Abstract
Objectives
As a first step in developing a protocol for multidimensional sialography using cone beam CT (CBCT), the objective of this study was to compare the effective radiation doses from sialography of the parotid and submandibular glands using plain radiography and CBCT.
Methods
The effective doses were calculated from dose measurements made at 25 selected locations in the head and neck of a radiation analogue dosimeter (RANDO) phantom, using International Commission on Radiological Protection 2007 tissue weighting factors.
Results
The effective dose (E) changed in relationship to changes in CBCT field of view (FOV), peak kilovoltage (kVp) and milliamperage (mA). Specifically, E decreased from a maximum of 932 μSv (30 cm FOV, 120 kVp, 15 mA) to 60 μSv (15 cm FOV, 80 kVp, 10 mA) for a parotid gland study and to 148 μSv (15 cm FOV, 80 kVp, 10 mA) for a submandibular study. The collective series of plain radiographs made during sialography of the parotid and submandibular glands yielded effective doses of 65 μSv and 156 μSv, respectively. The plain parotid gland series included one panoramic, two anterior–posterior skull and four lateral skull radiographs, whereas the submandibular gland series included one panoramic, one standard mandibular occlusal and four lateral skull radiographs.
Conclusion
The effective doses from CBCT examinations centred on the parotid and submandibular glands were similar to those calculated for plain radiograph sialography when a 15 cm FOV was chosen in combination with exposure conditions of 80 kVp and 10 mA.
Keywords: cone beam computed tomography, sialography, radiation dosimetry
Introduction
Imaging of the major salivary glands is performed using one of four techniques: sialography, ultrasound, CT or MRI. Of these methods, sialography has proven to be the most effective technique to assess salivary gland function, and obstructive conditions of the salivary glands in particular.1 Sialography was first performed in 1902,2 and depicts the ductal structures of the salivary glands following the introduction of a contrast agent into the orifice of a salivary gland duct.
Sialography is largely dependent on the imaging modality to which it is coupled. Traditionally, sialo-graphy has been combined with plain radiographs, and this has since become the gold standard with which all other imaging techniques are compared.3 More recently, three-dimensional (3D) depictions of gland ductal anatomy have been possible by combining sialography with CT or MRI, but these investigations have several limitations including cost and accessibility. Also, in the case of MRI and single-row CT, prolonged imaging times may cause visualization of the uptake of contrast material to be missed owing to its rapid clearance from the gland.4
Today, the rapid acquisition of a 3D image volume using cone beam CT (CBCT) has enabled us to overcome the temporal limitations of medical CT and MRI image acquisition. CBCT promises to revolutionize the practice of oral and maxillofacial radiology by offering major advantages such as short scan times and less dose to the patient.5 Consequently, it has found several applications in the field of dentistry, such as localization of impacted teeth and imaging of the temporomandibular joint.6,7 Imaging of the major salivary glands, however, is one application that has not yet been explored.
As a first step in developing a protocol for 3D CBCT sialography, we conducted a dose assessment study comparing this novel methodology with conventional two-dimensional (2D) plain radiography sialography. Dosimetry studies are especially crucial when the head and neck area is being examined because of the number of critically radiosensitive organs in the field being imaged.
Materials and methods
A head and neck RANDO (radiation analogue dosimeter) Alderson phantom (Alderson Research Laboratories, Stanford, CT) was used in this study. The phantom is a human skull covered with isocyanate rubber which has tissue radiation attenuation characteristics equivalent to human soft tissues with respect to both atomic number and tissue density.8 Only the first 10 axial slices, each 2.5 cm in thickness, of the phantom extending from the top of the head to the level of the clavicles were used. Following the methods of Ludlow et al,9 the absorbed radiation dose was measured at 25 selected locations that represent critical radiosensitive organs and sites of special interest to dental imaging (Table 1).
Table 1. Locations of the thermoluminescent dosimeter chips in the radiation analogue dosimeter (RANDO) phantom based on organ of interest.
| Organ | Location | Phantom level |
| Brain | Pituitary fossa | 3 |
| Mid-brain | 2 | |
| Eyes | Right/left orbit | 4 |
| Right/left eye lens | 4 | |
| Salivary glands | Right/left parotid | 6 |
| Right/left submandibular | 7 | |
| Right/left sublingual | 7 | |
| Thyroid | Surface | 9 |
| Midline | 9 | |
| Pharynx | Pharynx | 9 |
| Bone marrow | Calvarium anterior | 2 |
| Calvarium posterior | 2 | |
| Calvarium left | 2 | |
| Cervical spine | 6 | |
| Right/left mandibular body | 7 | |
| Right/left ramus | 6 | |
| Skin | Right cheek | 5 |
| Left back of neck | 7 |
Lithium fluoride thermoluminescent dosimeter (TLD-100) chips (3 × 3 × 1 mm) were used to record the absorbed dose at the 25 locations (Global Dosimetry Solutions Inc., Irvine, CA). Unexposed dosimeter chips were also analysed for environmental calibration during each exposure of the phantom. Each measurement was made in triplicate.
Imaging was performed with the Hitachi CB MercuRay system (Hitachi Medical Systems, Tokyo, Japan). The phantom was orientated in the unit with the left parotid or submandibular salivary gland centred in the image field. The images were acquired using three fields of view (FOV) (30 cm, 23 cm and 15 cm), three peak kilovoltage (kVp) settings (120 kVp, 100 kVp and 80 kVp) and two milliamperage (mA) settings (15 mA and 10 mA).
The number of plain radiographs made for a sialography series varied depending on the gland being imaged. Parotid gland examinations included one panoramic radiograph, two anterior–posterior skull radiographs and four lateral skull radiographs. For the submandibular gland, the anterior–posterior views were omitted and replaced with one pre-operative standard mandibular occlusal radiograph. The panoramic radiographs were made with the Sirona OrthophosDS (Sirona, Munich, Germany) at 60 kVp and 14 mA using Kodak Lanex Medium intensifying screens and Kodak T-Mat G panoramic film (Eastman Kodak Co., Rochester, NY). The occlusal radiographs were exposed using the S.S. White Spacemaker radiographic unit (S.S. White, Philadelphia, PA) at 70 kVp, 8 mA and 0.32 s using Kodak Ultraspeed (Eastman Kodak Co., Rochester, NY). For the skull radiographs, the Kodak DirectView CR850 PSP system (Kodak Medical Systems, Rochester, NY) was used, and the exposure parameters were 70 kVp and 15 mA. For the parotid gland, the exposure time was 0.8 s, and for the submandibular gland the exposure time was 0.5 s.
For each radiographic examination or series, the effective dose (E) was calculated based on the following equation:10
where WT is the weighting factor for tissue T, the sum over all tissues ΣWT = 1, HT is the equivalent dose to tissue T in μSv, DT is the average absorbed dose in the volume of tissue T and FT is the fraction of tissue type T irradiated in that view.
Tissue weighting factors were based on the recent International Commission on Radiological Protection (ICRP) 2007 recommendation in publication 103.11 The average absorbed dose was calculated as a mean of three independent measurements at the 25 sites in the tissues or organs of interest. Additionally, the FT irradiated within each FOV was estimated (Table 2), and included in the calculation of E, as proposed by Ludlow et al.9
Table 2. Estimated percentages of the proportion of tissue irradiated based on the volume of that tissue in the image field.
| 30 cm FOV | 23 cm FOV | 15 cm FOV, parotid | 15 cm FOV, submandibular | Plain radiography, parotid | Plain radiography, submandibular | |
| Thyroid | 100 | 80 | 20 | 100 | 100 | 100 |
| Oesophagus | 10 | 5 | 2.5 | 10 | 10 | 10 |
| Bone surface | 16.5 | 11 | 8.25 | 4.5 | 11 | 4.5 |
| Bone marrow | 16.5 | 11 | 8.25 | 4.5 | 11 | 4.5 |
| Salivary gland | 100 | 100 | 100 | 100 | 100 | 100 |
| Skin | 5 | 3 | 2.5 | 2.5 | 3 | 2.5 |
| Brain | 100 | 50 | 10 | 5 | 50 | 10 |
| Remainder | 20 | 15 | 10 | 10 | 15 | 10 |
Results
The effective dose (E) changed in relationship to changes in FOV, kVp and mA for CBCT. Specifically, E decreased from 466 μSv for the largest 30 cm FOV to 97 μSv for the smallest 15 cm FOV, when kVp and mA were held constant at 100 kVp and 10 mA. When kVp was decreased from 120 kVp to 100 kVp, E also decreased from 932 μSv to 683 μSv when the FOV and mA were held constant at 30 cm and 15 mA. Lastly, when mA was decreased from 15 mA to 10 mA, E decreased as well from 435 μSv to 275 μSv. Of note is that exposure time for the CB MercuRay is constant at 10 s. More importantly, E calculated for the collective series of plain radiographs made during sialography of the parotid and submandibular glands was similar to the E for CBCT examinations centred on the same glands when the 15 cm FOV was used in combination with 80 kVp, 10 mA. These results are summarized in Figures 1 and 2, which demonstrate the variability for each individual radiographic technique.
Figure 1.
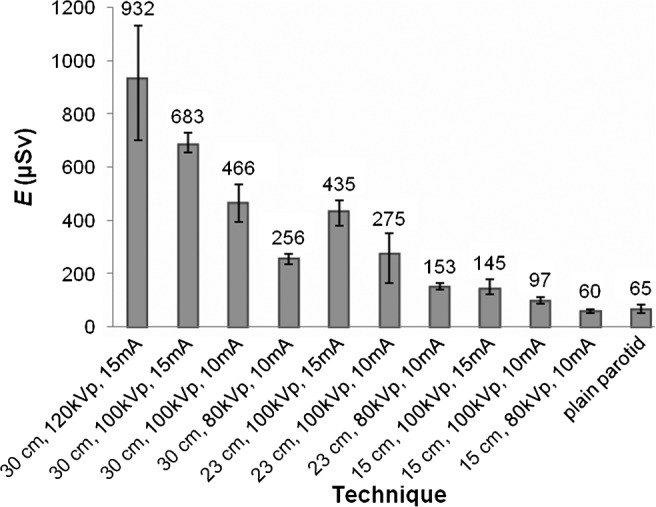
Variation of effective dose, E, with different fields of view (FOV) size, milliamperage (mA) and peak kilovoltage (kVp) settings. This graph compares E for the different cone beam CT techniques that were centred on the left parotid gland with the E calculated for the collective plain radiographs made during a sialography procedure of the same gland. The plain radiographs included one panoramic radiograph, two anterior–posterior skull radiographs and four lateral skull radiographs
Figure 2.

Variation of effective dose, E, with different fields of view (FOV) size, milliamperage (mA) and peak kilovoltage (kVp). In this graph, the effective doses for the 30 cm FOV, 23 cm FOV and 15 cm FOV cone beam CT examinations centred over the left submandibular gland are compared with E for the collective series of plain radiographs made during sialography of the same gland. The plain radiograph series included one panoramic radiograph, one mandibular standard occlusal and four lateral skull radiographs
The reproducibility of the TLD readings was assessed by computing the coefficient of variation; an example of these results is presented for the 30 cm FOV, 80 kVp and 10 mA setting in Table 3.
Table 3. Reproducibility of the thermoluminescent dosimeter (TLD) chip measurements based on a 30 cm field of view, 80 kVp and 10 mA.
| Reading 1 | Reading 2 | Reading 3 | SD | Mean | CV | |
| Thyroid midline | 3.2 | 2.63 | 2.89 | 0.29 | 2.91 | 10% |
| Thyroid surface | 2.42 | 2.37 | 2.59 | 0.12 | 2.46 | 5% |
| Oesophagus | 2.76 | 2.29 | 2.66 | 0.25 | 2.57 | 10% |
| Right mandibular body | 2.37 | 2.45 | 1.70 | 0.41 | 2.17 | 19% |
| Left mandibular body | 1.82 | 1.81 | 1.32 | 0.29 | 1.65 | 17% |
| Right ramus | 2.57 | 2.73 | 2.11 | 0.32 | 2.47 | 13% |
| Left ramus | 2.60 | 2.62 | 2.13 | 0.28 | 2.45 | 11% |
| Cervical spine | 1.79 | 1.73 | 1.75 | 0.03 | 1.76 | 2% |
| Anterior calvarium | 2.10 | 1.63 | 1.54 | 0.30 | 1.76 | 17% |
| Posterior calvarium | 1.29 | 1.26 | 1.38 | 0.06 | 1.31 | 5% |
| Left calvarium | 1.51 | 2.04 | 1.98 | 0.29 | 1.84 | 16% |
| Right parotid gland | 2.19 | 2.43 | 3.01 | 0.42 | 2.54 | 17% |
| Left parotid gland | 3.07 | 3.04 | 3.28 | 0.13 | 3.13 | 4% |
| Right submandibular gland | 2.32 | 2.29 | 2.27 | 0.03 | 2.29 | 1% |
| Left submandibular gland | 1.83 | 2.20 | 1.98 | 0.19 | 2.00 | 9% |
| Right sublingual gland | 2.40 | 2.39 | 2.18 | 0.12 | 2.32 | 5% |
| Left sublingual gland | 2.24 | 2.31 | 2.17 | 0.07 | 2.24 | 3% |
| Neck | 2.05 | 3.05 | 3.31 | 0.52 | 3.47 | 15% |
| Cheek | 2.78 | 2.47 | 2.63 | 0.16 | 2.63 | 6% |
| Right lens | 3.32 | 3.43 | 3.58 | 0.13 | 3.44 | 4% |
| Left lens | 3.2 | 3.23 | 2.92 | 0.17 | 3.12 | 5% |
| Pituitary fossa | 1.72 | 1.64 | 1.52 | 0.10 | 1.63 | 6% |
| Mid-brain | 1.47 | 1.21 | 1.58 | 0.19 | 1.42 | 13% |
| Right orbit | 2.29 | 2.38 | 2.29 | 0.05 | 2.32 | 2% |
| Left orbit | 1.93 | 2.44 | 1.67 | 0.39 | 2.01 | 19% |
| Mean CV | 9% |
CV, coefficient of variation.
Discussion
The potential radiation hazard from low doses of radiation associated with diagnostic investigations remains a major concern for both radiologists and patients alike. In the oral and maxillofacial region, this is especially true because of the radiosensitive organs in the area being imaged, and because of sporadic reports that implicate oral and maxillofacial radiography with intracranial diseases.12 In a population-based case–control study, Longstreth et al12 found that more than five full-mouth series (10–22 images) performed during a lifetime doubled the risk of development of intracranial meningioma. Consequently, healthcare providers, including oral and maxillofacial radiologists, are constantly developing new technologies and protocols to address the radiation dose concerns of patients without compromising diagnostic quality or patient care.
This study is a first step in the development and application of a novel, potentially improved technique for sialography. The overall goal of our work is to modulate radiation doses to levels that would be similar to those arising from plain radiography sialography, without compromising the quality of the CBCT images. Using TLD measurements on a RANDO phantom, the dependence of effective radiation doses on the exposure factors was estimated for CBCT examinations.
The Hitachi CB MercuRay system allows several technical factors to be controlled by the operator. Holding all other technical factors constant, the effect of varying an individual factor on the effective radiation dose was explored. Reducing the FOV from the larger size to the next available smaller size resulted in a significant reduction in the calculated E by approximately 40%. This reduction is due to some of the TLDs no longer being in the primary radiation field; some of the reduction in E may also be due to elimination of scatter radiation. Likewise, reducing mA from 15 mA to 10 mA resulted in a 37% reduction, as is expected because of the reduced output from the X-ray tube. Finally, E decreased by approximately 30% and 60% when the kVp setting was reduced from 120 kVp to 100 kVp and 80 kVp, respectively. These general findings are in agreement with the results of other published studies.9,13 The significance of these reductions in effective dose, however, is meaningful only if the image quality is not compromised because, as the amount of radiation decreases, the amount of noise increases. This trade-off between amount of radiation and image quality will be addressed in a future study as a next step in the process of developing a new protocol for sialography using CBCT.
The study by Palomo et al,13 like the present study, examined the influence of different CBCT settings on the effective radiation dose using a RANDO phantom and the CB MercuRay CBCT unit. These authors noted a dose reduction of 5–10% to the tissues that remained in the path of the direct beam as the FOV decreased from 30 cm to 23 cm and 15 cm. They also achieved a 38% reduction in the effective dose by reducing the kVp from 120 to 100. Milliamperage settings varied markedly (2, 5, 10 and 15) and produced a linear and exponential pattern of dose reduction in the same study. Consistently, altering the technical parameters significantly reduced the radiation dose, and certainly altering these technical factors should be considered to maintain patient radiation doses as low as reasonably achievable.
Our results are consistent with other dosimetry studies.9,13 Some of the differences we report in E are probably related to variations in the methodology of measuring the absorbed dose and in the calculations of effective dose. Two prominent differences in the methodology are the centring of the image field that we used as well as the number of times a single TLD chip was exposed. In the current study, the image field was asymmetrically centred on the salivary gland of interest (either the left parotid or left submandibular). In previous studies, the image field was centred in the midline of one or both jaws.9,13,14 Because this study is the first of its kind to calculate the effective dose for a specific application of CBCT, imaging the major salivary glands, we believed it to be more appropriate to localize the image field where we did. We firmly believe that this technical modification has led to a more accurate estimate of E for CBCT examinations of the parotid and submandibular glands.
Regarding the number of exposures, the TLD chips in the present study were exposed only once, as was done in the study by Paloma et al.13 In most other similar studies the TLD chips were exposed a minimum of three times, after which the measured absorbed doses were divided by the number of exposures.5,9,14 We believe that exposing the TLD chips only once allowed for a more realistic simulation of the patient situation as patients will undergo only one CBCT scan during the procedure. It also allowed us to truly examine the reproducibility of the dose measurement, which was determined by calculating the coefficient of variation, the mean of which was calculated to 9% for the 30 cm FOV, 80 kV and 10 mA CBCT.
The effective dose was calculated according to the ICRP definition but, as per Ludlow et al,9 it was necessary to estimate the fraction of irradiated tissue in each FOV. A unique feature of this study is that the effect of the variation in the percentage contribution of each tissue with changes in the FOV and image field centre was taken into account. For example, the fraction of brain irradiated in the 30 cm FOV centred on the left parotid gland was 100%, but decreased to 50% in the 23 cm FOV and decreased even further to 10% in the smallest 15 cm FOV. On the other hand, it was estimated that only 5% of the brain was irradiated in the 15 cm FOV when the FOV was centred on the submandibular gland. Tailoring the FOV centre for this imaging task and for each FOV may have yielded more meaningful dose results.
The calculated thyroid E was by far the largest contributor to the overall E in all examinations centred on the submandibular gland, whether using CBCT or plain radiography as the imaging modality. In fact, the E calculated for the thyroid contributed 71% and 76% of the total E for CBCT and plain radiograph examinations, respectively, when centred on the submandibular salivary gland. Because of the anatomical proximity of the two glands, it is inevitable that the thyroid will receive a higher radiation dose during examinations of the submandibular gland. This may be a source of concern because of the relative high radiosensitivity of the thyroid, especially in children. Fortunately, obstructive conditions of the salivary glands are very rare in children and adolescents,15 and it is unlikely that an individual from that age group will require a sialogram procedure. As for the risk of thyroid cancer in adults from diagnostic radiation exposure, the data are still inconclusive and no studies have been able to prove a causal relationship or even a statistically significant association.16,17 Nevertheless, the inconclusive nature of the data creates a dilemma for physicians and dentists interested in imaging the submandibular gland. This dilemma is an excellent example of where risk vs benefit judgment comes into play; that is, the excess risk of imaging vs the anticipated benefit in terms of improved patient care and management. Other tissues that contributed significantly to the overall calculated E, especially in examinations centred on the parotid gland, were the salivary glands and bone marrow.
Based on the findings of this study, a preliminary protocol for CBCT sialography has been developed. Following the introduction of radiographic contrast, a lateral skull plain image is made to ensure adequate filling of the gland with contrast material. This is then followed by CBCT image acquisition using the 15 cm FOV and X-ray tube factors of 80 kVp and 10 mA. After the completion of the CBCT scan, another lateral skull plain radiograph is made 5 min after removal of the catheter to assess contrast material clearance as this is regarded as an indirect indicator of gland function and saliva production. The two lateral skull radiographs were made with the Kodak DirectView CR850 PSP system using 70 kVp, 15 mA and 0.8 s exposure time. One of the initial cases performed according to this protocol is presented in Figure 3. The CBCT images demonstrate the secondary gland structure of the submandibular gland that is not readily apparent on the 2D conventional plain image owing to extravasation of contrast material into the gland capsule.
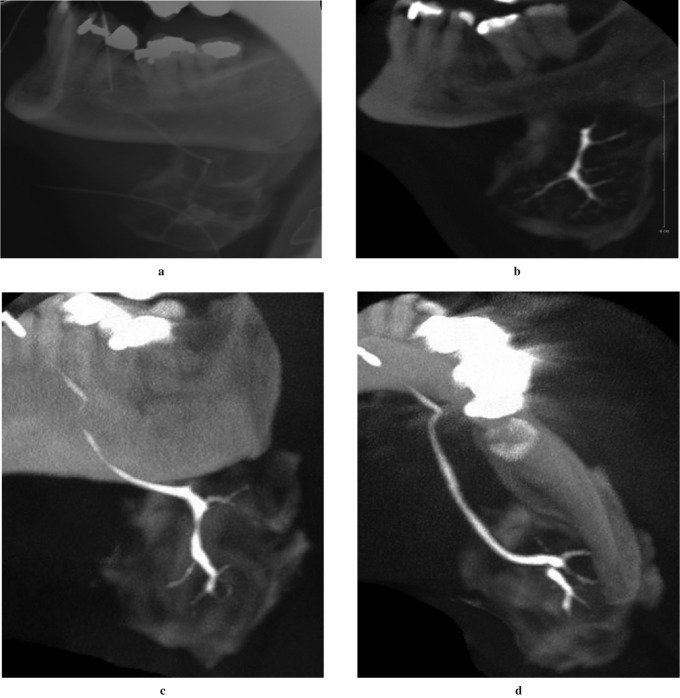
Figure 3.
Sialogram of the left submandibular gland using the proposed preliminary protocol detailed earlier. (a) Lateral skull plain radiograph of the gland following contrast administration. This image was made prior to the cone beam CT (CBCT) scan to ensure adequate fill of the gland with contrast material, and it demonstrates the lack of visibility of the secondary and tertiary ductal structures due to extravasation of the contrast material into the gland capsule. (b) Reformatted sagittal CBCT image of the same gland with the secondary and tertiary ducts clearly visible. Maximum intensity projection (MIP) CBCT images (c) in the coronal plane and (d) in the axial plane demonstrating the three-dimensional and multiplanar capabilities of CBCT. The CBCT images were acquired with the 15 cm FOV centred on the left submandibular gland and using X-ray tube factors of 80 kVp and 10 mA
In conclusion, the calculated effective doses from CBCT examinations centred on the parotid and submandibular glands were comparable to the E from plain radiograph sialography of the same glands when a smaller FOV was chosen in combination with lower kVp and mA settings (15 cm FOV, 80 kVp, 10 mA). Having acquired the dosimetric data for site-specific imaging using CBCT, a future goal is to optimize the exposure parameters for CBCT sialography by proposing kVp and mA settings for the CB MercuRay unit that will balance the signal-to-noise ratio of the images and the radiation dose to the patient.
Acknowledgments
The authors wish to thank Ms Virgilia Porretta, Ms Andrea Welsh and Ms Nancy Gow for their help with the technical aspect of this study. This work was supported by a Connaught Foundation Grant from the University of Toronto to EWNL.
References
- 1.Jager L, Menauer F, Holzknecht N, Scholz V, Grevers G, Reiser M. Sialolithiasis: MR sialography of the submandibular duct – an alternative to conventional sialography and US? Radiology 2000;216:665–671 [DOI] [PubMed] [Google Scholar]
- 2.Benson BW. Salivary gland radiology. In: White SC, Pharoah MJ. (eds).Oral radiology: principles and interpretation (6th edn) St. Louis, MO: Mosby, 2009, pp 578–598 [Google Scholar]
- 3.Varghese JC, Thornton F, Lucey BC, Walsh M, Farrell MA, Lee MJ. A prospective comparative study of MR sialography and conventional sialography of salivary duct disease. AJR Am J Roentgenol 1999;173:1497–1503 [DOI] [PubMed] [Google Scholar]
- 4.Szolar DH, Groell R, Braun H, Preidler K, Stiskal M, Kern R, et al. Ultrafast computed tomography and three-dimensional image processing of CT sialography in patients with parotid masses poorly defined by magnetic resonance imaging. Acta Otolaryngol 1996;116:112–118 [DOI] [PubMed] [Google Scholar]
- 5.Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;106:106–114 [DOI] [PubMed] [Google Scholar]
- 6.Liu DG, Zhang WL, Zhang ZY, Wu YT, Ma XC. Localization of impacted maxillary canines and observation of adjacent incisor resorption with cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:91–98 [DOI] [PubMed] [Google Scholar]
- 7.White SC. Cone-beam imaging in dentistry. Health Phys 2008;95:628–637 [DOI] [PubMed] [Google Scholar]
- 8.Schulze D, Heiland M, Thurmann H, Adam G. Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems and conventional radiography. Dentomaxillofac Radiol 2004;33:83–86 [DOI] [PubMed] [Google Scholar]
- 9.Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol 2006;35:219–226 [DOI] [PubMed] [Google Scholar]
- 10.ICRP publication 60: 1990 Recommendations of the International Commission on Radiological Protection, 60. Ann ICRP 1991;21:1–201 [PubMed] [Google Scholar]
- 11.ICRP publication 103: 2007 Recommendations of the International Commission on Radiological Protection. Ann ICRP 2007;37:1–332 [DOI] [PubMed] [Google Scholar]
- 12.Longstreth WT, Jr, Phillips LE, Drangsholt M, Koepsell TD, Custer BS, Gehrels JA, et al. Dental X-rays and the risk of intracranial meningioma: a population-based case-control study. Cancer 2004;100:1026–1034 [DOI] [PubMed] [Google Scholar]
- 13.Palomo JM, Rao PS, Hans MG. Influence of CBCT exposure conditions on radiation dose. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:773–782 [DOI] [PubMed] [Google Scholar]
- 14.Hirsch E, Wolf U, Heinicke F, Silva MA. Dosimetry of the cone beam computed tomography Veraviewepocs 3D compared with the 3D Accuitomo in different fields of view. Dentomaxillofac Radiol 2008;37:268–273 [DOI] [PubMed] [Google Scholar]
- 15.Bodner L, Fliss DM. Parotid and submandibular calculi in children. Int J Pediatr Otorhinolaryngol 1995;31:35–42 [DOI] [PubMed] [Google Scholar]
- 16.Hallquist A, Nasman A. Medical diagnostic X-ray radiation: an evaluation from medical records and dentist cards in a case-control study of thyroid cancer in the northern medical region of Sweden. Eur J Cancer Prev 2001;10:147–152 [DOI] [PubMed] [Google Scholar]
- 17.Wingren G, Hallquist A, Hardell L. Diagnostic X-ray exposure and female papillary thyroid cancer: a pooled analysis of two Swedish studies. Eur J Cancer Prev 1997;6:550–556 [DOI] [PubMed] [Google Scholar]