Abstract
Objective
The aim of the study was to evaluate the usefulness of cone beam CT (CBCT) in temporomandibular joints (TMJs) with soft tissue pathology.
Methods
106 TMJs of 55 patients with temporomandibular disorder (TMD) were examined by MRI and CBCT. MR images were used for the evaluation of disc displacement, disc deformity, joint effusion and obscurity of temporal posterior attachment (TPA). CBCT images were evaluated for the presence or absence of osseous abnormalities. The χ2 test was used to analyse the association between MRI and CBCT findings.
Results
MRI of 106 TMJs revealed disc displacement, disc deformity, joint effusion and obscurity of the TPA in 68, 73, 28 and 27 joints, respectively. Of the 68 TMJs with disc displacement, anterior disc displacement without reduction (ADDWR) was seen most frequently (47/68). CBCT imaging found 65 TMJs were characterized by the presence of osseous abnormalities and were significantly associated with disc deformity and ADDWR (P < 0.05). There was no statistically significant association between the presence of joint effusion and obscurity of TPA and TMJ osseous abnormalities.
Conclusions
TMD patients with confirmed ADDWR or disc deformity on MRI are at risk of having osseous abnormalities in the TMJ and further examination with CBCT is recommended.
Keywords: temporomandibular joint, soft tissue pathology, magnetic resonance imaging, cone beam computed tomography
Introduction
The temporomandibular joint (TMJ) is a unique joint that can be affected by different kinds of hard and soft tissue abnormalities. Several authors1–3 have shown the correct diagnosis of early abnormalities is paramount because they can result in a temporomandibular disorder (TMD).
MRI is considered the prime imaging of choice for the evaluation of soft tissue components of the TMJ4–6 and should precede cone beam CT (CBCT) for cases in which the diagnosis of soft tissue pathology is a concern, or in cases where ionizing radiation should be avoided.
CT or CBCT is considered the modality of choice for imaging the osseous components of the TMJ,7–9 and in these studies the authors emphasized the usefulness of CBCT due to its high spatial resolution and low radiation dose; however, no specific patient selection criteria have been published regarding the use of CBCT for TMD patients. Thus, the aim of the present study was to evaluate the usefulness of CBCT in TMJs with different soft tissue pathology, and to identify if any of these pathologies can be an indication for CBCT examination.
Materials and methods
Patients
55 Asian patients (110 TMJs) with clinical manifestations of TMD-like clicking, joint noise or joint pain, who consulted our hospital between December 2002 and April 2008, and underwent MRI and CBCT examinations, were included in this study. Four joints were excluded from the study due to motion artefacts of either modality and the remaining 106 TMJs were used. The patients comprised 24 males and 31 females with a mean age of 41 years (range, 13–69).
The study was approved by our Institutional Review Board and informed consent was obtained from all the patients before examination by both modalities.
MRI examination
All MR images were obtained using a 1.5 T scanner (Magnetom Vision, Siemens Medical Systems, Erlangen, Germany) with a 3-inch-diameter bilateral TMJ surface coil and a field of view size of 120 × 120 mm. On the sagittal plane both the proton density-weighted image sequence (PDWI) and fat-suppressed T2 weighted image sequence (T2WI) were obtained: repetition time (TR)/echo time (TE), 1000/20 ms (PDWI) or 2931/96 ms (T2WI); slice thickness, 3 mm; interslice gap, 0.3–0.6 mm; number of images, 7. On the coronal plane only PDWI was obtained: TR/TE, 960–980/15 ms; slice thickness, 3 mm; interslice gap, 0.3–0.6 mm; number of images, 7. All images were obtained in a closed-mouth position except in the sagittal plane, where another PDWI was obtained in the open-mouth position. Imaging time was 4.19 min for PDWI sagittal images, 2.0 min for PDWI coronal images and 3.19 min for T2WI sagittal images.
Cone beam CT examination
The CBCT apparatus was a 3DX multi-image micro CT (Morita Corporation, Kyoto, Japan) developed by Arai et al.7 The imaging area of the CBCT was a cylinder with a height of 30 mm (240 voxels) and a diameter of 40 mm (320 voxels) providing isotropic cubic voxels with sides approximating 0.125 mm. The TMJs were examined bilaterally and imaged at a tube voltage of 80 kV, a tube current of 4.5 mA and exposure time of 17 s. Examinations were performed by 360° rotation in an occlusal position. After scanning, contiguous sectional images in three directions, i.e. parasagittal section (vertical to the long axis of condylar head), coronal section (parallel to the long axis of condylar head) and horizontal section images, were reconstructed from the projected data with a slice width of 1 mm using dedicated CBCT software (Morita Corporation). The parasagittal images were not reformatted parallel to the ramus of the mandible.
Evaluation of images
MR images were evaluated on a cathode ray tube (CRT) monitor with installed Digital Imaging and Communications in Medicine (DICOM) image viewer. The presence or absence of disc displacement, disc deformity, joint effusion and temporal posterior attachment (TPA) was evaluated independently by two calibrated observers (MA and AK) with over 4 years' experience of MRI for maxillofacial diagnosis, including TMJ. If there was disagreement the observers evaluated the images for a second time and a consensus was reached after discussion. The interobserver agreement was evaluated using kappa statistics.
The criteria used by the observers were: disc displacement, when the posterior band of the disc is displaced from its normal position (12 o'clock position relative to the top of the condyle in the closed-mouth position); disc deformity, when there is an absence of a biconcave shape of the disc; joint effusion, when there is high signal intensity area in the joint space in at least two consecutive sections on T2WI; and TPA was considered obscured when it could not be visualized on both the closed and open-mouth PDWI. The disc was considered anteriorly displaced with reduction (ADDR) when the disc was displaced anteriorly in a closed-mouth position, but assumed a normal position relative to the condyle upon jaw opening and was considered anteriorly displaced without reduction (ADDWR) when the disc was displaced anteriorly in all mouth positions. Posterior disc displacement was recorded when the posterior band was located posteriorly relative to the top of the condyle.
When necessary the window setting was adjusted to optimize the images for evaluation.
Two calibrated oral radiologists (NO and SN) with over 10 years' experience of CBCT for maxillofacial diagnosis including the TMJ evaluated CBCT images for the presence or absence of osseous abnormalities. Evaluation was done without previous knowledge of MRI findings. The osseous abnormalities recorded were erosions, deformity, sclerosis, ankylosis, osteophytosis and flattening of the condyle, but for temporal component only erosions and sclerosis were recorded. The criteria used by the observers were: erosion, an area of loss of the cortical bone; deformity, abnormal size or shape of the condyle; sclerosis, an area of increased density of cortical or subcortical bone; ankylosis, an area of obliteration of joint space; osteophytosis, an area of marginal bone formation on the condyle; and flattening, a flat bony surface in a load-bearing area.
The images were evaluated on a CRT monitor using a CBCT viewer (I-View, Morita Corporation). When necessary, the window setting was adjusted to optimize the images for evaluation. If there was disagreement regarding image assessment, the images were evaluated again and a consensus was reached by discussion. The interobserver agreement was evaluated with kappa statistics. All TMJs were classified into two groups: TMJs with osseous abnormalities (65 TMJs, Figures 2 and 4) and TMJs without osseous abnormalities (41 TMJs, Figures 1 and 3).
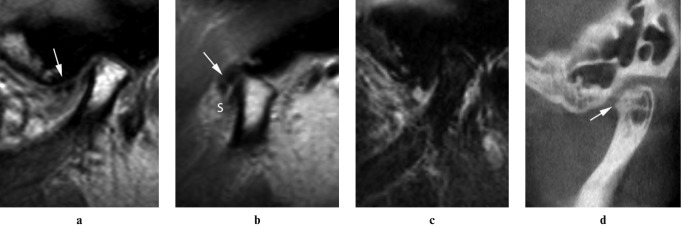
Figure 2.
Patient with suspected condylar osteophyte (s).The deformed articular disc is anteriorly displaced in closed sagittal proton density-weighted MR image (a, arrow) and was not reduced in open sagittal proton density-weighted MR image (b, arrow).There is no sign of joint effusion on T2 weighted image sequence (c) and the temporal posterior attachment could not be visualized in any image. The corresponding cone beam CT image revealed osteophyte in the condylar head (d, arrow)
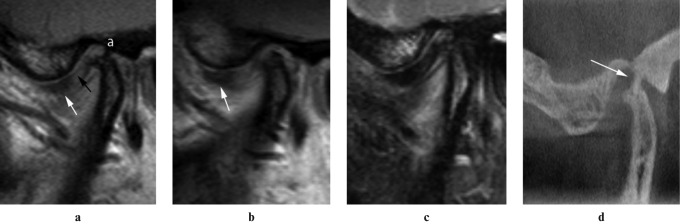
Figure 4.
Patient with suspected ankylosis (a). The deformed articular disc is anteriorly displaced in closed sagittal proton density-weighted MR image (a, white arrow) and was not reduced in open sagittal proton density-weighted MR image (b, arrow), there is no sign of joint effusion on T2 weighted image sequence (c) and the temporal posterior attachment could be visualized in closed sagittal proton density-weighted MR (a, black arrow). The corresponding cone beam CT image revealed ankylosis in the temporomandibular joint (d, arrow)
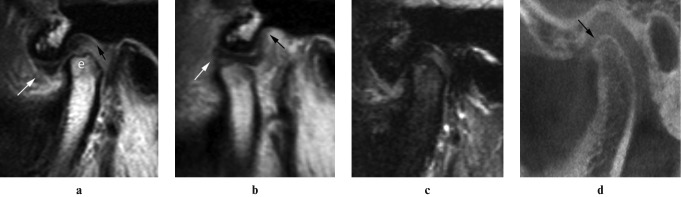
Figure 1.
Patient with suspected condylar erosion (e). The articular disc looks normal in shape and position on closed and open sagittal proton density-weighted MR image (a and b, white arrows), there is no sign of joint effusion on T2 weighted image sequence (c) and the temporal posterior attachment could be visualized (a and b, black arrows). The corresponding cone beam CT image revealed no osseous abnormality in the condylar head (d, arrow)
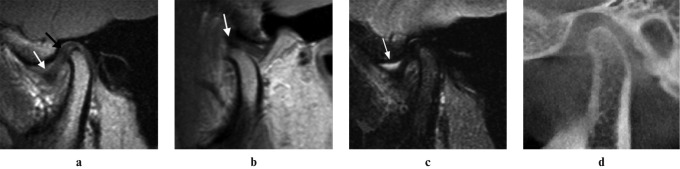
Figure 3.
Patient with joint effusion. The deformed articular disc is anteriorly displaced in closed sagittal proton density-weighted MR image (a, white arrow) and reduced on open sagittal proton density-weighted MR image (b, arrow). Superior joint space effusion was revealed on T2 weighted image sequence (c, arrow) and the temporal posterior attachment could be visualized in closed sagittal proton density-weighted MR (a, black arrow). The corresponding cone beam CT image revealed no osseous abnormality in the condylar head (d)
Statistical analysis
The χ2 test was used to assess the level of significance of the association between MRI findings of disc displacement, disc deformity, joint effusion and obscurity of TPA and osseous abnormalities of the TMJ.
Cohen's kappa (SPSS version 16, Chicago, IL) was used to determine the interobserver agreement based on the following criteria: kappa value of < 0.40 was considered to indicate poor agreement, 0.40–0.59 fair agreement, 0.60–0.74 good agreement and 0.75–1.00 excellent agreement.
Results
Of the 106 TMJs, MRI revealed disc displacement, disc deformity, joint effusion and obscurity of TPA in 68, 73, 28 and 27 joints, respectively (Table 1). Out of the 68 TMJs with disc displacement, ADDWR was seen most frequently (47/68, Table 2).
Table 1. Incidence of abnormalities in 106 temporomandibular joints (TMJ).
| Disc displacement | Disc deformity | Joint effusion | TPA obscurity | |
| TMJs with osseous changes | 49/65* | 53/65* | 19/65 | 18/65 |
| TMJs without osseous changes | 19/41 | 20/41 | 9/41 | 9/41 |
| Total | 68/106 | 73/106 | 28/106 | 27/106 |
*χ2 test, P < 0.05
TPA, temporal posterior attachment
Table 2. Incidence of different types of disc displacement in 68 temporomandibular joints (TMJ).
| Anterior with reduction | Anterior without reduction | Posterior | |
| TMJs with osseous changes | 7/49 | 40/49* | 2/49 |
| TMJs without osseous changes | 12/19 | 7/19 | 0/19 |
| Total | 19/68 | 47/68 | 2/68 |
*χ2 test, P < 0.05
For CBCT images the 106 TMJs were classified into two groups: TMJs with osseous abnormalities (n = 65) and TMJs without osseous abnormalities (n = 41). The frequency of osseous abnormalities for erosions, deformity, sclerosis, ankylosis, osteophytosis, and flattening of the condyle and temporal component were 42%, 25%, 40%, 5%, 13% and 18%, respectively.
Disc displacement and disc deformity were found in 49 and 53 of TMJs with osseous abnormalities (65 TMJs), respectively (Table 1). They were found significantly more frequently than in the other group (χ2 test, P < 0.05).
ADDR and ADDWR were found in the two groups of TMJs, whereas posterior disc displacement was only found in TMJs with osseous abnormalities (Table 2). Among the 68 TMJs with disc displacement, ADDWR was revealed in 40 TMJs with osseous abnormalities and this association was significant (χ2 test, P < 0.05).
Joint effusion and TPA obscurity were found in 19 and 18 TMJs with osseous abnormalities (65 TMJs), respectively and there was no statistically significant association (Table 1).
A statistically significant association between ADDWR and joint effusion, disc deformity and TPA obscurity was found (χ2, P < 0.05).
The interobserver agreement for MRI and CBCT was good for all types of soft tissue and osseous abnormalities.
Discussion
TMD patients can have different imaging findings of soft and hard tissue abnormalities of the TMJ, which can be studied using different imaging modalities. Among them, MRI is the primary imaging tool because it is not associated with ionizing radiation, offers direct visualization of the disc, shows surrounding muscles and attachments with high resolution and provides a comprehensive idea about the general condition of TMJ. However, its ability to detect osseous abnormalities is still considered poor or moderate and confirmation with CT or CBCT is needed.10,4
Osseous abnormalities can be identified with soft tissue pathology and this has clinical significance.11–14 They can lead to changes in the occlusion or conylar position on the affected side13,14 or can be associated with perforations15 and pain,12 even in cases without disc displacement. Recent treatment available to TMD patients is highly dependent on the presence or absence of osseous abnormalities,16 since the presence of osseous abnormalities can be a sign of a systemic disease or an irreversible condition that can be only treated by intra-articular injection of steroids or surgery. Therefore, the detection and correct diagnosis of such abnormalities is paramount.
To the best of our knowledge, there is no published research showing the association between MRI findings of TMJ soft tissue pathology and TMJ osseous abnormalities which have been confirmed by CBCT. By conducting this study we will be able to identify patients who are likely to benefit from CBCT examination.
TMJ osseous abnormalities can occur due to several predisposing factors such as, trauma, aging, parafunctional habits, systemic disease and disc displacement.1–3 Specifically, parafunctional habits or overloading is considered the most common local cause, as reported in the literature.1 Although disc displacement can be a cause of overloading1 and is commonly associated with osseous abnormalities,17,18 the cause–effect relationship between disc displacement and the occurrence of TMJ osseous abnormalities is still controversial and has not been fully established.19,20 Many TMD patients can adapt to overloading as a result of disc displacement or other causes,21,22 but can develop osseous abnormalities as a result of this.23,24
In agreement with other researchers17,18,25,26 our study showed a significant association between the presence of disc displacement or ADDWR and osseous abnormalities. Around 75% of TMJs with osseous abnormalities had disc displacement and around 82% of TMJs with ADDWR had one or more osseous abnormality. At the same time ADDWR was significantly associated with other MRI findings of disc deformity, joint effusion and obscurity of TPA; this could be due to the severity of the condition. Most of the TMJs with anterior disc displacement with reduction (ADDR) were more frequent in TMJs without osseous abnormality (12 out of 19 TMJs); this could support the hypothesis that there are normal variations in the location of the posterior band and it is not necessary to be in the 12 o'clock position, relative to the top of the condyle, on closing.3
Any case of ADDR can change into ADDWR and lead to disc deformity and finally result in perforation and bony changes.27 At the same time when deformation is localized to the posterior band this may influence the progression of ADDR to ADDWR.28 Westesson et al27 reported more frequent association of disc deformities and irregularities in the articular surface with transformation of disc displacement from partial to complete. These results indicate that some deformation of the disc can be seen before the occurrence of ADDWR and could increase after the occurrence of ADDWR and bony changes. In our study a significant association was noted between disc deformity and ADDWR, or between disc deformity and the presence of bony changes. Our results are in line with those of Westesson et al.27,29
Generally, the presence of fluid in the TMJ (i.e. joint effusion) is a sign of chronic inflammatory reaction and can be found frequently in asymptomatic patients30 or in patients with TMJ osseous abnormalities.31
However, in a study by Larheim et al32 the amount of joint fluid differed between the patients in the study, and the presence of a large amount of fluid was associated with internal derangement. In our study, we did not attempt to evaluate the amount of joint fluid and, in contrast with a study of Güler et al,33 the incidence of joint effusion was not significantly associated with TMJ osseous abnormalities. This could be due to the presence of joint effusion in TMJs without osseous abnormalities or because of differences in the underlying mechanisms involved in the formation of joint effusion and osseous abnormalities.
The bilaminar zone or posterior attachments of the disc can be divided into superior lamina or TPA, and inferior lamina or condylar posterior attachments. In one study by Katzberg et al34 TPA was visualized less in patients with disc displacements, either reduced or non-reduced disc displacement. In another study by Kuribayashi and Tallents35 the obscurity of TPA was significantly associated with disc perforation, and disc displacement was present in almost all patients with disc perforation.
In consensus with previous studies, our results showed a significant association between obscurity of TPA and the presence of ADDWR. One explanation could be that in the case of ADDWR the displacement results in stretching and thinning of TPA, which in turn causes difficulties in detecting the TPA in any mouth position. However, there was no significant association between obscurity of TPA and the presence of TMJ osseous abnormalities. In our study, in many TMJs with osseous abnormalities (47 of 65) a TPA was not considered obscured since it could be visualized in either the open- or closed-mouth position. Another explanation could be that under current spatial resolution of MRI the detection of TPA is difficult, even in cases without osseous abnormalities, and it was considered obscured in 9 TMJs out of 41 without osseous abnormalities. Since the visualization of TPA is related to discal status and spatial resolution of MRI, we could not find significant association between obscurity of TPA and the presence of TMJ osseous abnormalities.
In conclusion, TMD patients with confirmed ADDWR or disc deformity on MRI are at risk of having osseous abnormalities in the TMJ and further examination with CBCT is recommended.
References
- 1.Okeson JP. Management of temporomandibular disorders and occlusion (6th edn). St. Louis, MO: CV Mosby Company, 2007 [Google Scholar]
- 2.Laskin DM, Greene CS, Hylander WL. Temporomandibular disorders: an evidence-based approach to diagnosis and treatment (1st edn). Hanover Park, IL: Quintessence Publishing, 2006 [Google Scholar]
- 3.Wright EF. Manual of temporomandibular disorders (2nd edn). Ames, IA: Blackwell Munksgaard, 2005 [Google Scholar]
- 4.Westesson PL, Katzberg RW, Tallents RH, Sanchez-Wood-worth RE, Svensson SA. CT and MR of the temporomandibular joint: comparison with autopsy specimens. AJR Am J Roentgenol 1987;148:1165–1171 [DOI] [PubMed] [Google Scholar]
- 5.Westesson PL, Katzberg RW, Tallents RH, Sanchez-Woodworth RE, Svensson SA, Espeland MA. Temporomandibular joint: comparison of MR images with cryosectional anatomy. Radiology 1987;164:59–64 [DOI] [PubMed] [Google Scholar]
- 6.Tasaki MM, Westesson PL. Temporomandibular joint: diagnostic accuracy with sagittal and coronal MR imaging. Radiology 1993;186:723–729 [DOI] [PubMed] [Google Scholar]
- 7.Arai Y, Honda K, Iwai K, Shinoda K. Development of ortho cubic super high resolution CT. in: CARS 1998 computer assisted radiology and surgery Amsterdam: Elsevier; 1998; pp 780–785 [Google Scholar]
- 8.Honda K, Larheim TA, Maruhashi K, Matsumoto K, Iwai K. Osseous abnormalities of the mandibular condyle: diagnostic reliability of cone beam computed tomography with helical computed tomography based on an autopsy material. Dentomaxillofac Radiol 2006;35:152–157 [DOI] [PubMed] [Google Scholar]
- 9.Honey OB, Scarfe WC, Hilgers M, Klueber K, Silveira A, Haskell B, et al. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: comparisons with panoramic radiology and linear tomography. Am J Orthod Dentofacial Orthop 2007;132:429–438 [DOI] [PubMed] [Google Scholar]
- 10.Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, et al Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol 2009;107:844–860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Helenius LMJ, Tervahartiala P, Helenius I, Al-Sukhun J, Kivisaari L, Suuronen R, et al. Clinical, radiographic and MRI findings of the temporomandibular joint in patients with different rheumatic diseases. Int J Oral Maxillofac Surg 2006;35:983–989 [DOI] [PubMed] [Google Scholar]
- 12.Campos MI, Campos PS, Cangussu MC, Guimarães RC, Line SR. Analysis of magnetic resonance imaging characteristics and pain in temporomandibular joints with and without degenerative changes of the condyle. Int J Oral Maxillofac Surg 2008;37:529–534 [DOI] [PubMed] [Google Scholar]
- 13.Hirata FH, Guimaraes AS, Oliveira JX, Moreira CR, Ferreira ETT, Cavalcanti MGP. Evaluation of TMJ articular eminence morphology and disc patterns in patients with disc displacement in MRI. Braz Oral Res 2007;21:265–271 [DOI] [PubMed] [Google Scholar]
- 14.Sato S, Kawamura H. Changes in condylar mobility and radiographic alterations after treatment in patients with non-reducing disc displacement of the temporomandibular joint. Dentomaxillofac Radiol 2006;35:289–294 [DOI] [PubMed] [Google Scholar]
- 15.Takahashi A, Murakami S, Nishiyama H, Sasai T, Fujishita M, Fuchihata H. The clinicoradiologic predictability of perforations of the soft tissue of the temporomandibular joint. Oral Surg Oral Med Oral Pathol 1992;74:243–250 [DOI] [PubMed] [Google Scholar]
- 16.Scrivani SJ, Keirh DA, Kaban LB. Temporomandibular disorders. N Engl J Med 2008;359:2693–2705 [DOI] [PubMed] [Google Scholar]
- 17.Mills DK, Daniel JC, Herzog S, Scapino RP. An animal model for studying mechanisms in human temporomandibular joint disc derangement. J Oral Maxillofac Surg 1994;52:1279–1292 [DOI] [PubMed] [Google Scholar]
- 18.Helmy E, Bays R, Sharawy M. Osteoarthrosis of the temporomandibular joint following experimental disc perforation in Macaca fascicularis. J Oral Maxillofac Surg 1988;46:979–990 [DOI] [PubMed] [Google Scholar]
- 19.Pullinger AG, Seligman DA. TMJ osteoarthrosis: a differentiation of diagnostic subgroups by symptom history and demographics. J Craniomandib Disord 1987;1:251–256 [PubMed] [Google Scholar]
- 20.Pereira FJ, Jr, Lundh H, Westesson PL. Morphologic changes in the temporomandibular joint in different age groups. An autopsy investigation. Oral Surg Oral Med Oral Pathol 1994;78:279–287 [DOI] [PubMed] [Google Scholar]
- 21.Hall MB, Brown RW, Baughman RA. Histologic appearance of the bilaminar zone in internal derangement of the temporomandibular joint. Oral Surg Oral Med Oral Pathol 1984;58:375–381 [DOI] [PubMed] [Google Scholar]
- 22.Scapino RP. Histopathology associated with malposition of the human temporomandibular joint disc. Oral Surg Oral Med Oral Pathol 1983;55:382–397 [DOI] [PubMed] [Google Scholar]
- 23.Kurita H, Uehara S, Yokochi M, Nakatsuka A, Kobayashi H, Kurashina K. A long-term follow-up study of radiographically evident degenerative changes in the temporomandibular joint with different conditions of disk displacement. Int J Oral Maxillofac Surg 2006;35:49–54 [DOI] [PubMed] [Google Scholar]
- 24.Dimitroulis G. The prevalence of osteoarthrosis in cases of advanced internal derangement of the temporomandibular joint: a clinical, surgical and histological study. Int J Oral Maxillofac Surg 2005;34:345–349 [DOI] [PubMed] [Google Scholar]
- 25.De Leeuw R, Boering G, Stegenga B, De Bont LG. Symptoms of temporomandibular joint osteoarthrosis and internal derangement 30 years after non-surgical treatment. Cranio 1995;13:81–88 [DOI] [PubMed] [Google Scholar]
- 26.De Leeuw R, Boering G, Stegenga B, De Bont LG. Radiographic signs of temporomandibular joint osteoarthrosis and internal derangement 30 years after nonsurgical treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;79:382–392 [DOI] [PubMed] [Google Scholar]
- 27.Westesson PL, Bronstein SL, Liedberg J. Internal derangement of the temporomandibular joint: morphologic description with correlation to joint function. Oral Surg Oral Med Oral Pathol 1985;59:323–331 [DOI] [PubMed] [Google Scholar]
- 28.Westesson PL, Lundh H. Arthrographic and clinical characteristics patients with disk displacement who progressed to closed lock during a 6-month period. Oral Surg Oral Med Oral Pathol 1989;67:654–657 [DOI] [PubMed] [Google Scholar]
- 29.Westesson PL, Rohlin M. Internal derangement related to osteoarthrosis in temporomandibular joint autopsy specimens. Oral Surg Oral Med Oral Pathol 1984;57:17–22 [DOI] [PubMed] [Google Scholar]
- 30.Manfredini D, Basso D, Arboretti R, Guarda-Nardini L. Association between magnetic resonance signs of temporomandibular joint effusion and disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:266–271 [DOI] [PubMed] [Google Scholar]
- 31.Stegenga B, de Bont LG, Boering G, van Willigen JD. Tissue responses to degenerative changes in the temporomandibular joint: a review. J Oral Maxillofac Surg 1991;49:1079–1088 [DOI] [PubMed] [Google Scholar]
- 32.Larheim TA, Westesson PL, Sano T. MR grading of temporomandibular joint fluid: association with disk displacement categories, condyle marrow abnormalities and pain. Int J Oral Maxillofac Surg 2001;30:104–112 [DOI] [PubMed] [Google Scholar]
- 33.Güler N, Uçkan S, Imirzalioğlu P, Açikgözoğlu S. Temporomandibular joint internal derangement: relationship between joint pain and MR grading of effusion and total protein concentration in the joint fluid. Dentomaxillofac Radiol 2005;34:175–181 [DOI] [PubMed] [Google Scholar]
- 34.Katzberg RW, Tallents RH. Normal and abnormal temporomandibular joint disc and posterior attachment as depicted by magnetic resonance imaging in symptomatic and asymptomatic subjects. J Oral Maxillofac Surg 2005;63:1155–1161 [DOI] [PubMed] [Google Scholar]
- 35.Kuribayashi A, Okochi K, Kobayashi K, Kurabayashi T. MRI findings of temporomandibular joints with disk perforation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;106:419–425 [DOI] [PubMed] [Google Scholar]