CD, Van den Abbeele AD, Eisenberg B, Roberts PJ, Heinrich MC, Tuveson DA, Singer S, Janicek M, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002;347:472–480. doi: 10.1056/NEJMoa020461. [DOI] [PubMed] [Google Scholar]
- 40.Dematteo R, Owzar K, Antonescu CR, Maki CD, Demetri GD, McCarter M, von Mehren P, Pisters P, Brennan MF, Ballman KV, et al. Efficacy of adjuvant imatinib mesylate following complete resection of localized, primary gastrointestinal stromal tumor (GIST) at high risk of recurrence: The U.S. Intergroup phase II trial ACOSOG Z9000. 2008 Gastrointestinal Cancers Symposium.2008. [Google Scholar]
- 41.Dematteo RP, Ballman KV, Antonescu CR, Maki RG, Pisters PW, Demetri GD, Blackstein ME, Blanke CD, von Mehren M, Brennan MF, et al. Adjuvant imatinib mesylate after resection of localised, primary gastrointestinal stromal tumour: a randomised, double-blind, placebo-controlled trial. Lancet. 2009;373:1097–1104. doi: 10.1016/S0140-6736(09)60500-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Debiec-Rychter M, Sciot R, Le Cesne A, Schlemmer M, Hohenberger P, van Oosterom AT, Blay JY, Leyvraz S, Stul M, Casali PG, et al. KIT mutations and dose selection for imatinib in patients with advanced gastrointestinal stromal tumours. Eur J Cancer. 2006;42:1093–1103. doi: 10.1016/j.ejca.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 43.Heinrich MC, Owzar K, Corless CL, Hollis D, Borden EC, Fletcher CD, Ryan CW, von Mehren M, Blanke CD, Rankin C, et al. Correlation of kinase genotype and clinical outcome in the North American Intergroup Phase III Trial of imatinib mesylate for treatment of advanced gastrointestinal stromal tumor: CALGB 150105 Study by Cancer and Leukemia Group B and Southwest Oncology Group. J Clin Oncol. 2008;26:5360–5367. doi: 10.1200/JCO.2008.17.4284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Corless CL, Ballman KV, Antonescu C, Blanke CD, Blackstein ME, Demetri GD, von Mehren M, Maki RG, Pisters PW, Dematteo RP, et al. Relation of tumor pathologic and molecular features to outcome after surgical resection of localized primary gastrointestinal stromal tumor (GIST): Results of the intergroup phase III trial ACOSOG Z9001. 2010 Gastrointestinal Cancers Symposium.2010. [Google Scholar]
- 45.Joensuu H, Fletcher C, Dimitrijevic S, Silberman S, Roberts P, Demetri G. Management of malignant gastrointestinal stromal tumours. Lancet Oncol. 2002;3:655–664. doi: 10.1016/s1470-2045(02)00899-9. [DOI] [PubMed] [Google Scholar]
- 46.Bonvalot S, Eldweny H, Péchoux CL, Vanel D, Terrier P, Cavalcanti A, Robert C, Lassau N, Cesne AL. Impact of surgery on advanced gastrointestinal stromal tumors (GIST) in the imatinib era. Ann Surg Oncol. 2006;13:1596–1603. doi: 10.1245/s10434-006-9047-3. [DOI] [PubMed] [Google Scholar]
- 47.Sym SJ, Ryu MH, Lee JL, Chang HM, Kim TW, Kim HC, Kim KH, Yook JH, Kim BS, Kang YK. Surgical intervention following imatinib treatment in patients with advanced gastrointestinal stromal tumors (GISTs) J Surg Oncol. 2008;98:27–33. doi: 10.1002/jso.21065. [DOI] [PubMed] [Google Scholar]
- 48.Gronchi A, Fiore M, Miselli F, Lagonigro MS, Coco P, Messina A, Pilotti S, Casali PG. Surgery of residual disease following molecular-targeted therapy with imatinib mesylate in advanced/metastatic GIST. Ann Surg. 2007;245:341–346. doi: 10.1097/01.sla.0000242710.36384.1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Raut CP, Posner M, Desai J, Morgan JA, George S, Zahrieh D, Fletcher CD, Demetri GD, Bertagnolli MM. Surgical management of advanced gastrointestinal stromal tumors after treatment with targeted systemic therapy using kinase inhibitors. J Clin Oncol. 2006;24:2325–2331. doi: 10.1200/JCO.2005.05.3439. [DOI] [PubMed] [Google Scholar]
- 50.Andtbacka RH, Ng CS, Scaife CL, Cormier JN, Hunt KK, Pisters PW, Pollock RE, Benjamin RS, Burgess MA, Chen LL, et al. Surgical resection of gastrointestinal stromal tumors after treatment with imatinib. Ann Surg Oncol. 2007;14:14–24. doi: 10.1245/s10434-006-9034-8. [DOI] [PubMed] [Google Scholar]
- 51.Rutkowski P, Nowecki Z, Nyckowski P, Dziewirski W, Grzesiakowska U, Nasierowska-Guttmejer A, Krawczyk M, Ruka W. Surgical treatment of patients with initially inoperable and/or metastatic gastrointestinal stromal tumors (GIST) during therapy with imatinib mesylate. J Surg Oncol. 2006;93:304–311. doi: 10.1002/jso.20466. [DOI] [PubMed] [Google Scholar]
- 52.McAuliffe JC, Hunt KK, Lazar AJ, Choi H, Qiao W, Thall P, Pollock RE, Benjamin RS, Trent JC. A randomized, phase II study of preoperative plus postoperative imatinib in GIST: evidence of rapid radiographic response and temporal induction of tumor cell apoptosis. Ann Surg Oncol. 2009;16:910–919. doi: 10.1245/s10434-008-0177-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Eisenberg BL, Harris J, Blanke CD, Demetri GD, Heinrich MC, Watson JC, Hoffman JP, Okuno S, Kane JM, von Mehren M. Phase II trial of neoadjuvant/adjuvant imatinib mesylate (IM) for advanced primary and metastatic/recurrent operable gastrointestinal stromal tumor (GIST): early results of RTOG 0132/ACRIN 6665. J Surg Oncol. 2009;99:42–47. doi: 10.1002/jso.21160. [DOI] [PMC free article] [PubMed] [Google Scholar]


