Abstract
Chronic recurrent multifocal osteomyelitis (CRMO) is an aseptic inflammatory disorder of unknown cause occurring in children and adolescents. It is characterized by multifocal bone lesions with pain and swelling recurring over months to years. Lesions usually involve the metaphyses of the long bones and involvement of the jaw is rare. The clinical presentation, radiographic appearance and histology of a case of CRMO involving the mandible in an 8-year-old girl are documented. The radiographic appearance of another three cases is also described.
Keywords: chronic recurrent multifocal osteomyelitis, mandible, children, computed tomography
Introduction
Chronic recurrent multifocal osteomyelitis (CRMO) is an uncommon aseptic inflammatory disorder. It is characterized by bone lesions with pain and swelling with periods of exacerbation and improvement in different locations over several months to years. The aetiology of the condition is unknown.1,2 It is traditionally thought to affect children and adolescents.1 The current opinion is that CRMO is the paediatric and most severe form of SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, osteitis).3,4 The disease was first described by Giedion et al in 19725 and the term chronic recurrent multifocal osteomyelitis was coined by Bjorksten et al.2 It affects females four times more than males,1 and has a median age of onset of around 9-years-old.1,6,7 The median duration of disease activity is 5 years.6,8 Lesions are most commonly found in the metaphyses of the long bones and involvement of the mandible is rare.1
This article describes the clinical presentation, radiographic appearance and histology of a case of CRMO involving the mandible in an 8-year-old girl. The radiographic appearances using CT of another three cases are also described.
Case reports
Case A
An 8-year-old girl was referred to Queensland Diagnostic Imaging for radiographic investigation of a swelling in the left mandible. Clinical examination revealed swelling of the left masseter muscle and expansion of the left ramus of the mandible. Ultrasound of the region was performed and normal muscle striation and vascularity were reported. Bulging of the surface of the ramus of the mandible was noted, suggesting the presence of bony pathology. An orthopantomograph was obtained, which demonstrated expansion of the left ramus, loss of the normal trabecular pattern with patchy radiolucencies and absence of the cortical outline of the inferior dental canal (Figure 1). A CT examination using a multislice CT scanner was performed. Marked expansion, patchy sclerosis and areas of lysis were obvious in the left ramus, extending superiorly into the coronoid process and inferiorly into the left body to the first molar. Multiple areas of cortical perforation were noted in the left ramus. The thin overlying expanded cortex formed a “bone-on-bone” appearance (Figure 2a). The inferior dental canal was visible running through the medullary sclerosis without deviation. There was swelling of the soft tissues, including the masseter, overlying the area (Figure 3). An MRI of the mandible and skull base with contrast and fat saturation sequences were performed. Thickening of the left ascending ramus and body of the mandible was noted. The affected area and overlying masseter, and to a lesser degree the medial soft tissues, were thickened and enhanced with contrast. No skull base pathology was seen. The degree of soft tissue involvement excluded fibrous dysplasia. A three-phase bone scan of the head was performed with delayed planar scans of the whole body. The blood pool scans showed very subtle increased uptake over the left hemimandible. The planar scans showed intense increased uptake within the expanded left mandible involving the posterior portion of the body, the ramus and extending up to the condyle on the left (Figure 4). Linear increased uptake was seen in the right calcaneal epiphysis and a small focus was also seen in the cuboid bone. The lack of intense increased uptake of radiopharmaceutical in the affected area on the blood pool scan ruled out aggressive tumours, fibrous dysplasia and an acute inflammatory or infectious condition. Radiographs of the right foot and right calcaneum showed sclerosis of the calcaneal epiphysis and subtle increased density of the second metatarsal with increased density and slight thickening of the cortex along the shaft. The thickened cortex also showed linear longitudinal lucencies consistent with a minor periostitis.
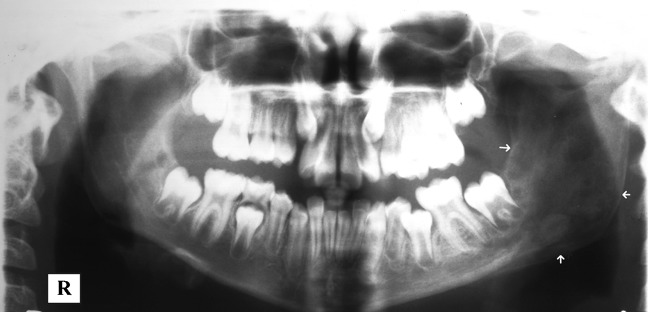
Figure 1.
Panoramic radiograph demonstrating expansion of the left ramus (arrows) and an altered trabecular pattern from Case A
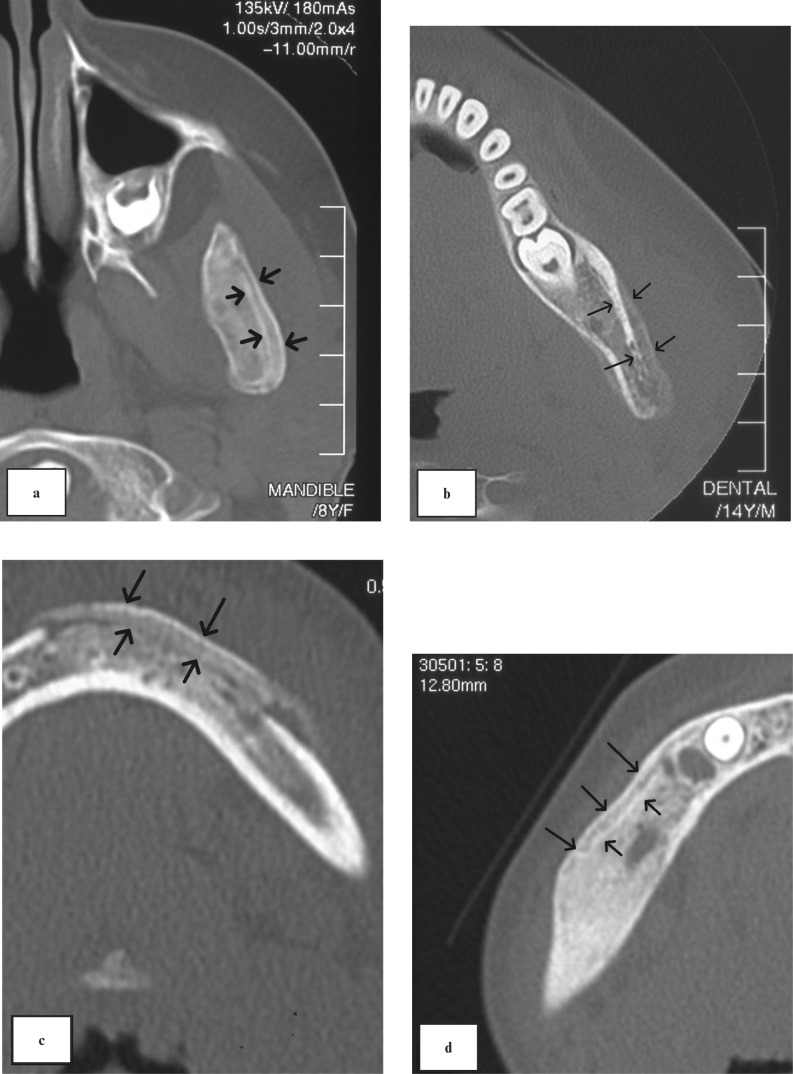
Figure 2.
Axial CT images from case A (a), case B (b), case C (c) and case D (d) all showing a “bone-on-bone” pattern (arrows)
Figure 3.
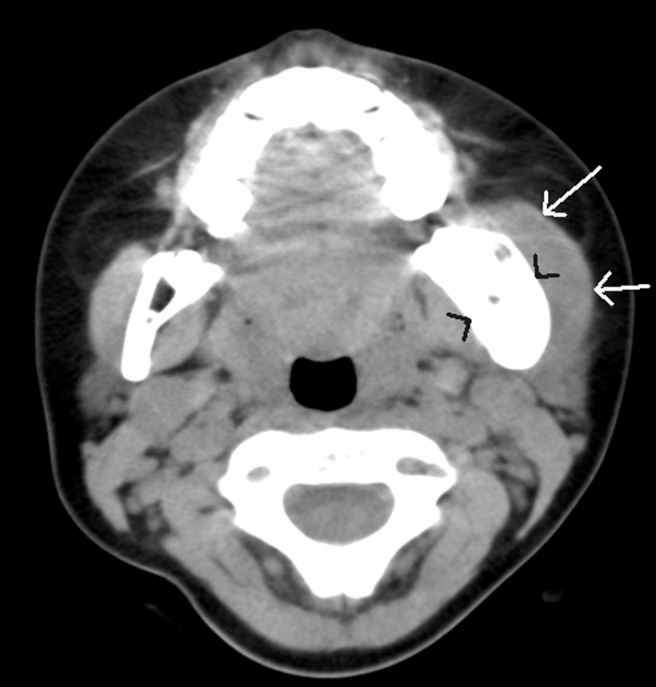
Axial CT in soft tissue window from case A. Arrows indicate swelling of the left masseter muscle. Arrow heads indicate expansion of the left ramus
Figure 4.

Planar bone scan showing uptake of radionucleotide in the left hemimandible of case A
The combination of radiographic appearance, soft tissue swelling on MRI and the bone scan appearance implied that a chronic osteomyelitic process was the likely cause. The presence of another lesion in the right foot supported the provisional diagnosis of CRMO.
Biopsies of the site were taken for diagnostic confirmation. Histopathology showed woven bone formation, some marrow oedema and mild fibrosis. There was no evidence of necrosis or inflammation nor were there any features to suggest a neoplastic process. Leukocytes were present but no bacteria were seen with Gram stain or culture. The pathologist concluded that chronic osteomyelitis was the most likely diagnosis.
Case B
Case B was a 14-year-old boy. The orthopantomogram showed an unusual appearance in the left condyle. A multislice CT examination was then performed and revealed marked expansion of the left mandibular ramus extending from the angle to the condyle and coronoid process. Erosion of the cortex and a bone-on-bone periosteal reaction were seen (Figure 2b). MRI and bone scans revealed a further lesion in the right acetabulum.
Case C
Case C was a 12-year-old girl with jaw pain and left foot pain. The orthopantomogram showed extensive sclerotic change in the anterior mandible extending from the right canine region to left first molar region. Periosteal new bone formation was noted. A multislice CT examination of the region showed increased bone density, expansion of the buccal and lingual cortical plates and a bone-on-bone appearance (Figure 2c). A bone scan confirmed further lesions in the metatarsals of the left and right feet, left acetabulum and the eighth vertebra.
Case D
Case D was a 7-year-old girl. A CT scan of the mandible showed a generalized increase in dimension and bone density of the right hemimandible extending from the right canine region to the right condyle. The cortical bone could not be distinguished from the cancellous bone and a bone-on-bone appearance was shown (Figure 2d).
Discussion
CRMO is characterized by insidious onset of pain, local bone expansion and radiological findings suggestive of osteomyelitis at multiple sites and, occurrance in children and adolescents. The disease course involves intermittent periods of exacerbation and improvement in different locations over several months to years.1,2 It can also be accompanied by fever and skin lesions.9 Palmoplantar pustulosis (PPP) is associated with CRMO in some cases, and chronic inflammatory bowel disease is also a common occurence.8
Beretta-Piccoli et al1 in a review of 260 cases found a female-to-male ratio of 4.3:1 (181:42). Median age of onset has been reported at between 9 and 10.8 years.1,6,7 The cases in the current report presented at ages 7–14. Spontaneous remission is extremely rare,6,8 and the median duration of disease activity has been reported as 5.3 years (range 2.1–10.7 years)6 and 5.6 years (range 0.5–19 years).8 However, Huber et al8 reported a small number of patients who were seemingly unresponsive to treatment and had an ongoing debilitating disease.
CRMO in children typically affects the metaphyses of the long bones, in particular the distal femoral metaphyses.1,4 Unilateral involvement is most common and bilateral involvement is rare, with only a few reported cases.10 Other sites include the clavicles and vertebrae; pelvis and ribs. Involvement of the sternum, scapula and spine are less common.1,4 Lesions involving the mandible are rare.3
Histopathology of biopsies of CRMO lesions by Girschick et al11 revealed a scattered inflammatory infiltrate, mainly of lymphocytes, plasma cells, histiocytes and neutrophil granulocytes. Immunohistochemistry shows a predominance of CD3(+), CD45RO(+) T-cells, which were mainly CD8(+). CD20(+) B cells and CD68(+) machrophages were also abundant. These findings were consistent with those of Huber et al,8 King et al9 and Suei et al.12 Reparative processes such as marrow fibrosis centrally in the lesion, apposition of osteoid on trabeculae, periosteal hyperostosis and osteosclerosis in the periphery of the lesion, as well as periosteal fibrosis were seen in all biopsies by Girschick.11 This is consistent with the histopathology reported in case A.
CRMO is uncommon in the jaws, and on panoramic radiographs may be mistaken for fibrous dysplasia, chronic diffuse sclerosing osteomyelitis or periostitis ossificans. Radiographs may show osteolysis in the early stages. Hyperostosis and sclerosis may be seen in later stages and periosteal reactions can occur at any stage.6 This is consistent with multiple sites of acute and chronic osteomyelitis.9 King et al9 also reported soft tissue swelling, which was present in case A. The radiographic features of CRMO may not always be apparent with conventional imaging and as the condition is multifocal, scintigraphy is the method of choice for assessing suspected cases of CRMO. There are several cases of bone scans detecting unknown asymptomatic lesions that were not visible on radiographs.6 The typical bone scan finding is increased uptake of the radiopharmaceutical at affected sites consistent with osteomyelitis.9
CT is commonly used to stage and follow lesions, particularly those involving the mandible as both active and quiescent disease can be seen. However, CT scanning involves high radiation exposure to young patients.13 Cone beam volumetric tomography, if available, should be considered for assessment of CRMO cases, as accurate three-dimensional information is obtained at a significantly lower dose. MRI is also a safer alternative, but appears to be less sensitive to inflammatory changes as marrow changes take months to normalize.13 MRI T1 weighted images are usually best as inflamed tissue creates low signal intensity in the normally bright signal of fat contained in the marrow. The periosteum may be thickened or of normal thickness, but shows a marked signal enhancement after intravenous contrast is administered.7 High signal intensity on T2 weighted images will be seen.1,6 These findings were consistent with the MRI appearance of case A. MRI does not show specific features capable of making a diagnosis, but does show the extent of the lesions and may be helpful in disease monitoring.1,6
In previously reported cases early mandibular lesions show changes, including diffuse and extensive resorption of the cortical and trabecular bone with cortical disruption. Sclerosis and periosteal's reaction with ossification results in bone enlargement and sequestrum formation. In chronic stages a mixed pattern of sclerotic changes and milder osteolytic changes occur.14,15 These features can be seen in all four cases. In the authors' experience, and as demonstrated in all the described cases, a bone-on-bone appearance on CT is a characteristic feature of this disease in children. This finding has not been reported previously, but was present in all the above cases.
The cause of CRMO is still unknown; although histology indicates inflammatory processes, an infectious causative agent seems unlikely.11 There are reports of bacteria being isolated from single CRMO lesions;16,17 however, it is generally concluded these single reports are due to contamination of the biopsy.9,11 No common infectious agent has been found by culture or polymerase chain reaction amplification in larger studies.2,11
Several theories of pathogenesis have been devised but none adequately explains the clinical findings. One theory is that a low-virulence micro-organism that remains undetected is responsible.9,16 However, a variety of antibacterial treatments have been tried and although there are some reports of initial improvement they are generally considered ineffective in the majority of cases.1,6 If a bacterial agent is the initial cause the inflammatory process has become independent of the agent and become a non-infectious inflammatory process.9,11 Several authors have suggested CRMO may be the result of immune deficiency. However, CRMO patients have no previous signs of immune compromise and immune response testing detected no abnormalities.2,9 Three theories of altered immune response have also been proposed. The first theory is an autoimmune response triggered by a micro-organism: a fragment from a micro-organism mimics a molecule in a bone or joint, the immune system then mistakenly attacks normal osteoarticular tissue. A similar theory is the immune complex theory: a fragment from the micro-organism couples with an immunoglobulin and is deposited in a bone or joint and activates sterile tissue. The final theory is the immune barrier breakdown hypothesis: a skin infection breaks down a barrier between immune cells and superficial skin tissues. The normal skin antigens are attacked by an immune cross-reaction causing inflammatory cascades.18–20 However, none of these theories adequately explains the pathogenesis of the disease.
Many treatment regimes have been used in the management of CRMO. Several classes and durations of antibiotics have been tried to no avail, and antibiotic therapy is no longer recommended for CRMO or SAPHO.6 Non-steroidal anti-inflammatory drugs (NSAIDS) are now the first-line therapy and are usually sufficient to manage symptoms.2,3,6,21,22
When pain is unresponsive to NSAIDs; corticosteroids, anti-tumour necrosis factor (TNF) agents and bisphosphonates have been used. The finding of increased production of TNF-α has prompted the use of TNF blocking agents with success in a small number of cases, including a patient with bilateral mandibular involvement.23 Improvement in pain and swelling have been reported with bisphosphonate treatment of CRMO,3 but the mechanism of action in CRMO is still unclear. Simm et al24 propose that the osteoclast inhibition action of bisphosphonates may act on the osteoclast-rich expansile edge of CRMO lesions and prevent expansion.4,24 Another theory is based on their anti-inflammatory properties and analgesic effects.24 Bisphosphonate-induced radiographic changes in children have been noted as dense metaphyseal bands at sites of rapid growth with cyclic administration of pamidronate.3,25 These areas are thought to be reversible.26 However, long-term safety data for use of bisphosphonates in paediatrics is lacking, and patients should be closely monitored and a regular dental review undertaken.4
The differential diagnosis for CRMO must include neoplastic diseases such as histiocytosis X or leukaemia, metastatic disease from Ewing's sarcoma or neuroblastoma. The radiographic and bone scan appearance of CRMO may mimic these pathologies,27 which must be excluded by biopsy.1 Ewing's sarcoma was included in the differential for case A, but was excluded by the presence of soft tissue swelling. Definitive diagnosis should be made by combination of the clinical presentation, radiographs, bone scan, bacterial culture and histology.11 Beretta-Piccoli et al1 advise CRMO can be diagnosed if the following criteria are filled: (i) a disease course of at least 3 months' duration, (ii) bioptical evidence of chronic bone inflammation with exclusion of other diseases and (iii) failure to cultivate an organism.
There is debate regarding whether CRMO is the same entity as SAPHO, or a paediatric form of this disease. Beretta-Piccoli et al,1 Girschick et al,11 Kahn and Chamot,28 Simm et al24 and Bjorksten and Boquist29 all support the view that CRMO is the paediatric form of SAPHO syndrome. SAPHO occurs in young to middle-aged adults. It presents with a number of the following symptoms: synovitis, acne, pustulosis, hyperostosis and osteitis; not all symptoms occur concurrently or are required for diagnosis.22,28 It mainly affects the chest wall, pelvis and spine, PPP is considered a strong diagnostic criteria.28
More than 60 cases of different skin abnormalities occurring with CRMO in children have been reported.1 As early as 1978 Bjorksten et al2 noted CRMO was associated with PPP. Van Howe et al30 reviewed 50 cases of CRMO and found 10% had PPP. Beretta-Piccoli et al1 reported eight cases of chronic skin disorders concurrent with CRMO in children. Higher incidences of classic psoriasis vulgaris, which is commonly associated with PPP have been noted.9
Furthermore, CRMO and SAPHO can affect the same sites. Traditionally CRMO is said to involve the metaphyses of long bones of the lower limbs, and SAPHO affects the chest wall, pelvis and spine. However, these sites have all been reported to have CRMO lesions in children.1,6 Job-Deslandre et al6 found 13% of cases occurred in the chest wall, 15% in the pelvis and 8% in the spine. Bjorksten and Boquist29 reported up to 23% of CRMO cases have anterior chest wall involvement. CRMO often occurs in the metaphyses of long bones in children. Diffuse sclerosing osteomyelitis (DSO) in older patients occurs less commonly in the long bones, possibly because of the disappearance of the metaphyses in adults.12 Furthermore SAPHO and CRMO lesions are histologically identical.6
Bone lesions in unifocal, multifocal, single episode and recurrent chronic non-bacterial osteomyelitis (CNO), as well as SAPHO, are histologically and radiographically similar.11,21,29 Recent articles suggest that unifocal and/or non-recurrent CNO may represent different levels of severity within the same clinical entity; CRMO being the most severe manifestation.1,31
The term DSO has been used in the literature to describe the radiographic bone changes related to chronic tendoperiostitis,32 the radiographic appearance of chronic osteomyelitis33 and a single sclerotic bone lesion of unknown aetiology,3 as well as the radiographic appearance of a bone lesion of CRMO or SAPHO.14 Several authors feel that DSO is an expression or localized form of CRMO.12,24 No difference exists between CRMO and DSO of the mandible clinically or radiographically.12 Initial diagnosis of DSO was changed to CRMO when additional lesions occurred or other non-symptomatic lesions were noted on bone scan. Suei et al12 believe that multiple bone lesions might have been found in previously reported cases of DSO if a bone scan had been carried out.
CRMO has been reported to be uncommon in the mandible, but it may be more common than thought if CNO and DSO are manifestations of the same condition. The present cases indicate that the CT findings of CRMO are very characteristic with a typical “bone-on-bone” appearance. Thus, if CT examination shows a bone-on-bone pattern, the patient should be further assessed to exclude CRMO in a young patient and SAPHO in an older patient.
References
- 1.Beretta-Piccoli BC, Sauvain MJ, Gal I, Schibler A, Saurenmann T, Kressebuch H, et al. Synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome in childhood: a report of ten cases and review of the literature. Eur J Pediatr 2000;159:594–601 [DOI] [PubMed] [Google Scholar]
- 2.Bjorksten B, Gustavson KH, Eriksson B, Lindholm A, Nordstrom S. Chronic recurrent multifocal osteomyelitis and pustulosis palmoplantaris. J Pediatr 1978;93:227–231 [DOI] [PubMed] [Google Scholar]
- 3.Compeyrot-Lacassagne S, Rosenberg AM, Babyn P, Laxer RM. Pamidronate treatment of chronic noninfectious inflammatory lesions of the mandible in children. J Rheumatol 2007;34:1585–1589 [PubMed] [Google Scholar]
- 4.Gleeson H, Wiltshire E, Briody J, Hall J, Chaitow J, Sillence D, et al. Childhood chronic recurrent multifocal osteomyelitis: Pamidronate therapy decreases pain and improves vertebral shape. J Rheumatol 2008;35:707–712 [PubMed] [Google Scholar]
- 5.Giedion A, Vischer D, Masel LF, Holthuse W. Subacute and chronic symmetrical osteomyelitis. Ann Radiol 1972;15:329–342 [PubMed] [Google Scholar]
- 6.Job-Deslandre C, Krebs S, Kahan A. Chronic recurrent multifocal osteomyelitis: Five-year outcomes in 14 pediatric cases. Joint Bone Spine 2001;68:245–251 [DOI] [PubMed] [Google Scholar]
- 7.Jurik AG, Egund N. MRI in chronic recurrent multifocal osteomyelitis. Skeletal Radiol 1997;26:230–238 [DOI] [PubMed] [Google Scholar]
- 8.Huber AM, Lam PY, Duffy CM, Yeung RSM, Ditchfield M, Laxer D, et al. Chronic recurrent multiflocal osteomyelitis: clinical outcomes after more than five years of follow-up. J Pediatr 2002;141:198–203 [DOI] [PubMed] [Google Scholar]
- 9.King SM, Laxer RM, Manson D, Gold R. Chronic recurrent multifocal osteomyelitis: a noninfectious inflammatory process. Pediatr Infect Dis J 1987;6:907–911 [DOI] [PubMed] [Google Scholar]
- 10.Buck F, Treumann T, Winiker H, Strobel K. Chronic recurrent multifocal osteomyelitis (CRMO) with symmetric involvement of both femora: x-ray, bone scintigram, and MR imaging findings in one case. J Magn Reson Imaging 2007;26:422–426 [DOI] [PubMed] [Google Scholar]
- 11.Girschick HJ, Huppertz HI, Harmsen D, Krauspe R, Muller-Hermelink K, Papadopoulos T. Chronic recurrent multifocal osteomyelitis in children: Diagnostic value of histopathology and microbial testing. Human Pathol 1999;30:59–65 [DOI] [PubMed] [Google Scholar]
- 12.Suei Y, Tanimoto K, Taguchi A, Yamada T, Yoshiga K, Ishikawa T, et al. Possible identity of diffuse sclerosing osteomyelitis and chronic recurrent multifocal osteomyelitis: one entity or two. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;80:401–408 [DOI] [PubMed] [Google Scholar]
- 13.Schuknecht B, Valavanis A. Osteomyelitis of the mandible. Neuroimaging Clin N Am 2003;13:605–618 [DOI] [PubMed] [Google Scholar]
- 14.Suei Y, Taguchi A, Tanimoto K. Diffuse sclerosing osteomyelitis of the mandible: its characteristics and possible relationship to synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome. J Oral Maxillofac Surg 1996;54:1194–1199 [DOI] [PubMed] [Google Scholar]
- 15.Suei Y, Taguchi A, Tanimoto K. Diagnostic points and possible origin of osteomyelitis in synovitis, acne, pustulosis, hyperostosis and osteitis (SAPHO) syndrome: a radiographic study of 77 mandibular osteomyelitis cases. Rheumatology 2003;42:1398–1403 [DOI] [PubMed] [Google Scholar]
- 16.Hummell DS, Anderson SJ, Wright PF, Cassell GH, Waites KB. Chronic recurrent multifocal osteomyelitis: are mycoplasmas involved. N Engl J Med 1987;317:510–511 [PubMed] [Google Scholar]
- 17.Katamura K, Okazaki S, Usami I, Tsuboyama T, Takeda N. Multifocal osteomyelitis and erythematous plaque associated with Yersinia pseudotuberculosis infection. Pediatr Int 2001;43:711–713 [DOI] [PubMed] [Google Scholar]
- 18.Laxer RM, Shore AD, Manson D, King S, Silverman ED, Wilmot DM. Chronic recurrent multifocal osteomyelitis and psoriasis: a report of a new association and review of related disorders. Semin Arthritis Rheum 1988;17:260–270 [DOI] [PubMed] [Google Scholar]
- 19.Boutin RD, Resnick D. The SAPHO syndrome: an evolving concept for unifying several idiopathic disorders of bone and skin. AJR Am J Roentgenol 1998;170:585–591 [DOI] [PubMed] [Google Scholar]
- 20.Machiels F, Seynaeve P, Lagey C, Mortelmans LL. Chronic recurrent multifocal osteomyelitis with MR-correlation: a case-report. Pediatr Radiol 1992;22:535–536 [DOI] [PubMed] [Google Scholar]
- 21.Carr AJ, Cole WG, Roberton DM, Chow CW. Chronic multifocal osteomyelitis. J Bone Joint Surg 1993;75:582–591 [DOI] [PubMed] [Google Scholar]
- 22.Hayem G, Bouchaud-Chabot A, Benali K, Roux S, Palazzo E, Silbermann-Hoffman O, et al. SAPHO syndrome: a long-term follow-up study of 120 cases. Semin Arthritis Rheum 1999;29:159–171 [DOI] [PubMed] [Google Scholar]
- 23.Deutschmann A, Mache CJ, Bodo K, Zebedin D, Ring E. Successful treatment of chronic recurrent multifocal osteomyelitis with tumor necrosis factor-alpha blockage. Pediatrics 2005;116:1231–1233 [DOI] [PubMed] [Google Scholar]
- 24.Simm PJ, Allen RC, Zacharin MR. Bisphosphonate treatment in chronic recurrent multifocal osteomyelitis. J Pediatr 2008;152:571–575 [DOI] [PubMed] [Google Scholar]
- 25.Grissom LE, Harcke HT. Radiographic features of bisphosphonate therapy in pediatric patients. Pediatr Radiol 2003;33:226–229 [DOI] [PubMed] [Google Scholar]
- 26.Land C, Rauch F, Glorieux FH. Cyclical intravenous pamidronate treatment affects metaphyseal modeling in growing patients with osteogenesis imperfecta. J Bone Mineral Res 2006;21:374–379 [DOI] [PubMed] [Google Scholar]
- 27.Kahn MF, Khan MA. The SAPHO syndrome. Baillieres Clin Rheumatol 1994;8:333–362 [DOI] [PubMed] [Google Scholar]
- 28.Kahn MF, Chamot AM. SAPHO Syndrome. Rheum Dis Clin N Am 1992;18:225–246 [PubMed] [Google Scholar]
- 29.Bjorksten B, Boquist L. Histopathological aspects of chronic recurrent multifocal osteomyelitis. J Bone Joint Surg 1980;62:376–380 [DOI] [PubMed] [Google Scholar]
- 30.Van Howe RS, Starshak RJ, Chusid MJ. Chronic, recurrent multifocal osteomyelitis: case-report and review of the literature. Clin Pediatr 1989;28:54–59 [DOI] [PubMed] [Google Scholar]
- 31.Girschick HJ, Raab P, Surbaum S, Trusen A, Kirschner S, Schneider P, et al. Chronic non-bacterial osteomyelitis in children. Ann Rheum Dis 2005;64:279–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Groot RH, Vanmerkesteyn JPR, Vansoest JJ, Bras J. Diffuse sclerosing osteomyelitis (chronic tendoperiostitis) of the mandible: an 11-year follow-up report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1992;74:557–560 [DOI] [PubMed] [Google Scholar]
- 33.White SC, Pharoah MJ. Oral radiology principles and interpretation (5th edn). St Louis, MO: Mosby, 2000 [Google Scholar]