Abstract
Ossifying fibroma is usually a unilocular lesion with a well-defined, thinly corticated margin radiographically, although various patterns have been noted. The patient was a 27-year-old woman with a painless radiolucent lesion demonstrated on panoramic radiography to involve the root-apex area of the left lower second and third molars. Radiographically, the lesion had some features of a benign tumour, such as an odontogenic myxoma. However, the deep invaginations towards the interalveolar septa suggested a simple bone cyst, whereas the irregular margin and lack of expansion or mandibular canal displacement were consistent with a malignant lesion. A hard tissue component was confirmed only by soft-tissue mode CT. Although this lesion was histopathologically diagnosed as ossifying fibroma, the conflicting imaging findings were challenging and very intriguing.
Keywords: fibroma, ossifying, radiography, computed tomography, mandible
Case report
A 27-year-old woman was referred to the outpatient clinic on 19 May 2006 with a painless swelling around the gingival aspect of the left mandibular wisdom tooth. The vitality of her teeth was confirmed with an electric pulp tester in the left first molar, left second molar and left third molar. Panoramic radiography at the initial visit revealed a radiolucent lesion with an irregular margin and sclerotic rim extending from the left second molar tooth to the mandibular angle (Figure 1). No expansion was seen on occlusal radiography. Intraoral radiography revealed the lesion to have deep invaginations towards the interalveolar septa, no divergence and no displacement of the inferior mandibular canal. The margin of the lesion showed a small vesicular area at the distal surface of the left third molar tooth. The lamina dura and periodontal space of the roots of the teeth were intact (Figure 2). Both benign lesions (e.g. simple bone cyst, odontogenic myxoma) and malignant lesions (e.g. squamous cell carcinoma) were considered from the radiolucent appearance of the lesion on plain radiography. Diagnostic imaging was then performed to more closely evaluate the lesion.
Figure 1.

Cropped panoramic radiograph showing a radiolucent lesion with an irregular margin and sclerotic rim extending from the left second molar tooth to the mandibular angle
Figure 2.
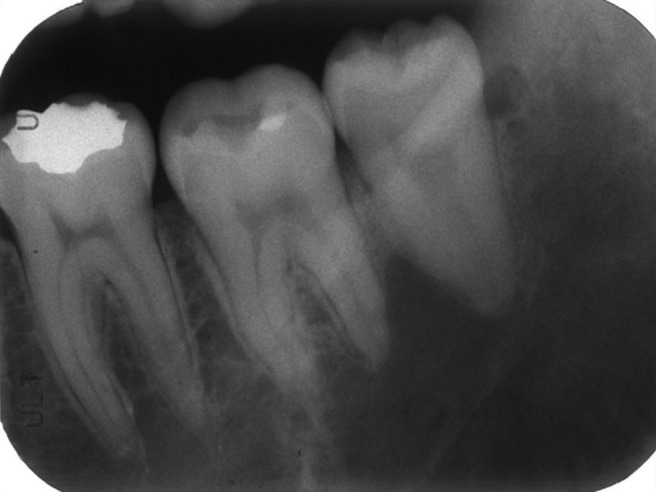
Intraoral radiograph shows deep invaginations toward the interalveolar septa and no displacement of the inferior mandibular canal. A small vesicular space appears in the cervical region, in contact with the distal surface of the left third molar tooth
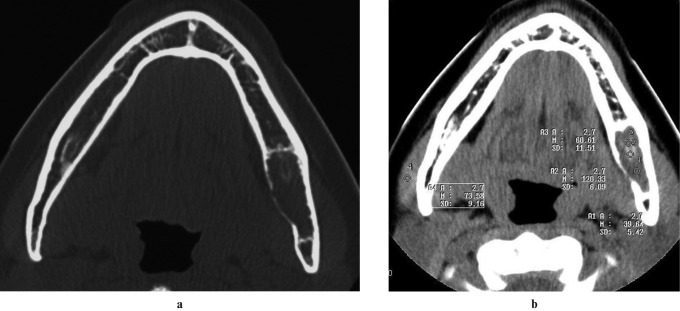
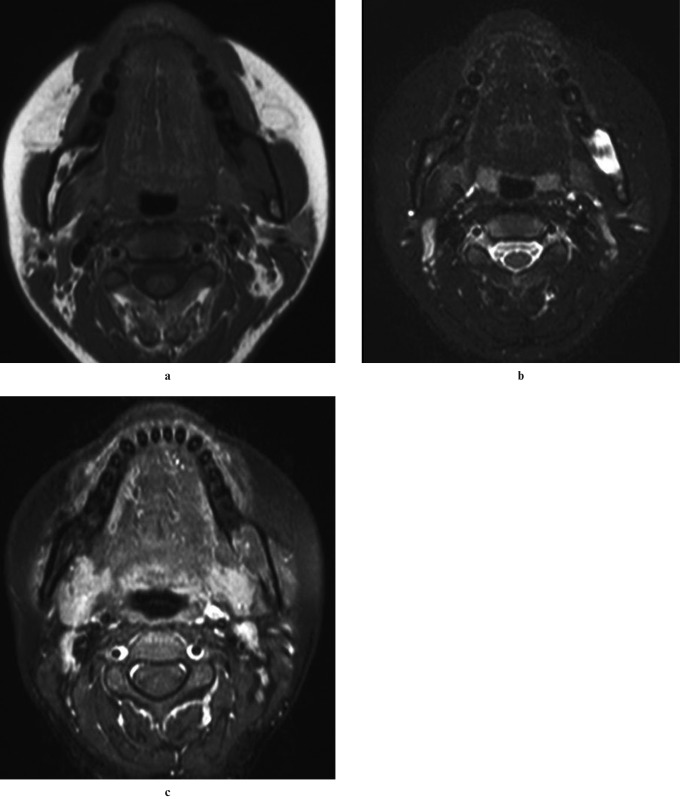
Conventional CT showed no destruction of the buccolingual cortical bone, but invasion of the internal surface of the cortical bone (Figure 3a). In axial section CT soft-tissue mode, three points of the lesion measured at random had CT values of 39 HU, 60 HU and 120 HU, compared with 73 HU for the masseter muscle (Figure 3b). Cone beam CT (CBCT) (Figure 4) was added to further evaluate the margin and interior of the lesion. This showed an irregular margin and sclerotic rim with no displacement of the inferior mandibular canal, and confirmed no calcification. On MRI, the interior of the lesion demonstrated well-defined low signal intensity on axial T1 weighted imaging (Figure 5a) and high signal intensity on axial short T1 inversion recovery (STIR) imaging (Figure 5b), and the margin showed enhancement on axial T1 weighted imaging after injection of diethylenetriamine-pentaacetic acid (Gd-DTPA) (Figure 5c).
Figure 3.
(a) CT showed no destruction of the buccolingual cortical bone, but invasion of the internal surface of the cortical bone. (b) CT appearance in soft-tissue mode. The CT value of various components of the lesion was 39 HU, 60 HU and 120 HU, compared with 73 HU for the masseter muscle
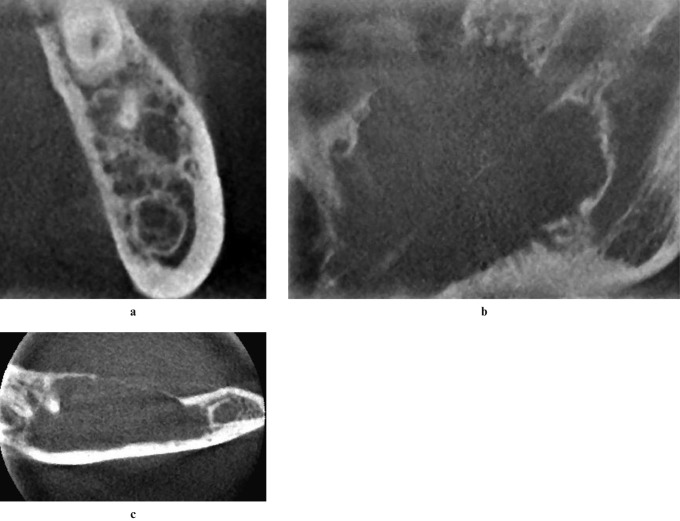
Figure 4.
(a) Cross-sectional cone beam CT image shows the lesion penetrating nearby bone tissue mesially. (b) Sagittal section cone beam CT shows irregular margin and sclerotic rim with no displacement of the inferior mandibular canal. (c) Axial section cone beam CT shows the interior to be homogeneous with no calcification, with thinning of the lingual cortex
Figure 5.
(a) The lesion demonstrated well-defined low signal intensity on axial T1 weighted imaging, time of repetition/time of echo (TR/TE): 579/10; (b) heterogeneously high signal intensity on STIR axial imaging, TR/TE: 3579/60 and (c) enhancement at the margin on axial T1 weighted imaging after injection of diethylenetriamine-pentaacetic acid (Gd-DTPA), TR/TE: 545/10
Visualization of the lesion on MRI made a fibro-osseous lesion unlikely. It was concluded from the imaging and clinical findings that the lesion was a benign tumour.
Therefore, 2 weeks after the initial visit, a biopsy specimen was obtained from the buccal aspect of the lower left third molar area, and histopathological examination revealed an ossifying fibroma (OF). After a further 5 weeks, the lesion was completely enucleated under general anaesthesia. The excised mass was a solid growth; the cut surface was white and had an hard, elastic consistency. Microscopically, the tumour was composed of cellular and collagenous fibrous stroma with spherical woven bone formation (Figure 6). The woven bone was lined by osteoblastic cells and equally distributed throughout the tumour. On the basis of clinical, radiological and pathological findings, the lesion was diagnosed as an OF. There was no evidence of recurrence at 2 years and 6 months after surgical excision.
Figure 6.
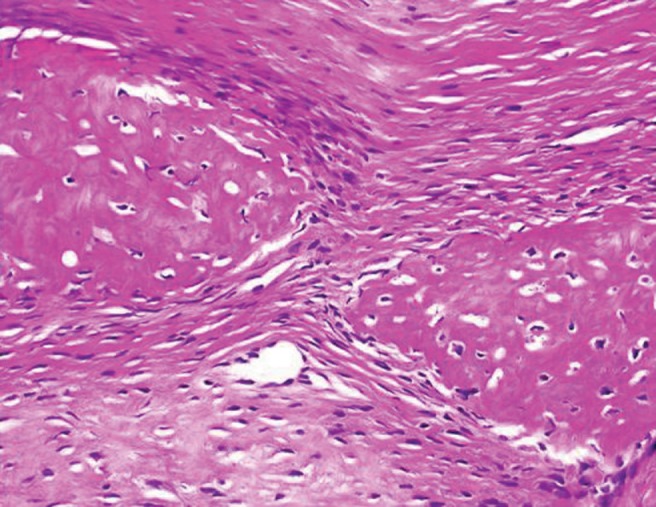
High-power view demonstrates the tumour to be composed of cellular and collagenous fibrous stroma with spherical woven bone. The woven bone is lined by osteoblastic cells and equally distributed throughout the tumour (haematoxylin–eosin stain; magnification 100×)
Discussion
Of all odontogenic tumours in the jaws, OF has the most variation in pattern.1,2 At its onset, OF often appears near the dental root. It is usually seen radiographically as a unilocular lesion with a well-defined, thinly corticated margin. Less commonly, it presents as a multilocular lesion and rarely as a mixed radiolucent–radiopaque structure with ill-defined, diffuse borders. The interior of an OF frequently shows minute calcification.1,3,5,6–8 Retrospective studies have shown that the radiographic appearance may be broadly divided into three types: radiolucent, mixed (mottled) and radiopaque.7–11
OF is essentially a benign tumour, but it often exhibits a similar radiographic and clinical appearance to fibrous dysplasia and osseous dysplasia.1,3,5 These lesions all arise from the periodontal membrane.1,6,9,12,13 OF has a clear female predilection and involves the mandible more often than the maxilla.1,4,6,8,9,11,12,14,15 It has its highest incidence in the third and fourth decades.1,3,6,10,14,15 Generally, the slower growing mature type of OF appears radiographically as a lesion with a mottled appearance, whereas fibrous dysplasia is similar in appearance but has a ground-glass pattern. Eversole et al6 studied 64 central OFs and divided them into 6 distinct radiographic patterns. Of these, 25 of the lesions with unilocular radiolucency arose at edentulous sites. However, many other lesions occur at edentulous sites, and this poses diagnostic problems in determining whether OF has recurred following surgical curettage or has subsequently developed after extraction of a tooth. The recurrence rate of OF after curettage was found to be 28%.6 In recent years, juvenile aggressive psammomatoid OF and juvenile trabecular OF have been included within histopathological classification category OF.9,16,17 They are uncommon, can grow rapidly and may recur after attempted excision. The patients are not always children. It is believed that they can be destructive locally18 or very aggressive.19–21 In addition, the irregular margin and no expansion with cortical bone of OF in this case may be a sign of an aggressive pattern.
In the present case, a radiolucent, multilocular pattern interposed between contiguous teeth was seen on panoramic tomography. In fact, the CT values of the lesion suggested that it was radiolucent with opaque foci. However, radiographic findings were inconclusive. Therefore, both benign and malignant lesions were considered in the differential diagnosis. The deep invaginations towards the interalveolar septa suggested a simple bone cyst; radiolucency and irregular margin pointed towards an odontogenic myxoma; and lack of expansion of cortical bone and absence of displacement of the inferior mandibular canal suggested a malignant lesion. It was very difficult to draw these divergent radiographic findings together. In this case, CT is very useful in the diagnosis as it gives more precise information about the internal structure and change in cortical bone. Both soft-tissue and bone modes can be used as the situation demands. CBCT has recently been used to evaluate the interior of bone tumours and other lesions.22–26 In the present case, the margin was irregular, the cortical bone was thinned on the lingual side but intact at the lower margin, and no displacement of the inferior mandibular canal was seen on CBCT images, whereas the front of the cross-section revealed an indented surface. These findings were valuable, as they enabled the anticipation of the consequences of a benign lesion. However, the calcification scattered through the lesion was not evident on CBCT and was confirmed only by soft-tissue mode CT. Confirmation of calcification was one of the deciding factors in the radiographic diagnosis of OF.
In conclusion, a 27-year-old woman presented with a painless swelling of the gingival aspect of the left mandibular third molar. Panoramic radiography showed a radiolucent lesion involving the root-apex area of the left lower second and third molars. CT was very useful in the radiographic differential diagnosis. CT gives precise information regarding the interior of such lesions and changes in the cortical bone, and soft tissue and bone modes can be used as the situation demands. Although CBCT is the best method of delineating intraosseous lesions with high resolution, it provides no detailed contrast between hard tissue and soft tissue. The authors believe that this is the crucial time to determine appropriate uses for medical CT and CBCT for lesions of the jaws.
References
- 1.Summerlin DJ, Tomich CE. Focal cemento-osseous dysplasia: a clinicopathologic study of 221 cases. Oral Surg Oral Med Oral Pathol 1994;78:611–620 [DOI] [PubMed] [Google Scholar]
- 2.Voytek TM, Ro JY, Edeiken J, Ayala AG. Fibrous dysplasia and cemento-ossifying fibroma. A histologic spectrum. Am J Surg Pathol 1995;19:775–781 [PubMed] [Google Scholar]
- 3.Su L, Weathers DR, Waldron CA. Distinguishing features of focal cemento-osseous dysplasia and cemento-ossifying fibromas. II. A clinical and radiologic spectrum of 316 cases. Oral Surg Oral Med Oral Pathol 1997;84:540–548 [DOI] [PubMed] [Google Scholar]
- 4.MacDonald-Jankowski DS. Focal cemento-osseous dysplasia: a systematic review. Dentomaxillofac Radiol 2008;37:350–360 [DOI] [PubMed] [Google Scholar]
- 5.Langlais RP, Langland OE, Nortje CH. Diagnostic imaging of the jaws. Baltimore: Williams & Wilkins, 1995 [Google Scholar]
- 6.Eversole LR, Merrell PW, Strub MA. Radiographic characteristics of central ossifying fibroma. Oral Surg Oral Med Oral Pathol 1985;59:522–527 [DOI] [PubMed] [Google Scholar]
- 7.Mintz S, Velez I. Central ossifying fibroma: an analysis of 20 cases and review of the literature. Quintessence Int 2007;38:221–227 [PubMed] [Google Scholar]
- 8.Waldron CA, Giansanti JS. Benign fibro-osseous lesions of the jaws: a clinical-radiologic histologic review of sixty-five cases. Part II. Benign fibro-osseous lesions of periodontal ligament origin. Oral Surg Oral Med Oral Pathol 1973;35:340–350 [DOI] [PubMed] [Google Scholar]
- 9.Sciubba JJ, Fantasia JE, Kahn LB. Atlas of tumor pathology, tumors and cysts of the jaw. Washington: Armed Forces Institute of Pathology, 2001, pp 141–160. [Google Scholar]
- 10.Chang CC, Hung HY, Chang JY, Yu CH, Wang YP, Liu BY, et al. Central ossifying fibroma: a clinicopathologic study of 28 cases. J Formos Med Assoc 2008;107:288–294 [DOI] [PubMed] [Google Scholar]
- 11.White SC, Pharoah MJ. Diseases of bone manifested in the jaws. In: White SC, Pharoah MJ.(eds).Oral radiology: principles and interpretation (5th edn) St Louis: Mosby Inc., 2001, pp485#x2013;515 [Google Scholar]
- 12.Eversole LR, Leider AS, Nelson K. Ossifying fibroma: a clinicopathologic study of sixty-four cases. Oral Surg Oral Med Oral Pathol 1985;60:505–511 [DOI] [PubMed] [Google Scholar]
- 13.Hamner JE, Scofield HH, Cornyn J. Benign fibro-osseous jaw lesions of periodontal membrane origin: analysis of 249 cases. Cancer 1968;22:861–878 [DOI] [PubMed] [Google Scholar]
- 14.MacDonald-Jankowski DS. Cemento-ossifying fibromas in the jaws of Hong Kong Chinese. Dentomaxillofac Radiol 1998;27:298–304 [DOI] [PubMed] [Google Scholar]
- 15.Vegas BE, Gargallo AJ, Berini AL, Gay EC. Benign fibro-osseous lesions of the maxillas: analysis of 11 cases. Med Oral Patol Oral Cir Bucal 2008;13:E653–656 [PubMed] [Google Scholar]
- 16.Barnes L, Eveson JW, Reichart P, Sidransky D. Ossifying fibroma. In: Slootweg PJ, El Mofty SK ,(eds). World Health Organization classification of tumors. Lyon: IARC Press, 2005, pp 319–322 [Google Scholar]
- 17.El-Mofty S. Psammomatoid and trabecular juvenile ossifying fibroma of the craniofacial skeleton: two distinct clinicopathologic entities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:296–304 [DOI] [PubMed] [Google Scholar]
- 18.Brademann G, Werner JA, Janig U, Mehdorn HM, Rudert H. Cemento-ossifying fibroma of the petromastoid region: case report and review of the literature. J Laryngol Otol 1997;111:152–155 [DOI] [PubMed] [Google Scholar]
- 19.Wenig BM, Vinh TN, Smirniotopoulos JG, Fowler CB, Houston GD, Heffner DK. Aggressive psammomatoid ossifying fibromas of the sinonasal region: a clinicopathologic study of a distinct group of fibro-osseous lesions. Cancer 1995;76:1155–1165 [DOI] [PubMed] [Google Scholar]
- 20.Bowyer JD, Majid MA, Ah-Fat F, Kaye BS, Kokai GK, May PL, et al. Giant cemento-ossifying fibroma of the maxilla causing proptosis in a young patient. J Pediatr Ophthalmol Strabismus 2001;38:359–362 [DOI] [PubMed] [Google Scholar]
- 21.Smith SF, Newman L, Walker DM, Papadopoulos H. Juvenile aggressive psammomatoid ossifying fibroma: an interesting, challenging, and unusual case report and review of the literature. J Oral Maxillofac Surg 2009;67:200–206 [DOI] [PubMed] [Google Scholar]
- 22.Araki M, Hashimoto K, Kawashima S, Matsumoto K, Akiyama Y. Radiographic features of enostosis determined with limited cone beam computed tomography in comparison with rotational panoramic radiography. Oral Radiol 2006;22:28–34 [Google Scholar]
- 23.Hashimoto K, Kawashima S, Araki M, Iwai K, Sawada S, Akiyama Y. Comparison of image performance between cone-beam computed tomography for dental use and four-row multidetector helical CT. J Oral Sci 2006;48:27–34 [DOI] [PubMed] [Google Scholar]
- 24.Hashimoto K, Arai Y, Iwai K, Araki M, Kawashima S, Terakado M. A comparison of a new limited cone beam computed tomography machine for dental use with a multidetector row helical CT machine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:371–377 [DOI] [PubMed] [Google Scholar]
- 25.Araki M, Kameoka S, Mastumoto N, Komiyama K. Usefulness of cone-beam CT for odontogenic myxoma. Dentomaxillofac Radiol 2007;36:423–427 [DOI] [PubMed] [Google Scholar]
- 26.Terakado M, Hashimoto K, Arai Y, Honda M, Sekiwa T, Sato H. Diagnostic imaging with newly-developed ortho cubic super high resolution CT (ortho-CT). Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;89:509–518 [DOI] [PubMed] [Google Scholar]