Abstract
The aim of the report was to establish puncture techniques for the temporomandibular joint (TMJ) cavity in rats.
The experimental sample comprised 30 male Sprague–Dawley rats. Under general anaesthesia the superior joint cavity of the rat was punctured either laterally (lateral puncture technique (LPT), n = 11), anteriorly (anterosuperior puncture technique (ASPT), n = 13) or anteroinferior puncture technique (AIPT), n = 6) using a 27-gauge needle. After the tip of the needle was confirmed by micro-CT (R-mCT®, Rigaku, Tokyo, Japan) located on the mandibular fossa, 0.05 ml of contrast media was injected under micro-CT fluoroscopic guidance. After confirmation that the joint cavity was filled with contrast media, micro-CT imaging was carried out.
The puncture for LPT was accurate in 5 of the 11 animals. The ASPT was accurate in all 13 animals. The AIPT punctured 3 of the 6 animals.
Furthermore, the ASPT and AIPT demonstrated improved preservation of the needle; it was harder to detach the needle, which led to greater stability.
These results suggest that ASPT assisted by R-mCT® is useful for basic research, including drug discovery and pathogenesis of TMJ diseases.
Keywords: micro-computed tomography, temporomandibular joint, puncture technique
Introduction
In studies of joint disease, such as osteoarthritis (OA) or rheumatoid arthritis (RA), animal models have been used extensively for the development of treatment methods and therapeutic agents, as well as the evaluation of the treatment effect.1,2 For the temporomandibular joint (TMJ), models of OA and temporomandibular arthrosis have been developed by the injection of antigens, such as complete Freund's adjuvant (CFA) and occlusal disruption.3–5 In particular, drug-induced models with small animals, such as rats and mice, have been extensively used in physiological, biochemical and histopathological studies. Many articles have described the injection of inflammation-inducing agents into the TMJ cavity; however, the TMJ cavity in model animals is very narrow, and only our previous report has provided evidence of insertion of a needle into the TMJ cavity.6 We developed a CFA-induced temporomandibular OA and reported that a micro-CT scanner for animal experiments (R_mCT®, Rigaku Corporation, Tokyo, Japan) allowed accurate diagnosis of deformity of the mandibular condyle. In a previous study, we used a lateral puncture technique (LPT) to inject CFA into the superior TMJ cavity from the lateral aspect of the joint in rats.6 For accurate injection into the superior joint cavity, a contrast study was conducted under fluoroscopic guidance with micro-CT to confirm that the puncture needle reached the superior joint cavity. The following problems were associated with the LPT: it is not reproducible and often requires re-puncture; and the puncture needle is not held securely in place and is often dislodged during some manipulations. These problems are due to the rat's mandibular fossa protruding laterally and covering the mandibular condyle, and tissues lateral to the TMJ are thin and preclude deep insertion and secure placement of a puncture needle.
The present study was conducted to establish a TMJ cavity puncture technique that is suitable for the structure of the TMJ in rats and allows more reliable, deeper needle insertion.
Materials and methods
Instrument
The micro-CT apparatus (R_mCT®) allows us to obtain high-resolution CT images in small living animals. The X-ray source operates at 90 kV and 88 μA, scan time 17 s, image range ϕ14.4 × 14.4 mm and voxel size 30 × 30 × 30 μm. The animal is placed on the sample bed in the central front portion of the instrument and the built-in laser pointer is used to adjust the position of the subject. It is then moved into the instrument and positioned under fluoroscopic guidance for scanning. The X-ray tube and flat panel rotate around the small animal (a rat in this study) to take cross-sectional X-ray CT images. The I-view-R (J. Morita Mfg. Corp., Kyoto, Japan) was used as the viewer, and diagnosis was made with slice images in any direction.
Subject
This study was approved by the Animal Experimentation Committee of Nihon University School of Dentistry.
The experimental animals were 30 male Sprague–Dawley rats aged 8–9 weeks and weighing 250–350 g. For puncture of the TMJ cavity, rats were anaesthetized with intraperitoneal injection of pentobarbital sodium (Somnopentyl®, 6.48 mg/100 g, Kyourituseiyaku, Tokyo, Japan) diluted in physiological saline. Once anaesthetized the buttocks and head were secured with surgical tape on the micro-CT stage. A 27-gauge injection needle (Nipro, Osaka, Japan) was connected to an extension tube (500 mm, JMS, Tokyo, Japan) and a 1 ml syringe (Nipro, Osaka, Japan) filled with contrast medium (Optiray 320, Tyco Healthcare, Tokyo, Japan), and the extension tube and injection needle were then filled with contrast medium.
Puncture technique
This study compared three techniques for puncture of the superior joint cavity: one puncture technique from the lateral aspect of the TMJ (LPT) and two puncture techniques from the anterior aspect of the TMJ (anterosuperior puncture technique (ASPT) and anteroinferior puncture technique (AIPT)). Puncture was performed by a single dentist (SK).
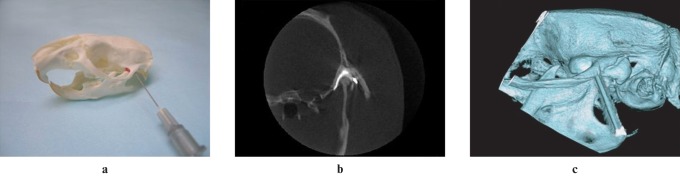
Lateral puncture technique
The zygomatic arch is examined to palpate the base of the zygomatic process of the squamosal bone. The structure from the mandibular angular process to the condylar process is then examined to palpate the base of the condylar process. A puncture needle is inserted from the midpoint between the base of the condylar process and the base of the zygomatic process to the lower base of the zygomatic process, until it reaches bone. When the puncture needle comes in contact with the bone surface it is pulled back approximately 1 mm. The angle of the puncture needle is altered horizontally about 10 degrees, and the puncture needle is advanced until it reaches the glenoid fossa (Figure 1).
Figure 1.
Lateral puncture technique (LPT): (a) simulation image of puncturing using LPT, (b) arthrographic micro-CT image (superior joint cavity was filled with contrast media), and (c) its three-dimensional image
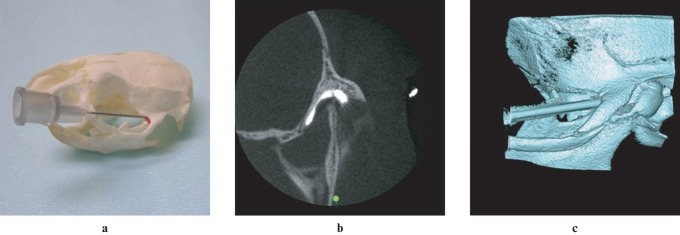
Anterosuperior puncture technique
From the lateral margin of the zygomatic arch, the base of the zygomatic process of the maxilla and the zygomatic process of the squamosal bone are palpated. The superior portion of the zygomatic arch at the midpoint between the base of the zygomatic process of the maxilla and the most prominent bulge of the zygomatic arch is identified as an insertion point, and the interior part of the zygomatic process punctured along the superomedial aspect of the zygomatic arch toward the glenoid fossa (Figure 2).
Figure 2.
Anterior superior puncture technique (ASPT): (a) simulation of puncturing using ASPT, (b) arthrographic micro-CT image (superior joint cavity was filled with contrast media), and (c) its three-dimensional image
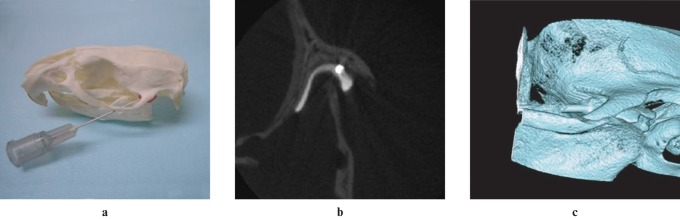
Anteroinferior puncture technique
As with the ASPT, the landmark is palpated from the lateral margin of the zygomatic arch. The inferior base of the zygomatic process of the maxilla is identified as an insertion point, and the interior part of the zygomatic arch punctured along the interior part of the zygomatic arch toward the glenoid fossa (Figure 3).
Figure 3.
Anterior inferior puncture technique (AIPT): (a) simulation image of puncturing using AIPT, (b) arthrographic micro-CT image (superior joint cavity was filled with contrast media), and (c) its three-dimensional image
Arthrography
To confirm the puncture, the tip of the puncture needle in the mandibular fossa was confirmed fluoroscopically and 0.05 ml of contrast medium was injected. The retention of contrast medium in the superior joint cavity was confirmed, and CT scan was performed.
Evaluation method
Success or failure of puncture
The success or failure of the puncture was determined by reviewing contrast-enhanced CT images taken by CT scanning after fluoroscopy. Puncture was considered a success when the superior joint cavity was enhanced and considered a failure when the inferior joint cavity was enhanced, or a large amount of contrast medium leaked into the surrounding tissue. The success rate for each puncture technique was calculated and the differences between puncture techniques were examined using the χ2 test or Fisher's exact probability test.
Puncture time
Rats were placed securely on a sample bed and the time from the start of puncture to fluoroscopic confirmation of injection of contrast medium into the superior joint cavity (completion of time measurement) was measured. The maximum puncture time was set at 20 min, and puncture was considered unfeasible after 20 min.
Arthrographic image
The contrast-enhanced CT images were independently assessed by two different oral and maxillofacial radiologists (KM and KH).
Results
Success and failure of puncture
The puncture for the LPT was accurate in 5 of the 11 animals. The ASPT was accurate in all 13 animals. The AIPT permitted puncture in 3 of the 6 animals (Table 1). There was a statistical difference among the three methods. The puncture success rate was significantly higher with the ASPT than with the other two techniques. There was no significant difference between the LPT and AIPT (Table 1).
Table 1. Failure was defined as puncture requiring manipulation for 20 min or longer. There was statistical difference among the three methods (P = 0.007; χ2 test). The anterosuperior puncture technique (ASPT) produced a higher success rate than the lateral puncture technique (LPT) and the anteroinferior puncture technique (AIPT) (P = 0.003, 0.02; Fisher's exact test). There was no difference between the LPT and the AIPT (P = 0.83; Fisher's exact test).
| Success | Failure | Total | % success | |
| LPT | 5 | 6 | 11 | 45 |
| ASPT | 13 | 0 | 13 | 100 |
| AIPT | 3 | 3 | 6 | 50 |
Puncture time
Almost of all of the success cases using LPT required 10 min or more to puncture. 9 of the 13 success cases using ASPT could be punctured within 10 min. When the AIPT was used puncture time was over 10 min (Table 2).
Table 2. The puncture time (up to 20 min) was defined as the time from the start of puncture to fluoroscopic confirmation of the flow of contrast medium into the joint cavity.
| Within 2 min | Within 5 min | Within 10 min | Over 10 min | |
| LPT | 0 | 1 | 0 | 4 |
| ASPT | 3 | 6 | 3 | 1 |
| AIPT | 0 | 0 | 0 | 3 |
LPT, lateral puncture technique; ASPT, anterosuperior puncture technique; AIPT, anteroinferior puncture technique
Arthrographic image
When puncture was successful, clear contrast-enhanced images were obtained regardless of the puncture technique used (Figure 1–3). The superior joint cavity filled with contrast media had approximately the same morphology in all cases, regardless of type of puncture. While the shape of the superior joint cavity of rats was similar to that of humans, the condyle of rat was widely covered by the joint cavity.
Discussion
The degree of difficulty of puncture of the TMJ cavity depends on the structure as well as the size of subjects. Puncture of the TMJ cavity is very difficult in small animals because the TMJ cavity is narrower compared with humans. There have been some reports providing evidence of puncture of the TMJ cavity in larger animals; however, similar reports in small animals, such as rats, are limited.6 Although the mechanisms of RA and OA are different from those of classic inflammation, lesions primarily occur in the synovium and cartilage constituting the joint cavity, leading to joint deformity. In comparison with injection of an inflammation-inducing agent into the joint cavity, injection outside the joint cavity may induce more extensive inflammation involving the muscle and the ligament, which is likely to impair joint function and prolong inflammatory symptoms. In preparation of an OA model, without the systemic symptoms seen in RA, injection outside the joint cavity may cause significant extra-articular manifestations and confound the interpretation of study results, particularly in physiological experiments. Sodium hyaluronate preparations and steroid formulations are now widely used as intra-articular injections; however, when sodium hyaluronate is injected into the tissue surrounding the joint cavity it is known to induce adverse reactions, such as pain. It is therefore necessary, from a clinical and experimental point of view, to establish a technique for injecting drugs into the TMJ cavity. In the present study, the puncture technique from the lateral aspect of the mandibular condyle (LPT), as commonly used in humans, was compared with the anterior puncture technique. In the coronal section, the glenoid fossa overhangs the mandibular condyle, and the TMJ in rats is not amenable to a LPT anatomically. In rats, the distance between the mandibular condyle and the glenoid fossa is about 0.5 mm, which makes accurate puncture difficult. Regarding the anterior puncture techniques, approaches from the anterosuperior aspect (ASPT) and the anteroinferior aspect (AIPT) of the zygomatic arch were selected. Posterior and inferior approaches to the TMJ were also considered; however, the posterior puncture technique was anatomically very difficult, and the inferior puncture technique resulted in excessively deep insertion and did not allow for fine adjustment. Puncture was not feasible in the preliminary experiment, and these approaches were not used in the main experiment. In the main experiment, the puncture success rate for the ASPT was significantly higher than for the LPT and the AIPT. When the insertion point is determined before puncture by the ASPT or the AIPT, the anterior root and the posterior root of the zygomatic arch are identified as landmarks by palpation, which makes palpation relatively easy. When the LPT is used, the mandibular condyle should be palpated; however, the mandibular condyle is flat anteroposteriorly in rats and the lateral structure of the mandibular fossa makes palpation difficult. When the ASPT or the AIPT is used the direction and angle of puncture are easily determined because puncture is performed along the zygomatic arch. Taken together, it is easier to determine the insertion point and direction by the anterior puncture techniques compared with the LPT. The major difference between the ASPT and the AIPT lies in whether the cavity is approached from the superior aspect or the inferior aspect of the zygomatic arch. Both techniques are better with respect to the determination of the insertion point and puncture angle as described above because a needle is advanced along the zygomatic arch. In the main experiment, the ASPT produced a higher success rate. When the AIPT is used, the anatomical structures make the puncture needle come in contact with the lower margin of the zygomatic arch, and excessively deep insertion makes fine adjustment difficult. These problems may be responsible for the difference in the success rate. Statistical analysis of the puncture time was not performed due to the operator's technical improvement and operating environments. However, analysis of the distribution of the puncture time suggests that the ASPT puncture time appeared shorter compared with the other two techniques. This may be explained by the accuracy and simplicity, as described above. The puncture needle is inserted into a very narrow space and is easily dislodged from the TMJ cavity when the experimental animal moves or the needle comes in contact with other objects during manipulation. To avoid this, the needle should be inserted as deeply as possible. In the AIPT, however, excessively deep insertion precludes fine adjustment and often requires repeat punctures, leading to greater surgical stress on the punctured tissue.
Clear arthrographical images of superior joint cavity in living rats were obtained using the R_mCT® in this study. The R_mCT® advantages include high resolution and short imaging time and we believe that the R_mCT® is the optimal apparatus for animal experiments. The morphological features of contrast-enhanced joint cavity of rats were the inner and outer spread around the condyle. It seems that the proportion of superior joint cavity to the condyle of rat is larger than that of human. This feature may have arisen from differences in eating habits and jaw movement systems.
Because puncture of the TMJ cavity is associated with risks of infection and damage to the cartilage, bone tissue and blood vessels,7 surgical stress should be minimized as much as possible. Particularly in experiments with small animals, puncture-induced tissue damage is likely to influence the experimental results. Anti-tumour necrosis factor-α drugs have recently been used for the treatment of RA in the temporomandibular joint, and their usefulness has been reported.8–10 Many cytokines are involved in TMJ disorders,11 and a variety of anti-arthritic drugs will be developed in the future. In the field of drug discovery, animal experiments are performed to develop therapeutic agents and evaluate efficacy. In these experiments, the ASPT may be more useful.
In the present study, all experimental procedures were performed by one dentist (SK); therefore, the data may be biased. However, we expect that many researchers will use ASPT in physiological and pharmacological studies in the future and this will develop the efficiency of ASPT and help to polish the methodology.
In conclusion, the ASPT puncture of the superior TMJ cavity in rats is more reliable than the commonly used lateral approach. This method may be a useful technique in animal experiments to evaluate the treatment of TMJ disorders, particularly in the context of observation of pathological changes and development of anti-arthritic drugs.
Acknowledgments
This study was supported by the Sato Fund and the Uemura Fund and a grant from the Dental Research Center, Nihon University School of Dentistry, a Grant for the Promotion of Multi-disciplinary Research Projects entitled “Translational Research Network on Orofacial Neurological Disorders” from the Japanese Ministry of Education, Culture, Sports, Science, and Technology.
References
- 1.Dinser R. Animal models for arthritis. Best Pract Res Clin Rheumatol 2008;22:253–267 [DOI] [PubMed] [Google Scholar]
- 2.Rainsford KD. Adjuvant polyarthritis in rats: is this a satisfactory model for screening anti-arthritic drugs? Agents Actions 1982;12:452–458 [DOI] [PubMed] [Google Scholar]
- 3.Mobireek AF, Darwazeh AM, Hassanin MB. Experimental induction of rheumatoid arthritis in temporomandibular joint of the guinea pig: a clinical and radiographic study. Dentomaxillofac Radiol 2000;29:286–290 [DOI] [PubMed] [Google Scholar]
- 4.D'Attilio M, Scarano A, Quaranta A, Festa F, Caputi S, Piattelli A. Modification of condyle anatomy following a monolateral bite rise: a histological study in rat. Int J Immunopathol Pharmacol 2007;20(Suppl 1):43–47 [DOI] [PubMed] [Google Scholar]
- 5.Tanaka E, Iwabe T, Dalla-Bona DA, Kawai N, van Eijden T, Tanaka M, et al. The effect of experimental cartilage damage and impairment and restoration of synovial lubrication on friction in the temporomandibular joint. J Orofac Pain 2005;19:331–336 [PubMed] [Google Scholar]
- 6.Kameoka S, Kuroki Y, Honda K, Kijima N, Matsumoto K, Asano M, et al. Diagnostic accuracy of micro-computed tomography for osseous abnormalities in the rat temporomandibular joint condyle. Dentomaxillofac Radiol 2009;38:465–469 [DOI] [PubMed] [Google Scholar]
- 7.Westesson PL, Eriksson L, Liedberg J. The risk of damage to facial nerve, superficial temporal vessels, disk, and articular surfaces during arthroscopic examination of the temporomandibular joint. Oral Surg Oral Med Oral Pathol 1986;62:124–127 [DOI] [PubMed] [Google Scholar]
- 8.Fahlgren A, Chubinskaya S, Messner K, Aspenberg P. A capsular incision leads to a fast osteoarthritic response, but also elevated levels of activated osteogenic protein-1 in rabbit knee joint cartilage. Scand J Med Sci Sports 2006;16:456–462 [DOI] [PubMed] [Google Scholar]
- 9.Kopp S, Alstergren P, Ernestam S, Nordahl S, Morin P, Bratt J. Reduction of temporomandibular joint pain after treatment with a combination of methotrexate and infliximab is associated with changes in synovial fluid and plasma cytokines in rheumatoid arthritis. Cells Tissues Organs 2005;180:22–30 [DOI] [PubMed] [Google Scholar]
- 10.Alstergren P, Larsson PT, Kopp S. Successful treatment with multiple intra-articular injections of infliximab in a patient with psoriatic arthritis. Scand J Rheumatol 2008;37:155–157 [DOI] [PubMed] [Google Scholar]
- 11.Matsumoto K, Honda K, Ohshima M, Yamaguchi Y, Nakajima I, Micke P, Otsuka K. Cytokine profile in synovial fluid from patients with internal derangement of the temporomandibular joint: a preliminary study. Dentomaxillofac Radiol 2006;35:432–441 [DOI] [PubMed] [Google Scholar]