Abstract
The aim of this study was to assess general dental practitioners' knowledge of dental radiography and radiation protection in order to alert the Belgian authorities and dental professional societies. Prior to attending a postgraduate course on intraoral radiology, general dental practitioners in Flanders, Belgium, were asked to fill in a questionnaire regarding the radiological equipment and the techniques they used for intraoral radiography. The availability and type of dental panoramic equipment were also assessed. A total of 374 questionnaires were available for this study. 15% of the attendants used radiographic equipment that was more than 27 years old and 43% reported equipment that operated with a clockwork timer. 32% and 75% respectively had no idea what the kV or mA settings were on their intraoral equipment. 5% were unaware which cone geometry or geometric technique (paralleling or bisecting angle technique) they were using. 81% claimed to be using a short cone technique. 47% did not know what collimation meant, whereas 40% stated that they were using circular collimation. 38% used digital intraoral image detectors (63% were photostimulable storage phosphorplate (PSPP)), but 16% were not sure about the type of sensor they were using (PSPP or solid-state sensors). 61% also had dental panoramic equipment available, 25% of which was digital (10% charge coupled device (CCD) and 15% PSPP). These results clearly indicate the need for continued education on this subject. The latter is an important signal to Belgian authorities and dental professional societies.
Keywords: general practitioners, knowledge, radiology, radiation protection
Introduction
General dental practitioners (GDPs), especially Belgian, are real omni-practitioners in the most broad sense of the word. As Belgian legislation obligates dental professionals to perform all radiographs personally, one could expect that they possess all the required knowledge to do so, in addition to all the other activities a GDP has to perform. The fact that Belgian GDPs are obligated to take all radiographs personally may be in strong contrast to other countries where a dental radiographer, an oral hygienist or any other dental auxiliary can perform these duties.
The question remains, however, how much knowledge, of each section of the dental profession, the GDPs still possess once they are qualified and working in the field. This is the reason for the existence of accreditation systems. Although a dental professional should always be prepared to improve his or her knowledge through continuous education, it is a well-known fact that this is more likely to occur if the continued education is mandatory for all dental professionals, for whatever local or federal reasons.
In Belgium, accreditation for dentists is linked to the recognition of the licence to practise. There are three dental specialties that are officially recognized as such in Belgium namely, general dentistry, orthodontics and periodontology. In order to maintain the licence to practise, a dentist is obliged to follow at least 500 units (10 units is 90 min) of postgraduate courses over a period of 5 years. These 500 units should be achieved in several domains of dentistry. The different domains are listed in Table 1. Domain 2, ethics, is mandatory for 50 units. Domain 3, medical imaging in dentistry, should also include radiation protection. It is, however, not specified how much time should be spent studying radiation protection within a 90 min course. It should be stressed that, at the time of the writing this article, the Belgian Federal Agency for Nuclear Control (FANC/AFCN) had proposed increasing the number of accreditation units that should be spent on medical imaging in dentistry and, especially, radiation protection. This is currently under discussion with the Belgian professional dental associations.
Table 1. Domains within dentistry of the accreditation for dentists in Belgium.
| Domain | Definition |
| 0 | No specific domain, could be a mix of the ones below, but should be of value to the profession |
| 1 | General medicine |
| 2 | Ethics and socioeconomic aspects, including organization, of the profession |
| 3 | Medical imaging in dentistry, with inclusion of radiation protection |
| 4 | Preventive and restorative dentistry and endodontics |
| 5 | Paediatric dentistry and orthodontics |
| 6 | Oral pathology, oral surgery and periodontology |
| 7 | Prosthodontics, occlusion and temporomandibular joint disorders |
The Belgian accreditation system for dentists has now been in existence for a little more than ten years, but there is no way of checking whether the quality of the dental care and/or whether individual dentists' knowledge has improved. That is the downside of the system. The positive side is that dentists are positively encouraged to follow these courses. The latter should obviously be acclaimed.
The aim of the present study was to evaluate Flanders' GDPs' knowledge of dental radiology, by means of a questionnaire. The reason for performing this study was to alert the Belgian authorities and Belgian dental professional societies that more attention should be paid to radiation protection in dentistry in our country.
Materials and methods
A questionnaire, which was validated for reproducibility, was used to collect the data for the study. The questionnaire was distributed immediately before an accreditation course on dental radiology, organized and taught by the author. The questionnaires were collected before the lecture started. This was done to avoid biased answers (dentists would get answers to some of the questions in the questionnaire during the lecture). Because this was not a postal questionnaire, the drop-out was nil. This also means that the dentists did not have an opportunity to check their equipment or to consult a book or the internet before answering the questions, as could be the case in a postal questionnaire.
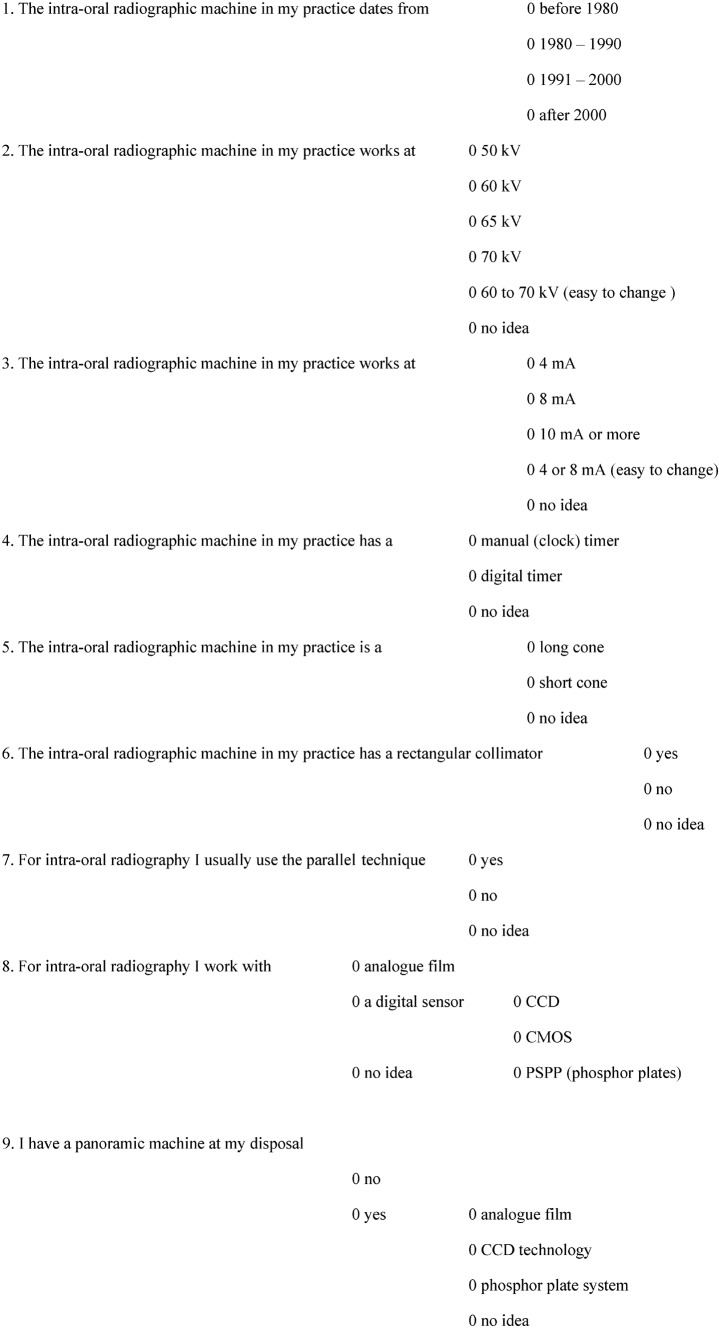
Figure 1 shows the questionnaire (translated from Dutch to English). In the questionnaire, details were asked about the age of the intraoral radiographic unit, kVp and mA of the equipment, the type of timer on the machine and, about the geometry of the machine and the geometric technique used for intraoral radiography. Furthermore, the questionnaire contained questions about the type of intraoral detectors that were used and whether the dentists were also using panoramic machines and, if so, which type of detector they had. Among the possible answers, one option was “no idea”.
Figure 1.
The nine-question questionnaire used in the study.
The results of the questionnaire were digitized as an Excel file (Office 2007 version), which made further descriptive statistical analysis of the data possible with a statistics software program called MedCalc (version 9.6.0.0-2008; Frank Schoonjans, Mariakerke, Belgium).
A total of 374 questionnaires were collected between April 2007 and May 2008. This total is representative of almost 10% of the Flemish dentist population (around 4000).
Results
Regarding the age of the intraoral radiographic equipment used by the questioned population of Flemish dentists, it was found that almost 16% were working with equipment that was at least 27-years-old. 30% were using equipment at least 17-years-old and 26% had equipment that was between 16 and 6-years-old. Another 26% were using radiographic machines for intraoral radiography of not more than 7-years-old.
As the variety of answers about the tube voltage of the intraoral equipment was too large, the answers were condensed into three groups. Therefore, tube voltage ranging from 60 to 70 kV was considered as one category. 63% of the equipment used in Flanders was reported to operate between 60 and 70 kVp. 32% of respondents had no idea at what kVp their equipment was working, whereas 5% claimed to be working at a tube voltage of 50 kVp.
The majority (75%) of the Flemish dentists had no idea at what mA their equipment for intraoral radiographs was working; 25% claimed they knew.
54% claimed to be working with a digital exposure timer, whereas 43% said they were still working with a manual (clock-like) exposure timer.
It was found that 81% said that they were working with a short cone geometry, whereas 14% claimed to be working with a long cone geometry; 5% answered that they had no idea.
47% of the dentists had no idea what collimation they were using. 40% responded that they were using circular collimation and 13% said they were using a rectangular collimator.
81% claimed to be working with the parallel technique, whereas 14% said they were working with the bisecting angle technique; 5% did not have any idea which technique they were using.
Concerning the different types of intraoral sensors, 370 questionnaires out of 374 included an answer. 46% of the dentists in Flanders were still using analogue films for intraoral radiography. 38% had digitized to intraoral sensors (13.5% charge coupled device (CCD), 0.5% complementary metal oxide semiconductor (CMOS) and 24% photostimulable storage phosphor plate (PSPP) for the 370 GDPs). The majority of the respondents (63%) were using PSPP technology. About 16% of the dentists had no idea which type of intraoral sensor they were using.
39% of Flemish dentists did not possess a dental panoramic machine. Of those who did, 34% used analogue films and 25% were equipped with digital machines. The latter were mostly (60%) phosphor plate technology. It is worth mentioning that there were missing replies, as 26 dentists did not answer this question.
The correlations between the answers to the questions about the intraoral detector and the type of panoramic machine used in Flemish private dental practices are shown in Table 2. Some figures have been shown as a percentage to make the sizes of the groups clearer to readers. Dentists using analogue films for intraoral and dental panoramic radiographs made up 20% of the Flemish dental population, whereas those working with CCD technology or PSPP technology for both types of radiographs made up 5% and 11% respectively.
Table 2. Frequency of the answers about the intraoral detector versus the availability and type of dental panoramic equipment.
| Panoramic detector | Intraoral detector |
||||||
| Analogue | CCD | CMOS | PSPP | CCD + PSPP | No idea | Blank | |
| No panoramic | 85 (23%) | 17 (5%) | 1(0.3%) | 20 (5%) | 0 | 10 (3%) | 3 |
| Analogue | 75 (20%) | 13 (3%) | 1(0.3%) | 17 (5%) | 0 | 4 (1%) | 8 |
| CCD | 6 (2%) | 20 (5%) | 0 | 8 (2%) | 0 | 0 | 2 |
| PSPP | 2 (0.5%) | 0 | 0 | 43 (11%) | 4 (1%) | 0 | 2 |
| No idea | 1 | 0 | 0 | 2 | 0 | 4 (1%) | 0 |
| Blank | 0 | 0 | 0 | 0 | 0 | 1 | 25 (7%) |
CCD, charge coupled device; CMOS, complementary metal oxide semiconductor; PSPP, photostimulable storage phosphor plate
Discussion
As mentioned above, the questionnaire was not posted, but was distributed and collected before a lecture on dentomaxillofacial radiology and radiation protection. This implies that some questions, for example the question about the mA setting of the machine may have been answered differently if respondents had had the chance to check their equipment. Nevertheless, a dental professional should know his or her equipment and is expected to know the main guidelines on radiation protection. The results of this study, however, show that this is not the case.
Table 3 shows a comparison between the results of the present study and 6 other surveys carried out less than 7 years ago. Two of these were also reports from Belgian surveys, whereas the others were conducted in Turkey, England and Wales, Syria, and Uganda.1–6 From this table it is clear that there are some similarities, for example the use of rectangular collimation, and some huge differences, for example the availability of panoramic dental equipment. The overall conclusion of all these studies, including the present one, is that there is still a great deal of work to be done to ameliorate the quality of radiographs and the knowledge and attitude of GDPs regarding dentomaxillofacial radiology. This is a task for dentomaxillofacial radiology specialists, who will have to concentrate in the first place on undergraduate teaching and then on postgraduate teaching. The latter is not less important than the first as the working dentist population needs to change their attitude regarding radiation protection and dentomaxillofacial radiology general knowledge. This has also been stressed in other surveys. In the opinion of the author, continued education in dentomaxillofacial radiology is essential, especially when considering a change from analogue to digital radiology.
Table 3. Comparison of the results of the present study with six similar studies carried out in Belgium (Gijbels et al1 and Jacobs et al2), Turkey (Ilgüy et al3), England and Wales (Tugnait et al4), Syria (Salti and Whaites5) and Uganda (Mutyabule and Whaites6).
| Aps, 2010 (n _ 374) | Gijbels et al, 2005 (n _ 350) | Jacobs et al, 2004 (n _ 500) | Ilgüy et al, 2005 (n _ 596) | Tugnait et al, 2003 (n _ 592) | Salti and Whaites, 2002 (n _ 202) | Mutyabule and Whaites, 2002 (n _ 47)∗ | |
| Age of equipment | 15% > 27 years | NM | NM | Mean was 11.3 ± 7.2 years | NM | 16% > 20 years | 42% no idea |
| 60% _ 7–27 years | 52% _ 10–20 years | ||||||
| 25% < 8 years | 32% < 10 years | ||||||
| kV | 63% at 60–70 kV | 76% at 60–70 kV | 70% at 60–70 kV | 87% no idea | NM | 45% at 50 kV or less | 19% at 50 kV |
| 5% at 50 kV | 64% no idea | 60% no idea | |||||
| 32% no idea | |||||||
| mA | 75% no idea | NM | 63% at 10-12 mA | NM | NM | NM | NM |
| Exposure timer | 43% manual | NM | 65% digital | NM | NM | 2% no visual warning signals | 51% manual |
| 54% digital | 4% no audible warning signals | 28% no visual warning signs | |||||
| 3% no idea | 17% no audible warning signs | ||||||
| Beam geometry | 81% short cone | NM | NM | 18% short cone | 63% long cone | NM | NM |
| 14% long cone | 44% long cone | ||||||
| 5% no idea | |||||||
| Collimation | 13% rectangular | 6% rectangular | 6% rectangular | 6% rectangular | 18% rectangular | 0% rectangular | 43% circular |
| 40% circular | 76% circular | 19% cone shape | 69% circular | 51% cone shape | |||
| 47% no idea | 16% cone shape | 19% no idea | 31% cone shape | 6% no idea | |||
| Projection technique | 81% parallel | 60% no aiming device | 60% no aiming device | 31% parallel | 31% parallel | 43% parallel | 13% parallel |
| 14% bisecting angle | 62% bisecting angle | 22% bisecting angle | 57% bisecting angle | 74% bisecting angle | |||
| 5% no idea | 7% no idea | 13% no idea | |||||
| Type of intraoral sensor | 46% analogue | 18% CCD | 16% CCD | 34% analogue | 72% analogue | 99% analogue | 40% no idea of filmspeed |
| 13.5% CCD | 12% PSPP | 18% PSPP | 14% CCD or PSPP | 1% digital with no specification of which type | |||
| 0.5% CMOS | 66% no idea about type of analogue film | 13% no idea of filmspeed | |||||
| 24% PSPP | |||||||
| 16% no idea | |||||||
| Panoramic equipment (DPT) | 39% no DPT | 12% CCD or PSPP | NM | 7% have DPT | 61% have DPT | 99% have DPT | 27% have DPT |
| 34% analogue | |||||||
| 10% CCD | |||||||
| 15% PSPP | |||||||
| 2% no idea |
Figures presented in this table, regarding Mutyabule and Whaites6 refer only to the private dentist's results mentioned in the study. CCD, charged coupled device; PSPP, photostimulable storage phosphor plate; DPT, dental panaramic tomography; NM, not mentioned
That 81% of the dentists in the present survey claimed to be working with a short cone radiographic machine is probably biased by the fact that they are not aware of the difference between a short cone and a short spacer cone, which is also called a beam indicating device or position indicating device. It can be assumed that dentists owning a machine with a short spacer cone, because the manufacturer positioned the focus near the rear end of the machine, gave the wrong answer. Therefore this result should be interpreted with care. The opposite for long cone could also be the case, of course.
The fact that 81% of the dentists in the survey claimed to be using the parallel technique for intraoral radiography may be biased by the way the question was formulated in the questionnaire (Figure 1). There was no choice between the parallel and bisecting angle technique, which probably caused many to choose the affirmative answer. Therefore, this figure of 81% should be ignored. Moreover, when comparing the answers to the questions regarding beam geometry and projection technique, one would get the impression that the Flemish dental population is taking intraoral radiographs with short cone equipment, but using the parallel technique. Can anyone think of more controversy and contradictions?
It is important for readers to know that, according to Belgian legislation, a dentist is obliged to take radiographs personally and cannot delegate this to an auxiliary. The latter can be done only by a medical doctor, according to Belgian law. Therefore, the results of this questionnaire are to be considered a very important message to Belgian authorities and educational boards at university and federal level, as well as to dental professional societies. Taking the results of this questionnaire into account, and the fact that Belgian GDPs are supposed to take radiographs personally, means that there is a great need for postgraduate and continued education on the subject of dentomaxillofacial radiology and radiation protection. This confirms studies carried out in other countries and continents.2–8 If postgraduate education were mandatory, it may have an impact on the GDPs' attitude towards radiation protection and it may result in better quality radiographs.9–11 However, this has been the case in Belgium for 10 years; but, the results do not indicate that there has been an improvement. The 5 year accreditation cycle includes at least 1.5 h of postgraduate education in dental radiography and radiation protection for every dentist. As this survey was carried out near the end of the second 5 year cycle, one can assume that most of the participants had already followed a course during their first 5 year cycle, or that some of them had graduated from dental school less than 5 years ago. The results are, therefore, worrying and should be an indication for the local authorities to act. This could mean, for instance, implementing an increase in the number of hours of under- and/or postgraduate education. If this can be decided by the local authorities and enforced at university level, it has a chance of succeeding. However, at present, every university has its own curriculum and, as known from other studies, it is not always easy to change curricula and convince faculty staff colleagues of this issue.12
Regarding the knowledge of Flemish GDPs, there are various reasons for the results of this questionnaire being so poor. Perhaps the quality and quantity of the undergraduate education is insufficient, perhaps the quantity of postgraduate education is insufficient or perhaps the quality of the available postgraduate education is insufficient. The answer cannot be given, as there is no study material available in Belgium concerning these issues. However, it is the author's personal impression that, for many years, dentomaxillofacial radiology has been taught at every university in the country by medical radiologists or general dentists without specific dentomaxillofacial radiology training. For the last few years, at both the University of Ghent and the Catholic University of Leuven, two qualified dentomaxillofacial radiologists have been in charge of the undergraduate dental radiology programme. Both were trained at King's College in London. It can be assumed that in a few years the results of a similar questionnaire would be more positive.
The major problem with the undergraduate education is the number of hours that should be dedicated to dental radiology. Despite individual efforts to change, the actual number of hours is low: 30 h of dental radiology and radiation protection taught in the third year of dental school. This should be increased in line with other European countries. Perhaps the fact that there is no recognition of dentomaxillofacial radiology being a specialty in Belgium makes the discussion more difficult with other faculty members, compared with the situation in other countries.
The age of the dentists was not assessed, nor was the university where they had studied. Age was not considered an important question in this study, as the age of a dentist does not always reflect that person's knowledge of dental radiology.10–13 Furthermore, it is known that not every young dentist starts with new equipment and, vice versa, that not every “older” dentist is working with old equipment. Therefore, the age of the intraoral radiographic equipment was considered more important and more relevant as a question.
Conclusion
Despite the existence of an accreditation system in Belgium to ensure postgraduate continued education for dentists, the results of this study showed that the knowledge of GDPs in Flanders regarding dentomaxillofacial radiology is poor. This emphasizes the need for better under- and postgraduate education in dentomaxillofacial radiology in Belgium. The present report is therefore an important statement for the Belgian authorities, universities and dental professional societies.
References
- 1.Gijbels F, Debaveye D, Vanderstappen M, Jacobs R. Digital radiographic equipment in the Belgian dental office. Radiat Prot Dosimetry 2005;117:309–312 [DOI] [PubMed] [Google Scholar]
- 2.Jacobs R, Vanderstappen M, Bogaerts R, Gijbels F. Attitude of the Belgian dentist population towards radiation protection. Dentomaxillofac Radiol 2004;33:334–339 [DOI] [PubMed] [Google Scholar]
- 3.Ilgüy D, Ilgüy M, Dincer S, Bayirli G. Survey of dental radiological practice in Turkey. Dentomaxillofac Radiol 2005;34:222–227 [DOI] [PubMed] [Google Scholar]
- 4.Tugnait A, Clerehugh V, Hirschmann PN. Radiographic equipment and techniques used in general dental practice. A survey of general dental practitioners in England and Wales. J Dent 2003;31:197–203 [DOI] [PubMed] [Google Scholar]
- 5.Salti L, Whaites EJ. Survey of dental radiographic services in private dental clinics in Damascus, Syria. Dentomaxillofac Radiol 2002;31:100–105 [DOI] [PubMed] [Google Scholar]
- 6.Mutyabule TK, Whaites EJ. Survey of radiography and radiation protection in general dental practice in Uganda. Dentomaxillofac Radiol 2002;31:164–169 [DOI] [PubMed] [Google Scholar]
- 7.Svenson B, Söderfeldt B, Gröndahl HG. Attitudes of Swedish dentists to the choice of dental X-ray film and collimator for oral radiology. Dentomaxillofac Radiol 1996;25:157–161 [DOI] [PubMed] [Google Scholar]
- 8.Davies C, Grange S, Trevor MM. Radiation protection practices and related continuing professional education in dental radiography: a survey of practitioners in the North-east of England. Radiography 2005;11:255–261 [Google Scholar]
- 9.Smith NJ. Continuing education in radiation protection: assessment of a one-day course. Br Dent J 1991;170:186–188 [DOI] [PubMed] [Google Scholar]
- 10.Svenson B, Söderfeldt B, Gröndahl HG. Knowledge of oral radiology among Swedish dentists. Dentomaxillofac Radiol 1997;26:219–224 [DOI] [PubMed] [Google Scholar]
- 11.Stavrianou K, Pappous G, Pallikarakis N. A quality assurance program in dental radiographic units in Western Greece. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:622–627 [DOI] [PubMed] [Google Scholar]
- 12.Geist JR, Katz JO. Radiation dose-reduction techniques in North-American dental schools. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:496–505 [DOI] [PubMed] [Google Scholar]
- 13.Geist JR, Katz JO. The use of radiation dose-reduction techniques in the practices of dental faculty members. J Dent Educ 2002;66:697–702 [PubMed] [Google Scholar]