Abstract
Objectives
The aim of this study was to investigate the correlation between disc displacement types and locations of disc perforation in the temporomandibular joint (TMJ).
Methods
157 patients (162 joints) with disc perforation observed through arthroscopy were included in this study. The types of disc displacement were analysed by TMJ MRI before operation. The locations of disc perforation under arthroscopy were recorded. The correlation between types of disc displacement and locations of disc perforation was analysed by Fisher's exact test.
Results
Medial disc perforation was observed in 55.6% of patients with anterolateral displacement without reduction, but was observed in only 3.7% of patients with pure anterior displacement, and was not observed in patients with anteromedial displacement without reduction. There was a statistically significant difference between these groups in the incidence of medial disc perforation.
Conclusions
There is a correlation between different disc displacements and locations of disc perforation. The incidence of medial disc perforation in patients with anterolateral displacement was significantly higher. The types of disc displacement may have direct influence over the locations of disc perforation.
Keywords: temporomandibular joint, magnetic resonance imaging, disc displacement, disc perforation
Introduction
Temporomandibular joint (TMJ) problems are common and affect up to one-third of all adults at some stage in their lives.1 These disorders can be of muscular origin or, less commonly, involve the joint.2 At a late stage of TMJ disorders, articular disc perforation may occur more frequently in discs that show anterior displacement without reduction than in those with reduction. The prevalence is higher in women than in men.3,4 The stage of internal derangement influences treatment planning of TMJ disorders, and evaluation for the presence or absence of disc perforation would be useful for treatment planning and for predicting the prognosis.
MRI is a non-invasive imaging technique with superior soft-tissue resolution, and it has been widely used as the gold standard for examination of TMJ disc displacement.5–8 However, its diagnostic value for assessing the presence or absence of TMJ disc perforation is limited. As a clinical modality, arthroscopic surgery has been shown to be a safe and effective technique that improves the state and function of TMJ disorder patients. During arthroscopic operation, the disc perforation and the locations of perforation can be directly observed and recorded.
The aim of this study was to investigate the correlation between disc displacement types and locations of disc perforation in TMJ.
Materials and methods
Subjects
1506 patients (1812 joints, 281 males /1225 females) who visited the TMJ clinic at the Ninth People's Hospital, Shanghai Jiao Tong University, from March 2007 to August 2008 with unilateral and/or bilateral TMJ complaints were treated by arthroscopy. 157 patients (162 joints) with disc perforation discovered during operation were asked to participate in the study. All patients had been examined by MRI before the operation. The study included 15 males and 142 females with a mean age of 32.9 ± 14.2 years. The mean duration of TMJ closed-lock before arthroscopy was 22.6 ± 12.1 months. The mean interincisal opening was 25.26 ± 7.42 mm before operation. Informed consent and ethics approval were obtained from all patients after explaining the purpose of MRI and arthroscopy. There were no contraindications for MRI and arthroscopy.
MRI examination
All scans were performed at one institution, on the same MRI scanner and using the same surface coils and scanning protocols, by a small group of highly experienced technologists. The scanner was a General Electric (Signa, General Electric, Milwaukee, WI) 1.5 T system with the “Excite” platform. Dual phased array dedicated TMJ surface coils were used. After an axial localizer image had been obtained, sagittal and coronal T1 weighted and T2 weighted images in the intercuspal position, and sagittal T1 weighted images in the open mouth position, were obtained. MRI images were taken graphically perpendicular (sagittal images) and parallel (coronal images) to the horizontal long axis of the condyle. The parameters for the sagittal and coronal images were as follows: repetition time (TR), 1820 ms; echo time (TE), 20.4 ms; number of excitations, 3; field of view, 12 cm. A slice thickness of 1 mm with a skip of 0.3 mm and a matrix of 320 × 192 pixels was used. The disc positions of the TMJ were classified according to the following MR criteria.9–11
Normal state: In the closed position, the junction of the posterior band with the retrodiscal area was located above the apex of the condylar head (12 o'clock position ±10 degrees). When the jaw opens, the disc remains interposed between the osseous components and moves anteriorly in a synchronized fashion. In the coronal plane of imaging, the disc is perfectly centred on the condylar head, without transgressing a line through the condylar poles.
Anterior disc displacement with reduction (ADDwR): In the closed position, the posterior band of the disc is anterior to the condylar head in all sagittal sections. When the jaw is opened, the disc is recaptured by the condyle and the disc condyle relation appears as normal.
Anterior disc displacement without reduction (ADDwoR): In the closed and open positions, the posterior band of the disc is anterior to the superior aspect of the condylar head in all sagittal sections. When the jaw is opened, the disc is anteriorly compressed.
Anteromedial disc displacement without reduction (AMDDwoR): There is an anterior component along with the medial displacement as determined from the corresponding sagittal imaging plane.
Anterolateral disc displacement without reduction (ALDDwoR): There is an anterior component along with the lateral displacement as determined from the corresponding sagittal imaging plane.
Arthroscopy
Arthroscopy was performed by the same specialist and assistants. A 2.4 mm arthroscope (Stryker, San Jose, CA) with a 2.7 mm outer protective cannula was used for arthroscopy of the superior joint space of the TMJ. Patients were under local anaesthesia during the examination and treatment. After upper joint distension was achieved with 2–3 ml of 2% lidocaine, a 3 mm incision was made on the skin about 1 cm prior to the tragus, and the space was entered with a 2.4 mm diameter sharp trocar protected by a 2.7 mm outer cannula. Once the capsule was entered (the surgeon confirmed the entry by the presence of fluid return in the cannula), a blunt obturator was used to replace the sharp trocar. The obturator allowed further confirmation of correct placement and gentle palpation of the fibrocartilage. Next, a 2.4 mm arthroscope was inserted, and an initial diagnostic sweep from posterior synovial pouch to anterior synovial pouch was performed. Capsular distension and intermittent lavage with Ringer lactate irrigation were maintained through an open irrigation system. In the upper compartment, the examined structures included the posterior attachment of the disc; the disc adhesions; the fibrocartilage of the glenoid fossa; and the synovium, except for the disc perforation. With the diagnosis of disc perforation of the TMJ being made, treatment can be accomplished at the same time. After the operation, the location and degree of perforation were recorded, with the disc being divided into nine parts (Figure 1) by the assistant according to their coincident opinions.12 If disc perforation was observed in more than one part, only the centre of the disc perforation was recorded.
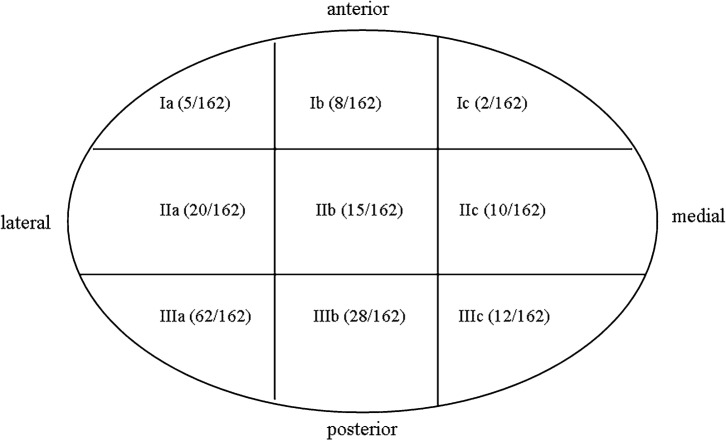
Figure 1.
Disc perforation location in different parts, with the disc being divided into nine parts under arthroscopy
Statistical analysis
The collected data were processed with SPSS 11.0 software. Fisher's exact test was used for statistical analysis of the relationship between disc displacement types and disc perforation locations.
Results
Of the 157 patients (162 joints) with disc perforation, disc displacement was observed in every joint. MRI showed ADDwR (Figure 2) in 12 joints (7.4%), ADDwoR (Figure 3) in 97 joints (59.9%), ALDDwoR (Figure 4) in 36 joints (22.2%) and AMDDwoR (Figure 5) in 17 joints (10.5%). 87 joints (53.7%) were observed to have disc perforation in the lateral part of the articular disc. 102 joints (63.0%) were observed to have disc perforation in the bilaminar zone (Figure 1).
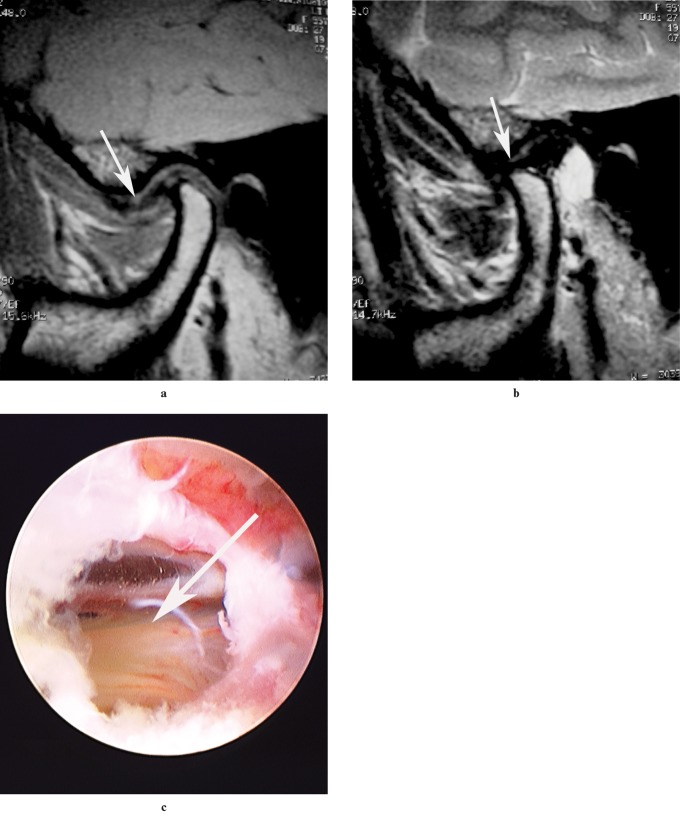
Figure 2.
MRI of a patient (27-year-old woman) with disc perforation, which was confirmed on arthroscopy of the TMJ. (a) Sagittal T1 weighted image in closed-mouth position in the left temporomandibular joint (TMJ). (b) Sagittal T2 weighted image in open-mouth position revealed anterior disc displacement with reduction in the left TMJ (arrows). (c) Disc perforation was confirmed on arthroscopy of the TMJ in the lateral part of bilaminar zone (arrow) (location IIIa)
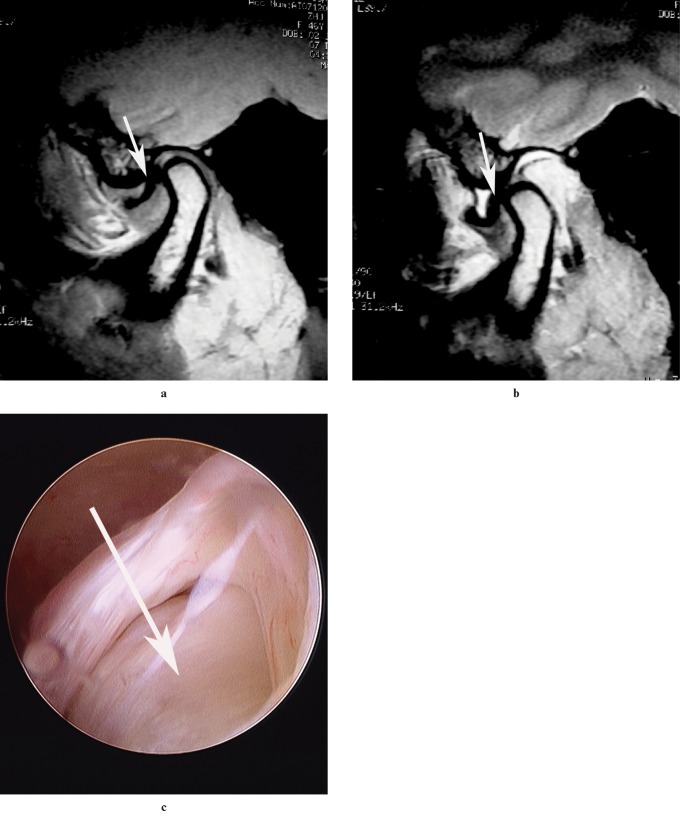
Figure 3.
MRI of a patient (34-year-old woman) with disc perforation, which was confirmed on arthroscopy of the TMJ. (a) Sagittal T1 weighted image in closed-mouth position in the left TMJ. (b) Sagittal T2 weighted image in open-mouth position revealed anterior disc displacement without reduction in the left TMJ (arrows). (c) Disc perforation was confirmed on arthroscopy of the TMJ in the lateral part of the disc (arrows) (location IIIa)
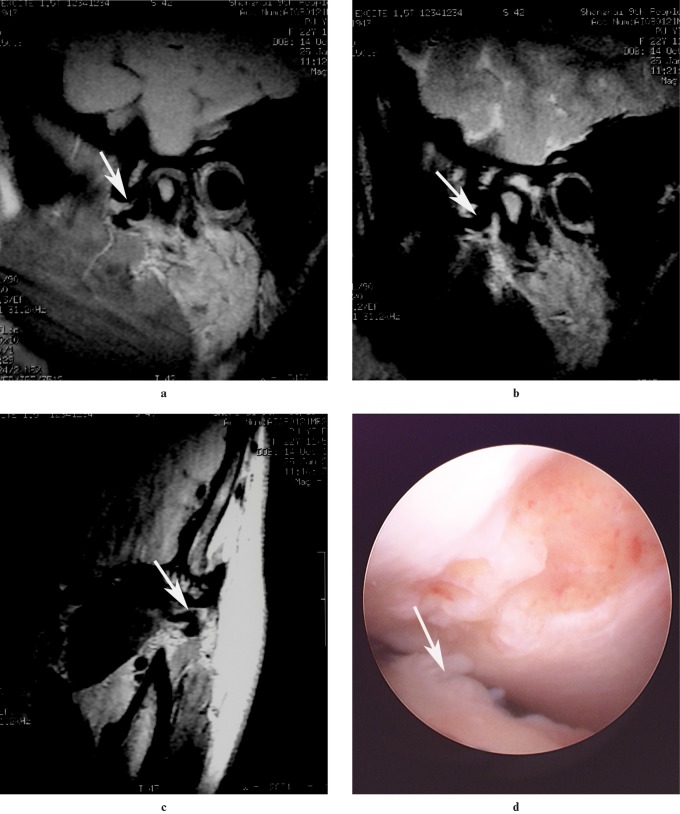
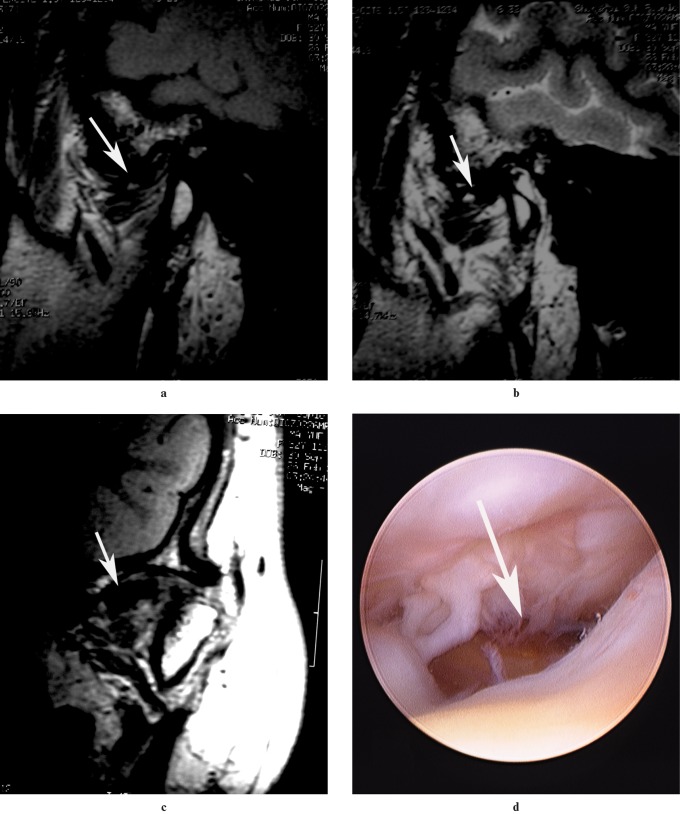
Figure 4.
MRI of a patient (24-year-old woman) with disc perforation, which was confirmed on arthroscopy of the TMJ. (a) Sagittal T1 weighted image in closed-mouth position. (b) Sagittal T1 weighted image in open-mouth position. (c) Coronal T1 weighted image in closed-mouth position revealed anterolateral disc displacement without reduction in the left TMJ (arrows). (d) Disc perforation (arrow) was confirmed on TMJ arthroscopy in the medial part of the disc (location IIIc)
Figure 5.
MRI of a patient (19-year-old woman) with disc perforation, which was confirmed on arthroscopy of the TMJ. (a) Sagittal T1 weighted image in closed-mouth position. (b) Sagittal T1 weighted image in open-mouth position. (c) Coronal T1 weighted image in closed-mouth position revealed anteromedial disc displacement without reduction in the left TMJ (arrows). (d) Disc perforation was confirmed by arthroscopy of the TMJ in the lateral part of the disc (location IIIa)
The relationship between disc perforation location and disc displacement is shown in Table 1. Medial disc perforations were observed in 55.6% patients with anterolateral displacement without reduction, but were observed in only 3.7% of patients with pure anterior displacement, and were not observed in patients with anteromedial displacement without reduction. There was a statistically significant difference between these groups in medial disc perforation incidence (Figure 6).
Table 1. The location of disc perforation in patients with different disc displacements.
| Disc displacement | Location of disc perforation |
|||
| Medial | Central | Lateral | Total | |
| ADD | 0 | 3 | 9 | 12 |
| ADDwoR | 4 | 33 | 60 | 97 |
| ALDDwoR | 20 | 11 | 5 | 36 |
| AMDDwoR | 0 | 4 | 13 | 17 |
ADD, anterior disc displacement; ADDwoR, anterior disc displacement without reduction; ALDDwoR, anterolateral disc displacement without reduction; AMDDwoR, anteromedial disc displacement without reduction
Figure 6.
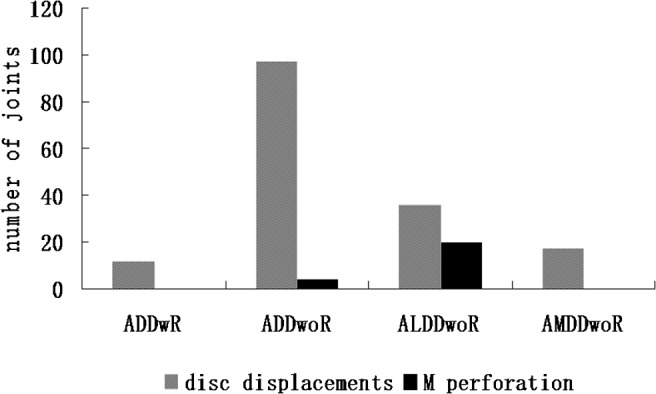
The proportion of medial disc perforations at different disc displacement types. ADDwR, anterior disc displacement with reduction; ADDwoR, anterior disc displacement without reduction; ALDDwoR, anterolateral disc displacement without reduction; AMDDwoR, anteromedial disc displacement without reduction; M perforation, disc perforation in medial part of the disc
Discussion
The most common cause of disc perforation is an abnormal relationship of the intra-articular disc to the condyle and temporal bone. MRI is a non-invasive imaging technique with superior soft-tissue resolution, and has been widely used as the gold standard for examining TMJ disc displacement. In the current study evaluated by MRI, all the cases with disc perforation also displayed disc displacement. Most cases, 92.6% (150 TMJs), were disc displacement without reduction, and the remaining 7.4% (12 TMJs) were anterior disc displacement with reduction. In addition, ALDDwoR was common, accounting for 22.2% (36 TMJs) of patients compared with 10.5% (17 TMJs) for AMDDwoR. This is in accordance with other studies evaluating different types of disc displacement.13–15 The likely cause is weakness of the lateral capsular attachment, whereas the medial capsular attachment is stronger and reinforced by the insertions of lateral pterygoid.16
Articular disc perforation in the TMJ frequently occurs near the posterolateral region of attachment of the disc to the retrodiscal tissue.17 In the current study, the majority of joints (63.0%) underwent disc perforation in the bilaminal zone. More than half of the joints (53.7%) were observed to have disc perforation in the lateral part of the articular disc. Stratmann et al18 demonstrated that there was a statistically significant gradient of decreasing disc thickness in a mediolateral axis of the middle dense part. The authors concluded that, as the disc possesses no mesenchymal cell-mediated regenerative or adaptive capacity, a gradual abrasive loss of substance cannot be compensated for and will eventually lead to a perforation of the thinnest discal region. According to the present data, perforation of the disc most frequently occurred in the bilaminal zone and the lateral part of the articular disc, but more than half the patients (55.6%) with anterolateral displacement without reduction were observed to have medial disc perforation, whereas only 3.7% with pure anterior displacement and no patients with anteromedial displacement without reduction, were observed to have medial disc perforation. This cannot be sufficiently explained by the hypothesis of Stratmann et al. The likely cause may be that the retrodiscal tissue is located at the central articulating surface following anterior disc displacement with or without reduction. The contralateral part of the retrodiscal tissue was located at the central articulating surface and endures high pressures during chewing; disc perforation formed more frequently in this area when sideways displacement occurred.
No clinical signs or symptoms were found to be specific for joints with disc perforation,19 and the diagnostic value of MRI for assessing the presence or absence of TMJ disc perforation is limited. So the diagnosis of disc perforation is difficult without an invasive technique, such as arthrography or arthroscopy. Treatment directed towards disc displacement (in some cases associated with disc perforation) under arthroscopy has been carried out for many years in the authors' TMJ clinic, but the location and size of the disc perforation were very important for the treatment. This study demonstrated that there was correlation between disc displacements and locations of disc perforation, and there may be some value for the diagnosis and treatment of disc perforation in TMJ.
In conclusion, this study shows that disc perforation commonly occurred in the bilaminar zone and the lateral part of articular disc, and patients with anterolateral displacement without reduction more frequently underwent medial disc perforation. The types of disc displacement may have direct influence over the locations of disc perforation.
Acknowledgments
This study was supported by the Science and Technology Commission of Shanghai (08DZ2271100), grant of Shanghai Leading Academic Discipline Project (Project Number S30206), grant from Shanghai Municipal Bureau of Health (Grant No. 2008160), Project of Shanghai “Phosphor” Science Foundation (Grant No. 04QMH1415), grant from the PhD Programs Foundation of Shanghai Jiao Tong University School of Medicine (No. BXJ0926). Research Fund of Medicine and Engineering of Shanghai Jiao Tong University (Grant No. YG2009MS42), a grant from the PhD Programmes Foundation of the Ministry of Education of China (Grant No. 2009007311 0068), a grant from the National Natural Science Foundation of Shanghai (Grant No. 10ZR1418200).
References
- 1.Bennett RB, Buxbaum JD. Epidemiologic studies of mandibular dysfunction: a critical review. J Prosthet Dent 1983;49:449. [DOI] [PubMed] [Google Scholar]
- 2.McNeill C, Mohl ND, Rugh JD, Tanaka TT. Temporomandibular disorders: diagnosis, management, education, and research. J Am Dent Assoc 1990;120:253–257 [DOI] [PubMed] [Google Scholar]
- 3.Widmalm SE, Westesson PL, Kim IK, Pereira FJ, Jr, Lundh H, Tasaki MM. Temporomandibular joint pathosis related to sex, age, and dentition in autopsy material. Oral Surg Oral Med Oral Pathol 1994;78:416–425 [DOI] [PubMed] [Google Scholar]
- 4.Kondoh T, Westesson PL, Takahashi T, Seto K. Prevalence of morphological changes in the surfaces of the temporomandibular joint disc associated with internal derangement. J Oral Maxillofac Surg 1998;56:339–344 [DOI] [PubMed] [Google Scholar]
- 5.Sano T, Westesson PL. Magnetic resonance imaging of the temporomandibular joint. Increased T2 signal in the retrodiskal tissue of painful joints. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;79:511–516 [DOI] [PubMed] [Google Scholar]
- 6.Westesson PL, Katzberg RW, Tallents RH, Sanchez-Woodworth RE, Svensson SA. CT and MR of the temporomandibular joint: comparison with autopsy specimens. AJR Am J Roentgenol 1987;148:1165–1171 [DOI] [PubMed] [Google Scholar]
- 7.Westesson PL, Katzberg RW, Tallents RH, Sanchez-Woodworth RE, Svensson SA, Espeland MA. Temporomandibular joint: comparison of MR images with cryosectional anatomy. Radiology 1987;164:59–64 [DOI] [PubMed] [Google Scholar]
- 8.Limchaichana N, Petersson A, Rohlin M. The efficacy of magnetic resonance imaging in the diagnosis of degenerative and inflammatory temporomandibular joint disorders: a systematic literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:521–536 [DOI] [PubMed] [Google Scholar]
- 9.Katzberg RW. Temporomandibular joint imaging. Radiology 1989;170:297–307 [DOI] [PubMed] [Google Scholar]
- 10.Drace JE, Enzmann DR. Defining the normal temporomandibular joint: closed-, partially open-, and open-mouth MR imaging of asymptomatic subjects. Radiology 1990;177:67–71 [DOI] [PubMed] [Google Scholar]
- 11.Zhang S, Yang C, Chen M, Fan X, Yun B, Peng Y, Yuan D. doi: 10.1016/j.bjoms.2008.09.007. Magnetic resonance imaging in the diagnosis of intra-articular adhesions of the temporomandibular joint. Br J Oral Maxillofac Surg 2009; 47: 389–392. [DOI] [PubMed] [Google Scholar]
- 12.Yang C, Zhang SY, Wang XD, Fan XD. Magnetic resonance arthrography applied to the diagnosis of intraarticular adhesions of the temporomandibular joint. Int J Oral Maxillofac Surg 2005;34:733–738 [DOI] [PubMed] [Google Scholar]
- 13.Foucart JM, Carpentier P, Pajoni D, Marguelles-Bonnet R, Pharaboz C. MR of 732 TMJs: anterior, rotational, partial and sideways disc displacements. Eur J Radiol 1998;28:86–94 [DOI] [PubMed] [Google Scholar]
- 14.Tasaki MM, Westesson PL, Isberg AM, Ren YF, Tallents RH. Classification and prevalence of temporomandibular joint disk displacement in patients and symptom-free volunteers. Am J Orthod Dentofac Orthop 1996;109:249–262 [DOI] [PubMed] [Google Scholar]
- 15.Whyte AM, McNamara D, Rosenberg I, Whyte AW. Magnetic resonance imaging in the evaluation of temporomandibular joint disc displacement-a review of 144 cases. Int J Oral Maxillofac Surg 2006;35:696–703 [DOI] [PubMed] [Google Scholar]
- 16.Tanne K, Tanaka E, Sakuda M. The elastic modulus of the temporomandibular joint disc from adult dogs. J Dent Res 1991;70:1545–1548 [DOI] [PubMed] [Google Scholar]
- 17.Holmlund A, Hellsing G. Arthroscopy of the temporomandibular joint. A comparative study of arthroscopic and tomographic findings. Int J Oral Maxillofac Surg 1988;17:128–133 [DOI] [PubMed] [Google Scholar]
- 18.Stratmann U, Schaarschmidt K, Santamaria P. Morphometric investigation of condylar cartilage and disc thickness in the human temporomandibular joint: significance for the definition of osteoarthrotic changes. J Oral Pathol Med 1996;25:200–205 [DOI] [PubMed] [Google Scholar]
- 19.Cholitgul W, Petersson A, Rohlin M, Akerman S. Clinical and radiological findings in temporomandibular joints with disc perforation. Int J Oral Maxillofac Surg. 1990;19:220–225 [DOI] [PubMed] [Google Scholar]