Abstract
Objective
The aim of this study was to compare periapical radiographs with cone beam CT (CBCT) imaging in detecting and localizing alveolar bone loss by comparing linear measurements of the height, depth and width of the defects and identifying combined bone defects in tomographic images.
Methods
The images were selected from a secondary database containing images of patients referred for periodontal evaluation. The sample consisted of 51 sites showing both horizontal and vertical bone loss, assessed by 3 trained examiners.
Results
The results showed that there were no statistically significant differences between the imaging methods in terms of identification of the pattern of bone loss. However, there were differences between the two methods when the distance between the cemento-enamel junction (CEJ) and the alveolar crest (AC) was measured. When the distance between the CEJ and the deepest point and width of the defect were measured, the methods showed no statistically significant difference. In this study, 30.8% of the 39 teeth evaluated had combined bone defects.
Conclusions
The two methods differ when detecting the height of the alveolar bone crest but present similar views of the depth and width of bone defects. CBCT was the only method that allowed for an analysis of the buccal and lingual/palatal surfaces and an improved visualization of the morphology of the defect.
Keywords: diagnosis, tomography, radiology, alveolar bone loss
Introduction
Correct assessment of the bone condition is essential for the diagnosis, treatment planning and prognosis of periodontal disease.1 Information derived from probing the gingival tissues in association with diagnostic imaging provides guidelines for assessing the alveolar bone height and checking for the presence of vertical bone defects.2,3 Radiographs provide information for the detection and measurement of changes brought about by periodontopathy4-7 and in addition make it possible to distinguish the pattern of bone resorption.7
Among two-dimensional (2D) radiographic diagnosis methods, bitewing and periapical radiographs are the most suitable because they are easily acquired, cheap and provide high-resolution images.2,3 However, these methods are limited by overlapping anatomical structures,8,9 difficulty in standardization2,9 and by underestimating the size and occurrence of bone defects.10 Digital images, besides improving diagnostic interpretation,10 are also 2D images.
In the experience of the authors, cone beam CT (CBCT) is still underused for periodontal diagnosis. Research comparing the use of three-dimensional (3D) volumetric images and 2D images4,9,11 in artificial bone defects have shown that CBCT has a sensitivity of 80–100% in the detection and classification of bone defects, while intraoral radiographs present a sensitivity of 63–67%.4,9,11 When compared with periapical and panoramic images,4,9,11,12 CBCT has also shown an absence of distortion and overlapping and the dimensions it presents are compatible with the actual size. The perception of images acquired using CBCT in the evaluation of alveolar bone loss and periodontal bone defects could lead to a new approach in the evaluation of patients with periodontal disease and prove to be an excellent resource when deciding on the most appropriate therapy.
The aim of this study was to compare CBCT and periapical radiographs when detecting and localizing alveolar bone loss, when carrying out linear measurements of the height, depth and width of defects and when identifying combined bone defects in tomographic images.
Materials and methods
This research was conducted in a secondary database with approval from the Research Ethics Committee.
Radiographic exams
This cross-sectional study used images belonging to the database of a private dental radiology clinic between July 2008 and April 2009. The periapical radiographs were obtained using a film holder device (Indusbello, Paraná, Brazil) and a bisector angle technique by the same operator. The dental X-ray was a Spectro 70X Seletronic Dental X-ray machine (Dabi Atlante, Salvador, Brazil) with 70 kV, 8 mA and an exposure time which, in accordance with the region imaged, varied from 0.5 s to 0.7 s. An X-ray Kodak Insight film (Eastman Kodak Co, Rochester, NY) was used. The conventional periapical radiographs were later digitized by using a scanner scanjet HP 4890 (Hewlett Packard, Palo Alto, CA) with a resolution of 300 dpi and were saved as TIFF files.
CBCT images were obtained using an i-CAT CBCT scanner (Imaging Sciences International, Hatfield, PA), with 120 kV and 36.12 mAs. The field of view (FOV) was 6 cm and the voxel size was 0.2×0.2×0.2 mm. The images were generated in the digital imaging and communications in medicine (DICOM) format, processed by Xoran Cat software, version 3.1.62, in an IntelR Pentium computer® D CPU 340GHz, 335GB RAM, Microsoft Windows XP Professional SP-2 program (Microsoft Corp, Redmond, WA) and analysed by axial, cross-sectional and sagittal reconstructions with a cutting interval of 1 mm.
Sample
A dental radiology specialist with 14 years' professional experience selected the images using these inclusion criteria: good image quality, defined as medium density and contrast, centralization of the region assessed and visualization of the cemento-enamel junction (CEJ). Sample images which presented interproximal overlap in periapical radiography, metallic restorations with scatter effects of metal restorations in CBCT images and those which had coronal destruction compromising the CEJ were excluded.
From a database of 1485 images, periapical and tomographic images of 21 adult patients who had been referred for a radiographic evaluation of periodontal disease were selected, giving a total of 218 teeth; however, 179 teeth which presented with a compromised CEJ were excluded from the sample. Consequently, the sample consisted of 39 teeth from 11 adult patients of both genders, aged between 39 and 66 years.
Imaging evaluation
The images were analysed by three examiners: examiner 1 was a radiologist with 2 years' professional experience and examiners 2 and 3 were Masters students in oral radiology. The examiners had been previously trained using 20 images not included in the study.
Examiner 2 selected the teeth and surfaces to be analysed in both imaging modalities. Each tomogram was selected separately for each distance measured since end points, such as the alveolar crest and the deepest point of the defect, could be viewed in different slices. Before measuring, each examiner converted the images from pixels into millimetres using the real dimensions of the radiographic film and printed tomogram.
The interpretation was carried out in a quiet darkroom, using a 17 inch monitor with 1280×1024 screen resolution. The images were analysed at different times, thereby characterizing a blind study of the results. Each examiner identified whether the pattern of bone loss was horizontal or vertical in both types of image.
The sites were measured first on periapical radiographs and later on CBCT with the help of the ruler in the Image Tool software (University of Texas Health Science Centre, San Antonio, TX) based on the method proposed by Misch et al.9 Three measurements were performed for each site: the height of the alveolar crest (AC), measured from the CEJ to the AC; the depth of the defect, measured from the CEJ to the bottom of the defect; and the width of the defect, measured from the highest point of the AC to the dental root adjacent to the defect (Figures 1 and 2). When the examiner observed two levels of the AC (from lingual/palatal and buccal surface) the deepest points were measured. The distance from the CEJ to the AC was also measured in the buccal and lingual/palatal surfaces in cross-sectional tomograms.
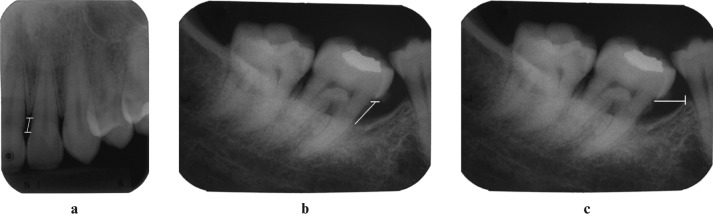
Figure 1.
Periapical radiograph illustrating the distances: (a) from the cemento-enamel junction (CEJ) to the alveolar crest (AC) in the mesial surface of tooth 22, (b) from the CEJ to the bottom of the defect and (c) the width of the defect on the mesial surface of tooth 47 (white lines)
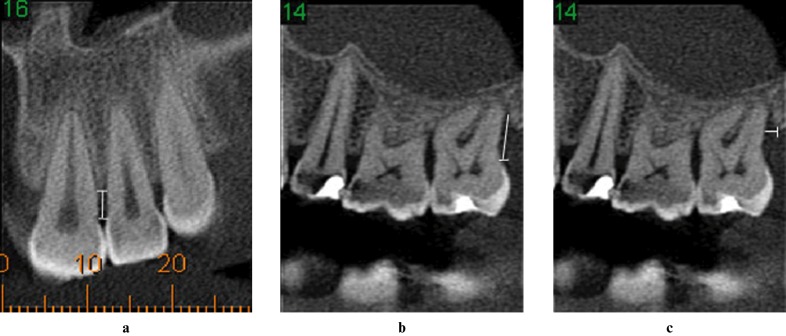
Figure 2.
Sagittal cone beam tomograms showing the measurements of the distances: (a) from the cemento-enamel junction (CEJ) to the alveolar crest (AC) in the mesial surface of tooth 22, (b) from the CEJ to the bottom of the defect and (c) the width of the defect in the distal surface of tooth 27 (white lines)
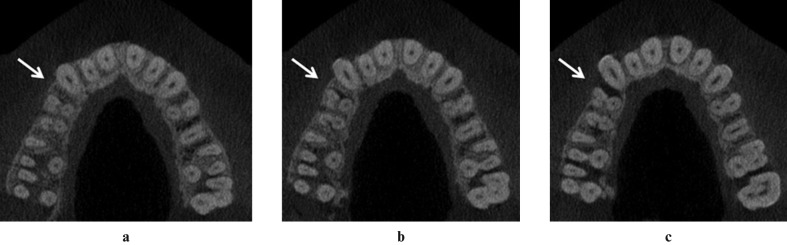
The axial slices were used to verify the presence of combined bone defects (Figure 3), identified according to the classification of Goldman and Cohen.13 After a 30 day interval, a second evaluation of all the images used in this study was conducted by examiner 2 to prove the reproducibility of the method.
Figure 3.
Axial tomograms illustrating the presence of combined bone defects (white arrows) in the mesial surface of tooth 14. (a) No evidence of defect, (b) defect with three walls remaining and (c) progression of the defect in cervical direction with one wall remaining
Statistical analysis
The Biostat 4.0 software (Civil Society Mamirauá/MCTCNPq, Brazil) and the SPSS software for Windows (version 18.0; SPSS Inc., Chicago, IL) were used, assuming a significance level of 5% (α = 0.05) for all tests. To evaluate the intra- and interexaminer concordance, the Kruskal–Wallis test was used while the Kolmogorov–Smirnov and Mann–Whitney tests were used to compare the two diagnostic methods.
Results
In order to classify the presence of alveolar bone loss, a distance of 3 mm from the CEJ to the AC was used as the parameter of normality. Bone loss was found at 51 sites in relation to 39 teeth. There were 36 sites with horizontal bone loss and 15 sites with vertical bone loss.
The result of the Kruskal–Wallis test for comparison between the measurements made by the three examiners showed a p-value of > 0.05, indicating a similarity between the intra- and interscores for data collected by the examiners.
There were no statistically significant differences in terms of the identification of the pattern of alveolar bone loss in either imaging modality. Examiners 1 and 2 were in agreement in 100.0% of the cases and differed from examiner 3 in 1.9% of the cases.
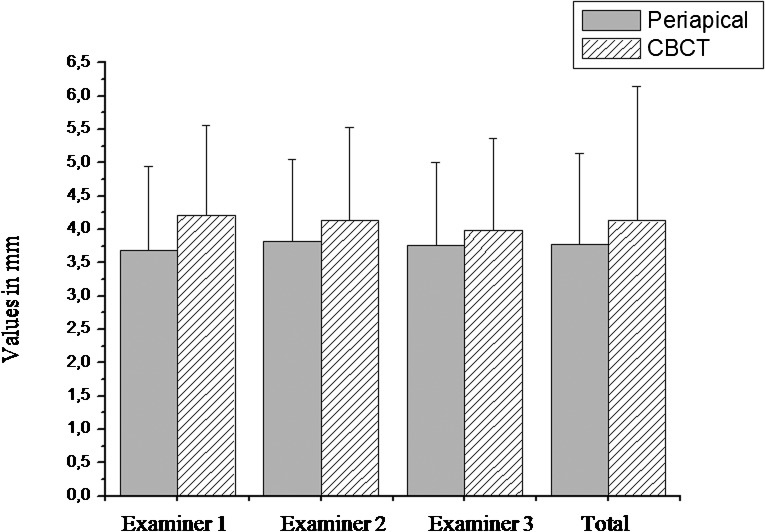
A statistical difference (p < 0.05) was only seen between the measurements of the distance from the CEJ to the AC (Figure 4), with an average of 3.8 mm for measurements taken in periapical radiography and 4.1 mm for CBCT images. When comparing the distance between the CEJ with the deepest point and width of the defect, this study showed p-values > 0.05, indicating that there were no statistically significant differences between these two measurements in either method. All the results described above can be seen in Table 1.
Figure 4.
Graphical representation of the mean (mm) and standard deviation (mm) for the distance from the cemento-enamel junction (CEJ) to the alveolar crest (AC) in periapical and cone beam CT (CBCT) images, for each examiner
Table 1. Mean (mm) of linear measurements of the height, depth and width of defects, according to the three examiners in both methods.
| Examiner 1 |
Examiner 2 |
Examiner 3 |
|||||
| P | CBCT | P | CBCT | P | CBCT | P* | |
| Height of the AC | 3.71 | 4.16 | 3.84 | 4.06 | 3.79 | 3.95 | 0.04 |
| Depth of the defect | 6.57 | 5.27 | 6.58 | 5.63 | 6.04 | 5.15 | 0.28 |
| Width of the defect | 1.75 | 1.19 | 1.83 | 1.19 | 1.56 | 1.06 | 0.66 |
AC, alveolar crest; CBCT, cone beam CT; P, periapical
*Mann–Whitney test
Measurements of the buccal and palatal/lingual surfaces in cross-sectional tomograms were not compared with the periapical images owing to the limitations of the latter, so we evaluated the agreement of the absolute measurements made between the three examiners, finding p-values of < 0.05 and showing that the cross-sectional slices allow for the assessment of bone loss in both buccal and lingual/palatal surfaces.
Of the 39 teeth evaluated in the axial slices, 27 (69.2%) showed no combined defects. According to the classification proposed by Goldman and Cohen,13 12 teeth (30.8%) presented combined defects with (1) 3 apical and 2 cervical walls remaining in 7.7% of the teeth; (2) 3, 2 and 1 cervical walls remaining in 15.4% of the teeth; (3) 2 apical and 1 cervical walls remaining in 5.1% of the teeth; and (4) 3 apical and no cervical walls remaining in 2.6% of the teeth. Examiners 1, 2 and 3 were in agreement in 100.0% of the cases.
Discussion
Although many studies have been undertaken to show the accuracy of imaging methods in the assessment of alveolar bone loss, an accurate diagnosis of bone loss in periodontal disease still remains a challenge for clinical dentistry. Studies comparing 2D and 3D imaging methods used in the diagnosis of periodontal disease are carried out mainly in macerated skulls and different criteria are adopted for comparison.4,8,9,11
In the literature there are wide variations for normal bone height in relation to the CEJ, ranging from 1 mm to 3 mm,8,14-17 although a distance of 2 mm is more widely adopted in studies of patients without periodontal disease.14 In young adults, the mean alveolar bone height in relation to the CEJ is 1.4 mm (± 0.7) and for people over 45 years this average is extended to 3 mm (± 1.5).18 As the images were obtained from live people with a mean age of 48 years, a measurement greater than 3 mm between the CEJ and the AC was adopted to indicate the presence of periodontal bone loss for this study. In a study to evaluate the accuracy of CBCT for detecting and quantifying periodontal bone defects, Mol and Balasundaram8 defined a distance equal to or greater than 3 mm for vertical bone defects. The same distance was adopted by Grimard et al19 to compare intraoral radiographs with CBCT in the assessment of bone gain after regenerative therapy.
In cases where 3D analysis is required, the use of CBCT is justified by the fact that the radiation dose to the patient is relatively less when compared with that of the traditional CT20,21 or multislice CT.22,23 Furthermore, the accuracy of this type of CT is more representative for dental24 and periodontal structures.8,9,12 The effective radiation dose of dental CT varies according to the brand of the appliance and the technical specifications selected during use (FOV, exposure time, kilovoltage and milliamperage).25 When compared with conventional radiography, the CBCT radiation dose is equivalent to a full-mouth series and approximately three to seven times the dose of a panoramic radiograph26 depending on the setting in use. On the other hand, when compared with conventional radiography, CBCT has far greater potential for providing information.
The quality of images obtained by CBCT depends on acquisition parameters, such as milliamperage, kilovoltage26,27 and voxel size.25,27 In order to view the periodontal structures which are important when establishing the diagnosis of periodontal disease, such as the periodontal ligament space, cortical bone, AC and alveolar cortical plate, images with better definition are needed as well as a smaller voxel size,25,27 consequently raising milliamperage and kilovoltage values. The voxel size used in this study was 0.2 mm, similar to that used by Grimard et al,19 which allowed for optimal image definition. However, other studies such as those of Misch et al9 and Vandenberghe et al11 used a 0.4 mm voxel size. The selection of the technical parameters of the image should be a balance between the need for image resolution and the use of a minimum amount of radiation. Another factor which may affect the quality of images obtained by CBCT is the presence of metallic artefacts in the image when patients have metal fillings or other devices. Metal artefacts can be problematic when one is interpreting images. In this study, care has been taken in the selection of images. Teeth with metallic restorations with scatter effects in their CBCT images were excluded. Thus, the examiners had no difficulty in making linear measurements on selected sites.
When comparing the measurements of the distance between the CEJ and the AC, it was seen that the methods were statistically different from each other, with an average of 3.8 mm for measurements taken in periapical radiography and 4.1 mm for the CBCT images. These are in agreement with the study of Mol and Balasundaram8 in human skulls, which showed that the measurements of the CBCT were slightly more accurate than those made in conventional intraoral radiographs. In this study, it was not possible to establish the most accurate method because there was no gold standard for comparison.
When measurements of the distance from the CEJ to the deepest point and the width of the defect were compared, this study showed p-values of > 0.05, indicating that there were no statistically significant differences between the methods. A similar result was reported by Misch et al,9 who saw no significant differences between measurements taken with a digital caliper in artificial bone defects and CBCT radiographic and periapical images. These authors found an average error of 0.27 mm for periapical and 0.41 mm for cross-sectional slices.
Vandenberghe et al11 observed that the cross-sectional slices allowed for a better assessment of periodontal bone levels with an average underestimation of 0.29 mm compared with 0.56 mm in periapical digital radiographs. These results are different from those of this study and also from those of Misch et al,9 which is probably owing to the different CBCT protocols used such as the ranges of slices and the size of the voxel. Other studies with similar parameters in addition to clinical validation and/or surgery should be performed in order to make a better comparison between the methods.
Axial slices made parallel to the occlusal plane allow for better visualization of the morphology of periodontal bone defects.1 Knowledge of the morphological component is of fundamental importance for the therapy and prognosis of periodontally compromised teeth because a larger number of remaining walls favour the prognosis of regenerative therapy.18 The results of this study showed that of the 39 teeth evaluated by axial slices, 12 (30.8%) presented combined bone defects. This result is lower than that of Grimard et al,18 who found combination bony defects present in 54% of a total of 35 bone defects analysed in their study.
This study reinforces the fact that while both imaging modalities are useful when diagnosing bone loss in interproximal surfaces, CBCT offers significant advantages when detecting and locating vertical bone defects,8,9,11,18 thereby facilitating surgical planning.
The results show that a request for CBCT is justified for the periodontal surgical planning of patients with severe periodontal disease, such as aggressive peridontitis, and especially for regenerative or mucogingival surgical planning because these surgical procedures are costly and difficult to plan. It is worth emphasizing that periapical radiographs result in lower radiation doses to the patient and are less costly and should be indicated for simpler cases. Therefore, information acquired from the clinical examination is of vital importance when choosing the most appropriate method for diagnosing periodontal disease.
Studies to assess the accuracy of these methods when used with live people could further clarify the precise indication for the different imaging methods by approximating the actual clinical conditions and thereby establishing the advantages and disadvantages of the available diagnostic methods. In conclusion, the two methods differ as to the measurement of the height of the alveolar bone crest but perform similarly when measuring the depth and width of periodontal bone defects. CBCT allowed for the identification of combined bone defects through a 3D evaluation of the alveolar bone crest.
Acknowledgments
We would like to thank UFG (PRPPG) for supporting this study.
References
- 1.Langen HJ, Fuhrmann R, Diedrich P, Gunther RW. Diagnosis of infra-alveolar bony lesions in the dentate alveolar process with high-resolution computed tomography: experimental results. Invest Radiol 1995;30:421–426 [DOI] [PubMed] [Google Scholar]
- 2.Jeffcoat MK. Current concepts in periodontal disease testing. J Am Dent Assoc 1994;125:1071–1078 [DOI] [PubMed] [Google Scholar]
- 3.Reddy MS. Radiographic methods in the evaluation of periodontal therapy. J Periodontol 1992;63:1078–1084 [DOI] [PubMed] [Google Scholar]
- 4.Fuhrmann RAW, Wehrbein H, Langen HJ, Diedrich PR. Assessment of the dentate alveolar process with high resolution computed tomography. Dentomaxillofac Radiol 1995;24:50–54 [DOI] [PubMed] [Google Scholar]
- 5.Jeffcoat MK. Radiographic methods for the detection of progressive alveolar bone loss. J Periodontol 1992;63:367–372 [DOI] [PubMed] [Google Scholar]
- 6.Albandar JM, Abbas DK. Radiographic quantification of alveolar bone level changes. Comparison of 3 currently used methods. J Clin Periodontol 1986;13:810–813 [DOI] [PubMed] [Google Scholar]
- 7.Mol A. Imaging methods in periodontology. Periodontology 2004;34:34–48 [DOI] [PubMed] [Google Scholar]
- 8.Mol A, Balasundaram A. In vitro cone beam computed tomography imaging periodontal bone. Dentomaxillofac Radiol 2008;37:319–324 [DOI] [PubMed] [Google Scholar]
- 9.Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol 2006;77:1261–1266 [DOI] [PubMed] [Google Scholar]
- 10.Eickholz P, Kim T-S, Benn DK, Staehle HK. Accuracy of radiographic assessments of interproximal bone loss. Oral Surg Oral Med Oral Pathol Oral Radiol Oral Endod 1998;85:99–106 [DOI] [PubMed] [Google Scholar]
- 11.Vandenberghe B, Jacobs R, Yang J. Diagnostic validity (or acuity) of 2D CCD versus 3D CBCT images for assessing periodontal breakdown. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:395–401 [DOI] [PubMed] [Google Scholar]
- 12.Mengel R, Candir M, Shiratori K, Flores-De-Jacoby L. Digital volume tomography in the diagnosis of periodontal defects: an in vitro study of native pigs and human mandibles. J Periodontol 2005;76:665–673 [DOI] [PubMed] [Google Scholar]
- 13.Goldman HM, Cohen DW. The intrabony pocket: classification and treatment. J Periodontol 1957;29:272–279 [Google Scholar]
- 14.Wong BKJ, Leichter JW, Chandler NP, Cullinan MP, Holborow DW. Radiographic study of ethnic variation in alveolar bone height among New Zealand dental students. J Periodontol 2007;78:1070–1074 [DOI] [PubMed] [Google Scholar]
- 15.Lennon MA, Davies RM. Prevalence and distribution of alveolar bone loss in a population of 15-year-old school children. J Clin Periodontol 1974;1:175–182 [DOI] [PubMed] [Google Scholar]
- 16.Latcham NL, Powell RN, Jago JD, Seymour GJ, Aikten JF. A radiographic study of chronic periodontitis in 15-year-old Queensland children. J Clin Periodontol 1983;10:37–45 [DOI] [PubMed] [Google Scholar]
- 17.Gargiulo AW, Wentz FM, Orban B. Dimensions and relations of the dentogingival junctions in humans. J Periodontol 1961;32:261–267 [Google Scholar]
- 18.Persson RE, Hollender LG, Laurell L, Persson GR. Horizontal alveolar bone loss and vertical bone defects in an adult patient population. J Periodontol 1998;69:348–356 [DOI] [PubMed] [Google Scholar]
- 19.Grimard BA, Hoidal MJ, Mills MP, Mellonig JT, Nummikoski PV, Mealey BL. Comparison of clinical, periapical radiograph, and cone-beam volume tomography measurement techniques for assessing bone level changes following regenerative periodontal therapy. J Periodontol 2009;80:48–55 [DOI] [PubMed] [Google Scholar]
- 20.Frederiksen NL, Benson BW, Sokolowski TW. Effective dose and risk assessment from film tomography used for dental implants. Radiol 1994;23:123–127 [DOI] [PubMed] [Google Scholar]
- 21.Silva MAG, Wolf U, Heinicke F, Bumann A, Visser H, Hirsch E. Cone beam computed tomography for routine orthodontic treatment planning: a radiation dose evaluation. Am J Orthod Dentofacial Orthop 2008;133:1–5 [DOI] [PubMed] [Google Scholar]
- 22.Nakajima A, Sameshima GT, Yoshinori A, Homme Y, Shimizu N, Dougherty H. Two and three-dimensional orthodontic imaging using limited cone beam – computed tomography. Angle Orthod 2005;75:895–903 [DOI] [PubMed] [Google Scholar]
- 23.Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol 2004;33:196–201 [DOI] [PubMed] [Google Scholar]
- 24.Holberg C, Steinhauser S, Geis P, Janson-Rudzki I. Cone-beam computed tomography in orthodontics: benefits and limitations. J Orofac Orthop 2005;66:434–444 [DOI] [PubMed] [Google Scholar]
- 25.Katsumata A, Hirukawa A, Okumura S, Naitoh M, Fujishita M, Ariji E, et al. Relationship between density variability and imaging volume size in cone-beam computerized tomographic scanning of the maxillofacial region: an in vitro study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:420–425 [DOI] [PubMed] [Google Scholar]
- 26.Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol 2006;35:219–226 [DOI] [PubMed] [Google Scholar]
- 27.Ballrick JW, Palomo JM, Ruch E, Amberman BD, Hans MG. Image distortion and spatial resolution of a commercially available cone-beam computed tomography machine. Am J Orthod Dentofacial Orthop 2008;134:573–582 [DOI] [PubMed] [Google Scholar]