Abstract
Objectives
The aim of this study was to compare diagnostic accuracy of cone beam CT (CBCT) and multislice CT in artificially created fractures of the sheep mandibular condyle.
Methods
63 full-thickness sheep heads were used in this study. Two surgeons created the fractures, which were either displaced or non-displaced. CBCT images were acquired by the NewTom 3G® CBCT scanner (NIM, Verona, Italy) and CT imaging was performed using the Toshiba Aquillon® multislice CT scanner (Toshiba Medical Systems, Otawara, Japan). Two-dimensional (2D) cross-sectional images and three-dimensional (3D) reconstructions were evaluated by two observers who were asked to determine the presence or absence of fracture and displacement, the type of fracture, anatomical localization and type of displacement. The naked-eye inspection during surgery served as the gold standard. Inter- and intra-observer agreements were calculated with weighted kappa statistics. The receiver operating characteristics (ROC) curve analyses were used to compare statistically the area under the curve (AUC) of both imaging modalities.
Results
Kappa coefficients of intra- and interobserver agreement scores varied between 0.56 – 0.98, which were classified as moderate and excellent, respectively. There was no statistically significant difference between the imaging modalities, which were both sensitive and specific for the diagnosis of sheep condylar fractures.
Conclusions
This study confirms that CBCT is similar to CT in the diagnosis of different types of experimentally created sheep condylar fractures and can provide a cost- and dose-effective diagnostic option.
Keywords: cone beam computed tomography, multislice computed tomography, condyle, fracture, sheep
Introduction
Following two consensus meetings1,2 in which researchers have had only limited agreement on an optimal treatment strategy in adults3 subject to more than six classification proposals in the past 80 years,4 the treatment of mandibular condyle fractures still remains a controversial topic in maxillofacial traumatology.5 Mandibular condyle fractures account for 17.5 – 52% of all mandibular fractures.6 80% of the cases are unilateral, occurring mainly between the ages of 20 to 39 years and the male to female ratio is 3:1.7 These fractures are mostly caused by indirect forces transmitted from a distant point to the condylar area. Consequently, these fractures are prone to misdiagnosis.6,8 Common clinical signs include bone deflections, difficulty in opening the mouth, malocclusion, oedema and swelling in the peripheral region of the external acoustic meatus.9 Conservative approaches with bimaxillary fixation or open reduction with internal fixation are the main treatment options for condylar fractures. To decide between these two treatment modalities it is essential to analyse variables, such as maximum mouth opening, protrusion, tendency for scarring and the imaging characteristics of the fracture localization.10
The accurate diagnosis of mandibular condyle fractures requires a thorough radiographic examination. Conventional plain radiography may result in images with superimpositions of the adjacent tissues and overlapping of bony structures, which often makes the interpretation difficult, especially in sagittal and intracapsular fractures.2 This is a significant disadvantage in the imaging of high condylar fractures because the treatment outcome depends on the position of the fracture line, the comminution of the proximal fragments and the shortening of the mandibular ramus.11 On the other hand, cross-sectional tomography has been shown to have an accuracy of 87.5–96% in revealing structural changes of temporomandibular joint (TMJ).12 As a result, the introduction of modern CT has allowed the TMJ to be clearly visualized without the interference of nearby anatomical structures. However, the conventional CT concept has been criticized for the high radiation doses used, the high cost, the large space requirements and the high level of skill needed for interpretation.13–16 Cone beam CT (CBCT) has been introduced to overcome these limitations in the imaging of craniofacial structures. This technique uses a cone-shaped X-ray beam, in contrast to the fan-shaped X-ray beam of spiral CT. The object to be evaluated is captured as the radiation source falls onto a two-dimensional (2D) detector, allowing the single, rotation of the radiation source to capture the entire region of interest (ROI).17 This cost-efficient imaging modality has been used by a broad range of specialties including orthodontics, implantology and oral surgery.18 It has been found to be successful in producing multiplanar images of the dental structures and the TMJ with lower radiation doses, achieving a higher spatial resolution owing to its limited exposure field.18–20
CBCT and CT have been tested separately under different clinical and experimental conditions for the imaging of TMJ bone structures;20 however, no study has compared the diagnostic accuracy of these two imaging modalities in maxillofacial fractures. Therefore, the purpose of this paper is to evaluate CBCT and CT imaging techniques in experimentally created fractures of the sheep mandibular condyle.
Materials and methods
63 fresh sheep heads bred for human consumption and purchased from a local butcher shop were used in this study. All left and right TMJ regions were numbered consecutively using permanent marker pens. Odd numbers were assigned to the left TMJ of animals whereas even numbers represented the right side. Maxillo-mandibular fixation was achieved using soft ligature wires (Remanium®; Dentaurum Group, Ispringen, Germany). Two surgeons (YS and SS) performed the procedures and registered the type of fractures created; this information was not made available to the other researchers. The naked-eye inspection served, therefore, as the gold standard for the radiographic examinations. A modified version of the method described by Long and Goss21 was used. Following a pre-auricular incision, the TMJ capsule was exposed and cleared of soft tissues by a blunt dissection, and the inferior joint space was opened by a horizontal incision through the capsule at the condylar neck. The condylar head was isolated with a periosteal elevator, and the superior joint space was exposed by separating the lateral attachment of the disc through the inferior joint space. The anterior and posterior attachments of the disc were cut. Some of the condyles were left intact and served as sham-operated joints. The fractures were planned to be either displaced (medial, lateral, anterior and posterior displacements) or non-displaced (complete, incomplete or comminuted) (Figures 1–6). Experimental groups were distributed unevenly in order to prevent the observers from estimating the exact number of fractures in the groups (Figure 7). A 0.9 mm diameter straight fissure diamond burr with a long shaft mounted on a high-speed dental hand piece was used to create a deep crack in the direction of the planned fracture under constant irrigation and suction to prevent scattering of bony particles into the soft tissues. A periosteal elevator was inserted into the prepared gap and turned around itself until the condylar fragment was separated from the ramus. The proximal bone segment was then repositioned to the pre-determined location using pliers to simulate the displacement or was left in place for non-displaced but complete fractures. For the fissure-type fracture, the condylar segment was not completely separated. Small parallel cuts in the horizontal and vertical directions were prepared and cracked through the condylar surface for the comminuted type of fracture. All fractures were stabilized in position using cyanoacrylate-containing universal instant adhesive (Pattex®; Henkel Gmbh., Istanbul, Turkey) and photographed. Surgical wounds were then closed with 5.0 silk sutures. The sheep heads were seated on a custom-made adjustable transparent plastic template and fixed for radiographic analysis.
Figure 1.

Three-dimensional CT view of an anterior condyle displacement
Figure 6.
Cone beam CT imaging from the sagittal plane, note the posterior displacement of the condyle fracture
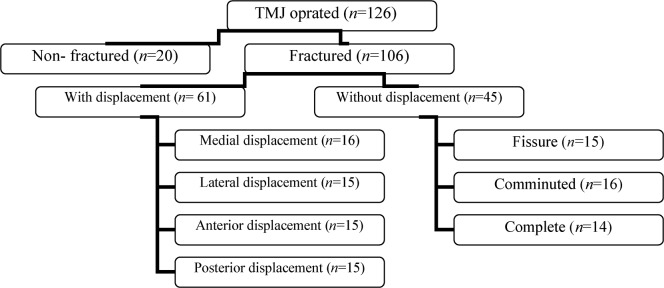
Figure 7.
Schematic presentation of the condylar fracture types and the distribution of experimental groups. TMJ, temporomandibular joint
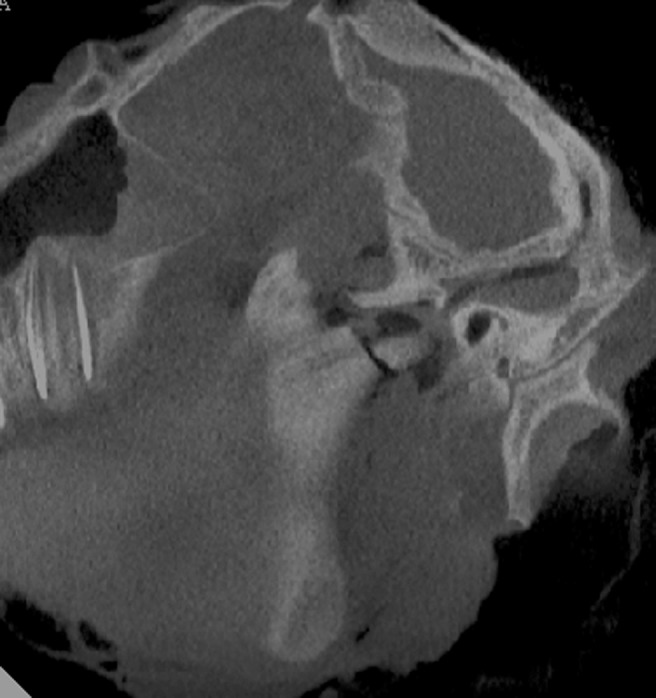
Figure 2.
Axial CT and cone beam CT views of bilateral condyle fractures with displacement. Right side (R): medial displacement, left side (L): lateral displacement
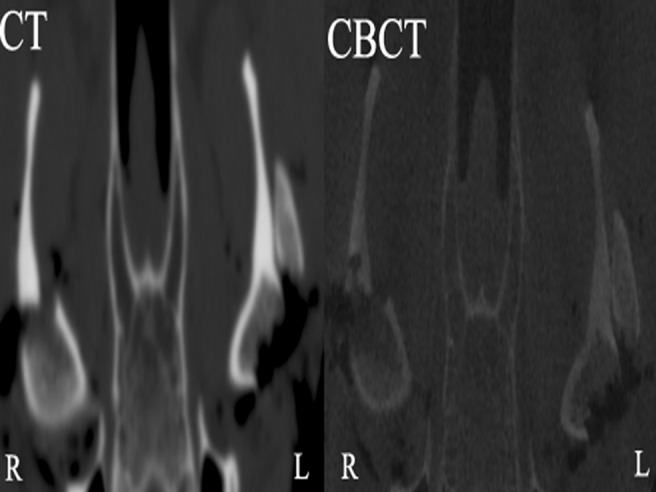
Figure 3.
Oblique CT view of a comminuted fracture (left) and a sham operated condyle (right)
Figure 4.
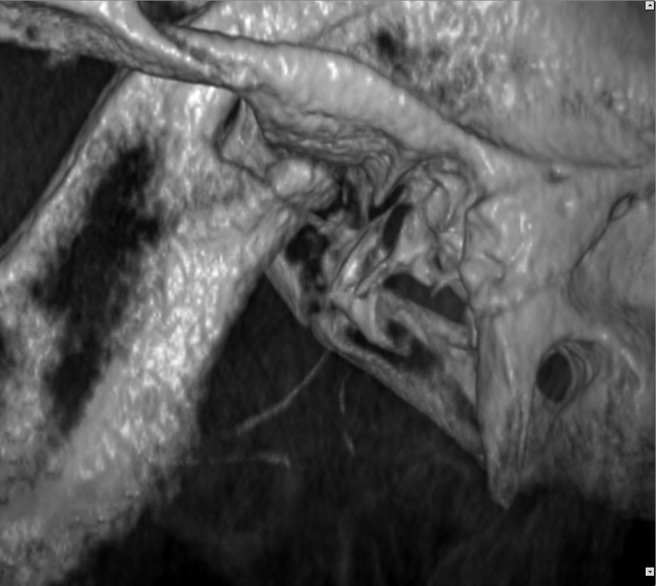
Three-dimensional reconstruction of a posteriorly displaced condyle fracture in cone beam CT
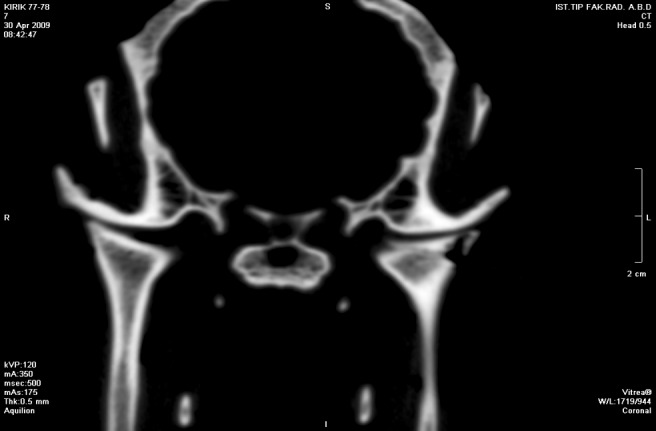
Figure 5.

Cone beam CT of bilateral fractured condyles from the coronal plane. Medial displacement on the left and a fracture without displacement on the right side are clearly visible
Conventional multislice spiral tomography
The sheep heads were scanned with a Toshiba Aquilion 64-slice scanner® (Toshiba Medical Systems, Otawara, Japan). After obtaining anterior–posterior and lateral scouts, the field of view (FOV) was decided at the table, as the sizes of the heads were different from each other, ranging from 24 to 32 cm. The scanning parameters were as follows: 0.5 mm collimation, 0.5 s gantry rotation time, 1.0 pitch, 120 kV and 175 mAs, acquisition time 9–15 s with volumetric data acquisition enabled. The images were reconstructed at 0.5 mm intervals in 64 slices without any interslice gaps using both head and bone tissue filters. The reconstructed images were transferred to the workstation using Vitrea 2 software®, version 4.1 (Vital Images Inc., Minnetonka, MN). The reconstructed images were analysed by standardized 0.5 mm slice thickness, 0.5 mm reconstruction interval in axial, coronal and sagittal multiplanar reformatted (MPR) views, and 3D views. Window levels were set to W 3000 and L 800, and a 23 inch Apple® high-definition display monitor (Apple Inc., Cupertino, CA) was used for image evaluation.
Cone beam CT
All sheep heads were scanned using the NewTom 3G® CBCT scanner (NIM, Verona, Italy) with a 9 inch detector field and automatic exposure parameters. The scanner operates with a maximum output of 110 kV and 15 mAs. Average scan time is 36 s and typical exposure time is 5.4 s. Safe Beam® and Smart Beam® technologies used in CBCT automatically adjust the radiation dose based on the patient size. Therefore, these exposure parameters were different for each sheep head. Specimens were placed in the supine position in the scanner's gantry by aligning the mid-sagittal plane of the sheep head to the scanner's medial light beam, and the lateral light spot was centred at the level of the condyle, indicating the optimized centre of the reconstruction area. The position of the specimen was checked and small adjustments were made according to frontal and lateral scout views. Scanning was performed by a single 360° rotation of the X-ray tube-detector system around the sheep heads. The CT data were imported into the NewTom 3G® software for the reconstruction of images. Post-processing was applied to the initial raw data by selecting a small field, high resolution and 0.5 mm of axial slice. A new FOV was formed with 240 axial cuts, and secondary reconstruction was performal to produce MPR images. Axial, coronal and sagittal images with 0.5 mm slice thickness and 0.5 mm reconstruction interval were displayed on a 23 inch Philips® (Royal Philips Electronics Inc., Amsterdam, the Netherlands) LCD monitor. The density and the contrast of the images were adjusted to a standard bone window and level (W/L 3000/800, respectively). The sheep heads were treated as medical waste and were disposed of in red bags as soon as the radiographs were taken.
A pre-calibration session was conducted to familiarize the two observers with the sheep head anatomy. Observer 1 (KG) was a general radiologist working in the head and neck region and observer 2 (SH) was an oral and maxillofacial radiologist. Both observers had over 5 years of experience with TMJ evaluation. They independently assessed left and right joints with both imaging modalities in different sessions in a randomized order for presence (1) or absence (0) of fracture and presence (1) or absence (0) of displacement. Whenever a displacement was detected, the observers were asked to describe the type of displacement (1, medial; 2, lateral; 3, anterior; 4, posterior) and in the case of a non-displaced, but fractured, condyle they had to decide the presence (1) or the absence (0) of either one of the fissure, comminuted or complete types of fractures. The TMJ regions labelled with odd numbers were assessed a second time after 3 weeks using the same procedures with both radiographic modalities to evaluate intra-observer reproducibility.
Statistical analysis
Data were analysed using MedCalc 7.2 statistical software® (MedCalc Inc., Mariakerke, Belgium). The weighted kappa values were calculated to measure intra- and interobserver variability and to assess the level of agreement between these values and the gold standard. These results were interpreted according to the criteria of Landis and Koch:22 0.81 (very good or excellent), 0.61–0.80 (good or substantial), 0.41–0.60 (moderate), 0.21–0.40 (fair) and 0.20 (poor) agreement. The diagnostic accuracies of the imaging modalities were compared with the gold standard by calculating the percentage of sensitivity and specificity values which were presented as receiver operating characteristics (ROC) curve areas. The area under the curve (AUC) was statistically compared in a confidence interval of 95%, and the results were considered significant when the P-value was less than or equal to 0.05.
Results
One sheep's head already had a posteriorly displaced bone fragment in the condylar area and a mandibular angle fracture, which was probably due to transportation. This case was also included in the study. The kappa values for intra-observer agreement of observer 1 varied between 0.56 and 0.92 (moderate to excellent) for CT and between 0.64 and 0.92 (good to excellent) for CBCT. Observer 2 had similar scores for both imaging modalities, 0.57–0.92 for CT and 0.79–0.92 for CBCT. The kappa values for the two observers revealed good to excellent agreement for CT and CBCT (0.62–0.98 and 0.60–0.97, respectively). The complete and comminuted fractures had the lowest agreement scores between the observers, although these differences were not statistically significant. Both tomographic devices were found to produce reliable images as the kappa values obtained in comparison with the gold standard were 0.69–0.97 for CT and 0.68–0.96 for CBCT. Furthermore, CT and CBCT were in good to excellent agreement as the kappa values were 0.64–0.94 for the interpretation of the reconstructed images. There was no difference in the diagnostic accuracies of CT and CBCT with respect to the variables examined, as the comparison of AUCs revealed no statistically significant results (Table 1).
Table 1. Statistical comparison of the area under the curve values for diagnostic accuracy of imaging modalities.
| CT |
Cone beam CT |
CT/Cone beam CT |
||
| AUC ± SE | AUC ± SE | Difference between areas | P-value | |
| Presence of fracture | 0.997 ± 0.002 | 0.995 ± 0.003 | 0.002 | 0.664 |
| Presence of displacement | 0.923 ± 0.014 | 0.931 ± 0.014 | 0.008 | 0.582 |
| Type of displacement | 0.709 ± 0.042 | 0.799 ± 0.042 | 0.009 | 0.772 |
| Fissure fracture | 0.949 ± 0.023 | 0.882 ± 0.034 | 0.067 | 0.076 |
| Comminuted fracture | 0.846 ± 0.036 | 0.891 ± 0.031 | 0.044 | 0.278 |
| Non-displaced complete fracture | 0.902 ± 0.032 | 0.887 ± 0.034 | 0.015 | 0.721 |
AUC, area under the curve; SE, standard error
Discussion
The selection criteria for an imaging modality suggest that a radiographic examination can contribute to the proper diagnosis and care of the patient.23 Radiographic analysis has long been considered an integral part of TMJ examination, which is often necessary for the treatment of diseases and conditions compromising the integrity of this region.24,25 Panoramic radiographs, transcranial projections and conventional tomography have been found to have limited accuracy in the imaging of TMJ,23,26,27 whereas MRI is thought to provide more information than any other imaging modality, especially for the soft tissue components of the joint.28,29 This option might be technically considered optimal for TMJ imaging; however, from a practical point of view, CT is the most useful imaging modality in the diagnosis of disorders affecting the bony components of TMJ. Complex anatomical structures surrounding the joint require high-quality cross-sectional and multiplanar views, particularly in the cases of condylar fractures which usually contain small bone fragments.30,23,29 To compare the accuracy of CT and CBCT, both of which are capable of producing such detailed images, an in vivo study model was used and modified by adding different types of fractures from in vivo experimental work21 on the healing of intracapsular condylar fracture in sheep. The results showed good correlation in intra- and extra-observer scores and were generally in good agreement with the gold standard.
Conventional CT has been used largely for the assessment of TMJ pathology.9,20,23,31 In earlier studies, Westesson et al32 compared the effectiveness of CT with MRI in detecting bone and soft tissue changes of the autopsy specimens and suggested that CT was superior to MRI in showing osseous abnormalities, whereas Tanitomo et al,33 who examined the diagnostic yield of the structural changes on TMJ, concluded that the temporal component is better visualized by axially corrected tomography than CT. However, these early results must be approached with caution as these studies probably do not reflect the true potential of today's CT technology. Accordingly, Katsumata et al34 found good agreement between CT and MRI in the remodelling of the condyle following mandibular setback osteotomy for prognatism. Cara et al35 tested the validity of single-slice and multislice CT for the detection of simulated condyle lesions on dry mandibles using different observation protocols. They reported that the best results for mandibular condyle assessment were obtained by using multislice CT with an axial/MPR protocol and correlated these findings with the extended anatomical coverage of TMJ using thinner slices. They also pointed out that these values could be changed owing to the attenuation of radiographs if there were soft tissues surrounding the joint. This approach was one of the reasons a full-thickness model was chosen for this study and similar equipment and protocols were used in detecting condylar fractures. The present results also support the use of the axial/MPR approach in the imaging of condylar fractures. Additionally, within the limits of this study, it is thought that existing soft tissues did not hamper the diagnostic capacity of CT for any type of fractures examined, as there was good agreement between this imaging modality and the gold standard. Costa e Silva et al30 evaluated the validity of 2D and 3D CT in condylar fractures of 18 patients, considering surgery as the gold standard. They concluded that the two reconstruction procedures presented similar diagnostic validity. They also noted that the 3D CT technique provided an improvement in the anatomical localization of the fracture and in the sensitivity of detecting comminution and bone displacements. The present study also used 3D techniques as a supplementary viewing process not only for diagnosis, but to confirm the position of the fractures.
Although CBCT is a relatively new concept in maxillofacial radiology, it has already been used specifically on TMJ imaging.19 Recently, Ikeda and Kawamura36 used limited CBCT to assess optimal condylar position. Furthermore, Alexiou et al37 evaluated the severity of TMJ osteoarthritis changes using CBCT and correlated these deformations with age. Cevidanes et al38 also used this modality to compare displacement of the condyle inside the glenoid fossa following orthognatic surgery using superimposition of 3D models constructed from CBCT. Similarly, Schlueeter et al16 examined optimal window levels and width needed for condyle examination on 3D reconstructions from CBCT. They suggested that the soft tissue will reduce the observer's capacity to view bone topography, and 3D reconstructed images may not be a reliable way to diagnose condylar pathology and morphology. Considering the fractures as lesions on the condyle, the present findings with CBCT reveal that this modality was able to produce results consistent with the naked-eye inspection when examined by both observers. 3D reconstructions were used as an adjunct to multiplanar examination of condylar fractures.
As this was the first in vitro study comparing the diagnostic accuracy of CT and CBCT in experimentally created condylar fractures, there are no previous articles that can be directly related to the results. However, these imaging modalities have previously been used to examine the TMJ in different experimental settings. Honda et al15 examined helical CT and CBCT in the detection of mandibular condyle osseous abnormalities on autopsy specimens. They found good agreement between the imaging modalities and macroscopic observations concerning normal cortical bone, condylar osteophytosis and condylar erosion. On the other hand, Hintze et al39 compared the reliability of CBCT and conventional tomography using the Cranex-Tome® unit detecting morphological changes of the condyle in dry skulls, described as flattening, defects and osteophytes. They observed low sensitivity, but high specificity for various types of changes, and they also stated that conventional spiral tomography showed a significantly higher specificity than CBCT, but only for the detection of defects on frontal views. Moreover, they reported large, but non-significant, observer variations in the assessment of condylar changes with conventional tomography for the detection of bone defects, and correlated these results with the particular difficulty arising from identifying these defects. Honey et al40 used a similar study design focusing on condylar erosion in which they compared the diagnostic reliability of CBCT, TMJ panoramic projections and corrected angle linear tomography. They obtained substantially greater intra-observer agreement than with plane projection linear tomography and higher diagnostic accuracy with CBCT than with other imaging modalities. The present findings show a mostly good level of agreement between the observers on the imaging modalities and the gold standard. Furthermore, no difference in the diagnostic accuracy of any imaging modality was observed with the experimental settings. The differences between our results and those of the aforementioned studies are probably related to the wide range of equipment and imaging protocols which were used. To overcome this predictable inconsistency, which is also a limitation in this study, the use of high-end devices was preferred, and the set-up of sophisticated observational standards by equalizing data acquisition and processing was used as far as possible within the limits of different hardware and software structures of the imaging modalities.
In conclusion, the accuracy of CBCT, which is a relatively new concept in maxillofacial radiology, is similar to that of CT in the diagnosis of different types of experimentally created sheep condylar fractures. Furthermore, CBCT is significantly cheaper and it uses a considerably lower radiation doses than conventional CT. From this point of view, CBCT provides a cost- and dose-effective alternative diagnostic method in maxillofacial imaging.
Acknowledgments
This work was supported by a Research Fund of the Istanbul University, project number, UDP-3786/22052009. This article has been partially presented as a poster in the 17th International Congress of Dentomaxillofacial Radiology, 28 June – 2 July 2009, Amsterdam, the Netherlands.
Footnotes
This article has been partially presented as a poster in the 17th International Congress of Dentomaxillofacial Radiology, 28 June – 2 July 2009, Amsterdam, the Netherlands.
References
- 1.Consensus conferenceonopenorclosedmanagementofcondylarfractures 12th ICOMS. Budapest, 1995. Int J Oral Maxillofac Surg 1998;27:243–267 [DOI] [PubMed] [Google Scholar]
- 2.Bos RR, Ward Booth RP, de Bont LG. Mandibular condyle fractures: a consensus. Br J Oral Maxillofac Surg 1999;37:87–89 [DOI] [PubMed] [Google Scholar]
- 3.Andersson J, Hallmer F, Eriksson L. Unilateral mandibular condylar fractures: a 31-year follow-up of non-surgical treatment. Int J Oral Maxillofac Surg 2007;36:310–314 [DOI] [PubMed] [Google Scholar]
- 4.Haug RH, Brandt MT. Closed reduction, open reduction, and endoscopic assistance: current thoughts on the management of mandibular condyle fractures. Plast Reconstr Surg 2007;120:90s–102s [DOI] [PubMed] [Google Scholar]
- 5.Ellis E, Throckmorton GS. Treatment of mandibular condylar process fractures: biological considerations. J Oral Maxillofac Surg 2005;63:115–134 [DOI] [PubMed] [Google Scholar]
- 6.Zachariades N, Mezitis M, Mourouzis C, Papadakis D, Spanou A. Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections on treatment and proposals. J Craniomaxillofac Surg 2006;34:421–432 [DOI] [PubMed] [Google Scholar]
- 7.Rutges JP, Kruizinga EH, Rosenberg A, Koole R. Functional results after conservative treatment of fractures of the mandibular condyle. Br J Oral Maxillofac Surg 2007;45:30–34 [DOI] [PubMed] [Google Scholar]
- 8.Silvennoinen U, Iizuka T, Lindqvist C, Oikarinen K. Different patterns of condylar fractures: an analysis of 382 patients in a 3-year period. J Oral Maxillofac Surg 1992;50:1032–1037 [DOI] [PubMed] [Google Scholar]
- 9.Raustia AM, Pyhtinen J, Oikarinen KS, Altonen M. Conventional radiographic and computed tomographic findings in cases of fracture of the mandibular condylar process. J Oral Maxillofac Surg 1990;48:1258–1262 [DOI] [PubMed] [Google Scholar]
- 10.Carneiro S, Vasconcelos B, Caldas A, Jr, Leal J, Frazao M. Treatment of condylar fractures: A retrospective cohort study. Med Oral Patol Oral Cir Bucal 2008;13:E589–E594 [PubMed] [Google Scholar]
- 11.Hlawitschka M, Loukota R, Eckelt U. Functional and radiological results of open and closed treatment of intracapsular (diacapitular) condylar fractures of the mandible. Int J Oral Maxillofac Surg 2005;34:597–604 [DOI] [PubMed] [Google Scholar]
- 12.Manzione JV, Katzberg RW, Manzione TJ. Internal derangements of the temporomandibular joint. II. Diagnosis by arthrography and computed tomography. Int J Periodontics Restorative Dent 1984;4:16–27 [PubMed] [Google Scholar]
- 13.Loubele M, Bogaerts R, Van DE, Pauwels R, Vanheusden S, Suetens P, et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol 2009;71:461–468 [DOI] [PubMed] [Google Scholar]
- 14.Schulze D, Heiland M, Thurmann H, Adam G. Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems and conventional radiography. Dentomaxillofac Radiol 2004;33:83–86 [DOI] [PubMed] [Google Scholar]
- 15.Honda K, Larheim TA, Maruhashi K, Matsumoto K, Iwai K. Osseous abnormalities of the mandibular condyle: diagnostic reliability of cone beam computed tomography compared with helical computed tomography based on an autopsy material. Dentomaxillofac Radiol 2006;35:152–157 [DOI] [PubMed] [Google Scholar]
- 16.Schlueter B, Kim KB, Oliver D, Sortiropoulos G. Cone beam computed tomography 3D reconstruction of the mandibular condyle. Angle Orthod 2008;78:880–888 [DOI] [PubMed] [Google Scholar]
- 17.Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am 2008;52:707–30, v [DOI] [PubMed] [Google Scholar]
- 18.De Vos W, Casselman J, Swennen GR. Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: a systematic review of the literature. Int J Oral Maxillofac Surg 2009;38:609–625 [DOI] [PubMed] [Google Scholar]
- 19.Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol 2004;33:196–201 [DOI] [PubMed] [Google Scholar]
- 20.Hussain AM, Packota G, Major PW, Flores-Mir C. Role of different imaging modalities in assessment of temporomandibular joint erosions and osteophytes: a systematic review. Dentomaxillofac Radiol 2008;37:63–71 [DOI] [PubMed] [Google Scholar]
- 21.Long X, Goss AN. A sheep model of intracapsular condylar fracture. J Oral Maxillofac Surg 2007;65:1102–1108 [DOI] [PubMed] [Google Scholar]
- 22.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–174 [PubMed] [Google Scholar]
- 23.Brooks SL, Brand JW, Gibbs SJ, Hollender L, Lurie AG, Omnell KA, et al. Imaging of the temporomandibular joint: a position paper of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;83:609–618 [DOI] [PubMed] [Google Scholar]
- 24.Westesson PL. Arthrography of the temporomandibular joint. J Prosthet Dent 1984;51:535–543 [DOI] [PubMed] [Google Scholar]
- 25.Roberts C, Katzberg RW, Tallents RH, Espeland MA, Handelman SL. The clinical predictability of internal derangements of the temporomandibular joint. Oral Surg Oral Med Oral Pathol 1991;71:412–414 [DOI] [PubMed] [Google Scholar]
- 26.Larheim TA. Current trends in temporomandibular joint imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;80:555–576 [DOI] [PubMed] [Google Scholar]
- 27.Ludlow JB, Davies KL, Tyndall DA. Temporomandibular joint imaging: a comparative study of diagnostic accuracy for the detection of bone change with biplanar multidirectional tomography and panoramic images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;80:735–743 [DOI] [PubMed] [Google Scholar]
- 28.Boeddinghaus R, Whyte A. Current concepts in maxillofacial imaging. Eur J Radiol 2008;66:396–418 [DOI] [PubMed] [Google Scholar]
- 29.Schimming R, Eckelt U, Kittner T. The value of coronal computer tomograms in fractures of the mandibular condylar process. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;87:632–639 [DOI] [PubMed] [Google Scholar]
- 30.Costa eSilva AP, Antunes JL, Cavalcanti MG. Interpretation of mandibular condyle fractures using 2D- and 3D-computed tomography. Braz Dent J 2003;14:203–208 [DOI] [PubMed] [Google Scholar]
- 31.Choi BH, Huh JY, Yoo JH. Computed tomographic findings of the fractured mandibular condyle after open reduction. Int J Oral Maxillofac Surg 2003;32:469–473 [PubMed] [Google Scholar]
- 32.Westesson PL, Katzberg RW, Tallents RH, Sanchez-Woodworth RE, Svensson SA. CT and MR of the temporomandibular joint: comparison with autopsy specimens. AJR Am J Roentgenol 1987;148:1165–1171 [DOI] [PubMed] [Google Scholar]
- 33.Tanimoto K, Petersson A, Rohlin M, Hansson LG, Johansen CC. Comparison of computed with conventional tomography in the evaluation of temporomandibular joint disease: a study of autopsy specimens. Dentomaxillofac Radiol 1990;19:21–27 [DOI] [PubMed] [Google Scholar]
- 34.Katsumata A, Nojiri M, Fujishita M, Ariji Y, Ariji E, Langlais RP. Condylar head remodeling following mandibular setback osteotomy for prognathism: a comparative study of different imaging modalities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:505–514 [DOI] [PubMed] [Google Scholar]
- 35.Cara AC, Gaia BF, Perrella A, Oliveira JX, Lopes PM, Cavalcanti MG. Validity of single- and multislice CT for assessment of mandibular condyle lesions. Dentomaxillofac Radiol 2007;36:24–27 [DOI] [PubMed] [Google Scholar]
- 36.Ikeda K, Kawamura A. Assessment of optimal condylar position with limited cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2009;135:495–501 [DOI] [PubMed] [Google Scholar]
- 37.Alexiou K, Stamatakis H, Tsiklakis K. Evaluation of the severity of temporomandibular joint osteoarthritic changes related to age using cone beam computed tomography. Dentomaxillofac Radiol 2009;38:141–147 [DOI] [PubMed] [Google Scholar]
- 38.Cevidanes LH, Bailey LJ, Tucker SF, Styner MA, Mol A, Phillips CL, et al. Three-dimensional cone-beam computed tomography for assessment of mandibular changes after orthognathic surgery. Am J Orthod Dentofacial Orthop 2007;131:44–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hintze H, Wiese M, Wenzel A. Cone beam CT and conventional tomography for the detection of morphological temporomandibular joint changes. Dentomaxillofac Radiol 2007;36:192–197 [DOI] [PubMed] [Google Scholar]
- 40.Honey OB, Scarfe WC, Hilgers MJ, Klueber K, Silveira AM, Haskell BS, et al. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: comparisons with panoramic radiology and linear tomography. Am J Orthod Dentofacial Orthop 2007;132:429–438 [DOI] [PubMed] [Google Scholar]