Abstract
Angiomyomas of the oral cavity are rare benign vascular neoplasms. In particular, the congenital form has not been reported before in the English language literature. We present a congenital angiomyoma of the tongue that was found on the posterior middle of the tongue in an infant. On MRI, the mass showed an isointense signal to muscle on the T1 weighted image and a slightly hyperintense signal on the T2 weighted image. Immunohistochemically, tumour cells were positive to desmin and smooth muscle actin, but negative to vimentin and S100. The treatment was surgical excision and no recurrence was found during the 26 month follow-up period.
Keywords: angiomyoma, tongue neoplasm, magnetic resonance imaging
Introduction
Angiomyoma, sometimes called angioleiomyoma, is a benign smooth muscle neoplasm that can be classified as three histological types on the basis of their cytoarchitecture: solid, venous and cavernous subtypes.1 Most angiomyomas have been observed in the subcutaneous tissue of the lower extremities.1 It is very rare in the oral cavity, especially in the tongue.2 In a previous study, the incidence of oral angiomyoma was reported as 2.7%.3 In a study of the head and neck, angiomyoma was not found in the tongue but was found in the lip in three cases.4 Another study reports that out of 12 oral lesions only 1 was found on the tongue.5
Oral angiomyomas are usually found between the ages of 30 and 50 years and are rarely seen in children.4,6 It is very hard to decide the proper time for surgical resection of the congenital lesion. In the case of congenital angiomyoma, it is very hard to find any information for treatment timing because of its rarity. If there is a congenital tongue mass in a neonate, radiographic findings are especially important because of the risk of general anaesthesia when performing the biopsy.7 We experienced a case of congenital angiomyoma in the tongue and present it along with a literature review.
Case report
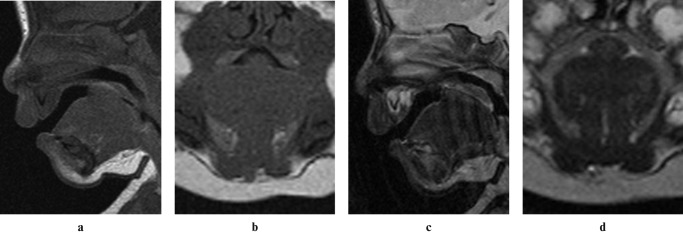
A 2-month-old infant presented with a congenital soft tissue mass in the posterior tongue. The mass was sessile and covered by reddish mucosa and the appearance was not pathognomonic. As the condition of the patient did not allow an incisional biopsy under local or general anaesthesia, MRI was performed under sedation. MRI showed an elevated mass on the base of the tongue (Figure 1). It also showed an isointense signal to muscle on T1 weighted images and a slightly hyperintense signal with a hyperintense rim on T2 weighted images. The tentative diagnosis was a benign lesion of the tongue. The mass was excised under general anaesthesia when the patient was 6 months old.
Figure 1.
Pre-operative MRI. (a, b) T1 weighted images show an isointense signal to muscle and a well-defined margin. (c, d) T2 weighted images show a slightly hyperintense signal with a partially hyperintense rim
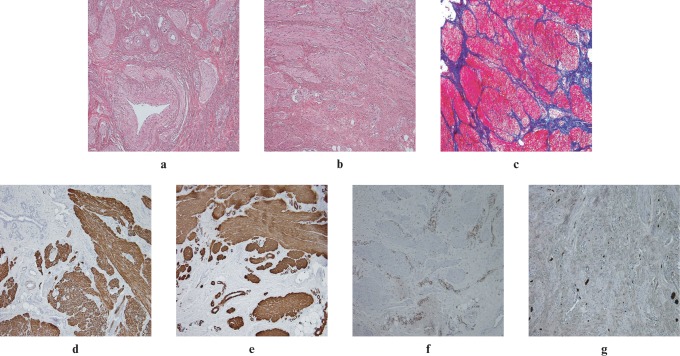
The mass size was approximately 2.5 × 2.0 cm. Histopathologically, the lesion was partially circumscribed and composed of variably prominent and thickened vessel walls consisting of benign and mature smooth muscle cells (Figure 2a). The smooth muscle bundles were interspersed with collagen fibres and tumour cells were spindle shaped with elongated nuclei (Figure 2b). There were few mitotic figures. Masson trichrome (MT) staining showed that the muscle fibre of the lesion stained a purple colour, which indicated the presence of myofibrils in the tumour cells (Figure 2c). In the immunohistochemical studies, the tumour cells showed a positive reaction to desmin (Figure 2d) and smooth muscle actin (SMA) (Figure 2e), but the tumour cells reacted negatively to vimentin (VMT) and S100 (Figure 2 f,g). The final diagnosis was angiomyoma.
Figure 2.
(a) The islands of tumour cells were scattered and the vessel walls were thickened (haematoxylin and eosin, original magnification ×100). (b) The smooth muscle bundles were interspersed with collagen fibres and tumour cells were spindle shaped with elongated nuclei (haematoxylin and eosin, original magnification ×200). (c) Masson trichrome staining revealed red in tumour cell nests (original magnification ×100). (d) The tumour cells were positive to desmin (original magnification ×100). (e) The tumour cells and vessel walls had a positive reaction to smooth muscle actin (original magnification ×100). (f) The tumour cells were negative to vimentin (original magnification ×100). (g) The tumour cells were negative to S100 (original magnification ×100)
The post-operative course was uneventful, and there was no evidence of recurrence 26 months post-operatively.
Discussion
Angiomyoma is usually found in the subcutaneous tissue of the extremities and is rarely found in the oral cavity.8 In the case of lesions in the oral cavity, it is frequently reported on the lip.5 The mean prevalent age for oral angiomyoma is the early fifth decade.3,5 To the best of our knowledge, our case of congenital angiomyoma is the first case report in an English language journal.
Characteristically, angiomyoma on MRI can be described as a well-demarcated, strongly enhancing mass with an isointense to slightly hyperintense signal compared with muscle on T1 weighted images and hyperintense signals on T2 weighted images.8 The MRI findings of our case were in accord with the findings in the literature.8 On the basis of MRI findings, a vascular lesion and benign tumour were suspected. As we had already ruled out malignant tumour, we delayed the biopsy until the risk of general anaesthesia was reduced. Therefore, the radiographic findings of congenital lesions are very important in neonates who cannot receive an incisional biopsy. All vascular lesions, except for lymphatic malformations, are isointense or hyperintense on T1 weighted images and markedly so on T2 weighted images.9 However, the MRI findings of our case showed slightly hyperintense signals, unlike ordinary vascular lesions (Figure 1).
Histologically, the proliferation of smooth muscle cells may resemble other benign spindle-shaped lesions, such as haemangiopericytoma, neurofibroma, neurilemmoma, myofibroma and nodular fasciitis. Special stains like MT or phosphotungstic acid haematoxylin (PTAH) and immunohistochemical stains such as SMA, desmin and VMT can be helpful in the diagnosis. In our case, tumour cells showed positive reactivity to desmin and SMA, and the muscle fibres in the tumour were stained purple in the MT stain (Figure 2). These characteristics demonstrated that the tumour cells originated from primitive muscle cells. The final diagnosis was confirmed as angiomyoma.
Angiomyoma is a slow-growing, firm, elastic, asymptomatic tumour.10 Differential diagnosis includes benign lesions such as fibroma, haemangioma, lymphangioma, teratoma, neurofibroma, granular cell tumour and minor salivary gland tumours. The radiographic study is highly valuable to differentiate the vascular lesion from the others. The vascular lesion from the lymphatic channel will show mixed intensity on MRI without flow voids.11 Fast-flow lesions such as arteriovenous malformation will show many flow voids on MRI.12 Our case did not show prominent flow voids but showed slightly hyperintense signals unlike ordinary vascular lesions on an MRI (Figure 1). The different findings of our case may be due to the immature vessel of the congenital lesion. As congenital angiomyoma has not been presented before, the radiographic and the immunohistochemical features would be valuable for future differential diagnosis.
The treatment for oral angiomyoma is usually surgical excision and recurrence is extremely rare, regardless of the pathological subtype.3 Our case also showed a slow growth rate and showed no recurrence at 26 months' follow-up and there were no complaints. Therefore, congenital angiomyoma might have the same prognosis as oral angiomyoma and urgent resection might not be needed. As this case report was based on a single case, in order to determine the optimum time for resection of congenital angiomyoma and its prognosis, further case reports or case series with long-term follow-up should be encouraged.
References
- 1.Enzinger FM, Weiss SW. Benign tumors of smooth muscle. In:Enzinger FM, Weiss SW. (eds).Soft tissue tumors (4th edn) St Louis, MO: Mosby, 2001. pp 699–700 [Google Scholar]
- 2.Toida M, Koizumi H, Shimokawa K. Painful angiomyoma of the oral cavity: report of a case and review of the literature. J Oral Maxillofac Surg 2000;58:450–453 [DOI] [PubMed] [Google Scholar]
- 3.Hachisuga T, Hashimoto H, Enjoji M. Angioleiomyoma. A clinicopathologic reappraisal of 562 cases. Cancer 1984;54:126–130 [DOI] [PubMed] [Google Scholar]
- 4.Wang CP, Chang YL, Sheen TS. Vascular leiomyoma of the head and neck. Laryngoscope 2004;114:661–665 [DOI] [PubMed] [Google Scholar]
- 5.Brooks JK, Nikitakis NG, Goodman NJ, Levy BA. Clinicopathologic characterization of oral angioleiomyomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:221–227 [DOI] [PubMed] [Google Scholar]
- 6.Ramesh P, Annapureddy SR, Khan F, Sutaria PD. Angioleiomyoma: a clinical, pathological and radiological review. Int J Clin Pract 2004;58:587–591 [DOI] [PubMed] [Google Scholar]
- 7.Bernard JC, Ramon LR. Cleft lip and palate: Comprehensive treatment planning and primary repair. In: Miloro M, Ghali GE.(eds).Peterson’s principles of oral and maxillofacial surgery (2nd edn) Hamilton, Canada: BC Decker, 2004: p 844 [Google Scholar]
- 8.Marden FA, Calilao GC, Guzman G, Roy SS. Glossal angiomyoma: Imaging findings and endovascular treatment. Head Neck 2004;26:1084–1088 [DOI] [PubMed] [Google Scholar]
- 9.Shapiro NL, Malis DJ, Brewster DF, Kearns DB. Evaluation and management of benign, non-congenital tongue masses in children. Int J Pediatr Otorhinolaryngol 1999;48:223–229 [DOI] [PubMed] [Google Scholar]
- 10.Praal FR, Ioannides CA, van Beek GJ, van deMolengraft F. Oral leiomyomas. J Maxillofac Surg 1982;10:229–235 [DOI] [PubMed] [Google Scholar]
- 11.Baker LL, Dillon WP, Hieshima GB, Dowd CF, Frieden IJ. Hemangiomas and vascular malformations of the head and neck show MR characterization. Am J Neuroradiol 1993;14:307–314 [PMC free article] [PubMed] [Google Scholar]
- 12.Shapiro NL, Cunningham MJ, Bhattacharyya , Choi IS, Pile-Spellman J, Joseph MP. Osseous craniofacial arteriovenous malformations in the pediatric population. Arch Otolaryngol Head Neck Surg 1997;123:101–105 [DOI] [PubMed] [Google Scholar]