Abstract
Objective
The aim of this study was to assess the accuracy and reliability of cone beam CT (CBCT) images compared with multidetector CT (MDCT) images for the detection of surface osseous changes in temporomandibular joints (TMJs).
Methods
Naked-eye inspection of 110 sites in 10 TMJs from 5 dry human skulls provided the gold standard. Two radiologists interpreted the images. Sensitivity, specificity and kappa statistics were used for analysis.
Results
The sensitivities of both modalities were low and comparable whereas the specificities were high and comparable. Intraobserver reliabilities for CBCT (p=0.0005) and for MDCT (p=0.0001) showed significant agreement. Interobserver reliability was higher for CBCT than for MDCT.
Conclusion
CBCT and MDCT accuracy was comparable in detecting surface osseous changes with comparable intraobserver reliabilities. However, since CBCT requires less radiation exposure, it should be encouraged for imaging TMJ with suspected surface osseous changes.
Keywords: temporomandibular joint, multidetector computed tomography, cone beam computed tomography, osseous changes
Introduction
Many diagnostic imaging techniques have been proposed to visualize osteoarthritic changes. However, no general consensus has been reached as to which diagnostic imaging technique should be the gold standard in detecting these lesions in the temporomandibular joint (TMJ). Some of these techniques, such as plain and panoramic radiographs, are good screening tools for gross bony changes. However, these tools are often limited because of the anatomy of the region, superimpositions and the presence of overlapping structures.1
The application of conventional CT in imaging the TMJ has been most significant for the evaluation of hard tissue or bony changes of the joint. CT has been found to be superior to plain films and MRI, with 87–96% accuracy in detecting degenerative arthritis.2,3 CT imaging protocols that associate axial with multiplanar reconstructed images in multidetector CT (MDCT) demonstrated the highest accuracy, with 93% sensitivity and 100% specificity.4 Although the use of CT as a diagnostic tool has been used in medicine for many years, its application in dentistry is limited, mainly because of the high cost of equipment, the large space required for its operation and the high dose of radiation involved. Cone beam CT (CBCT) was introduced as an alternative to CT and is considered appropriate for a wide range of craniofacial indications.5 CBCT uses a cone-shaped X-ray beam instead of the collimated fan beam used with CT. The tube detector system performs a 360° rotation around the head of the patient with a constant beam angle. The primary images can then be used for further secondary reconstructions in all planes and for three-dimensional (3D) reconstruction.6 Several authors have reported high dimensional accuracy of maxillofacial CBCT in examining facial structures,7-9 including the TMJ.6,10,11 Two studies showed the superiority of CBCT compared with MDCT in displaying hard tissue in the maxillofacial region while substantially decreasing the X-ray dose to the patient.12,13 Furthermore, CBCT was shown to have extra dentotechnical applications for the end user, in the form of oblique planar reformation and curved planar reformation, which favour it over MDCT.14 A study by Tsiklakis et al6 showed that the reconstruction technique for obtaining lateral and coronal CBCT images and 3D reconstructions of the TMJ had high diagnostic quality, short examination time and lower patient radiation dose compared with conventional CT.2,3 Honey et al3 compared the radiographic morphological characteristics of mandibular condyles with the microscopic observation of osseous changes in 10 TMJs from 5 human cadavers. They found high detectability of CBCT images for bony morphological features compared with conventional tomography and helical CT.3 When Hintze et al15 compared the diagnostic capability of CBCT in detecting osseous changes in the TMJ with conventional CT, they found no significant differences in diagnostic accuracy between the two modalities.15
Most of these studies show that CBCT, compared with other modalities, can depict anatomy or function. However, it is important to assess the diagnostic ability of CBCT and its accuracy compared with the true value gold standard and with CT, which has already been proven to provide optimal imaging of the osseous components of the TMJ. However, only one study has evaluated the diagnostic reliability of CBCT and helical CT in detecting osseous abnormalities (erosion and osteophytes) of the TMJ condyle by using 21 TMJ autopsy specimens; no significant difference was found between CBCT and helical CT in detecting erosion and osteophytes.16 The present study was done to compare the diagnostic accuracy between MDCT and CBCT and to examine the intraobserver and interobserver reliability of CBCT compared with MDCT.
Materials and methods
The sample consisted of 10 TMJs from 5 dried human skulls. They were obtained from the Anatomy Department, College of Medicine, King Saud University, Saudi Arabia. No demographic data were available for the skulls; they were not identified by age, sex or ethnicity. Temporal components and condyles of the 10 TMJs were evaluated morphologically and reported to be free from physical damage.
Gold standard case definitions
The following gold standard definitions were applied in assessing the TMJs:
(1) No osseous changes—rounded area with or without intact cortical bone.17
(2) Flattening—loss of convexity of the condyle, loss of concavity of the fossa, decrease in posterior slope of the tubercle eminence or shallow overall.17,18 If either the glenoid fossa was shallow or the posterior slope of the tubercle eminence was flat, the worst of these scenarios was scored as positive for flattening.
(3) Erosion—local area of bone defect or rarefaction in the layer of compact bone.17,19
(4) Osteophyte—local outgrowth of bone arising from the mineralized surface.15 Osteophytes usually appear on the anterosuperior surface of the condyle with a lack of cortical surface and thus only this site was observed in order to detect osteophytes.
For the gold standard observation session, the surfaces of the condyles, mandibular fossae and articular tubercles were examined for flattening, erosion and osteophytes by naked-eye inspection using white fluorescent illumination and a 3× magnifier. Each TMJ was inspected for the presence or absence of surface osseous changes according to the case definitions described earlier. Five anatomical sites in the condylar head and temporal bone were inspected for surface osseous changes. In the condylar head, surface osseous changes were observed in four anatomical sites: the lateral pole of the condyle, the medial pole of the condyle, the anterosuperior slope of the condyle and the posterosuperior slope of the condyle. In the temporal bone, the glenoid fossa and the tubercle eminence together were considered to be the fifth anatomical site to be observed.
A total of 110 sites were examined to detect surface osseous changes: 50 (5 sites of 10 TMJs) for flattening, the same 50 for erosion and 10 in the anterior slope of the condyle of 10 TMJs for osteophytes. Two blinded, trainee and calibrated oral maxillofacial radiologists with more than 5 years' experience did the data collection. For the gold standard, the two observers reached agreement if their detection of the osseous changes was different in any of these sites. In order to have data for intra- and interobserver reliability for MDCT and CBCT, Observer A performed two readings for each of the two modalities and Observer B performed one reading for each of the two modalities. The total number of images read by the 2 observers for the 2 modalities was 660.
Imaging the skulls
The maxilla and mandible were then mounted in centric occlusion with a rubber band around the skull and a cotton roll was used to support the occlusion in the edentulous skull. For imaging with CBCT, the skull was placed into a custom-made plastic box with dimensions of 20×20×20 cm (height×width×depth), which was filled with water to provide the equivalent of soft tissue attenuation.11,20,21 For scanning with MDCT, the skull was stabilized in a supine position with a plastic, open-sided rectangular base placed underneath the cranial bone to support the skull and prevent it from backward and sideways tilting. A piece of double-sided adhesive tape was used to separate the condyle from the glenoid fossa so that the outer surface of the condyle and the temporal bone could be clearly imaged. The skulls were then coded for each modality individually to blind the observers and imaged in a spiral MDCT scanner with 16 rows of detectors [Light Speed 2002; General Electric Company (GE), Fairfield, CA] (Figure 1a). The acquisition time for the axial slices was 1 rotation s−1 (i.e. 16 images s−1). The slice thickness was 1.25 mm with 0.625 mm spacing overlapping. The axial-z slope was 90°. The beam pitch was 0.562:1. The sectional images were acquired at 80 mA and 100 kV. The display field of view was 512×512 and 18 cm in bone resolution. 1-mm slices were generated in corrected sagittal and coronal views in which the sections were created through the long axis of the condyles. The images of each skull were then copied with a Centricity DICOM Viewer (GE) to a compact disc and labelled with its unique code. The images were later examined in the same monitor that was used for CBCT interpretation. The skull within its water-filled box was then imaged with a CBCT device (ILUMA; IMTEC, Ardmore, OK) with a flat panel detector (FPD) composed of 127 µm amorphous silicon (Figure 1b). The detector size was 19×24 cm and the focal spot size was 0.3 mm. 602 base images were acquired at 3.8 mA and 120 kVp. The reconstructed voxels were isotropic and 0.29 mm in all three dimensions. The reconstructed axial projection images were processed with reformatting software (ILUMA Vision 3D, version 1.0.2.5; IMTEC). Reformatted sagittal and coronal views were obtained by pressing the TMJ program icon. TMJ corrected lines were drawn along the long axis of the condyles; the spacing between the lines was 1 mm. The observers were free to manipulate the images interactively. For statistical analysis, the efficiency of the imaging modality was measured by sensitivity and specificity tests. The kappa test was performed with its p values to determine the extent of the agreements. All tests were done using Stata software (StataCorp LP, College Station, TX).
Figure 1.
Skull immersed in water. (a) Placed in supine position in the multidetector CT. (b) Placed in upright position in the cone beam CT
Results
The sensitivity and specificity of the two modalities for the three readings are listed in Table 1. Figure 2 shows examples of correctly detected osseous changes using both modalities.
Table 1. Sensitivity and specificity for the detection of surface osseous changes in condyles and temporal bone using MDCT and CBCT.
| Observer | Modality | reading | True+n=48 | True− n=62 | False positive | False negative | Sensitivity % | 95% CI | Specificity % | 95% CI |
| A | MDCT | 1st reading | 12 | 54 | 8 | 36 | 25 | 13.64–39.60 | 87.10 | 76.15– 94.26 |
| 2nd reading | 13 | 55 | 7 | 35 | 27.08 | 15.28–41.85 | 88.71 | 78.11–95.34 | ||
| CBCT | 1st reading | 19 | 52 | 10 | 29 | 39.58 | 25.77–54.73 | 83.87 | 72.33–91.98 | |
| 2nd reading | 11 | 56 | 6 | 37 | 22.92 | 12.03–37.31 | 90.32 | 80.12–96.37 | ||
| B | MDCT | 24 | 53 | 9 | 24 | 50 | 35.23–64.77 | 85.48 | 74.22–93.14 | |
| CBCT | 17 | 56 | 6 | 31 | 35.42 | 22.16–50.54 | 90.32 | 80.12–96.37 |
CBCT, cone beam CT; CI, confidence interval; MDCT, multidetector CT.
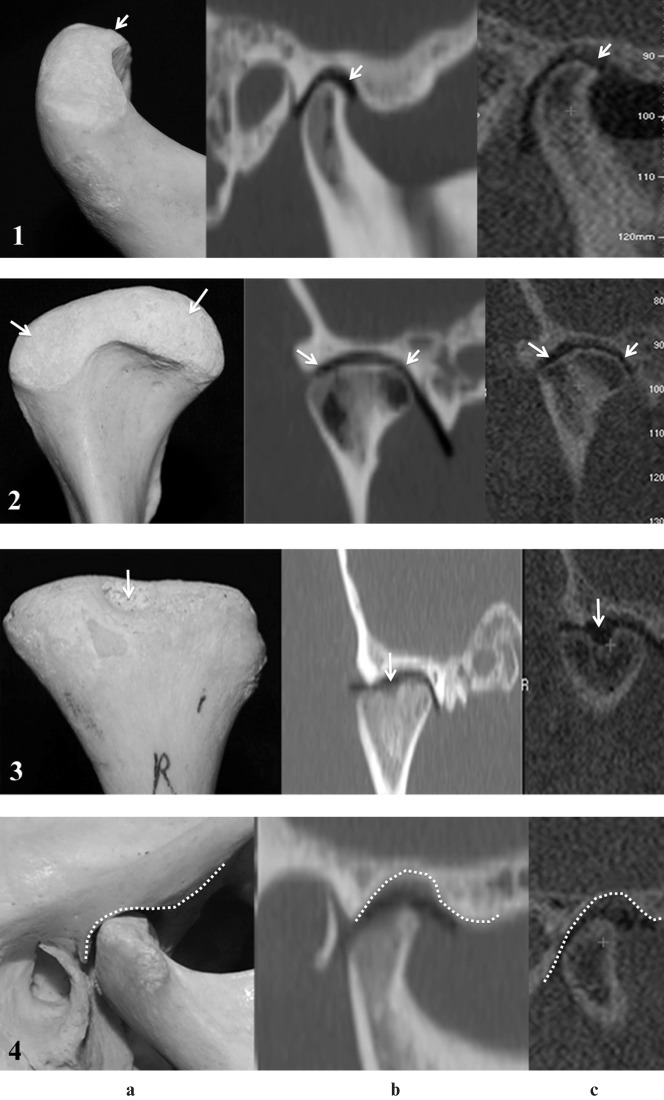
Figure 2.
Correctly detected surface osseous changes using both modalities. (1) Flattening in the anterosuperior slope of the condyle. (2) Flattening of the medial and lateral pole of the condyle. (3) Erosion. (4) Shallow fossa. (a) The gold standard; (b) multidetector CT; (c) cone beam CT
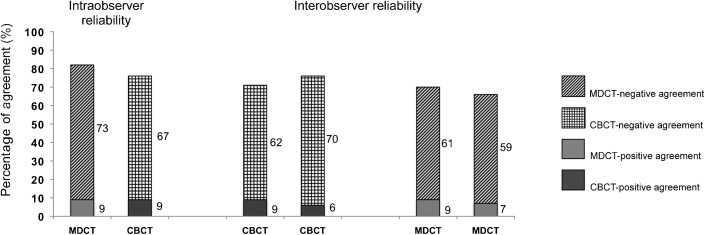
For the CBCT intraobserver reliability (Figure 3), the first and second readings were significantly correlated (p=0.0005; κ=0.30 with agreement of 76.36%). For the MDCT intraobserver reliability (Figure 3), the first and second readings were also significantly correlated (p=0.0001; κ=0.39 with agreement of 81.82%). For CBCT interobserver reliability (Figure 3), the first CBCT reading by Observer A significantly correlated with the CBCT reading of Observer B (p=0.0181; κ=0.20 with agreement of 70.91%) and the second CBCT reading by Observer A significantly correlated with the CBCT reading by Observer B (p=0.0127; κ=0.21 with agreement of 76.63%). For MDCT interobserver reliability (Figure 3), the first MDCT readings by Observer A significantly correlated with the MDCT readings by Observer B (p=0.0155; κ=0.20 with agreement of 70%), whereas the second MDCT reading of Observer A and the MDCT reading of Observer B were not significantly correlated (p=0.1403; κ=0.10 with agreement of 66%).
Figure 3.
The intraobserver reliability and interobserver reliability for both multidetector CT (MDCT) and cone beam CT (CBCT) in interpreting surface osseous changes of temporomandibular joints
Discussion
In this study, CBCT and MDCT were similarly effective in identifying surface osseous changes. The sensitivity of CBCT (22.92–39.58%) was slightly lower than that of MDCT (25–50%), with overlapping confidence intervals, whereas the specificity of MDCT (85.48–88.71%) was slightly lower than that of CBCT (83.87–90.32%), with overlapping confidence intervals. The highest sensitivity was 39.58% for CBCT and 50% for MDCT, with approximately 10% difference between the two modalities in detecting surface osseous changes in the TMJs.
Surface osseous changes were present in 10 TMJs in 48 of the 110 sites examined. On average, 23–50% of all readings were correctly identified. This finding is comparable with that in the study by Hintze et al,15 in which they reported that both tomography and CBCT were ineffective for identifying flattening defects and osteophytes and that condylar flattening was present in 40% of the 159 examined joints. On average, only 23–40% of their readings were identified correctly by assessing a combination of frontal and sagittal images.15
Agreement between helical CT and CBCT in detecting osseous changes in TMJs was investigated by Honda et al,16 who reported a sensitivity of 80% for CBCT compared with a sensitivity of 70% for helical CT. This finding is comparable with the present study, in which there was a 10% difference between the highest sensitivity scored for each modality. The overlap between the confidence intervals of the sensitivities for the two modalities indicates that they are comparable. In Honda's study, the overall sensitivity in detecting osseous changes in TMJs by both helical CT (70%) and CBCT (80%) was high compared with the present study, which had an overall lower range of sensitivities for both MDCT (25–50%) and CBCT (22.92–39.58%). The specificity in the study by Honda et al for both modalities was a perfect 100%. In the present study, the maximum specificity did not exceed 90.32%, but this finding is considered to be reasonably high.
The overall lower sensitivity for both imaging modalities may be due to the mild surface osseous changes of the TMJs in our sample. Mild changes are usually difficult to visualize radiographically,19 making the images more challenging and subjective to read and providing less true-positive identification. Another reason for lower sensitivity in the present study compared with that in Honda et al's study is that we immersed skulls in water as soft tissue compensation to resemble the clinical situation. The image quality and the interpretation is different between a mandible that is scanned dry and one that is scanned immersed in water.22 CT image quality is dependent upon balancing characteristics and parameters to produce the best possible image for the anatomical region being scanned. Image noise and artefacts are the two biggest enemies of CT image quality. Increasing the milliamp seconds or kilovolt peak decreases image noise, but an increase in patient dose occurs.23 In our study, we used the clinical situation protocol, a tube current of 80 mA and a tube voltage of 100 kV, whereas Honda et al used 80 mA and 120 kV, thus increasing exposure factors. In addition, scanning the skulls without soft tissue compensation may have produced images that had less noise in the study by Honda et al;24 hence, it was easier to detect osseous abnormalities with a higher sensitivity and specificity. Another main difference between the two studies is that Honda et al used CBCT with an image intensifier detector and compared it with helical unidetector CT (K Honda, August 2009, personal communication), whereas we used an FPD CBCT and compared it with MDCT. Thus, the parameters and physical descriptors that are commonly enlisted to characterize the quality of an image were somewhat different between the two studies. In CBCT, the advantages of FPD technology is that it typically affords greater spatial resolution with a relatively low patient dose when compared with the X-ray intensifier/charge-coupled device. Other studies, however, have claimed that CBCT image quality, regardless of the type of the detector, is comparable or even superior to MDCT.25
The difference in image display of the 16-row detector CT used in this study compared with the unidetector image display used in the study by Honda et al was examined in another study by Cara et al.4 They investigated the validity of single- and multislice CT for assessments of 15 dry mandibular condyles and found that the highest accuracy was obtained with multislice axial-associated multiplanar reconstructed images. This finding shows that MDCT allows high image quality from thinner slices (0.5 mm) than can be obtained with single-slice CT.4 This difference can be explained by the fact that the lesions with a depth of less than 1 mm were better detected with thinner slices. However, MDCT has a dose profile that is 27% higher than that of unidetector CT in the plane of imaging and 69% higher adjacent to the plane of imaging.26,27 This difference encourages the use of CBCT devices that are designed for the maxillofacial region with a substantially smaller radiation dose.
The intraobserver agreements with both modalities were significantly high. This observation was somewhat surprising because CBCT is more interactive during examination; it was expected to have less intraobserver reliability. This finding is comparable with that in the study by Hintze et al in which the variation in intraobserver agreement for all three observers for the assessment of the various changes of the TMJ was about the same for CBCT and tomography.15 The authors commented that this similarity occurred despite the observers' unfamiliarity with CBCT compared with tomography and concluded that CBCT images are very reader friendly and easy to familiarize oneself with.15
As seen from the results of the present study, the interobserver agreements for CBCT showed that both readings of Observer A correlated significantly with those of Observer B (p=0.0181 and 0.0127). However, for the interobserver agreement of MDCT, only one of the two readings of Observer A significantly correlated with the reading of Observer B (p=0.015). The second reading did not significantly correlate with that of Observer B, which could mean that the MDCT is operator dependent. A possible explanation is that the MDCT images can be reformatted to sagittal and coronal images only in the workstation and then transferred as fixed images. Thus, the interpretation depends only on the operator and what he or she can see from a previously designed protocol and previously reformatted images. The flexibility of CBCT software may help the operator to easily define osseous change when interpreting the images. Although there was high agreement in intraobserver and interobserver reliability, the kappa values were low (κ=0.20–0.40, which represents fair agreement). The kappa value in this study shows that agreement for positive findings was less than agreement for negative findings.
One of the limitations of the present study is that we examined only surface osseous changes without including other subcortical bone changes that appear in radiographs, such as sclerotic changes and subcortical degeneration within the condyle. From the results of other studies on the TMJ and other joints, researchers have hypothesized that changes in the subcortical tissues may constitute the primary change in osteoarthritis.17,28 These changes were excluded from our study because we do not have a gold standard to indicate positive detection. To do so, we would need to grind the cortical bone of the condyle and thus permanently damage the skulls. Another limitation is that the sample was small and the TMJs that we used had only mild to moderate osseous changes. If the sample were larger, there would be a greater probability of having a higher prevalence of all three types of surface osseous changes. Accordingly, it is possible to have lesion-specific sensitivity and specificity. For example, in a study by Hintze et al with a sample of 80 dry human skulls, they were able to have sensitivities for various types of osseous changes.15 The mean lesion-specific sensitivity was low (0.11 for flattening in tomography and 0.40 for erosion in CBCT). By contrast, the mean lesion-specific specificities were high (0.87 for flattening in tomography and 0.99 for osteophytes in tomography).15 Further research into this issue is recommended with a larger sample.
In conclusion, no difference was found between CBCT and MDCT for accuracy of detecting surface osseous changes. Both modalities had comparable intraobserver reliability. The more flexible reformatting capabilities of the software available for the end user in CBCT may have provided better interobserver reliability compared with MDCT.
Acknowledgment
The authors thank Dr Wafa Alfaleh, Assistant Professor in the Department of Oral Medicine and Diagnostic Sciences, King Saud University, Saudi Arabia, for her aid and efforts during the conduction of the study. The authors also thank Mr Mohammad Saeed, Head Radiology Technician at the College of Dentistry, King Saud University and Mr Kamal Al-Batsh, Head CT Technician at King Khalid University Hospital, Saudi Arabia, for their efforts during the conduction of the study.
References
- 1.Cohen H, Ross S, Gordon R. Computerized tomography as a guide in the diagnosis of temporomandibular joint disease. J Am Dent Assoc 1985;110:57–60 [DOI] [PubMed] [Google Scholar]
- 2.Lewis EL, Dolwick MF, Abramowicz S, Reeder SL. Contemporary imaging of the temporomandibular joint. Dent Clin North Am 2008;52:875–890, viii [DOI] [PubMed] [Google Scholar]
- 3.Honey OB, Scarfe WC, Hilgers MJ, Klueber K, Silveira AM, Haskell BS, et al. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: comparisons with panoramic radiology and linear tomography. Am J Orthod Dentofacial Orthop 2007;132:429–438 [DOI] [PubMed] [Google Scholar]
- 4.Cara AC, Gaia BF, Perrella A, Oliveira JX, Lopes PM, Cavalcanti MG. Validity of single- and multislice CT for assessment of mandibular condyle lesions. Dentomaxillofac Radiol 2007;36:24–27 [DOI] [PubMed] [Google Scholar]
- 5.Draenert FG, Coppenrath E, Herzog P, Muller S, Mueller-Lisse UG. Beam hardening artefacts occur in dental implant scans with the NewTom cone beam CT but not with the dental 4-row multidetector CT. Dentomaxillofac Radiol 2007;36:198–203 [DOI] [PubMed] [Google Scholar]
- 6.Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol 2004;33:196–201 [DOI] [PubMed] [Google Scholar]
- 7.Kobayashi K, Shimoda S, Nakagawa Y, Yamamoto A. Accuracy in measurement of distance using limited cone-beam computerized tomography. Int J Oral Maxillofac Implants 2004;19:228–231 [PubMed] [Google Scholar]
- 8.Lascala CA, Panella J, Marques MM. Analysis of the accuracy of linear measurements obtained by cone beam computed tomography (CBCT-NewTom). Dentomaxillofac Radiol 2004;33:291–294 [DOI] [PubMed] [Google Scholar]
- 9.Marmulla R, Wortche R, Muhling J, Hassfeld S. Geometric accuracy of the NewTom 9000 cone beam CT. Dentomaxillofac Radiol 2005;34:28–31 [DOI] [PubMed] [Google Scholar]
- 10.Hilgers ML, Scarfe WC, Scheetz JP, Farman AG. Accuracy of linear temporomandibular joint measurements with cone beam computed tomography and digital cephalometric radiography. Am J Orthod Dentofacial Orthop 2005;128:803–811 [DOI] [PubMed] [Google Scholar]
- 11.Ludlow JB, Laster WS, See M, Bailey LJ, Hershey HG. Accuracy of measurements of mandibular anatomy in cone beam computed tomography images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:534–542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hashimoto K, Arai Y, Iwai K, Araki M, Kawashima S, Terakado M. A comparison of a new limited cone beam computed tomography machine for dental use with a multidetector row helical CT machine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:371–377 [DOI] [PubMed] [Google Scholar]
- 13.Hashimoto K. Comparison of image validity between cone beam computed tomography for dental use and multidetector row helical computed tomography. Dentomaxillofac Radiol 2007;36:465–471 [DOI] [PubMed] [Google Scholar]
- 14.Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc 2006;72:75–80 [PubMed] [Google Scholar]
- 15.Hintze H, Wiese M, Wenzel A. Cone beam CT and conventional tomography for the detection of morphological temporomandibular joint changes. Dentomaxillofac Radiol 2007;36:192–197 [DOI] [PubMed] [Google Scholar]
- 16.Honda K, Larheim TA, Maruhashi K, Matsumoto K, Iwai K. Osseous abnormalities of the mandibular condyle: diagnostic reliability of cone beam computed tomography compared with helical computed tomography based on an autopsy material. Dentomaxillofac Radiol 2006;35:152–157 [DOI] [PubMed] [Google Scholar]
- 17.Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:844–860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiese M, Svensson P, Bakke M, List T, Hintze H, Petersson A, et al. Association between temporomandibular joint symptoms, signs, and clinical diagnosis using the RDC/TMD and radiographic findings in temporomandibular joint tomograms. J Orofac Pain 2008;22:239–251 [PubMed] [Google Scholar]
- 19.Flygare L, Rohlin M, Akerman S. Microscopy and tomography of erosive changes in the temporomandibular joint. An autopsy study. Acta Odontol Scand 1995;53:297–303 [DOI] [PubMed] [Google Scholar]
- 20.Lopes PM, Moreira CR, Perrella A, Antunes JL, Cavalcanti MG. 3-D volume rendering maxillofacial analysis of angular measurements by multislice CT. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:224–230 [DOI] [PubMed] [Google Scholar]
- 21.Jung H, Kim HJ, Kim DO, Hong SI, Jeong HK, Kim KD, et al. Quantitative analysis of three-dimensional rendered imaging of the human skull acquired from multi-detector row computed tomography. J Digit Imaging 2002;15:232–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suomalainen A, Vehmas T, Kortesniemi M, Robinson S, Peltola J. Accuracy of linear measurements using dental cone beam and conventional multislice computed tomography. Dentomaxillofac Radiol 2008;37:10–17 [DOI] [PubMed] [Google Scholar]
- 23.Bushong SC. Radiologic Science for Technologists. 6th edn Maryland Heights, MO: Mosby; 1997 [Google Scholar]
- 24.Bushberg JT, Seibert JA, Leidholdt EM, Jr, Boone JM. The Essential Physics of Medical Imaging. 2nd edn Philadelphia, PA: Lippincott Williams & Wilkins; 2002 [Google Scholar]
- 25.Liang X, Jacobs R, Hassan B, Li L, Pauwels R, Corpas L, et al. A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice CT (MSCT) Part I. On subjective image quality. Eur J Radiol 2010;75:265–269 [DOI] [PubMed] [Google Scholar]
- 26.Thomton FJ, Paulson EK, Yoshizumi TT, Frush DP, Nelson RC. Single versus multi-detector row CT: comparison of radiation doses and dose profiles. Acad Radiol 2003;10:379–385 [DOI] [PubMed] [Google Scholar]
- 27.Fuchs T, Kachelriess M, Kalender WA. Technical advances in multi-slice spiral CT. Eur J Radiol 2000;36:69–73 [DOI] [PubMed] [Google Scholar]
- 28.Katakami K, Shimoda S, Kobayashi K, Kawasaki K. Histological investigation of osseous changes of mandibular condyles with backscattered electron images. Dentomaxillofac Radiol 2008;37:330–339 [DOI] [PubMed] [Google Scholar]