Abstract
Objectives
For surgical procedures involving the posterior mandible, it is important to be familiar with the details of the bifid mandibular canal. To our knowledge, there have been no systematic studies evaluating the bifid mandibular canal using sectional imaging. The purpose of this study is to evaluate the incidence and configuration of the bifid mandibular canal using cone beam CT.
Methods
252 patients (301 mandible sides) underwent cone beam CT between October 2004 and September 2005 and were included in this study. The cone beam CT images were evaluated for the presence and configuration of the bifid mandibular canal. The patterns of bifurcation were classified into four types according to the classification of Nortjé et al (Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg 1977; 15: 55–63). The diameter of the accessory canal was classified into two categories: 50% or more and less than 50% of the diameter of the main mandibular canal.
Results
Of the 301 subjects, 47 (15.6%) demonstrated a bifid mandibular canal. They were Type I in 2, Type II in 40, Type III in 0, and Type IV in 5 cases. The diameter of the accessory canal was greater than or equal to 50% of the main canal in 23, and less than 50% in 24 cases.
Conclusions
On the basis of the cone beam CT, a bifid mandibular canal was found in 15.6% of cases, a markedly higher proportion than found in previous reports using panoramic images. Cone beam CT is considered a suitable modality for detailed evaluation of bifid mandibular canals.
Keywords: cone beam computed tomography, bifid mandibular canal, panoramic radiography
Introduction
The mandibular canal runs from the mandibular foramen to the mental foramen and contains the inferior alveolar artery, vein and nerve. Its anatomical location and configuration have been studied by several researchers. Carter and Keen1 classified the intramandibular course of the inferior alveolar nerve into three types on the basis of their anatomical study: Type I, the inferior alveolar nerve is a single large structure lying in a bony canal; Type II, the nerve is situated substantially lower down the mandible; and Type III, the inferior alveolar nerve separates posteriorly into two large branches. Type III is considered to correspond to the bifid mandibular canal.
For surgical procedures involving the posterior mandible it is important to be familiar with details of the bifid mandibular canal. There have been many radiological studies that have evaluated panoramic images and reported the incidence of the bifid mandibular canal. In these studies, the incidence has varied widely, ranging from 0.08% to 8.3%. Recently, sectional imaging including CT and cone beam CT has been widely used in the field of dentistry. These methods provide high-resolution three-dimensional images which are considered to be superior to panoramic images for detailed evaluation of mandibular canals. To our knowledge, there have been no systematic studies that have evaluated the bifid mandibular canal using these modalities.
The purpose of this study was to investigate the incidence and configuration of the bifid mandibular canal on the basis of cone beam CT images.
Materials and methods
The study was approved by our institutional review board, and written informed consent was obtained from all participants.
Patients
252 patients (301 mandible sides) who consulted our dental hospital for extraction of impacted mandibular third molars and underwent both panoramic radiography and cone beam CT examination between October 2004 and September 2005 were included in this study. The patients consisted of 158 women and 94 men, with a mean age of 33 years (range 18–74).
Imaging
A cone beam CT apparatus, the 3DX multi-image micro CT (Morita, Kyoto, Japan), which was developed by Arai et al,2 was used with the following parameters: a tube voltage of 80 kV, a tube current of 2 mA and an exposure cycle of 17 s. The imaging area of the 3DX is a cylinder with a height of 30 mm (240 voxels) and a diameter of 40 mm (320 voxels), providing isotropic cubic voxels with sides of approximately 0.125 mm.
Contiguous sectional images in three directions, parallel section (parallel to the dental arch), cross-section (perpendicular to the dental arch) and horizontal section images, were reconstructed from the projection data with a slice width of 1 mm. Viewing the contiguous sectional images using dedicated 3DX software, the observers evaluated the images in each section on a cathode ray tube (CRT) monitor. When necessary, the window setting was adjusted to optimize the images for evaluation.
Evaluation of images
Two oral radiologists (AK, HW) twice independently evaluated the cone beam CT images for the presence or absence of the bifid mandibular canal. When present, the configuration and diameter of the accessory canal were also evaluated. The diameter of the mandibular canal was measured using dedicated 3DX software. The diameter of the accessory canal was classified into two categories: greater than or equal to 50% or less than 50% of the diameter of the main mandibular canal. The patterns of bifurcation were classified into four types according to the classification of Nortjé et al3 (Table 1). When disagreement existed between the two observers, consensus was reached by discussion.
Table 1. Types of bifid mandibular canal according to the classification of Nortjé et al3.
| Type I | Two canals originating from one foramen |
| Type II | A short supplemental upper canal extending to the second molar or third molar teeth |
| Type III | Two mandibular canals of equal dimension apparently arising from separate foramina in the mandibular ramus and joining together to form one canal in the molar region |
| Type IV | A supplemental canal arising in the retromolar pad region and joining with the main canals in the retromolar area |
Results
Of the 301 subjects, 47 (15.6%) demonstrated a bifid mandibular canal (16 men and 31 women). As shown in Table 2, the patterns of the 47 bifid mandibular canals were as follows: Type I in 2 (0.7%), Type II in 40 (13.2%), Type III in 0 (0%) and Type IV in 5 (1.7%) cases. The diameter of the accessory canal was greater than or equal to 50% of the main canal in 23 (49%) and less than 50% in 24 (51%) cases. The mean diameter of the bifid mandibular canal was 1.68 mm (range 0.88–3.40 mm), and that of the mandibular canal was 3.28 mm (range 2.02–4.63 mm).
Table 2. The occurrence of bifid mandibular canals in 301 mandible sides.
| Type | Diameter of the accessory canal |
|||
| Narrow | Wide | Total | % | |
| Type I | 0 | 2 | 2 | 0.7 |
| Type II | 21 | 19 | 40 | 13.2 |
| Type III | 0 | 0 | 0 | 0 |
| Type IV | 3 | 2 | 5 | 1.7 |
| Total | 24 | 23 | 47 | 15.6 |
Narrow, diameter less than 50% of that of the main mandibular canal; wide, diameter 50% or more of that of the main mandibular canal
Percentages are given relative to the total number of all subjects (301 mandible sides)
Representative images are shown in Figures 1–3.
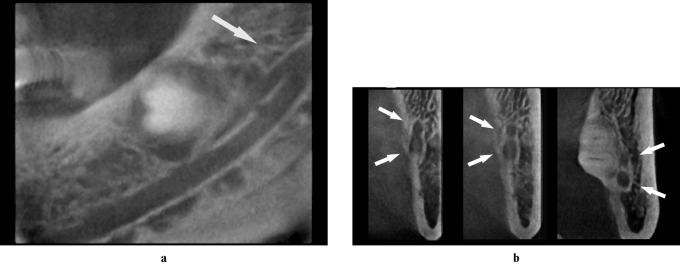
Figure 1.
(a and b) Cone-beam CT images of the left mandible (male, 54 years). The cone-beam CT images clearly reveal a narrow upper canal originating from a foramen (Type I, arrows)
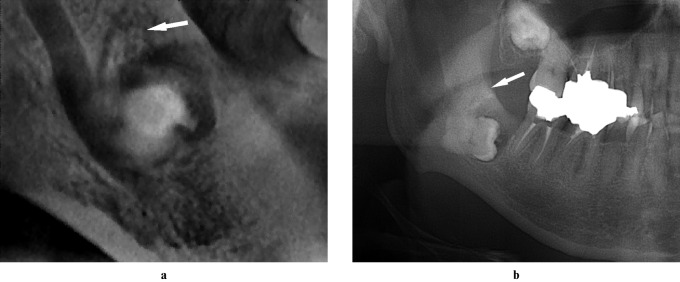
Figure 3.
(a) Cone beam CT image of the right mandible. (b) Panoramic image. The cone beam CT image (a) clearly reveals an accessory canal that arose in the retromolar pad lesion and joined the main canal in the retromolar area (Type IV, arrow). The accessory canal is not seen on (b) (arrow)
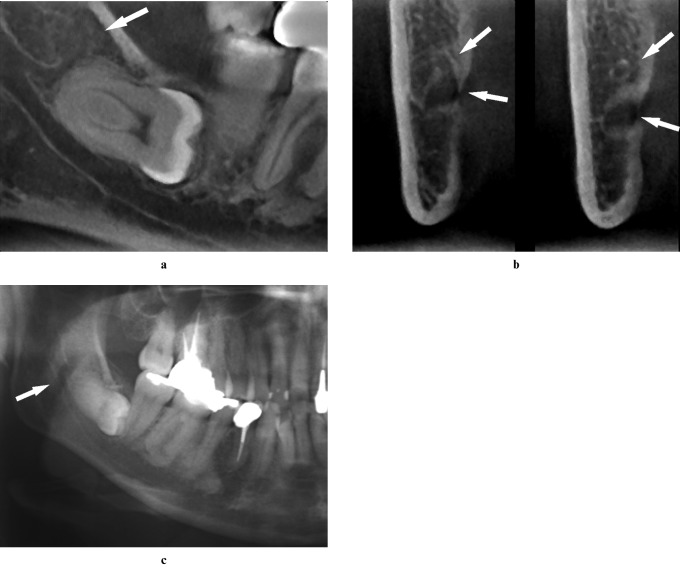
Figure 2.
(a and b) Cone beam CT images of the right mandible (male, 52 years). (c) Panoramic image. The cone beam CT images (a and b) clearly reveal a short bifid mandibular canal extending to the third molar area (Type II, arrows), which is not seen on (c) (arrow)
Discussion
There have been several studies that have evaluated the anatomical location and configuration of the bifid mandibular canal using panoramic images. Among them, Nortjé et al3 reported the incidence of bifid mandibular canals as 0.9% (33/3612), whereas Durst and Snow4 reported an incidence of 8.3% (85/1024). Reported incidences by other researchers include 0.08% (4/5000),5 0.95% (57/6000),6 0.4% (3/700)7 and 0.35% (7/2012);8 it can be seen therefore the bifid mandibular canal incidences reported in radiological studies to date vary widely (0.08–8.3%), and no consensus has been reached. We consider that the true incidence may be much higher since panoramic images are not sufficient to detect all bifid canals. Klinge et al9 reported in their study using cadavers that panoramic images failed to show the mandibular canal in 36.1% of specimens. Bogdán et al10 performed a comparative examination of dry mandibles and panoramic images. According to their study, the bifid mandibular canal was visible in only 0.2% the latter, whereas it was visible in 19.6% of the former. These studies suggest that the incidence of the bifid mandibular canal is underestimated when using panoramic images.
Using cone beam CT, we found that 47 (15.6%) of the 301 subjects had a bifid mandibular canal. In other words, the incidence in our study was much higher than that in a previous study using panoramic images and was relatively consistent with the above-mentioned anatomical study using dry mandibles.10
The cone beam CT was able to detect narrow canals that may not have been detected by panoramic images. The diameter of the bifid mandibular canal was less than half of that of the main mandibular canal in 24 out of 47 cases (51%). Cone beam CT was able to detect canals with diameters of only 0.88 mm. Furthermore, it was able to easily detect canals that bifurcated in the buccal or lingual directions, which might not have been possible using two-dimensional images as in panoramic radiography.
According to the classification by Nortjé et al,3 the patterns of the 47 bifid mandibular canals were as follows: Type I in 2 (0.7%), Type II in 40 (13.2%), Type III in 0 (0%) and Type IV in 5 (1.7%) cases. Thus, Type II was the most commonly found and constituted 85% of all bifid canals.
This result was inconsistent with that obtained by Nortjé et al. They reported that among 33 bifid mandibular canals found in panoramic radiographs, 26 were Type I and only 5 were Type II.3,11 Type II bifid mandibular canals mostly extend to the distal area of the third molar teeth, which are often obscured by the shadow of the soft palate on panoramic images. This explains the difficulty in detecting Type II bifid mandibular canals on panoramic images.
On the other hand, some anatomical structures may form thin cortical outlines on panoramic images that mimic the bifid mandibular canal. Such cortical outlines may be due to the imprint of the mylohyoid nerve on the internal mandibular surface where it separates from the inferior alveolar nerve and runs to the floor of the mouth.8,12 Auluck et al12 reported that the cortical outlines surrounding the different canals may join to form a triangular island of bone, with its vertex at the root of the separation of the bifid canals, which is a characteristic feature that indicates the presence of a bifid mandibular canal. Cone beam CT is considered more useful for distinguishing true from false bifid mandibular canals than panoramic images. Rouas et al13 reported a case involving panoramic findings of a bilateral enlarged mandibular canal, which subsequently turned out to be a deep mylohyoid groove by cone beam CT.
For surgical procedures involving the posterior mandible, it is important to be familiar with the incidence and configuration of the bifid mandibular canal because during a lower third molar extraction, complications, including unexpected bleeding, paraesthesia and traumatic neuroma, may occur due to damage to the accessory canal. Furthermore, the presence of an accessory canal can result in inadequate anaesthesia. Lew et al14 reported a case in which the presence of an accessory canal resulted in inadequate anaesthesia at the time of inferior alveolar nerve block.
Although panoramic radiographs are routinely used for pre-operative assessment of such surgical procedures, they have limitations when used to evaluate the presence and configuration of bifid mandibular canals. In this study, we evaluated cone beam CT and were able to detect many bifid mandibular canals, including Type II and those with a narrow diameter, which are considered to be undetectable by panoramic radiographs. Thus, we recommend cone beam CT as a technique for detailed pre-operative evaluation of the bifid mandibular canal.
In conclusion, bifid mandibular canal was found in 15.6% of our series, and 85% of those were classified as Type II, i.e. short upper canals extending to the second molar or third molar teeth. The incidence in our study (15.6%) was markedly higher than that of previous reports using panoramic images.
Since cone beam CT can provide high-resolution three-dimensional images, it can detect accessory canals with a narrow diameter and those that bifurcate in any direction. Furthermore, it can correctly differentiate true from false mandibular canals. Cone beam CT was considered a suitable modality for detailed evaluation of the presence and configuration of bifid mandibular canals.
References
- 1.Carter RB, Keen EN. The intramandibular course of the inferior alveolar nerve. J Anat 1971;108:433–440 [PMC free article] [PubMed] [Google Scholar]
- 2.Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol 1999;28:245–248 [DOI] [PubMed] [Google Scholar]
- 3.Nortjé CJ, Farman AG, Grotepass FW. Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg 1977;15:55–63 [DOI] [PubMed] [Google Scholar]
- 4.Durst JH, Snow JE. Multiple mandibular canals: oddities or fairly common anomalies? Oral Surg Oral Med Oral Pathol 1980;49:272–273 [DOI] [PubMed] [Google Scholar]
- 5.Grover PS, Lorton L. Bifid mandibular nerve as a possible cause of inadequate anaesthesia in the mandible. J Oral Maxillofac Surg 1983;41:177–179 [DOI] [PubMed] [Google Scholar]
- 6.Langlais RP, Broadus R, Glass BJ. Bifid mandibular canals in panoramic radiographs. J Am Dent Assoc 1985;110:923–926 [DOI] [PubMed] [Google Scholar]
- 7.Zografos J, Kolokoudias M, Papadakis E. The types of mandibular canal. Hell Period Stomat Gnathopathoprosopike Cheir 1990;5:17–20 [PubMed] [Google Scholar]
- 8.Sanchis JM, Peãarrocha M, Soler F. Bifid mandibular canal. J Oral Maxillofac Surg 2003;61:422–424 [DOI] [PubMed] [Google Scholar]
- 9.Klinge B, Petersson A, Maly P. Location of the mandibular canal: comparison of macroscopic findings, conventional radiography, and computed tomography. Int J Oral Maxillofac Implants 1989;4:327–332 [PubMed] [Google Scholar]
- 10.Bogdán S, Pataky L, Barabás J, Németh Z, Huszár T, Szabó G. Atypical courses of the mandibular canal: comparative examination of dry mandibles and x-rays. J Craniofac Surg 2006;17:487–491 [DOI] [PubMed] [Google Scholar]
- 11.Nortjé CJ, Farman AG, De V., Joubert JJ The radiographic appearance of the inferior dental canal: an additional variation. Br J Oral Surg 1977;15:171–172 [DOI] [PubMed] [Google Scholar]
- 12.Auluck A, Pai KM, Shetty C. Pseudo bifid mandibular canal. Dentomaxillofac Radiol 2005;34:387–388 (letter). [DOI] [PubMed] [Google Scholar]
- 13.Rouas P, Delbos Y, Nancy J. Pseudo multiple and enlarged mandibular canals: the evidence-based response of cone beam computed tomography. Dentomaxillofac Radiol 2006;35:217–218 (letter). [DOI] [PubMed] [Google Scholar]
- 14.Lew K, Townsen G. Failure to obtain adequate anaesthesia associated with a bifid mandibular canal: a case report. Aust Dent J 2006;51:86–90 [DOI] [PubMed] [Google Scholar]