Abstract
Objectives
The purpose of this study was to compare the diagnostic accuracy of cone beam CT (CBCT) with that of conventional dental radiography in the detection of root fractures and to evaluate the influence of root canal fillings on root fracture detection.
Methods
We investigated 128 patients with clinically suspected root fractures in 135 teeth. These patients underwent conventional dental radiography, CBCT and eventually surgical exploration. Among the 135 teeth, 86 were non-endodontically treated teeth and 49 were endodontically treated teeth. Two oral radiologists independently analysed the dental radiographs and CBCT images of each patient and reached a consensus. The CBCT findings of root fractures were set as the detection of a separation of the adjacent root segments on at least two contiguous sections and on at least two of the three-dimensional (3D) planes.
Results
Root fracture was intraoperatively detected in 95 of the 135 teeth. The sensitivity and specificity of root fractures diagnosed on the basis of the consensus between the 2 evaluators were 26.3% and 100%, respectively, for dental radiography and 89.5% and 97.5%, respectively, for CBCT. CBCT was significantly more accurate than dental radiography in detecting root fractures (P < 0.001). The sensitivity of CBCT was reduced in the presence of root canal fillings but its specificity remained unaffected. Both the sensitivity and specificity of dental radiography were not influenced by the presence of root canal fillings.
Conclusions
CBCT appears to be more accurate than conventional dental radiography in the detection of root fractures.
Keywords: cone-beam computed tomography, dental radiography, diagnosis, dental root fracture
Introduction
The definitive diagnosis of dental root fractures is a challenge encountered in clinical practice. Often these fractures extend through the pulp to the periodontal ligament.1 In the majority of cases, the diagnosis is suspected only when a combination of the following symptoms or signs is observed: pain, local swelling, mobility of the tooth, periodontal pocket, sinus tract, abscess or sensitivity to palpation or percussion.2 The prognosis of teeth with extensive root fracture is poor, and in many cases extraction is the only possible treatment option. Therefore, accurate diagnosis is essential to avoid unnecessary and inappropriate treatment.3 Approximately one-quarter2 to one-third4 of fracture lines may be directly visualized on conventional dental radiographs. Conventional CT is superior to dental radiography and may detect 70% of the fractures.2 However, the higher cost and radiation dose associated with conventional CT outweigh these advantages in the light of endodontic practice.5,6 Cone-beam CT (CBCT) involves lesser radiation dose and yields higher spatial resolution than conventional CT. Prototype local CT systems, flat-panel detector CBCT systems that are used to scan ex vivo samples, are found to be valuable for detecting root fractures,7,8 but they cannot be used to scan patients. Clinical dental CBCT systems appear to be superior to conventional dental radiography in detecting artificially created root fractures.9 However, these findings have not been verified in clinical studies on large patient populations.
The purpose of this clinical study was to compare the accuracy of a clinical CBCT system with that of conventional dental radiography in detecting root fractures in untreated and endodontically treated teeth and to analyse the influence of root canal fillings on detecting root fractures by the two diagnostic modalities.
Materials and methods
Dental periapical radiographs and CBCT images of 135 teeth from 128 patients who were clinically suspected to have root fractures were acquired and analysed. Within 28 months of acquiring the images, these patients were referred to our department by endodontists or periodontists to confirm the presence of a root fracture using CBCT. Thereafter, these patients underwent surgical intervention for the treatment of the affected teeth (namely extraction, amputation or root-end resection). For all the teeth, the initial dental radiographs had been reviewed and the necessity of CBCT scans had been justified. Cases of root fractures that might be related to acute trauma were excluded and teeth for which surgical intervention was not attempted during this period were excluded. The 128 patients included 68 males and 60 females, with a median age of 45 years (range: 22–82 years). Among the 135 teeth involved, 86 were non-endodontically treated and 49 were endodontically treated (with root canal fillings). The main clinical signs included pain on mastication or percussion, periodontal pockets, sinus tracts and an inconsistency in the electronic and radiological determination of the working length. This study was approved by our institutional review board.
The CBCT images were acquired at our department by using a commercially available unit (3DX Accuitomo; J Morita Mfg. Corp, Kyoto, Japan). The 3DX CT scanner has a radiation field of 30 mm height and 40 mm width at the centre of rotation. The imaging time was 17.5 s at 80 kV and 5 mA. Reconstructed slices of 0.5 mm thickness and 360° rotation were routinely used. The size of the isotropic voxel was 0.125 mm. The 3DX images were optimized for the visualization of the affected teeth by reslicing in different planes and adjusting histograms by using the software supplied with the machine (i-dixel 3DX version 1.68). Periapical films were obtained for all patients by using a dental X-ray unit (Trophy Radiologie SA, Croissy-Beaubourg, France). A paralleling technique was used in the routine manner. Size 2 Kodak E-speed (Eastman Kodak, France) films with an exposure time of 0.1–0.3 s at 60 kV and 7 mA were used. Radiographs were processed in the automatic processor XR-25S (Dürr Dental, Bietigheim-Bissinger, Germany). The periapical films were initially analysed with the aid of magnifying glasses on a light box and were thereafter digitized on a scanner (Scanmaker i800, Shanghai Zhongjing Co., Shanghai, China) at 1200 dpi and saved in the TIFF format. During the acquisition of both the dental radiographs and CBCT images, the patients were protected with lead aprons and thyroid collars. All CBCT images and dental radiographs were displayed on a 17-inch LCD monitor with screen resolution set at 1152 × 864 pixels (ViewSonic, Shanghai, China). The CBCT images were reviewed in three planes by the One Data Viewer software provided by the manufacturer. For dental radiographs, the observers were allowed to adjust the brightness, contrast and zoom by using the software Adobe Photoshop (version 8.0.1; Adobe Systems Inc., San Jose, CA). One investigator, who was not involved in the observation, coded the teeth and masked their clinical signs to exclude the possibility of observer bias to the presence or absence of fractures.
Two observers (oral radiologists) were calibrated by training them for 10% of the cases. Both of them had more than 5 years of clinical experience in CBCT imaging. The diagnostic criteria were based upon the suggestions in the literature, which were revised according to their experiences. In the cases for calibration, they observed the images respectively and then were allowed to compare their diagnoses with the final clinical diagnoses. For questionable cases where a disagreement of diagnosis existed, they discussed them to achieve a consensus of the criteria. These cases were later included into the evaluation but the initial reviewing results were not used. The diagnosis of a fracture on dental radiographs was based on direct visualization of a radiolucent line, which traversed the root, separating it partially or completely into two segments.2,9 The CBCT findings of a root fracture were set as the detection of a separation of the adjacent root segments on at least two contiguous sections without the continuation of the hypoattenuated line into the adjacent tissue2,9 (Figure 1) and the presence of a hypoattenuated line on at least two of the three-dimensional (3D) planes (Figures 2 and 3). Cases with metallic restorations or root fillings that usually exhibited multiple streak artifacts that traversed the root and adjacent bone were considered to be negative. For the two imaging modalities, the examiners recorded their responses on a dichotomous scale (fractured/non-fractured). 4 weeks after independent examination, the two oral radiologists compared their findings and discussed them in order to arrive at a consensus.
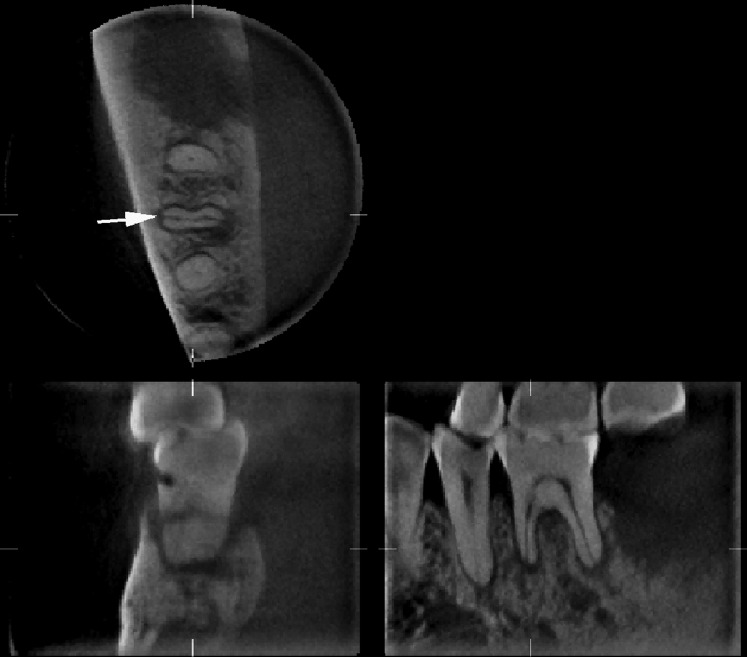
Figure 1.
Cone beam CT images of the right first mandibular molar of a 65-year-old man. A radiolucent fracture line (arrow) is clearly seen in the axial slice of the mesial root
Figure 2.
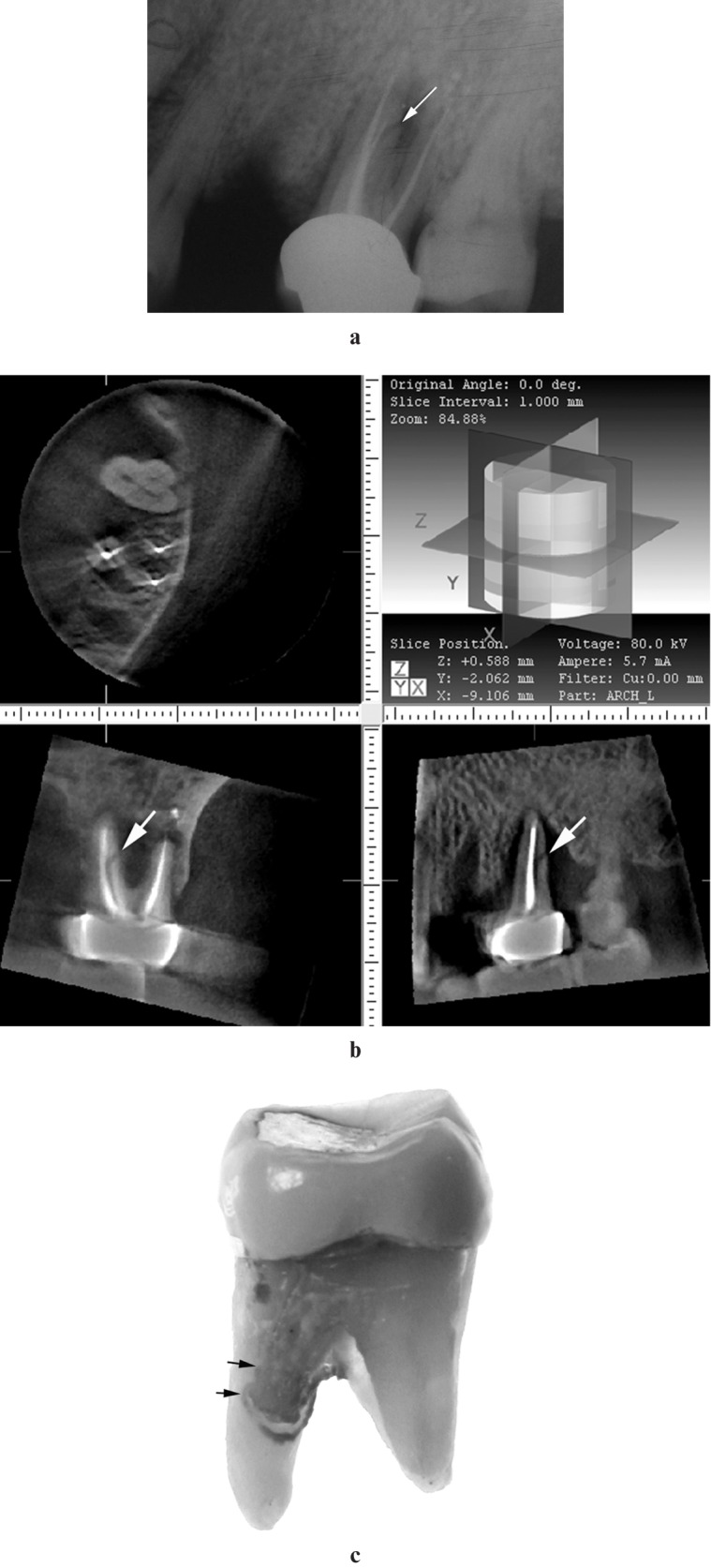
A 75-year-old woman with root fracture of the left maxillary first molar. (a) Dental radiograph shows a fracture line (arrow) and accompanying periradicular bone loss in the distal aspect of the palatal root of the left first maxillary molar. (b) Cone beam CT images of the left maxillary teeth. Despite the artifacts of imaging, a fracture line (arrows) and accompanying periradicular bone defect can be detected on the coronal and sagittal slices of the palatal root of the first maxillary molar. (c) After extraction, the fracture line can easily be seen in the palatal root of the left first maxillary molar, extending from the middle third to the cervical region of the root (double arrow)
Figure 3.
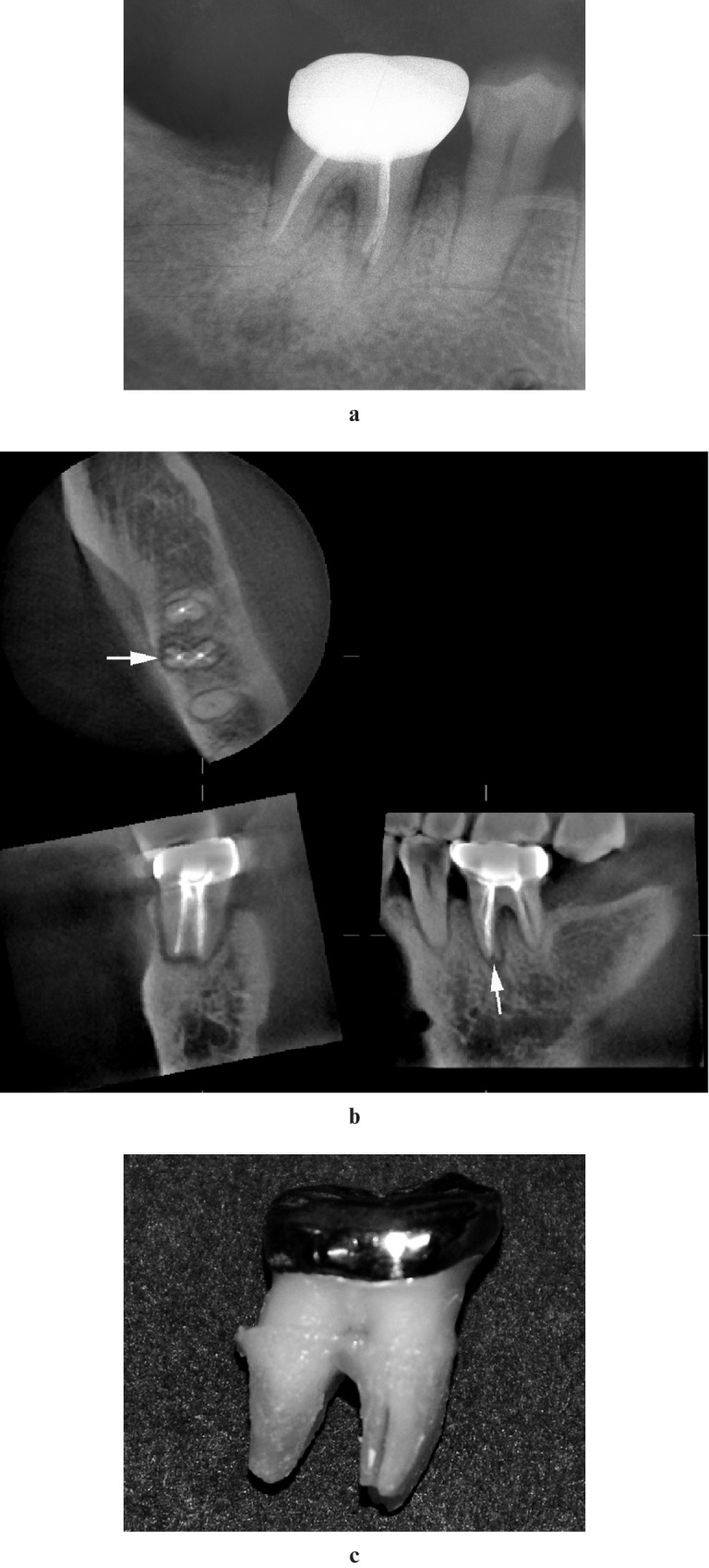
A 60-year-old woman with root fracture of right first mandibular molar. (a) Dental radiograph shows incomplete root canal filling and widening of the root canal space in the apical third of the mesial root of the right first mandibular molar, suggestive of a vertical root fracture. (b) Cone beam CT images reveal a fracture line (arrows) on both the axial and sagittal slices of the mesial root of the first mandibular molar. (c) Vertical fracture line can easily be seen in the mesial root of the extracted molar
The teeth studied were subjected to surgical exploration 1–3 months after the CBCT scans were performed. The type of treatment was decided on the basis of the clinical situations and radiographic findings. For the tooth that was determined to be extracted, the root surface was inspected with a magnifying glass (×2.5) after extraction. Most of these cases were mobile and easily extracted. For the teeth that were not mobile, special techniques were used to exclude the possibility of intraoperative fracture of the root. A mucoperiosteal flap was elevated and the buccal and/or lingual bone was then carefully removed. Excessive forces for rotation were avoided. For the tooth to be preserved, the root surface was inspected with a dental operating microscope during surgery. Fractures were diagnosed when separation of fragments were seen or when lines were darker than the surrounding root structure. For the preserved teeth, the corresponding author participated in the procedure and was responsible for the final diagnosis.
The results of image evaluations were compared with the findings of direct visualization to assess the sensitivity and specificity of dental radiographs and CBCT in the detection of root fractures.
Statistical analyses were conducted using the SPSS software program (version 11.0, SPSS Inc., Chicago, IL). The kappa coefficient was calculated to determine the reliability and reproducibility of the imaging evaluations by the two observers. χ2 tests were used to compare the diagnostic sensitivity and specificity (calculated on the basis of consensus reading) of CBCT with those of dental radiography for detecting root fractures. Moreover, the sensitivity and specificity were separately calculated for non-endodontically treated teeth vs endodontically treated teeth. The level of significance was set at P < 0.05.
Results
Of the 135 teeth assessed, 95 were found to have root fractures. Among the 95 teeth, the fractures were vertically oriented in 84 teeth and obliquely oriented in 11 teeth. Among the 95 teeth with root fractures, 91 teeth were extracted; root amputation (n = 2) or root-end resection (n = 2) was performed for the other teeth. Among the 40 teeth without fractures, 35 teeth were extracted and root amputation (n = 2) or root-end resection (n = 3) was performed for the remaining 5 teeth. With regard to tooth location, the 95 fractured teeth included 3 maxillary incisors, 14 premolars, 38 maxillary molars (Figures 2 and 4) and 40 mandibular molars (Figures 1 and 3); the 40 non-fractured teeth included 1 maxillary canine, 5 premolars, 16 maxillary molars and 18 mandibular molars.
Figure 4.
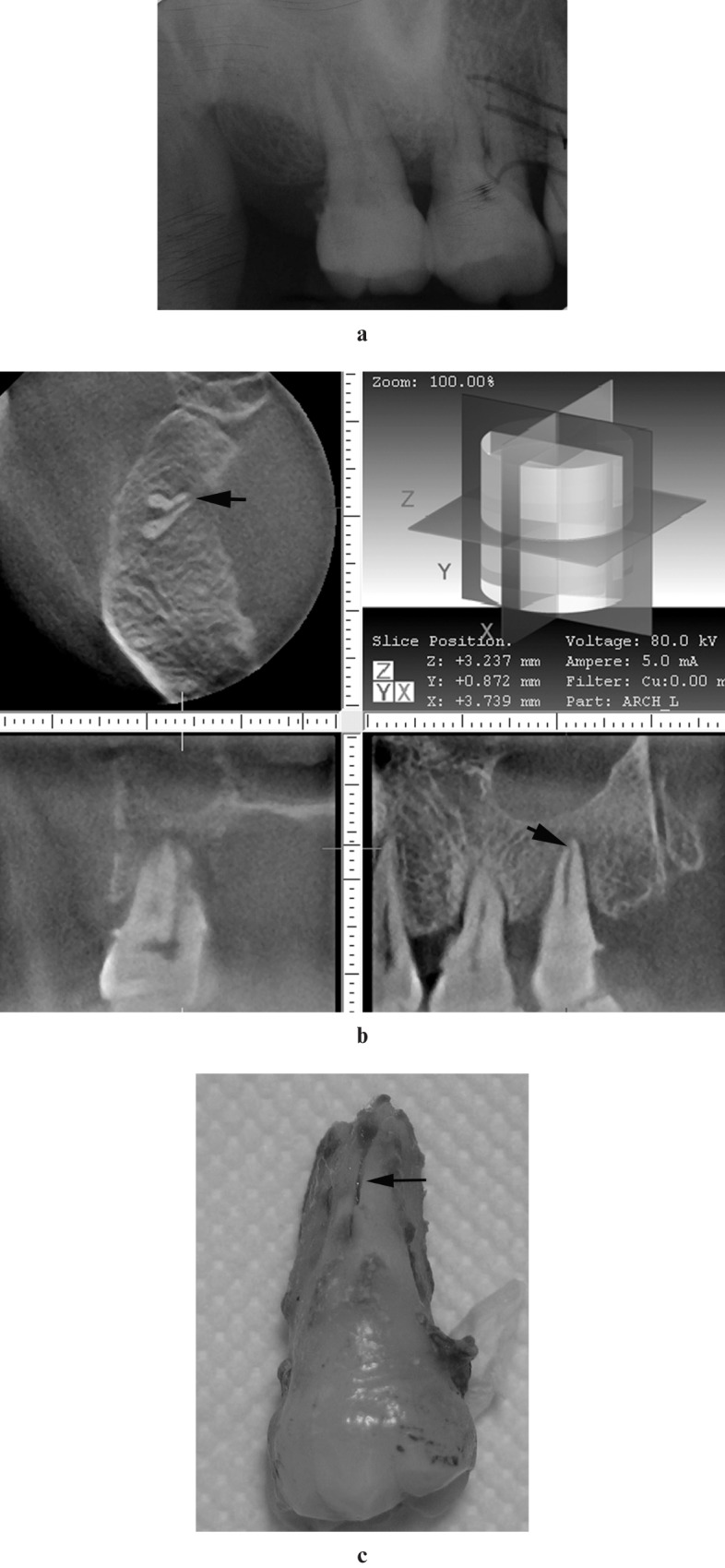
A 52-year-old woman with root fracture of right second maxillary molar. (a) Dental radiograph shows an irregular radiolucency in the apical region of the right second maxillary molar. No fracture line can definitely be seen. (b) Cone beam CT slices show a vertical root fracture in the palatal root of the right second maxillary molar. (c) The extracted right second maxillary molar. Note the vertical fracture line in the palatal root
The sensitivity and specificity for dental radiographs and CBCT scans are presented in Tables 1 and 2, respectively. In dental radiographs, the kappa coefficient between the two observers was 0.79; between the readings of observer A and the consensus reading it was 0.892; and between the readings of observer B and the consensus reading it was 0.92. In the CBCT scans, the kappa coefficient between the two observers was 0.94; between the readings of observer A and the consensus reading it was 0.95; and between the readings of observer B and the consensus reading it was 0.95.
Table 1. Statistical analysis of dental radiographic findings.
| Statistical index | Observer A |
Observer B |
Consensus reading |
Non-treated |
Treated |
| (%) | (%) | (%) | (%) | (%) | |
| Sensitivity | 32.6 | 23.2 | 26.3 | 26.9 | 25 |
| Specificity | 100 | 100 | 100 | 100 | 100 |
| PV (+) | 100 | 100 | 100 | – | – |
| PV (−) | 38.5 | 35.4 | 36.4 | – | – |
| Accuracy | 52.6 | 45.9 | 48.1 | – | – |
PV (+), positive predictive value; PV (−), negative predictive value; Non-treated, non-endodontically treated teeth; Treated, endodontically treated teeth
Table 2. Statistical analysis of cone-beam computed tomography findings.
| Statistical index | Observer A |
Observer B |
Consensus reading |
Non-treated |
Treated |
| (%) | (%) | (%) | (%) | (%) | |
| Sensitivity | 91.6 | 89.5 | 89.5 | 97.0 | 71.4 |
| Specificity | 95 | 95 | 97.5 | 94.7 | 100 |
| PV (+) | 97.8 | 97.7 | 98.8 | – | – |
| PV (−) | 82.6 | 79.2 | 79.6 | – | – |
| Accuracy | 92.6 | 91.1 | 91.9 | – | – |
PV (+), positive predictive value; PV (−), negative predictive value; Non-treated, non-endodontically treated teeth; Treated, endodontically treated teeth
The sensitivity of CBCT scans, calculated using the consensus reading, for detecting root fractures was significantly higher than that of dental radiographs (P < 0.001). The specificity was high and comparable for both dental radiographs and CBCT scans. Overall, CBCT scans (91.9%) were significantly more accurate than dental radiographs (48.1%) in detecting root fractures (P < 0.001). The presence of root canal fillings did not significantly influence the sensitivity and specificity of dental radiographs (P > 0.05). For CBCT, it reduced the sensitivity (P = 0.001) with no significant influence on specificity (P = 0.475).
Discussion
Dental root fractures can occur in vital teeth with an intact pulp or in endodontically treated teeth.10-12 The fracture lines can be limited to the root apex or involve the entire length of the root.2 In this in vivo study, the value of a clinical CBCT in the diagnosis of root fractures was determined and compared with that of dental radiography. The study samples comprised both non-endodontically treated teeth and endodontically treated teeth.
The causes of root fractures in endodontically treated teeth include excessive lateral condensation force during root canal filling procedures; wedging effects of endodontic posts; corrosion; and expansion of posts.11-14 True root fractures in non-endodontically treated teeth confined to the root surface are infrequently seen in English literature, but are common in Chinese patients.11,12 In our study, 67 (70.5%) teeth with root fractures were non-endodontically treated. The true causes of root fracture in non-endodontically treated teeth are still unknown. Yang et al15 proposed that these fractures might be related to special diet patterns or chewing habits in Chinese people. Yeh16 suggested that the root fractures might result from excessive, repetitive and heavy masticatory stress.
An early definite diagnosis is essential to avoid inappropriate treatment. However, it is often difficult to reach an accurate diagnosis on the basis of the presenting signs and symptoms because these symptoms are variable or non-specific.1-3 Conventional radiographs can be helpful for the diagnosis when the X-ray beam is parallel to the plane of the fracture, but this is scarcely possible. Superimposition of neighbouring structures further limits the ability to detect root fractures by using conventional radiographs.17,18 In a study of 375 cases, Rud and Omnell4 found that a fracture line was observed on dental radiographs in only 35.7% of the cases. In Youssefzadeh's study,2 the sensitivity of conventional dental radiographs in the assessment of root fractures was 25%; the lower sensitivity might be explained by the limitation of the actual clinical situations. Today, various digital imaging modalities are available. It can digitally acquire, store, enhance and transfer radiographical information with a reduced radiation dose compared with conventional film. Tsesis et al18 compared charge-coupled device (CCD) images and conventional films to detect vertical root fractures in extracted, endodontically treated maxillary molars and found no difference between the two imaging modalities ex vivo. In Hassan's study9 of 40 artificially fractured teeth, the sensitivity for root fracture detection of storage phosphor dental digital radiographs was 37.1%. In the present clinical study, root fractures were definitely detected in 26.3% of the teeth on dental radiographs. The sensitivity was distinctly limited by the actual clinical situations. It was postulated that the causes might include the following factors: (1) for the maxillary molars, superimposition of the multiple roots and the neighbouring skeletal structures might obscure the fracture line; (2) the radiolucent line, sometimes seen in the roots of premolars and mandibular molars, cannot be differentiated from the images of root canal spaces or periodontal ligaments; and (3) radiopaque substances, such as gutta-percha cones in endodontically treated teeth, might obscure the fracture line.9,19 Several limitations of the actual clinical situations in the present study might result in a bias (presumably underestimation) of dental radiographs in detecting root fractures. First, 20–30° angled radiographs were not routinely exposed on each patient; this might reduce the visualization of the fractures.9 Second, digitally scanned radiographs were used for reviewing; this reportedly produces inferior image quality to the original film.20 Further studies are required that focus on the comparison between digital imaging systems and CBCT in the detection of root fractures in vivo.
For clinical CBCT systems, the probability of detecting root fractures is expected to be higher than two-dimensional (2D) radiography. Visualizing fractures in transmission measurements is only dependent on the probability that a sufficient number of measured rays are tangent to the fracture.21 Since 3D techniques such as CBCT rely on many projections acquired from a circle around the object, the chances of having the fracture visualized on some of these projections are much higher. Even if a lot of detailed information is lost in the 3D reconstruction process, the chances of visualizing the fracture in the 3D volume are still much higher than in a 2D projection image. In Hassan's study,9 the sensitivity and specificity of CBCT for artificial root fracture detection were 79.4% and 92.5%, respectively. In Bernardes et al's report19 of 20 patients with suspected root fractures, CBCT (3DX Accuitomo) clearly reviewed root fractures in 18 cases, whereas conventional radiographs could show root fractures in only 2 cases. In the present study, the sensitivity of CBCT images for the detection of root fractures was 89.5%. In the remaining 10.5% of the teeth, root fractures could not be definitively detected. Statistical analysis showed that the presence of root canal fillings reduced the sensitivity (P < 0.01). The possible causes may have been: (1) for the teeth that had undergone root canal treatment and crown restorations, the star-shaped streak artifacts on tomographic slices might compromise the quality of the images, thus decreasing the observers' confidence in the diagnosis and leading to false-negative results based on our diagnostic criteria;9,19,22 (2) the fracture confined to the root apex was sometimes not distinguishable from root resorption; and (3) the theoretical spatial resolution of CBCT in this study was 0.25 mm. Owing to the Nyquist theorem, two voxel sizes are required to be able to detect the structure. This also meant that the fracture lines with a width less than 0.25 mm could not be detected. Notably, teeth for which surgical intervention was not attempted were excluded from this study; this might lead to an overestimation of the sensitivity of CBCT scans.
The overall specificity for both dental radiographs and CBCT scans was high and comparable and was not significantly influenced by the presence of root canal fillings. The high specificities can be attributed to the rigorous diagnostic criteria used in this clinical study. For CBCT images, only hypoattenuated lines confined to the root that were detectable on at least two contiguous sections and on at least two of the 3D planes were considered to be fracture lines. Cases with metallic restorations or root fillings that exhibited multiple streak artifacts were considered to be negative. For dental radiographs, only cases with a radiolucent line separating the root partially or completely into two segments were diagnosed as positive. This can also explain the fact that the positive-predictive value was 100% (suggesting that no false-positive readings of dental radiographs were observed) in the present study. Owing to the limitation of clinical situations, the disease prevalence in the present study was not balanced and this may affect sensitivity and specificity. Despite this, our aim was to compare the accuracy of two radiographic techniques and this was performed under the same conditions for both techniques.
Despite the advantages, CBCT scans expose the patients with additional radiation. According to Hirsch et al,23 the Accuitomo system has an effective dose of 20.02 μSv on the 4 × 4 cm field of view (FOV). Additionally, there are some limitations for CBCT imaging. The presence of beam hardening and streak artifacts often compromises the quality of images. There is a lot of training needed for interpreting 3D images and a radiologist report is required for every scan.19 Consequently, CBCT scans should be preserved for those cases where root fractures are suspected, not confirmed, by clinical signs and periapical radiographs. For those cases which have definite root fractures and are expected to be preserved, CBCT pictures are taken to assist surgeons in choosing the appropriate surgical approach, identifying the root that should be resected and reducing the amount of surgical trauma on the adjacent tissues.
In conclusion, CBCT provided high-quality 3D images which were valuable for detecting dental root fractures and for planning the treatment strategy. The sensitivity of CBCT images for the detection of root fractures was 89.5%, which was much higher than that of dental radiographs (26.3%). The presence of root canal fillings did not significantly influence the sensitivity of dental radiographs, but reduced the sensitivity of CBCT scans. The overall specificity of both dental radiographs and CBCT scans was high and comparable and remained largely unaffected by the presence of root canal fillings.
References
- 1.Cohen S, Berman LH, Blanco L, Bakland L, Kim JS. A demographic analysis of vertical root fractures. J Endod 2006;32:1160–1163 [DOI] [PubMed] [Google Scholar]
- 2.Youssefzadeh S, Gahleitner A, Dorffner R, Bernhart T, Kainberger FM. Dental vertical root fractures: value of CT in detection. Radiology 1999;210:545–549 [DOI] [PubMed] [Google Scholar]
- 3.Pitts DL, Natkin E. Diagnosis and treatment of vertical root fractures. J Endod 1983;9:338–346 [DOI] [PubMed] [Google Scholar]
- 4.Rud J, Omnell KA. Root fractures due to corrosion. Scand J Dent Res 1970;78:397–403 [DOI] [PubMed] [Google Scholar]
- 5.Suomalainen AK, Salo A, Robinson S, Peltola JS. The 3DX multi image micro-CT device in clinical dental practice. Dentomaxillofac Radiol 2007;36:80–85 [DOI] [PubMed] [Google Scholar]
- 6.Saskabe J, Kuroki Y, Fujimaki S, Nakajima I, Honda K. Reproducibility and accuracy of measuring unerupted teeth using limited cone beam X-ray CT. Dentomaxillofac Radiol 2007;36:2–6 [DOI] [PubMed] [Google Scholar]
- 7.Mora MA, Mol A, Tyndall DA, Rivera EM. In vitro assessment of local computed tomography for the detection of longitudinal tooth fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:825–829 [DOI] [PubMed] [Google Scholar]
- 8.Hannig C, Dullin C, Hülsmann M, Heidrict G. Three-dimensional, non-destructive visualization of vertical root fractures using flat panel volume detector computer tomography: an ex vivo in vitro case report. Int Endod J 2005;38:904–913 [DOI] [PubMed] [Google Scholar]
- 9.Hassan B, Elissavet M, Ozok AR, van derStelt P, Wesselink PR. Detection of vertical root fractures in endodontically treated teeth by a cone beam computed tomography scan. J Endod 2009;35:719–722 [DOI] [PubMed] [Google Scholar]
- 10.Tamse A, Fuss Z, Lustig J, Kaplavi J. An evaluation of endodontically treated vertically fractured teeth. J Endod 1999;25:506–508 [DOI] [PubMed] [Google Scholar]
- 11.Chan CP, Tseng SC, Lin CP, Huang CC, Tsai TP, Chen CC. Vertical root fracture in nonendodontically treated teeth – a clinical report of 64 cases in Chinese patients. J Endod 1998;10:678–681 [DOI] [PubMed] [Google Scholar]
- 12.Chan CP, Lin CP, Tseng SC, Jeng JH. Vertical root fracture in endodontically versus nonendodontically treated teeth – a survey of 315 cases in Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;87:504–507 [DOI] [PubMed] [Google Scholar]
- 13.Meister F, Lommel TJ, Gerstein H. Diagnosis and possible causes of vertical root fractures. Oral Surg Oral Med Oral Pathol 1980;49:243–253 [DOI] [PubMed] [Google Scholar]
- 14.Tamse A. Iatrogenic vertical root fractures in endodontically treated teeth. Endod Dent Traumatol 1988;4:190–196 [DOI] [PubMed] [Google Scholar]
- 15.Yang SF, Rivera EM, Walton RE. Vertical root fracture in nonendodontically treated teeth. J Endod 1995;21:337–339 [DOI] [PubMed] [Google Scholar]
- 16.Yeh CJ. Fatigue root fracture: a spontaneous root fracture in nonendodontically treated teeth. Br Dent J 1997;182:261–266 [DOI] [PubMed] [Google Scholar]
- 17.Kositbowornchai S, Nuansakul R, Sikram S, Sinahawattana S, Saengmontri S. Root fracture detection: a comparison of direct digital radiography with conventional radiography. Dentomaxillofac Radiol 2001;30:106–109 [DOI] [PubMed] [Google Scholar]
- 18.Tsesis I, Kamburoğlu K, Katz A, Tamse A, Kaffe I, Kfir A. Comparison of digital with conventional radiography in detection of vertical root fractures in endodontically treated maxillary premolars: an ex vivo study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;106:124–128 [DOI] [PubMed] [Google Scholar]
- 19.Bernardes RA, de Moraes IG, Duarte MA, Azevedo BC, Azevedo JR, Bramante MB. Use of cone-beam volumetric tomography in the diagnosis of root fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:270–277 [DOI] [PubMed] [Google Scholar]
- 20.Grassl U, Schulze RKW. In vitro perception of low-contrast features in digital, film, and digitized dental radiographs: A receiver operating characteristic analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:694–701 [DOI] [PubMed] [Google Scholar]
- 21.Quinto ET. Singularities of the x-ray transform and limited data tomography in R2 and R3. Siam J Math Anal 1993;24:1215–1225 [Google Scholar]
- 22.Zhang Y, Zhang L, Zhu X, Lee A, Chamber M, Dong L. Reducing metal artifacts in cone-beam CT images by preprocessing projection data. Int J Radiat Oncol Biol Phys 2007;67:924–932 [DOI] [PubMed] [Google Scholar]
- 23.Hirsch E, Wolf U, Heinicke F, Silva MAG. Dosimetry of the cone beam computed tomography Veraviewepocs 3D compared with the 3D Accuitomo in different fields of view. Dentomaxillofac Radiol 2008;37:268–273 [DOI] [PubMed] [Google Scholar]