Abstract
Objectives
The aim of this study was to evaluate the principal features of “glandular odontogenic cyst” (GOC), by systematic review (SR), and to compare their frequencies among four global groups.
Methods
The databases searched were the PubMed interface of MEDLINE and LILACS. Only those reports of GOCs that occurred in a series in the reporting authors' caseload were considered. All cases were confirmed histopathologically.
Results
18 reports on 17 series of consecutive cases were included in the SR. GOC affected males twice as frequently and the mandible almost three times as frequently. The mean age at first presentation was 44 years, coincident with that of the Western global group, in which the largest proportion of reports and cases first presented in the second half of the fifth decade. However, age at presentation of GOCs in the East Asian and sub-Saharan African global groups was nearly a decade younger, this was significant. Six reports included details of at least one clinical presentation. Eight reports included at least one conventional radiological feature. There were some significant differences between global groups. The Western global group had a particular predilection for the anterior sextants of both jaws. The sub-Saharan African group displayed buccolingual expansion (as did the Latin American group) and tooth displacement in every case. 18% of GOCs recurred overall, except in the sub-Saharan African global group.
Conclusions
GOCs have a marked propensity to recur in most global groups. GOCs presented in older patients and with swellings, affected the anterior sextants of both jaws, and radiologically were more likely to present as a well-defined unilocular radiolucency with buccolingual expansion. Tooth displacement, root resorption and an association with unerupted teeth occurred in 50%, 30% and 11% of cases, respectively.
Keywords: bone, glandular odontogenic cyst, jaw, radiology
Introduction
The “glandular odontogenic cyst” (GOC) has two clinically important attributes: it has “a high recurrence rate”1 and it displays “an aggressive growth potential”.2 Although a relatively new clinical entity, it affords the oral and maxillofacial radiologist the potential of playing an important role in reaching the definitive diagnosis of GOC in some cases. This is, in large part, due to the GOC's complex and frequently non-specific histopathology. Slootweg3 added that the mucus-producing cell contributes to the GOC's histopathological resemblance to a well-differentiated (low-grade) mucoepidermoid carcinoma, requiring entirely different management.
The GOC, also known as the “sialo-odontogenic cyst”, was first clearly identified as a separate entity by Gardner and co-authors4 in 1988. The second edition of the World Health Organization's (WHO) histological classification5 of odontogenic tumours in 1992 recognized it as “a cyst arising in the tooth-bearing areas of the jaws and characterised by an epithelial lining with cuboidal or columnar cells both at the surface and lining crypts or cyst-like spaces within the thickness of the epithelium”.
Although only a recently recognized clinical entity, the GOC is nevertheless an important lesion to recognize and diagnose, because of its potential for aggressive behaviour and a tendency to recur. Since this lesion was first recognized, an adequate number of case series have been published to permit a systematic review (SR) to be performed to determine not only the clinical and radiological features and outcomes of this lesion globally, but also any variation in its presentations within specific communities. Furthermore, such an SR is more likely to reveal any deficiencies in this reported knowledge that should be addressed in later reports. One important point is now clear: Kaplan and co-authors1 recently recommended more stringent criteria for the histopathological diagnosis of GOC (see Discussion). From this recommendation it can be readily concluded that the histopathology of the GOC can be so non-specific, in some cases, as to render it insufficient as the sole test for every case of suspected GOC. Therefore, clinical and radiological features, if they exist with any degree of specificity, should be identified and be recruited to refine further the diagnosis of those cases for which histopathological diagnosis is ambiguous. For example, such a radiological criterion, marginal definition, has been applied to distinguish between the two fibro-osseous lesions, the fibrous dysplasia, a hamartoma; and the ossifying fibroma, a neoplasm.6
Although many syntheses have been published so far, none has followed the formal approach of the SR. This is required to determine whether there may be a specific feature/s that will not only lead the clinician to consider it specifically in a differential diagnosis, but also contribute to the definitive diagnosis. Sackett and co-authors7 defined an SR as a summary of the medical literature that uses explicit methods to search systematically, appraise critically and synthesize the world literature on a specific issue. This means that, unlike a traditional review, the SR, like any other form of primary research, will have a “Materials and methods” section and a “Results” section.8
The SR has generally been applied to treatment and drug trials (most recently to osseointegrated implants),9,10 but has also become a powerful tool when adapted to the clinical and radiological presentations of important oral and maxillofacial lesions6 and on temporomandibular joint disorders.11
Aims and research question
The principal aims are to include as many reports of consecutive series of cases of GOCs presenting for the first time in a particular community, and to evaluate the principal clinical and conventional radiological features of GOC by SR, and then to compare their frequencies between four global groups.
The research question for this SR is: “Can clinical and conventional radiological features assist the histopathologist in reaching a definitive diagnosis of GOC?” This follows the four-part format required for the SR's research question set out by MacDonald-Jankowski and Dozier.8 In order to include as many reports as possible, a wide search of the literature was made, including non-English reports. In addition to a MeSH search, it integrated a free-text search supported both by handsearching of those journals, which are the natural destinations for reports on oral and maxillofacial lesions and by reference-harvesting of those reports identified by the database searches and handsearching.
The four global groups are Western/Caucasian, sub-Saharan African, East Asian and Latin American. They broadly reflect the main ethnic grouping of humanity. It has, hitherto, been generally well recognized that the frequencies and presentations of certain lesions differ between world communities. A purpose of this SR is to identify such groups and to compare frequencies and presentations among them. Although these global groups cannot be wholly composed of one of the divisions of humanity, the Western/Caucasian group containing large minorities of the others, it gives the reader a more relevant view of the clinical and radiological picture of the presentation of a GOC affecting a particular patient presenting within his/her community.
Materials and methods
Systematic review
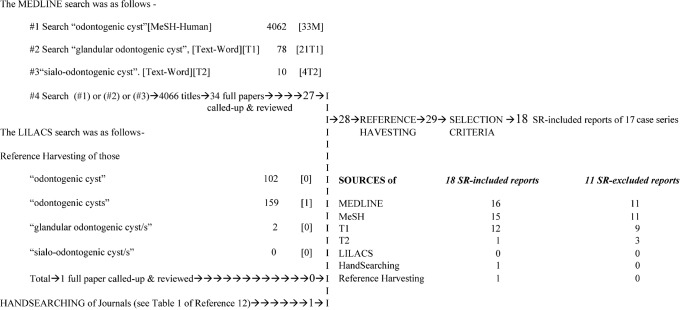
The approach follows the SR procedure set out in earlier SRs for other oral and maxillofacial lesions, most recently the SR on fibrous dysplasia.6 The research question has already been addressed, the search strategy, the strategy for sifting the literature and the interpretation of the data retrieved are set out below. The search strategy and strategy for sifting the literature are set out in Figure 1.
Figure 1.
Glandular odontogenic cyst: systematic review – search strategy and results
The search strategy
The search is based on the foregoing “research question”. The databases searched were the PubMed interface of MEDLINE (National Library of Medicine) and LILACS (Literatura Latino Americana e do Caribe em Ciências da Saúde) by BIREME (Latin American and Caribbean Center on Health Sciences Information). LILACS provides access to important Latin American publications largely not indexed by MEDLINE and has been discussed in the SR on focal osseous dysplasia (FocOD).12
The PubMed interface of MEDLINE was interrogated by the sole MeSH (Medical Subject Heading) “odontogenic cyst”, and the “free-text” terms (text-word) “glandular odontogenic cyst” and “sialo-odontogenic cyst”. These terms were also used to search LILACS. In order to include as many reports as possible, the emphasis is placed on “recall” rather than “precision”, bearing in mind that MeSH for both dentistry and radiology is generally inadequate. Furthermore “free-text” searching may not “hit” the relevant article if the term used was not included in the title or abstract. Therefore, the search strategy was further augmented by reference to the bibliographies (or citation lists) of the reports identified by the databases (reference-harvesting) or handsearching of journals listed in Table 1 of the SR on FocOD.12 Both handsearching and reference-harvesting employed the search terms “glandular odontogenic cyst” and “sialo-odontogenic cyst”. Both database searches and handsearches were last conducted on 10 February 2009.
Table 1. Glandular odontogenic cyst: systematic review–analysis of the included reports.
| First author (year) [database] | National and/or ethnic origin | Period covered | Number of GOCs per year | Gender |
Age, mean (range) in years |
Presenting | Site |
Comments |
||||||
| signs and symptoms | ||||||||||||||
| Males | Females | Presenting duration mean (range) in years | Swelling | Pain | Other | Mandible ant. post. | Maxilla ant. post. | Follow-up (FU) and recurrence | ||||||
| Patron et al (1991)14 [M; Me, T1] | Spanish | ING | 3 | 3 | 0 | 45.3 SD 6.5 (39–52) | 3 | 2 | 0 | 1 (2) 0 | 1 | |||
| 13 SD 9.9 (6–20) | FU 14.7 SD 5.0 | |||||||||||||
| 0 recur | ||||||||||||||
| Günzl et al (1993)15 [M; Me, T1, T2] | German | ING | 4 | 2 | 2 | 41.5 SD 8.8 | ING | ING | ING | 2 | 2 | 0 | 0 | |
| ING | FU ING: 0 recur | |||||||||||||
| Kreider et al (1993)16 [R] | German | 5 years | 6 (1.2) | ING | ING | ING | ING | ING | ING | ING | ||||
| ING | FU ING: ING recur | |||||||||||||
| Daley et al (1994)17 [M; Me, T1] | Canadian | 1967–1993 | 3*(0.1) | ING | ING | ING | ING | ING | ING | ING | *3 referred cases deleted | |||
| 26 years | ING | FU ING | ||||||||||||
| Hussain et al (1995)18 [M; Me, T1] | British (3W, 1B) | ING | 4 | 1 | 3 | 44.0 SD 5.7 (37–49) | 3 | 2 | 0 | 4 | 0 | 0 | 0 | All cross midline |
| DiffDiag: 2 GOC | ||||||||||||||
| 7.5 SD 2.1 (6–9) | FU 37.2 | |||||||||||||
| 1 recur 7 years | ||||||||||||||
| Magnussson et al (1997)19 [M; Me, T1] | Swedish | 19 years | 7 (0.4) | 4 | 3 | 55.6 SD 14.4 (46–75) | 4 | 1 | 3 incid | 3 (5) 1 | 2 | 0 | ||
| 1 diastema | ||||||||||||||
| ING | FU ING: 3 recur | |||||||||||||
| Piloni et al (2000)20 [M; T1] | Argentinian | 1975–1998 | 10 (0.4) | 6 | 3 | 52.0 (10–76) | 10 | 4 | 0 | 3 (9) 3 | 1 | 0 | ||
| 24 years | ING | 2 recur: 1 and 4 years | ||||||||||||
| Tosios et al (2000)21 [M, Me, T1] | Greek | 1986–1990 | 3 (0.6) | 2 | 1 | IIG | ING | ING | ING | ING | ING | |||
| 5 years | ING | FU ING; 2 recur | ||||||||||||
| Mosqueda-Taylor et al (2002)22 [M; Me] | Mexican | 1979–2000 | 2 (0.1) | 2 | 0 | ING | ING | ING | ING | ING | ING | |||
| 22 years | ING | FU ING: ING recur | ||||||||||||
| Noffke et al (2002)23 [M; Me, T1] | South African (Black) | 10 years | 9 (0.9) | 4 | 5 | 35.0 | ING | ING | ING | 0 (6*) 1 | 2 (3) 0 | * 4 cross midline | ||
| ING | FU poor but 0 recur post 10 years | |||||||||||||
| Kaplan et al (2005)24 [M; Me, T1] | Israeli | 1993–2003 | 7 (0.6) | 6 | 1 | 43.0 SD 20.7 | 7 | 0 | 1 numb | 3 | 1 (4) 0 | |||
| 11 years | ING | FU 4.7 SD 2.7 | ||||||||||||
| 1 recur twice | ||||||||||||||
| Shen et al (2006)25,26 [M; Me, T1] | Chinese | 1965–2002 | 12 (0.4) | 8 | 4 | 37.6 (21–64) | 11 | 3 | 1 incid | 4 (7) | 5 | |||
| 37 years | ING | 0 numb | 10 FU 13.3 (2–40) years; 1 recurs after 3 years | |||||||||||
| Jones et al (2006)27 [M; Me, T1] | British | 1975–2004 | 11 (0.4) | 8 | 2 | 48.5 SD 17.0 (31–81) | ING | ING | ING | 11 | 0 | 0 | ||
| 30 years | ING | FU ING | ||||||||||||
| Meningaud et al (2006)28 [M: Me] | French | 1995–2001 | 2 (0.2) | 2 | 0 | 47.5 SD 10.6 | ING | ING | ING | 2 | 0 | |||
| 10 years | ING | FU ING: ING Recur | ||||||||||||
| Shear et al (2006)2 [H] | South African | 1992–2004 | 6 (0.5) | ING | ING | ING | ING | ING | ING | ING | ||||
| 13 years | ING | FU ING: ING Recur | ||||||||||||
| Grossmann et al (2007)29 [M; Me] | Brazilian | 1953–2003 | 2 (0.0) | 0 | 2 | IIG 6th decade | ING | ING | ING | ING | ING | Unspecified referral | ||
| 50 years | ING | FU ING: ING recur | ||||||||||||
| Ochsenius et al (2007)30 [M; Me] | Chilean national | 1976–2004 | 1 (0.1) | 0 | 1 | ING | ING | ING | ING | 1 | 0 | |||
| 18 years | ING | FU ING: ING recur | ||||||||||||
Ant., anterior; B, Black; DiffDiag, differential diagnosis; FU, follow-up; [H], handsearching; IIG, inadequate information given; ING, information not given; Incid, incidental finding; [M], MEDLINE; [Me], MeSH; post, posterior; recur, recurrences; SD, standard deviation; [T1], text-word (glandular odontogenic cyst); [T2], text-word (sialo-odontogenic cyst); W, White/Caucasian * in table refers to * in Comments column
Table 2. Glandular odontogenic cyst: systematic review–mean number of features per systematic review-included reports in relation to global groups.
| Features | Global groups |
||||
| All (no. of reports) | East Asian (no. of reports) | Sub-Saharan African (no. of reports) | Latin American (no. of reports) | Western (no. of reports) | |
| Number of cases | 5.41 SD 3.45 (17) | 12.00 (1) | 7.50 SD 2.12 (2) | 3.75 SD 4.19 (4) | 5.00 SD 2.75 (10) |
| Number of years | 20.00 SD 12.80 (14) | 37.00 (1) | 11.50 SD 2.12 (2) | 26.00 SD 16.33 (4) | 15.14 SD 10.03 (7) |
| Number of GOCs/year | 0.42 SD 0.33 (14) | 0.40 (1) | 0.70 SD 0.28 (2) | 0.15 SD 0.17 (4) | 0.50 SD 0.36 (7) |
| Age at first presentation | 45.00 SD 6.25 (10) | 37.60 (1) | 35.00 (1) | 52.00 (1) | 46.48 SD 4.70 (7) |
| Prior awareness (years) | 10.25 SD 3.89 (2) | ING | ING | ING | 10.25 SD 3.89 (2) |
| Statistical analysis: Student's t-test | |||||
| Number of years: sub-Saharan African vs Latin American | t = 1.87, 4DF, P > 0.05 | ||||
| Number of GOCs/year: sub-Saharan African vs Latin American | t = 2.50, 4DF, P > 0.05 | ||||
| Age at first presentation: Western vs East Asian and sub-Saharan African | t = 5.14, 7DF, 0.01 > P > 0.001 | ||||
ING, information not given
Table 3. Glandular odontogenic cyst: systematic review–number of features per systematic review-included reports in relation to global groups.
| Features | All (no. of reports) | Global groups |
|||
| East Asian (no. of reports) | Sub-Saharan African (no. of reports) | Latin American (no. of reports) | Western (no. of reports) | ||
| Male:female | 48:27 (14) | 8:4 (1) | 4:5 (1) | 8:6 (4) | 28:12 (8) |
| Number of cases; swelling, Y:N | 38:5 (6) | 11:1 (1) | ING | 10:0 (1) | 17:4 (4) |
| Number of cases; pain, Y:N | 13:22 (6) | 3:9 (1) | ING | 4:6 (1) | 6:7 (4) |
| Number of cases; incidental findings, Y:N | 4:39 (6) | 1:11 (1) | ING | 0:10 (1) | 3:18 (4) |
| Number of cases; numb, Y:N | 1:18 (2) | 0:12 (1) | ING | ING | 1:6 (1) |
| Number of jaws; mandible:maxilla | 54:16 (11) | 7:5 (1) | 6:3 (1) | 10:1 (2) | 31:7 (7) |
| Number of sextants; mandible, ant:post | 28:8 (8) | 4:0 (1) | 0:1 (1) | 3:3 (1) | 21:4 (5) |
| Number of sextants; maxilla, ant:post | 7:0 (5) | ING | 2:0 (1) | 1:0 (1) | 4:0 (3) |
| Number of recurrent lesions: Y:N | 10:47 (9) | 1:9 (1) | 0:9 (1) | 2:8 (1) | 7:21 (6) |
There is no significant statistical difference in Table 3
Y:N; yes:no; ant:post; anterior:posterior; ING, information not given; parakeratin.; parakeratinized variant of the odontogenic keratocyst, or now simply the KCOT; orthokeratin.; orthokeratinized variant of the odontogenic keratocyst, or now the orthokeratinizing odontogenic cyst
Strategy for sifting the literature
The titles and abstracts of all reports identified by the databases and handsearching were reviewed to determine whether they could possibly report a consecutive series of cases of GOC first presenting within a particular community. The full papers of those reports that required further consideration were called and reviewed. Only those reports that reported more than one case of GOC were allowed to proceed to the selection criteria stage. The only exception was those reports which reported the presence of just one GOC within a particular community over a stated period of time. Prior to this, their bibliographies (reference lists) were reviewed (reference-harvesting) to ensure that as many reports as possible could be included.
Selection criteria
There were two inclusion (criteria 1 and 2) and three exclusion (criteria A–C) criteria for the SR. Each report passed through these criteria in strict sequence. (For the sake of brevity, only those reports that cannot be readily included, by reference to their title or abstract, will be discussed and cited.)
Information included in the SR was generally reduced to numbers and tabulated, which took account of the number of cases that passed the selection criteria, and, therefore, may differ from the numbers available in the original report. ING (“information not given”) was applied whenever information on a particular feature could not be determined (either expressly or inferentially) from the original text. IIG (“inadequate information given”) is entered against those features which the reporters had not adequately quantified. Other details concerning the selection criteria were set out in a recent paper.6
Inclusion criteria
Criterion 1. Consistency with the WHO classification.
The lesions had to be consistent, at least, with the histopathology established by the WHO's second edition of its classification of odontogenic tumours, which recognized it as the “glandular odontogenic cyst” or the “sialo-odontogenic cyst”.
Criterion 2. A complete collection of GOC cases.
The study should represent a complete collection of cases of GOC, arising within a particular community, occurring in the reporters' caseload. Reports that were merely a selection of cases and those studies which were primarily concerned with specific investigations or a discrete age group, such as children or a particular jaw, were excluded. Single and double case reports were excluded unless it was clear that they were not selected and arose within a particular community within a stated time interval.
Exclusion criteria
Criterion A. Excluded reports already reported and included in the SR.
This prevents double reporting of the same clinical cases, by excluding those reports whose data had already been reported and included in the SR by either the same or different authors, unless the degree of overlap did not exceed 50% and there was at least one statistically different feature between them. Invariably, the most recent, largest and most detailed reports were included in the SR.
Occasionally, data from a report that would normally be excluded under “criterion A” were included in the SR ancillary to the SR-included report for that case series because it contained a detail or feature not reported by the SR-included report.
Criterion B. Excluded cases which recurred after primary treatment performed elsewhere and/or earlier than the range in years of the study.
It reinforces “criterion 2” both by minimizing dilution of the data arising primarily within a specific community and by minimizing contamination of the SR by features that are likely to reflect a recurrent lesion rather than a primary lesion. In order to include only those reports of primary cases arising with that community, it excluded reports:
if the details of their recurred cases could not be identified and deleted
if these unidentified recurred cases exceeded the “less than 5% allowance”, then the whole report was excluded unless there remained at least one feature that clearly referred only to the primary (never been treated before) lesions. The report was included only with regards to that particular feature.
Criterion C. Excluded referred cases
This reinforced “criterion 2” by minimizing dilution of the data arising primarily within a specific community. Therefore, it excluded those reports which included referred cases from outside that community. This is because they may possess unusual features that could skew the profile of GOC within that community, which would, in turn, skew the SR. In order to include only reports of cases arising with that community, it excluded reports:
if their referred cases could not be identified and excluded
if their unidentified referred cases exceeded the “less than the 5% allowance”, then the whole report was excluded unless there remained at least one feature that clearly referred only to those cases arising within that community. The report was included only with regards to that particular feature.
Interpretation of the literature retrieved
Definition of parameters
The definitions of the parameters, such as the “number of years” a report covered, the “number of GOCs per year”, the division of each jaw into sextants and the radiologically apparent boundaries between the basal and alveolar processes for each jaw, are exactly the same as those for the recent SR on FocOD.12
Analysis of features that are either present or absent could be construed from a report. In this SR, such features were cortication and perforations. The mention of their presence in some cases, but not in others in the same report was interpreted as these features being absent. This strategy was not applied to those features pertaining to teeth, such as tooth displacement, root resorption and impaction or non-eruption, unless the reports expressly quantified the number of cases that were edentulous or otherwise, in the affected site.
In the absence of the term “radiolucency” or a synonym, “radiolucency” was implied from the reference to the radiological shape of lesions as “unilocular” or “multilocular”, as these necessarily imply that the lesion was a “radiolucency”.
Global groups
The reports are divided into four global groups based broadly on ethnicity; these are East Asian (represented in this SR by Chinese), sub-Saharan African (predominantly Black African), Western/Caucasian (North America and Europe (including Turkey), Middle East, North Africa and India), and Latin American. Although the “Western” group is predominantly White (Caucasian, classically Europe and the Middle East), it contains significant non-White minorities, particularly from sub-Saharan Africa. The population of the USA was at the last census 69.1% White.13 Reports from the Indian subcontinent were included in the Western/Caucasian group, because 95% of Indians are Caucasian (Indo-Aryans and Dravidians). Although these four global groups are cartographically represented by four almost discrete regions, they are not primarily regional, because variable socioeconomic and other ethnocultural factors also play important roles that affect the availability and provision of diagnosis and treatment. For example, the South Asian nations, including India, although largely Caucasian nations, are still developing their economies, along with many of those of sub-Saharan Africa. Although Africa itself is divided between a largely Caucasian North and a substantially Black sub-Saharan South, it is the latter that constitutes the bulk of both the population of the African continent and the African diaspora. The important point of this global distribution is to determine the number, size and quality of the SR-included reports to determine which communities are well reported and which are underreported.
Statistical analysis
Significant differences in frequencies were tested by the χ2 test with P < 0.05. Significant differences in age were tested by a Student's t-test, with P < 0.05. Only those statistical analyses that are significant are detailed in the text and tables.
Results
Systematic review
The results of the SR are set out in Figure 1. Many of the reports were readily rejected because it was clear from their titles and/or abstracts that they were not of consecutive series of cases of primary GOCs presenting first within a particular community. Of those, MEDLINE and LILACS revealed 34 and 0 reports, respectively; the only report identified by handsearching was that by Shear and Speight.2 Although this was not a periodical, it contained data on a consecutive series of cases of GOC.
For further consideration, the full papers of all 35 reports were called up. Seven were excluded because they were either review articles or reports of odontogenic cysts, which did not include GOCs. The reference lists of the remaining reports were subject to reference-harvesting, which found another report. In total, 29 reports were considered by the selection criteria.
Selection criteria
The selection criteria included 18 reports of 17 case series. The clinical data including follow-up and recurrence are provided in Tables 1–3.2, 14–30 Their distribution according to age in decades and gender is shown in Table 4.14, 15, 18, 19, 23–26,29 Their radiological data and the analysis are given in Tables 52,14,18–20,23–25 and 6. The 11 excluded reports are listed in the Appendix.4,31,35,42,48,–54
Table 4. Glandular odontogenic cyst: systematic review–distribution of cases according to age (in decades) .
| Report (reference) decade | Patron et al (1991)14 | Günzl et al (1993)15 | Hussain et al (1995)18 | Magnussson et al (1997)19 | Noffke and Roubenheimer (2002)23 | Kaplan et al (2005)24 | Qin et al (2005)26 for Shen et al (2006) | Grossmannet al (2007)29 | Overall total | Decade % of total | % of males/decade |
| 0–9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.0 | 00.0 |
| 10–19 | 0 | 0 | 0 | 0 | 4(3:1) | 1(1:0) | 0 | 0 | 5(4:1) | 10.0 | 80.0 |
| 20–29 | 0 | 0 | 0 | 0 | 1(0:1) | 2(1:1) | 6(5:1) | 0 | 9(6:3) | 18.0 | 66.7 |
| 30–39 | 1(1:0) | 2(2:0) | 1(1:0) | 1(1:0) | 0 | 0 | 4(1:3) | 0 | 9(6:3) | 18.0 | 66.7 |
| 40–49 | 1(1:0) | 1(0:1) | 3(0:3) | 1(0:1) | 4(1:3) | 1(1:0) | 2(2:0) | 0 | 13(5:8) | 26.0 | 38.5 |
| 50–59 | 1(1:0) | 1(0:1) | 0 | 2(1:1) | 0 | 2(2:0) | 2(0:2) | 0 | 8(4:4) | 16.0 | 50.0 |
| 60–69 | 0 | 0 | 0 | 2(2:0) | 0 | 0 | 0 | 2 | 4(2:0) | 8.0 | 100.0 |
| 70–79 | 0 | 0 | 0 | 1(0:1) | 0 | 1(1:0) | 0 | 0 | 2(1:1) | 4.0 | 50.0 |
| 80–89 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.0 | 00.0 |
| Total | 3(3:0) | 4(2:2) | 4(1:3) | 7(4:3) | 9(4:5) | 7(6:1) | 14(8:6) | 2 | 50(28:20) | 100.0 | 58.3 |
The number of males and females are in parentheses
Table 5. Glandular odontogenic cyst. systematic review: analysis of the radiology in the systematic review-included reports.
| No of cases | Radiological features |
Expansion |
Tooth displacement |
Root resorption |
Cyst around crown of unerupted tooth? |
||||||||||||||||
| Completely radiolucent? |
Shape |
Degree of marginal definition |
Cortication or sclerosis of the periphery |
Buccolingual |
Lower border of the mandible displaced (and/or eroded) |
Antral involvement |
|||||||||||||||
| Author (year) | Yes | No | Unilocular | Multilocular | Well-defined | Poorly defined | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| Patron et al (1991)14 | 3 | 3 | 0 | 2 | 1 | 3 | 0 | 1 | 2 | ING | ING | ING | ING | ING | ING | 2 | 1 | ING | ING | IIG | IIG |
| Hussain et al (1995)18 | 4 | 4 | 0 | 2 | 2 | 4 | 0 | 3 | 1 | IIG | IIG | ING | ING | ING | ING | ING | ING | 2 | 1 | IIG | IIG |
| Magnusson et al (1997)19 | 7 | 7 | 0 | 3 | 3 | 5 | 0 | IIG | IIG | 3 | 4 | ING | ING | ING | ING | IIG | IIG | ING | ING | ING | ING |
| Piloni et al (2000)20 | 10 | 10 | 0 | 1 | 5 | ING | ING | ING | ING | 10 | 0 | ING | ING | ING | ING | IIG | IIG | IIG | IIG | ING | ING |
| Noffke and Roubenheimer (2002)23 | 9 | 9 | 0 | 7 | 2 | 7 | 2 | 2 | 7 | 9 | 0 | IIG | IIG | ING | ING | 8 | 0 | 0 | 8 | 0 | 8 |
| Kaplan et al (2005)24 | 7 | 6 | 1 | 6 | 1 | 7 | 0 | 1 | 6 | 5 | 2 | ING | ING | 3 | 1 | 3 | 4 | 3 | 4 | 1 | 6 |
| Shen et al (2006)25 | 12 | 12 | 0 | 7 | 5 | 12 | 0 | ING | ING | ING | ING | ING | ING | ING | ING | 2 | 10 | 4 | 8 | 2 | 10 |
| Shear et al (2006)2 | 6 | 6 | 0 | 3 | 3 | 6 | 0 | ING | ING | ING | ING | ING | ING | ING | ING | ING | ING | ING | ING | ING | ING |
| Total | 58 | 57 | 1 | 31 | 22 | 44 | 2 | 7 | 16 | 27 | 6 | 0 | 0 | 3 | 1 | 15 | 15 | 9 | 21 | 3 | 24 |
15 out of the 17 SR-included case series were identified by the MEDLINE database, whereas all 11 SR-excluded reports were identified by MEDLINE; this was not significant (χ2 = 1.45, 1 degree of freedom (df), P > 0.05). 14 of the 15 MEDLINE-indexed SR-included case series were captured by the MeSH; only one, that by Piloni and co-authors,20 was captured solely by the “text-word” “glandular odontogenic cyst”.
The East Asian reports were over-represented among the SR-excluded reports, 4 to only 1 SR-included report, this was significant (χ2 = 4.05, 1df, 0.05 > P > 0.01). There were only two reports excluded under “criterion 1”.
Only one SR-included report was not published in English: Günzl and co-authors' report15 was in German. Two Latin American reports were bilingual,20,22 but, as one of the languages was English, they were considered to be written solely in the English language. The two SR-excluded non-English reports were in Chinese.49,53 The differences between SR-included and SR-excluded reports for English, was not significant (χ2 = 0.99, 1df, P > 0.05).
Analysis of the SR
All SR-included reports were of complete consecutive series of histologically confirmed cases of GOC presenting for the first time for diagnosis and treatment within a particular community.
18 reports were included in the SR (Table 1).14–30 Qin and co-authors'26 report was subsumed (by virtue of “criterion A”) into the more recent report by Shen and co-authors.25 The former26 replaced the latter report25 in Table 4, because it reported the gender and age of each case. Therefore, 17 case series were included in the SR.
Although all four global groups are represented, only Shen and co-authors' report25 (supplemented by Qin and co-authors26) represented the East Asian global group. Nearly 60% of the reports were derived from the Western group.
There was a predilection for males overall and in most global groups, except for the sub-Saharan African global group (Table 3).
The mean age at first presentation was significantly lower for the East Asian and sub-Saharan African global group (each represented by only one report) than for the Western global group (Table 2). The sole Latin American representative first presented at the age of 52 years,20 which was older that the mean age in the Western global group.
Table 4 shows a comparison among eight reports of the distribution according to age in decades. Only one report each represented the East Asian, sub-Saharan African and Latin American global groups. Most of the cases occur in the fifth decade. No cases are reported for the first decade. Men predominate in the second to the fourth decades, whereas women predominate in the fifth.
Two reports, both Western, disclosed the period of awareness by the patients of their lesions prior to presentation for diagnosis and treatment. These periods were 7.5 years in Britain18 and 13 years in Spain.14 They are both small with four and three cases, respectively.
Swelling, pain and discovery as an incidental finding upon first presentation displayed no significant predilection for any global group. Swelling was the most frequent clinical presentation. A case of numbness was observed in only one Western report,24 but had been at least considered in an East Asian report.25
There were 11 reports disclosing the distribution of GOCs between the mandible and maxilla. The mandible was affected almost three times more frequently than the maxilla. Location of the lesions by quadrant or sextant was specified only in eight reports for the mandible and five for the maxilla (Table 3). The GOC has a predilection for the anterior sextants of the mandible and maxilla. Although five of Noffke and Raubenheimer's23 six mandibular GOCs affected both anterior and posterior sextants, the most conspicuous feature of four of them was that they were bilateral and thus crossed the midline.
Table 5 contains eight SR-included reports covering all global groups; only one report each represented the East Asian, sub-Saharan African and Latin American global groups. The general paucity of radiological details is illustrated by the frequent “INGs” and “IIGs” for those features associated with expansion and the GOCs' relationship and effect on teeth (Table 5). The overwhelming majority of GOCs were well-defined unilocular radiolucenies, displaying buccolingual expansion. All GOCs of a sub-Saharan African report23 and a Latin American report20 displayed buccolingual expansion. A sub-Saharan African report23 exhibited a significantly greater number of GOCs associated with tooth displacement, whereas the East Asians exhibit the least. There was a high frequency of root resorption (43%) between the global groups. The association with unerupted teeth was low (11%) for all global groups.
The larger case series reported by Noffke and Raubenheimer23 and the SR-excluded report by Manor and co-authors31 (excluded under “criterion A”) included measurements in metric units. In the former these were derived from panoramic radiographs and in the latter by clinical examination. The former's mesiodistal length of 6.54 cm (SD 4.19) was not significantly longer than the latter's 5.30 cm (SD 1.49) (t = 0.67, 12df, P > 0.05). There was not a significant difference in height between the former's 3.20 cm (SD 0.45) and the latter's 3.19 cm (SD 0.81) (t = 0.09, 12df, P > 0.05). The former's two multilocular GOCs had a greater mesiodistal length than the seven unilocular lesions, whereas the latter's two largest mesiodistally were unilocular and were not associated with perforations.
Perforation of the cortex was reported in three SR-included reports. Magnusson and co-authors,19 Noffke and Raubenheimer23 and Kaplan and co-authors24 reported four cases each. Together they suggest a 52% frequency of perforation. There was no significant difference in frequencies between the two Western and one sub-Saharan African reports (Table 6).
Table 6. Glandular odontogenic cyst: systematic review–number of radiological features per systematic review-included reports in relation to global groups.
| Features | All (no. of reports) | Global groups |
|||
| East Asian (no. of reports) | Sub-Saharan African (no. of reports) | Latin American (no. of reports) | Western (no. of reports) | ||
| Radiolucency, yes:no | 57:1 (8) | 12:0 (1) | 15:0 (2) | 10:0 (1) | 20:1 (4) |
| Shape, Unilocular: multilocular | 31:22 (8) | 7:5 (1) | 10:5 (2) | 1:5 (1) | 13:7 (4) |
| Marginal definition, good:poor | 44:2 (7) | 12:0 (1) | 13:2 (2) | ING | 19:0 ( 4) |
| Cortication, yes:no | 7:16 (4) | ING | 2:7 (1) | ING | 5:9 (3) |
| Perforation, yes:no | 12:11 (3) | ING | 4:5 (1) | ING | 8:6 (2) |
| Buccolingual expansion, yes:no | 27:6 (4) | ING | 9:0 (1) | 10:0 (1) | 8:6 (2) |
| Tooth displacement, yes:no | 15:15 (4) | 2:10 (1) | 8:0 (1) | ING | 5:5 (2) |
| Root resorption, yes:no | 9:21 (4) | 4:8 (1) | 0:8 (1) | ING | 5:5 (2) |
| Associated unerupted tooth, yes:no | 3:24 (3) | 2:10 (1) | 0:8 (1) | ING | 1:6 (1) |
The only statistically significant difference between the above are: Tooth displacement: East Asian vs Western: χ2 = 13.39, 1df, p<0.001 Tooth displacement: Sub-Saharan African vs Western: χ2 = 4.97, 1df, 0.05>p<0.01 Root resorption: Sub-Saharan African vs Western: χ2 = 4.97, 1df, 0.05>p<0.01
Nine reports distributed between all four global groups considered recurrence; only one report each represented the East Asian, sub-Saharan African and Latin American global groups. The overall recurrence rate was 17.5% (Table 3). Although the recurrence rate varied between the global groups from none for the sub-Saharan African to 33% for the Western global groups, this was not significant.
Discussion
A major difference between this SR and the previously published non-SR syntheses on GOCs is that the former does not include case reports per se and is inclusive of a report regardless of the community reported, language of publication and its source. Gardner32 criticized one such non-SR synthesis as he considered it not to be “an accurate source of such information as prevalence and incidence, racial predilection and recurrence rates”.
Although 12 SR-included reports were found by the “text-word” “glandular odontogenic cyst”, 15 were also captured by the only relevant MeSH “odontogenic cyst”. This MeSH was introduced in 1965 and is defined as “Cysts found in the jaws and arising from epithelium involved in tooth formation. They include follicular cysts (e.g. primordial cyst, dentigerous cyst, multilocular cyst), lateral periodontal cysts, and radicular cysts. They may become keratinized (odontogenic keratocysts). Follicular cysts may give rise to ameloblastomas and, in rare cases, undergo malignant transformation.”33 Although this definition is clearly very outdated (follicular cyst is not even an “entry term” (synonym) for dentigerous cysts34), the MeSH itself has a very high “recall” for GOC reports. As expected, there were no GOC reports published earlier than 1987, when Padayachee and Van Wyk35 first reported this lesion.
The necessity to include LILACS in the database search was discussed in an earlier SR.12 The absence of LILACS-indexed Latin American reports on GOC stood in sharp contrast to the four identified by MEDLINE. This suggested that LILACS was not an effective source for GOC reports in this global group. Although this discrepancy may have arisen, as observed in the SR on fibrous dysplasia,6 by not using the WHO's classification of odontogenic neoplasms, MEDLINE's MeSH with the out-of-date definition actually identified more reports than the “text-words”. This indicates that the definition had little or no effect on the MeSH's ability to recall those GOC reports indexed in MEDLINE. Only Piloni and co-authors' report20 had not been indexed under the MeSH “odontogenic cyst”, even though “odontogenic cyst” was their first keyword and thus should not have been overlooked by the indexer. A reason for this oversight may have been that the Spanish text preceded the English part of this bilingual report. MeSH indexing errors were certainly an issue when Piloni and co-authors' report was published.8
Kaplan and co-authors1 recently stated that “due to similarities in microscopic characteristics between GOC and lesions such as botryoid cyst, radicular and dentigerous cysts with mucous metaplasia and more importantly low-grade mucoepidermoid carcinoma, a definitive diagnosis can be difficult to make.” Nevertheless, they added that a diagnosis of GOC had to be based on the mandatory presence of the five major features. These are squamous epithelium, varying thickness, cuboidal eosinophilic (“hob-nail”) cells, mucous (goblet) cells and intraepithelial glandular or duct-like structures.1 Although it is unlikely that any reports used such strict criteria, this statement clearly indicates that the histopathology alone may be considered to be insufficiently specific in each and every case of GOC. Nevertheless, it does raise the possibility that GOCs were underreported in many if not all of the SR-included reports. This could have occurred because the histopathologists assigned a diagnosis of GOC only to those lesions that they were absolutely satisfied fulfilled the requirements of this diagnosis.
To give a better indication of the mean annual incidence the reported community may have experienced, the “number of cases per year” was given rather than the “relative period prevalence” used by many reports, in particular those reporting more than one lesion.22,28–30 Such “relative period prevalences” are dependent upon the classification in vogue.
In Table 4, although men predominated overall and for most decades, women predominated in the fifth decade, which was also the decade with the overall peak incidence for the SR. This anomaly may reflect the hormonal changes occurring in females during the perimenopause or menopause. As a gynaecological and/or obstetric history is unlikely to feature in history-taking in most dental facilities, there are few data to develop this discussion at the present.
88% of GOCs first presented with swelling, whereas 9% were discovered as incidental findings. The wide range of periods of prior awareness in the two, albeit very small, West European reports14,18 was not easy to explain, as the patients in both reports should have had easy access to socialized medicine.
GOCs displayed a predilection for the mandible, and for the anterior sextants of both jaws. Therefore, their minimal association with unerupted teeth can be readily understood, as the majority are distant from the third molars, which account for the great majority of unerupted teeth. Furthermore, Noffke and Raubenheimer23 remarked that their cases had no association with unerupted teeth, but rather displaced erupted teeth. This and the first presentation of GOCs, largely during the third to fifth decades, suggest a predilection for the individual in the prime of his/her life, long after the majority of the adult dentition has erupted.
The multilocular expansile radiological presentation in the anterior sextant recalls that of the general dispositions of both the central giant cell lesion and the solid (multilocular) type of ameloblastoma. 50% of mandibular and 75% of maxillary central giant cell lesions in a recent large Dutch case series were sited in the anterior sextant.36 Although the central giant cell lesion may be readily distinguished from GOCs by their younger mean age at first presentation,36 mean age does not assist in differentiating between the GOC and the solid type of ameloblastoma. Piloni and co-authors20 reported that, out of their 10 GOCs, 4 were thought to be ameloblastomas prior to biopsy; the GOC was not considered in a single case. In one of the most detailed case series of ameloblastomas,37 the solid type of ameloblastoma first presented in the second half of the fourth decade, whereas the GOC in this SR first presented in the later fourth decade and first half of the fifth decade. Furthermore, both lesions displaced teeth and caused root resorption and had little association with unerupted teeth. In the light of the discussion in the preceding paragraph this last feature is not surprising.
Manor and co-authors'31 review of all cases and case series reported in the literature clearly indicated that the primary conventional radiograph for most GOCs is the panoramic radiograph. Some others were imaged solely by periapical radiographs. A single lateral projection was supplemented by an occlusal in only 4 out of the 51 cases they included in their synthesis. This paucity of occlusal radiographs may have contributed to the lack of comment with regards not only to buccolingual expansion, but also to the perforation of the cortex. Five of Manor and co-authors'31 GOCs were also imaged by CT, which displayed these perforations. Nevertheless, they suggested that CT should be “reserved for large lesions, especially multilocular or lesions involving extragnathic structures, such as the sinuses, floor of the nose or the orbital floor”. Although Hisatomi and co-authors38 were able to correlate the presentations of a range of radiological modalities, including MRI in a case of GOC associated with ameloblastoma, in another report they determined that MRI images of a GOC could not be distinguished from those of dentigerous, radicular and nasopalatine cysts.39 Interestingly, distinguishing between these very lesions on the basis of conventional radiology would have presented little trouble in most cases. The GOC's infrequent association with unerupted teeth would have distinguished it from the dentigerous cyst. As the majority of GOCs were multilocular they would have been readily distinguished from the others, which were almost exclusively unilocular. For those GOCs which are unilocular, there was the frequent root resorption to distinguish them.
Several reports included measurements of the GOCs. Only measurements made on CT alone can be considered accurate.40 Noffke and Raubenheimer's23 measurements, made on panoramic radiographs, could be compromised by the distortion inherent in this modality. Measurements on panoramic radiographs are subject to “unequal magnification and geometric distortion across the image”.41 Furthermore, Noffke and Raubenheimer's23 report made no mention of adjustment for their machines' magnification factor, which can be considered only reasonably reliable for those measurements made vertically. Manor and co-authors'31 measurements were made clinically, which means that they are likely to have been smaller than the actual lesion's full extent within the jawbones, which will only be apparent radiologically. Nevertheless, the potential overestimate of the former and the underestimate of the latter did not result in a significant difference between them.
Although Kaplan and co-authors1 reported 85% occurrence of perforation of cortical plate in their non-SR synthesis, this is at variance with the 61% of this SR. A reason for this disagreement has already been expounded in the first paragraph of the discussion.
Not one SR-included report considered a downward expansion of the lower border of the mandible. The only report that did was the SR-excluded double case report by Koppang and co-authors.42
Although 17.5% of GOCs recurred globally, not one GOC recurred in the sub-Saharan African global group, whereas one-third recurred in the Western global group. Even taking into account the Black South African's younger mean age at first presentation, the WHO life expectancy is 50 and 53 years for men and women, respectively.43 Thus, it may be that the individual could have died from other causes before the lesion recurred, whereas the life expectancy in the UK (supplier of most Western cases) is 75 and 80 years for men and women, respectively; 44 the life expectancy in Latin America (Argentina)45 and East Asia (China)46 is 72/78 and 72/75 years respectively. Therefore, there is still ample time for recurrence in these global groups.
Long-term follow-up of GOCs should be undertaken, until risk factors for recurrence, if they exist, can be identified. Although, Kaplan and co-authors24 recommend that GOCs should be followed up for at least 3 years, preferably 7 years, one of Shen and co-authors'25 cases recurred after 3 years and one of Hussain and co-authors'18 recurred after 7 years. Thor and co-authors47 followed up a GOC for 13 years; they treated 11 recurrences during the first 10 years. After the GOC was marginally resected, there were no subsequent recurrences.
Kaplan and co-authors24 stated that the risk of a recurrence increases with size and multilocular appearance. The type of treatment also affects recurrence. So far, resection resulted in no recurrence, reinforcing Thor and co-authors'47 experience.
Conclusions
SR-included reports derived from Western communities were most frequent. Latin American communities were the next best represented.
The language of publication and source had no significant effect on the inclusion or exclusion of a report.
Although GOCs have a predilection for men, except in sub-Saharan Africa, the majority of GOCs occur in the fifth decade, when women may predominate and when they are most likely to be experiencing their menopause. Therefore, consideration should be given to whether a gynaecological history should be included in the history-taking for this and other important oral and maxillofacial lesions.
It is clear from the frequency of “INGs”, distributed particularly in Table 5, that the 8 reports out of the 17 SR-included case series detailed little radiology beyond the fact that the vast majority of GOCs are well-defined unilocular radiolucencies. Only 4 of these reports considered buccolingual expansion. A reason for this is that occlusal images accompanied only a few reported cases. The expectation that a lesion will be imaged in two planes is generally not realized in practice.
There is also a paucity of information on the effects of GOCs on adjacent structures, including teeth. Not only are such phenomena readily and more cheaply displayed on conventional radiography than on cross-sectional imaging, but also in the case of root resorption they are best visualized because of the former's better spatial resolution. Determination of such features could be adequate to assist the definitive diagnosis of those cases for which the histopathology is ambiguous.
In addition to recurrence and aggressive behaviour, the GOC has another clinically important aspect: its differential diagnosis. This differential diagnosis varies with perspective; there is the radiological diagnosis, which is largely different from its histopathological differential diagnosis.
The GOC has a high rate of recurrence, particularly in Western communities.
In addition to the most appropriate treatment, it would be valuable to determine whether there are clinical and radiological features which may suggest a particular GOC is at an increased risk of recurrence.
Acknowledgments
I wish to express my gratitude to H. Lin of the Faculty of Arts (Asian Studies), the University of British Columbia, for her assistance with the Chinese text.
Appendix 1
Glandular odontogenic cysts: excluded reports
| Selection criterion | Report (first author's surname and date of publication) | Group | Language of publication | Database |
| 2 | Gratzinger et al (2008)48 | W | English | M: Me.</emph>T1 |
| 2 | Lu et al (2007)49 | E | Chinese | M: Me |
| 2 | Velez (2006)50 | W | English | M: Me.</emph>T1 |
| 1 | Takeda et al (2005)51 | E | English | M: Me.</emph>T1 |
| A | Manor et al (2003)31 | W | English | M: Me.</emph>T1 |
| 2 | Koppang et al (1998)42 | W | English | M: Me.</emph>T1,</emph>T2 |
| 1 | High et al (1996)52 | E | English | M: Me.</emph>T1,</emph>T2 |
| A | Wang et al (1994)53 | E | Chinese | M: Me.</emph>T1 |
| 2 | van Heerden et al (1992)54 | A | English | M: Me.</emph>T1 |
| 2 | Gardner et al (1988)4 | W | English | M: Me.</emph>T1 |
| 2 | Padayachee and Van Wyk (1987)35 | A | English | M: Me.</emph>T2 |
A, sub-Saharan Africa; E, East Asia; W, Western/Caucasian. Database: M, MEDLINE; Me, MeSH, T1, text-word (glandular odontogenic cyst); T2, text-word (sialo-odontogenic cyst).
Two reports were excluded under “criterion 1”. The report by High and co-authors52 was based on an uncertain histopathological basis. Takeda and co-authors51 undoubtedly included GOCs, but their study had to be excluded because the exact number was neither identified by the authors nor could be distinguished by the reviewer.
Seven reports were excluded under “criterion 2”. Gardner and co-authors' report4 was derived from cases from several institutions. Gratzinger and co-authors'47 and Koppang and co-authors'42 reports were excluded for the same reason.
Two reports were excluded under “criterion A”. Wang and co-authors' report53 was superseded by two larger more detailed reports of the same Chinese community,25,26 and excluded under “criterion A”. Both larger reports were retained as they complemented each other. Manor and co-authors' report31 was superseded by the larger report by Kaplan and co-authors;24 the former31 was excluded under “criterion A”.
References
- 1.Kaplan I, Anavi Y, Hirshberg A. Glandular odontogenic cyst: a challenge in diagnosis and treatment. Oral Dis 2008;14:575–581 [DOI] [PubMed] [Google Scholar]
- 2.Shear M, Speight P. Cysts of the oral and maxillofacial regions, 4th edn. Oxford: Blackwell Publishing, 2007, pp 94–99. [Google Scholar]
- 3.Slootweg PJ. Lesions of the jaws. Histopathology. doi: 10.1111/j.1365-2559.2008.03097.x. 2009, 52: 401–418. [DOI] [PubMed] [Google Scholar]
- 4.Gardner DG, Kessler HP, Morency R, Schaffner DL. The glandular odontogenic cyst: an apparent entity. J Oral Pathol 1988;17:359–366 [DOI] [PubMed] [Google Scholar]
- 5.Kramer IRH, Pindborg JJ, Shear M. Histological typing of odontogenic tumours. In: WHO international histological classification of tumours, 2nd edn. London: Springer-Verlag, 1992, pp 38 [Google Scholar]
- 6.MacDonald-Jankowski DS. Fibrous dysplasia: a systematic review. Dentomaxillofac Radiol. doi: 10.1259/dmfr/16645318. 2009, 38: 196–215. [DOI] [PubMed] [Google Scholar]
- 7.Sackett DL, Strauss SE, Richardson WS, Rosenberg W, Haynes RB. Evidence-based medicine. How to practice and teach EBM, 2nd edn. Edinburgh: Churchill-Livingstone, 2000, pp 133–136. [Google Scholar]
- 8.MacDonald-Jankowski DS, Dozier MF. Systematic review in diagnostic radiology. Dentomaxillofac Radiol 2001;30:78–83 [DOI] [PubMed] [Google Scholar]
- 9.Bryant R, MacDonald-Jankowski DS, Kim K. Does the type of implant prosthesis affect outcomes for the completely edentulous arch? Int J Oral Maxillofac Implant 2007;22 1–31 [PubMed] [Google Scholar]
- 10.Ribeiro-Rotta RF, Lindh C, Rohlin M. Efficacy of clinical methods to assess jawbone tissue prior to and during endosseous dental implant placement: a systematic literature review. Int J Oral Maxillofac Implants 2007;22:289–300 [PubMed] [Google Scholar]
- 11.Hussain AM, Packota G, Major PW, Flores-Mir C. Role of different imaging modalities in assessment of temporomandibular joint erosions and osteophytes: a systematic review. Dentomaxillofac Radiol 2008;37:63–71 [DOI] [PubMed] [Google Scholar]
- 12.MacDonald-Jankowski DS. Focal cemento-osseous dysplasia: a systematic review. Dentomaxillofac Radiol 2008;37:350–360 [DOI] [PubMed] [Google Scholar]
- 13.United States2000census Available at: http: // www.censusscope.org\us\chart_race.html (accessed 16 February 2009) [Google Scholar]
- 14.Patron M, Colmenero C, Larrauri J. Glandular odontogenic cyst: clinicopathologic analysis of three cases. Oral Surg Oral Med Oral Pathol 1991;72:71–74 [DOI] [PubMed] [Google Scholar]
- 15.Günzl HJ, Horn H, Vesper M, Hellner D. Diagnosis and differential diagnosis of sialo-odontogenic (glandular-odontogenic) cyst [in German]. Pathologe 1993;14:346–350 [PubMed] [Google Scholar]
- 16.Kreidler JF, Raubenheimer EJ, van Heerden WF. A retrospective analysis of 367 cystic lesions of the jaw: the Ulm experience. J Craniomaxillofac Surg 1993;21:339–341 [DOI] [PubMed] [Google Scholar]
- 17.Daley TD, Wysocki GP, Pringle GA. Relative incidence of odontogenic tumors and oral and jaw cysts in a Canadian population. Oral Surg Oral Med Oral Pathol 1994;77:276–280 [DOI] [PubMed] [Google Scholar]
- 18.Hussain K, Edmondson HD, Browne RM. Glandular odontogenic cysts. Diagnosis and treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;79:593–602 [DOI] [PubMed] [Google Scholar]
- 19.Magnusson B, Göransson L, Odesjö B, Gröndahl K, Hirsch JM. Glandular odontogenic cyst. Report of seven cases. Dentomaxillofac Radiol 1997;26:26–31 [DOI] [PubMed] [Google Scholar]
- 20.Piloni MJ, Paparella ML, Keszler A. Glandular odontogenic cyst. A retrospective clinical, radiographic and histological study [English, Spanish]. Med Oral 2000;5:159–164 [PubMed] [Google Scholar]
- 21.Tosios KI, Kakarantza-Angelopoulou E, Kapranos N. Immunohistochemical study of bcl-2 protein, Ki-67 antigen and p53 protein in epithelium of glandular odontogenic cysts and dentigerous cysts. J Oral Pathol Med 2000;29:139–144 [DOI] [PubMed] [Google Scholar]
- 22.Mosqueda-Taylor A, Irigoyen-Camacho ME, Diaz-Franco MA, Torres-Tejero MA. Odontogenic cysts. Analysis of 856 cases [English, Spanish]. Med Oral 2002;7:89–96 [PubMed] [Google Scholar]
- 23.Noffke C, Raubenheimer EJ. The glandular odontogenic cyst: clinical and radiological features; review of the literature and report of nine cases. Dentomaxillofac Radiol 2002;31:333–338 [DOI] [PubMed] [Google Scholar]
- 24.Kaplan I, Gal G, Anavi Y, Manor R, Calderon S. Glandular odontogenic cyst: treatment and recurrence. J Oral Maxillofac Surg 2005;63:435–441 [DOI] [PubMed] [Google Scholar]
- 25.Shen J, Fan M, Chen X, Wang S, Wang L, Li Y. Glandular odontogenic cyst in China: report of 12 cases and immunohistochemical study. J Oral Pathol Med 2006;35:175–182 [DOI] [PubMed] [Google Scholar]
- 26.Qin XN, Li JR, Chen XM, Long X. The glandular odontogenic cyst: clinicopathologic features and treatment of 14 cases. J Oral Maxillofac Surg 2005;63:694–699 [DOI] [PubMed] [Google Scholar]
- 27.Jones AV, Craig GT, Franklin CD. Range and demographics of odontogenic cysts diagnosed in a UK population over a 30-year period. J Oral Pathol Med 2006;35:500–507 [DOI] [PubMed] [Google Scholar]
- 28.Meningaud JP, Oprean N, Pitak-Arnnop P, Bertrand JC. Odontogenic cysts: a clinical study of 695 cases. J Oral Sci 2006;48:59–62 [DOI] [PubMed] [Google Scholar]
- 29.Grossmann SM, Machado VC, Xavier GM, Moura MD, Gomez RS, Aguiar MC, et al. Demographic profile of odontogenic and selected nonodontogenic cysts in a Brazilian population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:e35–41 [DOI] [PubMed] [Google Scholar]
- 30.Ochsenius G, Escobar E, Godoy L, Peãafiel C. Odontogenic cysts: analysis of 2,944 cases in Chile. Med Oral Patol Oral Cir Bucal 2007;12:E85–91 [PubMed] [Google Scholar]
- 31.Manor R, Anavi Y, Kaplan I, Calderon S. Radiological features of glandular odontogenic cyst. Dentomaxillofac Radiol 2003;32:73–79 [DOI] [PubMed] [Google Scholar]
- 32.Gardner DG. Critique of the 1995 review by Reichart, et al. of the biologic profile of 3677 ameloblastomas. Oral Oncol 1999;35:443–449 [DOI] [PubMed] [Google Scholar]
- 33.National LibraryofMedicine(UnitedStatesGovernment) MeSH “Odontogenic cysts”. Available at: http: // www.ncbi.nlm.nih.gov\sites\entrez (accessed 16 February 2009) [Google Scholar]
- 34.National LibraryofMedicine(UnitedStatesGovernment) MeSH “Dentigerous cyst”. Available at: http: // www.ncbi.nlm.nih.gov\sites\entrez (accessed 16 February 2009) [Google Scholar]
- 35.Padayachee A, Van Wyk CW. Two cystic lesions with features of both the botryoid odontogenic cyst and the central mucoepidermoid tumour: sialo-odontogenic cyst? J Oral Pathol 1987;16:499–504 [DOI] [PubMed] [Google Scholar]
- 36.de Lange J, van denAkker HP, van denBerg H. Central giant cell granuloma of the jaw: a review of the literature with emphasis on therapy options. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:603–615 [DOI] [PubMed] [Google Scholar]
- 37.MacDonald-Jankowski DS, Yeung R, Lee KM, Li TK. Ameloblastoma in the Hong Kong Chinese. Part 2. Systematic review and radiological presentation. Dentomaxillofac Radiol 2004;33:141–151 [DOI] [PubMed] [Google Scholar]
- 38.Hisatomi M, Asaumi J, Konouchi H, Yanagi Y, Kishi K. A case of glandular odontogenic cyst associated with ameloblastoma: correlation of diagnostic imaging with histopathological features. Dentomaxillofac Radiol 2000;29:249–253 [DOI] [PubMed] [Google Scholar]
- 39.Hisatomi M, Asaumi J, Konouchi H, Shigehara H, Yanagi Y, Kishi K. MR imaging of epithelial cysts of the oral and maxillofacial region. Eur J Radiol 2003;48:178–182 [DOI] [PubMed] [Google Scholar]
- 40.Loubele M, Van Assche N, Carpentier K, Maes F, Jacobs R, van Steenberghe D, et al. Comparative localized linear accuracy of small-field cone-beam CT and multislice CT for alveolar bone measurements. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:512–518 [DOI] [PubMed] [Google Scholar]
- 41.Langland OE, Langlais RP, McDavid WD, DelBalso AM. Panoramic radiography, 2nd edn. Philadelphia: Lea & Febiger, 1989, pp 51–58. [Google Scholar]
- 42.Koppang HS, Johannessen S, Haugen LK, Haanaes HR, Solheim T, Donath K. Glandular odontogenic cyst (sialo-odontogenic cyst): report of two cases and literature review of 45 previously reported cases. J Oral Pathol Med 1998;27:455–462 [DOI] [PubMed] [Google Scholar]
- 43.World HealthOrganization Available at: http:// www.who.int\countries\zaf\en\ (accessed 16 February 2009) [Google Scholar]
- 44.World HealthOrganization Available at: http:// www.who.int\countries\gbr\en\ (accessed 16 February 2009) [Google Scholar]
- 45.World HealthOrganization Available at: http:// www.who.int\countries\arg\en\ (accessed 16 February 2009) [Google Scholar]
- 46.World HealthOrganization Available at: http:// www.who.int\countries\chn\en\ (accessed 16 February 2009) [Google Scholar]
- 47.Thor A, Warfvinge G, Fernandes R. The course of a long-standing glandular odontogenic cyst: marginal resection and reconstruction with particulated bone graft, platelet-rich plasma, and additional vertical alveolar distraction. J Oral Maxillofac Surg 2006;64:1121–1128 [DOI] [PubMed] [Google Scholar]
- 48.Gratzinger D, Salama ME, Poh CF, Rouse RV. Ameloblastoma, calcifying epithelial odontogenic tumor, and glandular odontogenic cyst show a distinctive immunophenotype with some myoepithelial antigen expression. J Oral Pathol Med 2008;37:177–184 [DOI] [PubMed] [Google Scholar]
- 49.Lu DP, Shu P, Xing RD, Tatemoto Y, Osaki T. Glandular odontogenic cyst: report of two cases with cytokeratin 18 expression [in Chinese]. Zhonghua Kou Qiang Yi Xue Za Zhi 2007;42:741–743 [PubMed] [Google Scholar]
- 50.Velez I. Glandular odontogenic cyst. Report of two cases and review of the literature. N Y State Dent J 2006;72:44–45 [PubMed] [Google Scholar]
- 51.Takeda Y, Oikawa Y, Furuya I, Satoh M, Yamamoto H. Mucous and ciliated cell metaplasia in epithelial linings of odontogenic inflammatory and developmental cysts. J Oral Sci 2005;47:77–81 [DOI] [PubMed] [Google Scholar]
- 52.High AS, Main DM, Khoo SP, Pedlar J, Hume WJ. The polymorphous odontogenic cyst. J Oral Pathol Med. 1996;25:25–31 [DOI] [PubMed] [Google Scholar]
- 53.Wang SZ, Chen XM, Li Y. Clinicopathologic analysis of glandular odontogenic cyst [in Chinese]. Zhonghua Kou Qiang Yi Xue Za Zhi 1994;29:329–331, 383 [PubMed] [Google Scholar]
- 54.van Heerden WF, Raubenheimer EJ, Turner ML. Glandular odontogenic cyst. Head Neck 1992;14:316–320 [DOI] [PubMed] [Google Scholar]