Abstract
This report presents the imaging appearances of an uncommon case of intradiploic frontal bone aneurysmal bone cyst (ABC) in a 10-year-old girl. ABCs are rare in the calvarium. The radiological and aetiopathological differences between the more commonly occurring ABCs of the long bones and vertebrae, and their rarer counterparts in the calvarium and facial bones, have been discussed. Unique also to this case is the reconstruction performed using the outer table of the bone flap after excising the tumour.
Keywords: aneurysmal bone cyst, frontal bone
Introduction
Aneurysmal bone cysts (ABCs) occur uncommonly in bones of the calvarium. In most such cases, they occur as a secondary phenomenon in pre-existing fibrous dysplasia. We present the imaging features and pathology of a rare case of a primary ABC of the frontal bone, with no underlying bony abnormality. After excision of the tumour, the reconstructive surgery performed in this case using the outer table of the bone is a novel approach to treatment.
Case report
A 10-year-old girl presented to the neurosurgery department complaining of a painful and rapidly increasing swelling in the right side of the forehead that began 1 year previously. On examination of the area, a bulge with ill-defined edges was felt. There was oedema of the right periorbital region and she had no neurodeficit.
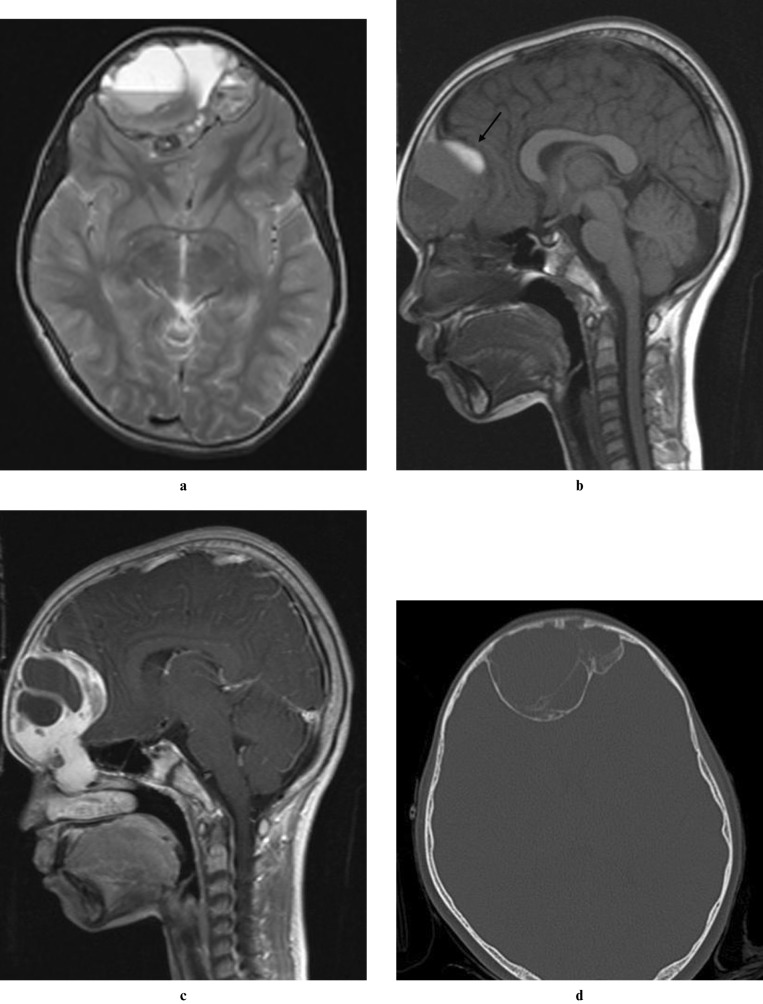
An MRI of the brain was performed, which showed a large mass arising from the frontal bone. The lesion extended into the right anterior and middle ethmoid air cells. No intra-axial extension was present. The soft-tissue mass contained haemorrhage and multiple fluid–fluid levels, which were best observed on T2 weighted (Figure 1a) and susceptibility images. On T1 weighted images, subacute blood products were seen in the lesion as areas of T1 hyperintensity (Figure 1b). The solid periphery of the tumour displayed intense enhancement, whereas the central cystic components did not enhance (Figure 1c). Frontal and lateral radiographs of the skull and a CT study of the brain was performed with the intention of demonstrating the bone details. Radiographs of the skull and CT brain showed an expansile osteolytic lesion of the right frontal bone. CT confirmed that the mass was intradiploic (Figure 1d). An initial radiological diagnosis of ABC was made.
Figure 1.
(a) T2 weighted axial image shows an intradiploic lesion in the frontal bone with multiple fluid–fluid levels. (b) Sagittal T1 weighted MR image shows subacute blood products (arrow) in the superior aspect of the lesion. (c) On the post-contrast T1 weighted sagittal image, there is intense enhancement of the peripheral solid component of the tumour. The central cystic components do not enhance. (d) Axial CT image (bone window) confirms that the lesion is intradiploic
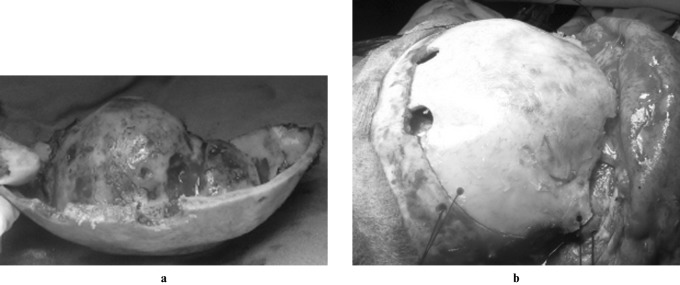
The patient underwent surgery under general anaesthesia. A bifrontal craniotomy was performed with a significant margin around the expanded bony mass, which included the superior margin and roof of both orbits. The bone flap raised, therefore, included the entire tumour mass (Figure 2a), except for a small residue in the ethmoid air cells. The portion extending into the ethmoid sinuses was microscopically excised separately. The tumour was dissected off the outer layer of the bone, which was preserved to provide a cosmetic bony closure. A vascularized pericranial flap was placed over the orbit and the opened ethmoidal air cells. The reconstructed outer shell of the bone flap was anchored (Figure 2b) and the wound was closed in layers. The immediate post-operative period was uneventful. Post-operative MRI and CT scans showed complete excision of the lesion.
Figure 2.
(a) Bifrontal, free bone flap with the tumour involving the inner table, along with the superior margin and roof of both orbits. (b) Reconstruction using the outer shell of the bone flap after excising the tumour mass
On pathological gross examination of the lesion, the cyst wall was smooth. Microscopic examination revealed cystic spaces filled with blood. The cystic spaces did not have an endothelial lining and were surrounded by solid and cellular tissue fragments showing a variable admixture of cells resembling fibroblasts, plump spindloid cells, histiocytic cells and numerous osteoclastic giant cells, along with foci of haemorrhage and congested blood vessels (Figure 3). Also seen were trabeculae of woven bone (osteoid) with focal mineralization. At the periphery, there was sclerosed host bone along with tissue resembling callus. In some fragments, there was uniform distribution of osteoclastic giant cells with 2–30 nuclei. There was no nuclear atypia, mitosis or necrosis. The final diagnosis was ABC.
Figure 3.
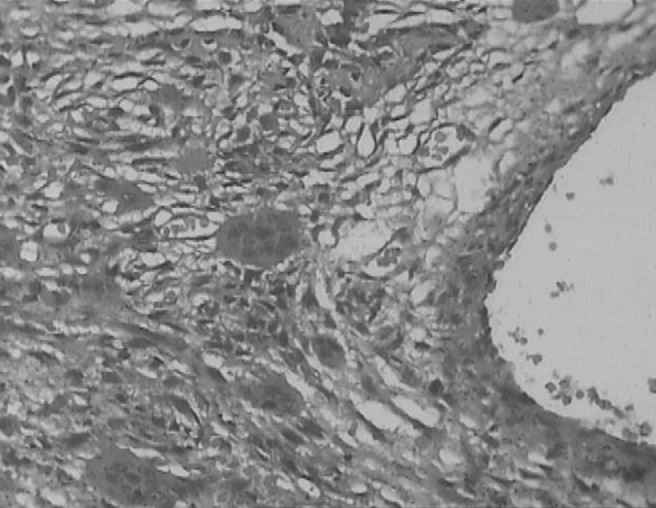
A cystic space filled with red blood cells and surrounded by fibrous stroma, rich in osteoclastic giant cells (haematoxylin and eosin, ×100)
Discussion
An interesting theory about the aetiology of primary ABCs is that the lesions occur because of haemorrhage in the bone as a result of increased venous pressure. The haemorrhage is thought to lead to osteolysis. The osteolysis, in turn, causes further haemorrhage, leading to exponential growth of the tumour. This theory would perhaps explain why ABCs are uncommon in the calvarium and bones of the facial skeleton, where the venous pressure is low. On the other hand, ABCs are common in long bones, where the venous pressure is high and the marrow content is greater.1
Conventional thinking; however, ascribes these lesions either to a reaction to physical injury, which may sometimes be remote, or to a vascular disturbance. ABCs also arise secondarily in a host of other primary bone lesions, such as giant cell tumours (GCTs), fibrous dysplasia, non-ossifying fibromas, haemangiomas, osteoblastomas, simple bone cysts, chondroblastomas, chondromyxoid fibromas and even osteosarcomas.2 They are also known to develop in fractures. Thus, it is often thought that the ABC is more of a pathophysiological change in a pre-existing primary bone lesion rather than a single, unique entity.3
The most common imaging appearance of an ABC is that of an eccentric, expansile osteolytic lesion in a long bone with a narrow zone of transition. The word “aneurysmal” alludes to the characteristic expansile nature of this lesion. The hallmark of an ABC is the blood–fluid level; however, this is not a specific finding and has been reported to occur in telangiectatic osteosarcoma, malignant fibrous histiocytoma, fibrous dysplasia, synovial sarcoma, haemangioma and simple bone cyst.
Primary ABCs most commonly occur in the first and second decades of life, but are rare below the age of 5 years. Only 3–6% of ABCs develop in the bones of the cranium.4 A review of the literature shows 15 cases of ABC of the frontal bone.5–18 Other than the frontal bone, ABCs have been reported in the temporal,19 parietal20 and occipital21 bones, as well as in the facial skeleton. Among the facial bones, ABC most commonly involves the mandible.22,23 Unlike the present case, which radiopathologically represented a primary ABC, many cases of calvarial and facial ABCs occur secondarily in fibrous dysplasia.20,24,25 In contrast, secondary ABCs of the long bones most commonly arise in a pre-existing GCT.
As ABCs are known to recur, the optimal treatment is total excision. Other established treatment modalities, especially in complex areas such as the skull base, include arterial embolization, injection sclerotherapy, curettage (with or without bone grafting), cryotherapy, aspiration and drainage, radionuclide ablation, radiotherapy or a combination of these modalities. Radiotherapy alone, however has recently fallen out of favour owing to the risk of post-irradiation sarcoma.4 In secondary ABCs, the treatment plan is formulated according to the primary lesion that is identified. For example, an ABC in an osteosarcoma is treated more aggressively than an ABC that has developed in pre-existing fibrous dysplasia.
The first case of a frontal bone ABC reported in the literature in 19665 was managed conservatively and followed up for 2 years. All 15 cases of frontal bone ABC reported subsequently in the literature were treated with surgical excision, and some of the more recent case reports describe reconstructive cranioplasty.9,10 In the present case, the reconstruction performed using the outer table of the bone flap after excising the bone tumour is a novel approach to the surgery.
Conclusion
Intradiploic ABCs of the calvarium are rare, and this is especially true of the primary variety. Unlike this case, in the few instances of calvarial location of this lesion reported in the literature, the ABC occurs as a secondary phenomenon in pre-existing fibrous dysplasia. The authors feel that the rarity of this tumour in the calvarium may be related to the low venous pressure. This is supported by an interesting hypothesis found in the literature regarding the aetiology of primary ABCs, which states that the lesion is due to haemorrhage in the bone as a result of increased venous pressure. This is probably why ABCs are common in long bones, where the venous pressure is high and the marrow content is greater. Also unique to our case is the reconstruction performed using the outer table of the bone flap after excising the bone tumour.
References
- 1.Boyd RC. Aneurysmal bone cysts of the jaws. Br J Oral Surg 1979;16:248–253 [DOI] [PubMed] [Google Scholar]
- 2.Martinez V, Sissons HA. Aneurysmal bone cyst: a review of 123 cases including primary lesions and those secondary to other bone pathology. Cancer 1988;61:2291–2304 [DOI] [PubMed] [Google Scholar]
- 3.Kransdorf MJ, Sweet DE. Aneurysmal bone cyst: concept, controversy, clinical presentation, and imaging. AJR Am J Roentgenol 1995;164:573–580 [DOI] [PubMed] [Google Scholar]
- 4.Gan YC, Hockley AD. Aneurysmal bone cysts of the cranium in children. Report of three cases and brief review of the literature. J Neurosurg 2007;106:401–406 [DOI] [PubMed] [Google Scholar]
- 5.Burns-Cox CJ, Higgins AT. Aneurysmal bone cyst of the frontal bone. J Bone Joint Surg Br 1969;51:344–345 [PubMed] [Google Scholar]
- 6.Mufti ST. Aneurysmal bone cyst of the skull. Case report. J Neurosurg 1978;49:730–733 [DOI] [PubMed] [Google Scholar]
- 7.Cataltepe O, Inci S, Ozcan OE, Saglam S, Erbengi A. Aneurysmal bone cyst of the frontal bone. Surg Neurol 1990;33:391–394 [DOI] [PubMed] [Google Scholar]
- 8.Wojno KJ, McCarthy EF. Fibro-osseous lesions of the face and skull with aneurysmal bone cyst formation. Skeletal Radiol 1994;23:15–18 [DOI] [PubMed] [Google Scholar]
- 9.Guida F, Rapanè A, Conti C, Cagliari E, Civelli F, Trincia G. Cranial aneurysmal bone cyst: a diagnostic problem. With a review of the literature. Childs Nerv Syst 2001;17:297–301 [DOI] [PubMed] [Google Scholar]
- 10.Perić P, Antić B, Radić-Tasić O. Aneurysmal bone cyst of the frontal bone. Vojnosanit Pregl 2005;62:491–494 [DOI] [PubMed] [Google Scholar]
- 11.Clavel Escribano M, Robles Balibrea A, Clavel Laria P, Robles Cano V. Frontal bone aneurysmal cyst: case report. Neurocirugia (Astur) 2001;12:166–169 [PubMed] [Google Scholar]
- 12.Lin WC, Wu HT, Wei CJ, Chang CY. Aneurysmal bone cyst arising from fibrous dysplasia of the frontal bone. Eur Radiol 2004;14:930–932 [DOI] [PubMed] [Google Scholar]
- 13.O'Brien DP, Rashad EM, Toland JA, Farell MA, Phillips J. Aneurysmal bone cyst of the frontal bone: case report and review of literature. Br J Neurosurg 1994;8:105–108 [DOI] [PubMed] [Google Scholar]
- 14.Senol U, Karaali K, Akyuz M, Gelen T, Tuncer R, Luleci E. Aneurysmal bone cyst of the orbit. AJNR Am J Neuroradiol 2002;23:319–321 [PMC free article] [PubMed] [Google Scholar]
- 15.Nakoaka T, Matsuura H, Kamada H, Yamamoto Y, Itoh K. Aneurysmal bone cyst: transcranial contrast sonographic examination with pulse inversion harmonic imaging method. No To Shinkei 2002;54:1075–1080 [PubMed] [Google Scholar]
- 16.Alessio L, Iob I, Mottaran R, Salar G, Fiore D. Aneurysmal bone cyst of the frontoparietal bone. Riv Neurol 1989;59:53–57 [PubMed] [Google Scholar]
- 17.Tehranzadeh J, Jenkin JJ, Horton JA. Osteoblastoma with secondary aneurysmal bone cyst of the frontal bone. Skeletal Radiol 1983;10:276–280 [DOI] [PubMed] [Google Scholar]
- 18.Saha MM, Kapoor R. Aneurysmal bone cyst of the frontal bone: a case report. Australasian Radiol 1986;30:8–9 [DOI] [PubMed] [Google Scholar]
- 19.Paige ML, Chiu YT, Christ M. Aneurysmal bone cyst of the temporal bone. Neuroradiology 1979;18:161–164 [DOI] [PubMed] [Google Scholar]
- 20.Branch CL, Jr, Challa VR, Kelly DL., Jr Aneurysmal bone cyst with fibrous dysplasia of the parietal bone. Report of two cases. J Neurosurg 1986;64:331–335 [DOI] [PubMed] [Google Scholar]
- 21.Luccarelli G, Fornari M, Savoiardo M. Angiography and computerized tomography in the diagnosis of aneurysmal bone cyst of the skull: case report. J Neurosurg 1980;53:113–116 [DOI] [PubMed] [Google Scholar]
- 22.El Deeb M, Sedano HO, Waite DE. Aneurysmal bone cyst of the jaws. Report of a case associated with fibrous dysplasia and review of the literature. Int J Oral Surg 1980;9:301–311 [DOI] [PubMed] [Google Scholar]
- 23.Kalantar Motamedi MH. Aneurysmal bone cysts of the jaws: clinicopathological features, radiographic evaluation and treatment analysis of 17 cases. J Craniomaxillofac Surg 1998;26:56–62 [DOI] [PubMed] [Google Scholar]
- 24.Rappaport ZH. Aneurysmal bone cyst associated with fibrous dysplasia of the skull. Neurochirurgia (Stuttg) 1989;32:192–194 [DOI] [PubMed] [Google Scholar]
- 25.Som PM, Schatz CJ, Flaum EG, Lanman TH. Aneurysmal bone cyst of the paranasal sinuses associated with fibrous dysplasia: CT and MR findings. J Comput Assist Tomogr 1991;15:513–515 [DOI] [PubMed] [Google Scholar]