Abstract
Objectives
The purpose of this study was to determine the accuracy and effectiveness of digital panoramic radiographs for pre-operative assessment of dental implants.
Methods
We selected 86 patients (221 implants) and calculated the length of the planned implant based on the distance between a selection of critical anatomical structures and the alveolar crest using the scaling tools provided in the digital panoramic system. We analysed the magnification rate and the difference between the actual inserted implant length and planned implant length according to the location of the implant placement and the clarity of anatomical structures seen in the panoramic radiographs.
Results
There was no significant difference between the planned implant length and actual inserted implant length (P > 0.05). The magnification rate of the width and length of the inserted implants, seen in the digital panoramic radiographs, was 127.28 ± 13.47% and 128.22 ± 4.17%, respectively. The magnification rate of the implant width was largest in the mandibular anterior part and there was a significant difference in the magnification rate of the length of implants between the maxilla and the mandible (P < 0.05). When the clarity of anatomical structures seen in the panoramic radiographs is low, the magnification rate of the width of the inserted implants is significantly higher (P < 0.05), but there is no significant difference between the planned implant length and actual inserted implant length according to the clarity of anatomical structures (P < 0.05).
Conclusions
Digital panoramic radiography can be considered a simple, readily available and considerably accurate pre-operative assessment tool in the vertical dimension for dental implant therapy.
Keywords: panoramic radiograph, dental implant
Introduction
Before dental implant surgery it is a prerequisite to assess the height of residual alveolar bone in the area where implants are to be placed, the location of the nasal floor and the maxillary sinus floor, the location of the mandibular canal, detection of lesions within the jaw bones, the interval to the adjacent dental roots and so on. Panoramic radiographs have been used frequently as a radiographic method for pre-implant evaluation and the preparation of treatment protocols. In addition, a linear tomogram may be used and recently the frequency of the application of CT for pre-implant evaluation has risen.
CT facilitates the understanding of bone thickness of the buccolingual side, three-dimensional (3D) maxillary sinus floor as well as nasal floor, the buccolingual position of the mandibular canal, and so on. Additionally, in cases where important anatomical structures cannot be detected clearly on panoramic radiographs, it may be of help while performing implant surgery.1-3 However, pre-implant CT is not required in all cases. In previous studies it has been shown that the use of panoramic radiographs is sufficient for evaluation before implant surgery. In particular, it was revealed that for measuring the height of residual alveolar bone for the placement of implants in the mandibular posterior region, without the use of CT, panoramic radiographs were sufficient4 and there was little difference from cases that used linear or spiral CT.5 In addition, the width of residual alveolar bone could be evaluated by clinical tests. The width of the alveolar ridge and the presence and extent of lingual undercuts in the edentulous region can be evaluated by manual examination of the superficial bone structures. If necessary, a more meticulous assessment could be done for an impression model.5
In comparison with CT and other expensive precision tests, panoramic radiography is rapid and inexpensive and its radiation dose is low. Furthermore, if metal prostheses, posts or pins are present, CT may generate streak artefacts. It also has the disadvantage that the patient should not move during the relatively long CT imaging period.6
This study was conducted to evaluate the efficacy and accuracy of cases in which pre-implant diagnosis as well as treatment protocols were prepared through the application of the digital panoramic radiation system without performing CT and other expensive precision tests.
Materials and methods
This study was conducted on 86 patients (50 male, 36 females). Between July 2007 and December 2007, 221 implants (124 in males, 97 in females) were consecutively placed at the dental clinic in the Seoul National University Bundang Hospital. All of the patients enrolled in this study were partially edentulous or had single missing teeth. Since dental implants cannot be located accurately in completely edentulous patients without the use of a radiographic stent, these patients were excluded from this study. The mean age of patients was 54.7 ± 12.5 years (Table 1).
Table 1. Age and gender distribution of participants.
| Age (years) | Males | Females | Total |
| 20–29 | 1 (1) | 3 (5) | 4 (6) |
| 30–39 | 2 (8) | 5 (7) | 7 (15) |
| 40–49 | 13 (28) | 2 (4) | 15 (32) |
| 50–59 | 10 (40) | 12 (18) | 22 (58) |
| 60–69 | 21 (41) | 11 (57) | 32 (98) |
| 70–79 | 3 (6) | 3 (6) | 6 (12) |
| Total | 50 (124) | 36 (97) | 86 (221) |
| Mean age (years) | 55.0 ± 11.3 | 53.8 ± 14.1 | 54.7 ± 12.5 |
Numbers in parentheses = no. of implants
On all patients, digital panoramic radiographs were taken before the treatment and after implant surgery. For 10 of the 86 patients, CT was also performed before surgery (4 males, 6 females). CT was performed in some cases depending on whether the surgeon decided:
the margins between the major anatomical structures were obscured on panoramic radiography;
major operations, such as bone grafting, were needed;
multiple dental implants were placed simultaneously on the left and right sides of the maxilla and mandible; or
the height of residual bone up to the level of the inferior alveolar canal was very insufficient.
The digital panoramic radiographic equipment used was the Orthopantomograph® OP100 (Instrumentarium Corp., Tuusula, Finland), and the CT equipment used was the MX 8000 IDT (Philips, Eindhoven, the Netherlands). All digital panoramic radiographs were taken by one technician according to the standard method provided by the manufacturer.
While standing, patients were asked to look at the equipment and then bite on the biting portion of the radiographic equipment using the anterior teeth; this established the location. As described, the Frankfort horizontal (FH) plane was placed parallel to the horizontal plane. This maintained a consistent head position.
On digital panoramic radiographs, the distance between anatomical structures as well as the length and width of placed implants were measured by the IMPAX® (Agfa, Belgium) system.
For each implant included in the research participants, the following factors were measured and analysed. Before treatment, one dentist subjectively determined the clarity of images shown on panoramic radiographs and classified them as good, moderate or poor. “Good” described cases in which the inferior alveolar canal, the mental foramen, the nasal floor and the maxillary sinus floor could be observed distinctly; “poor” included cases in which those structures could hardly be distinguished; and “moderate” were cases approximately in the middle. Any difference in clarity of the images of observed anatomical structures depending on gender or age was also examined. The implant length to be placed in the area was determined based on major anatomical structures.
The concurrence rate of the planned implant length to the implants actually placed, the magnification rate of panoramic radiographs and so on were analysed by one dentist, who did not participate in the surgery.
Concurrence rate of the length of implants planned before treatment to the length of actually placed implants
The length of the dental implants to be placed was determined by a single surgeon (YKK). Before treatment, one dentist measured the vertical length to major anatomical structures (location of the maxillary sinus floor, the nasal floor, the inferior alveolar canal, the mental foramen, etc.) on digital panoramic radiographs. Up to the level of the inferior alveolar canal and mental foramen of the mandible, the safe distance was set at 2 mm–5 mm. In the maxilla, where the sinus bone graft was performed, the safe distance was not significant. Dental implants > 10 mm in length were selected. The location of dental implants for a partial edentulous ridge was determined clinically, considering the adjacent and opposing teeth. Based on a magnification rate of 30%, stated by the manufacturer, the length of the dental implants to be placed was determined. No objects, such as radiographic stents, were used.
Magnification rate of the length and width of placed implant fixture on digital panoramic radiographs
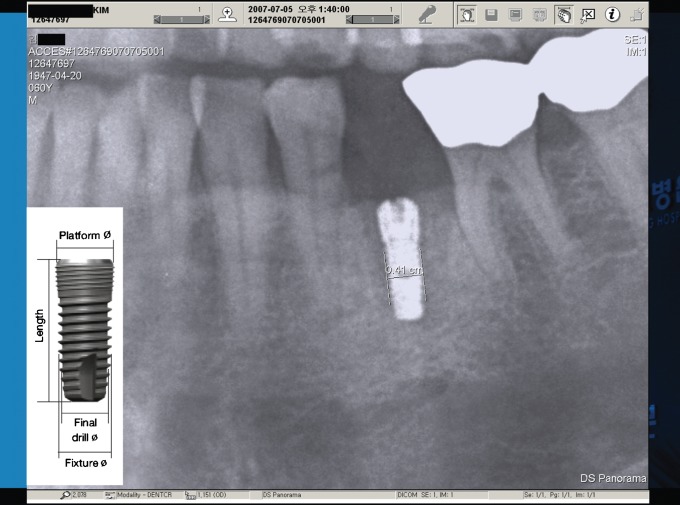
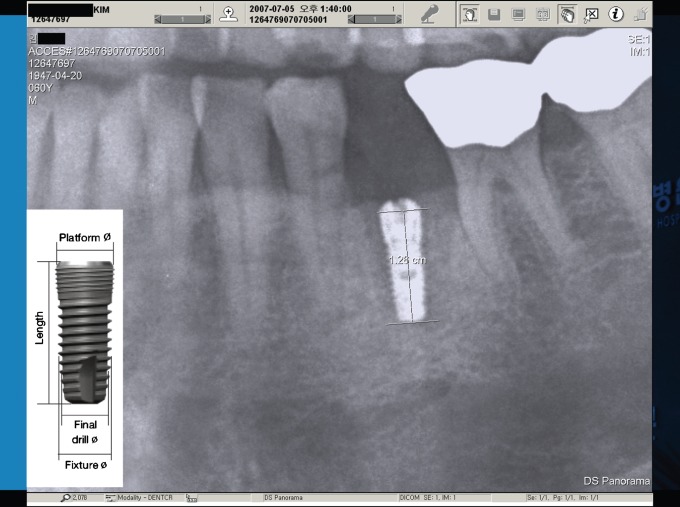
After implant surgery, based on the length and width of the implant fixture actually placed, the length and width of implants shown on post-surgical digital panoramic radiographs were measured by one dentist and the magnification rate of each placed area was calculated (Figures 1 and 2). The magnification rate was calculated by the following formulae:
Figure 1.
Measurement of implant width
Figure 2.
Measurement of implant length
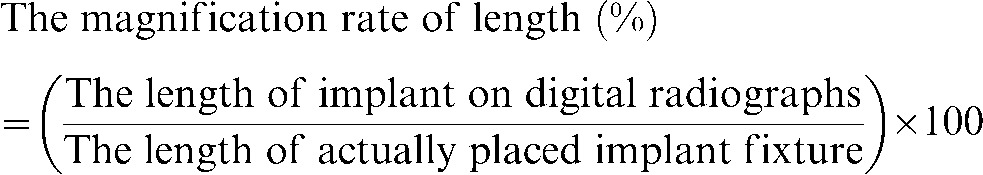 |
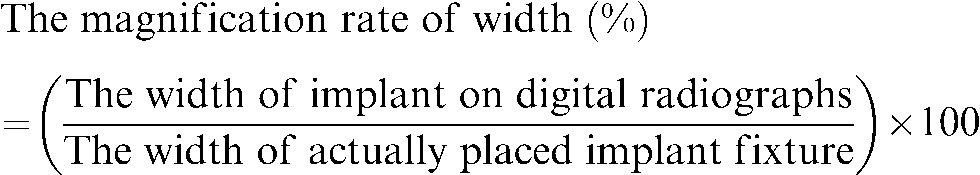 |
In addition, we assessed whether there was a difference in the magnification rate depending on the clarity level of the images of anatomical structures seen on panoramic radiographs. The magnified implant image shown on post-surgical panoramic radiographs is the image reflecting the placement of the implant inclined to the long axis of the buccolingual side, and thus it has a different meaning from cases imaged vertically to the direction of the radiation. By assessing the magnification rate of the width and length of already placed implants, in each placement area the magnification rate of digital panoramic radiographs was assessed by reflecting the placement angle of implants and was more clinically relevant.
70 implants were placed in the maxillary molar region, 45 implants in the maxillary premolar region, 24 implants in the maxillary anterior region, 55 implants in the mandibular molar region, 14 implants in the mandibular premolar region and 13 implants were placed in the mandibular anterior region. When the width and length of placed implants were measured on digital panoramic radiographs, the distance corresponding to the width and length of fixture suggested by the implant manufacturer was measured.
Comparison of patients additionally imaged by CT before surgery compared with patients imaged only by panoramic radiography
Cases imaged only by digital panoramic radiography before implant surgery (76 patients, 158 implants) were compared with cases additionally imaged by CT (10 patients, 63 implants) in terms of development of post-surgical dysaesthesia, the rate of replacement, maxillary sinus elevation and the frequency of performing bone graft.
Statistical analysis
SPSS 12.0 KO for windows release 12.0.1 program (SPSS Inc., Chicago, IL) was used at the 5% significant level. To examine whether the length of implant fixture planned before surgery was statistically different from the length of the actually placed implant fixture, the paired t-test was applied. In addition, to examine whether the planned length was significantly different from the placed length depending on gender and age, the t-test and ANOVA were applied. To examine whether the clarity of the images of anatomical structures seen on digital panoramic radiographs was different depending on gender and age, cross-tabulation analysis was applied.
The magnification rate of the mean width and length of placed implants as well as the magnification rate of the width and length of implants in each placement area were calculated, and ANOVA was used to examine whether the magnification rate of the width and length of implant in each placement area was statistically significantly different. The magnification rate of the width and length of the placed implant was analysed to see if there were significant differences depending on gender, age and clarity of the anatomical structures.
Results
Concurrence rate of the length of implant fixture planned before treatment to the length of actually placed implant fixture
The length of implant fixture planned before surgery was on average 11.59 ± 1.72 mm, and the length of the actually placed fixture was shown to be an average of 11.52 ± 1.61 mm. The result of the paired t-test was P = 0.446, and there was no statistically significant difference (Table 2).
Table 2. Mean and standard deviation of inserted implant length and planned implant length.
| Inserted implant length | Planned implant length | Sig. (two-tailed) | |
| Mean±SD | 11.523 ± 1.606 | 11.588 ± 1.716 | 0.446 |
SD, standard deviation; Sig, significance of paired t-test between inserted implant length and planned implant length
Similarly, according to each placement area, the planned length and the actually placed length was shown not to be significantly different (one-way ANOVA; P = 0.75; Tukey's test; Duncan analysis method).
The clarity of the image of anatomical structures on panoramic radiographs was classified as good, moderate or poor. The planned length of the fixture and the concurrence rate was compared with the actually placed length, and it was found that, according to the clarity of the image of anatomical structures, the concurrence rate was not significantly different (one-way ANOVA; P = 0.241). In addition, it was examined whether there was a difference in the clarity of the image of anatomical structures on panoramic radiographs depending on gender or age. It was found that the clarity of anatomical structures was different depending on gender (cross-tabulation analysis; P = 0.000). All 28 cases identified as “poor” who did not show anatomical structures clearly were female (Table 3). A significant difference according to age was not detected.
Table 3. Gender and radiographic clarity of anatomical structure.
| Clarity of anatomical structure | Male | Female | Total |
| Clearly seen | 96 | 46 | 142 |
| Moderately seen | 28 | 23 | 51 |
| Poorly seen | 0 | 28 | 28 |
| Total | 124 | 97 | 221 |
Significance of cross-tabulation analysis for gender and radiographic clarity of anatomical structure; P = 0.000
It was examined whether the planned length was significantly different from the placed length by t-test, and a significant difference between males and females was shown (P = 0.032) (Table 4). In males, the actually placed implant fixture was shorter than the length planned before surgery by an average of 0.371 mm, and in females the placed length was longer than the planned length by 0.139 mm. However, a significant difference between the planned length and the placed length according to age was not detected.
Table 4. Difference between inserted implant length and planned implant length by gender.
| Male | Female | Sig. (two-tailed) | |
| Mean±SD | −0.371 ± 1.898 | 0.139 ± 1.519 | 0.032* |
SD, standard deviation; Sig, significance of t-test for difference between inserted implant length and planned implant length by gender; *P < 0.05
Magnification rate of the width and length of placed implant fixture on digital panoramic radiographs
The magnification rate of the width of the placed implant fixture on the digital panoramic radiography system was an average of 127.28% ± 13.47%, and the magnification rate of the length was shown to be 128.22% ± 4.17%.
The result of the one-way ANOVA test showed that F = 29.503 and P = 0.000, the magnification rate of width was significantly different depending on the area, and the magnification rate of the length was also significantly different (F = 21.475 and P = 0.000) depending on the area. The groups showing a significant difference in the magnification rate of the width as well as the length are shown in Tables 5 and 6.
Table 5. Radiographic magnification rate of implant diameter by location.
| Implant fixture diameter (%) |
|||
| Location | n | mean | SD |
| Maxillary anterior | 24 | 129.63 | 12.10 |
| Maxillary premolar | 45 | 124.48 | 7.17 |
| Maxillary molar | 70 | 123.38 | 7.44 |
| Mandibular anterior | 13 | 159.07 | 25.03 |
| Maxillary premolar | 14 | 135.63 | 14.35 |
| Mandibular molar | 55 | 123.85 | 7.43 |
| Total | 221 | 127.28 | 13.47 |
| Sig. | 0.000* | ||
| Homogeneous subsetsa | ABCF < E < D | ||
n, number of implants inserted; mean, mean magnification rate; SD, standard deviation; sig, significance of one-way ANOVA of radiographic magnification rate of implants diameter by locations
aSubsets are symbolized as follows: A, maxillary anterior; B, maxillary premolar; C, maxillary molar; D, mandibular anterior; E, mandibular premolar; F, mandibular molar
*P < 0.05
Table 6. Radiographic magnification rate of implant length by location.
| Implant fixture diameter (%) |
|||
| Location | n | mean | SD |
| Maxillary anterior | 24 | 129.69 | 1.97 |
| Maxillary premolar | 45 | 130.55 | 2.38 |
| Maxillary molar | 70 | 129.83 | 2.59 |
| Mandibular anterior | 13 | 124.28 | 6.49 |
| Mandibular premolar | 14 | 125.73 | 4.66 |
| Mandibular molar | 55 | 125.17 | 4.03 |
| Total | 221 | 128.22 | 4.17 |
| Sig. | 0.000* | ||
| Homogeneous subsetsa | DEF < ABC | ||
n, number of implants inserted; mean, mean magnification rate; SD, standard deviation; sig, significance of one-way ANOVA of radiographic magnification rate of implants length by locations
aSubsets are symbolized as follows: A, maxillary anterior; B, maxillary premolar; C, maxillary molar; D, mandibular anterior; E, mandibular premolar; F, mandibular molar
*P < 0.05
The magnification rate of the width was divided into three groups; the mandibular anterior region was the largest, followed by the mandibular premolar area and other areas. The magnification rate of the length was divided into two groups, the maxilla and the mandible, and it was slightly more enlarged in the maxilla than the mandible.
The result of the one-way ANOVA test showed F = 6.146 and P = 0.003. Depending on the clarity of the image of anatomical structure on panoramic radiographs, the magnification level of the width of implant fixture was shown to be different, and in cases showing a “poor” clearness level, the magnification rate of width was shown to be significantly larger, while “good” and “moderate” did not show a significant difference (one-way ANOVA; Duncan analysis; Table 7). Nevertheless, it was found that the magnification rate of the length of implant fixture was not significantly different depending on the clarity of the image of anatomical structures.
Table 7. Radiographic magnification rate of implant diameter and clarity of anatomical structure.
| Implant fixture diameter (%) |
|||
| Clarity of anatomical structure | n | mean | SD |
| Clearly seen | 142 | 126.05 | 11.95 |
| Moderately seen | 51 | 126.22 | 12.75 |
| Poorly seen | 28 | 135.44 | 18.92 |
| Total | 221 | 127.28 | 13.47 |
| Sig. | 0.003* | ||
| Homogeneous subsetsa | AB < C | ||
n, number of implants inserted; mean, mean magnification rate; SD, standard deviation; sig, significance of one-way ANOVA of radiographic magnification rate of implants diameter and clarity of anatomical structure
aSubsets are symbolized as follows: A, clearly seen; B, moderately seen; C, poorly seen
*P < 0.05
It was shown that according to gender and age the magnification rate of the width and length of the images on radiographs was not significantly different (t-test; one-way ANOVA).
Comparison of cases additionally imaged by CT before surgery compared with patients imaged only by panoramic radiography
The rate of performing maxillary sinus elevation during the placement of maxillary implants in the group in which only panaromic radiographs were taken (Group 1) was 29.41%, and in the group in which CT images were additionally taken (Group 2) was shown to be 37.85%. In the maxilla and the mandible, the rate of performing bone grafts was 41.77% for Group 1, and 31.75% for Group 2 (Table 8). The result of Pearson's χ2 test showed that, regarding the rate of performing maxillary sinus elevation and bone graft, there was no significant difference between the group additionally imaged by CT and the group imaged only by the panoramic radiography (P = 0.587, P = 0.168).
Table 8. Comparison between pre-operative panoramic only group and CT group.
| Panoramic radiographs only | Pre-operative CT group | Sig. | |
| Sinus elevation (%) | 29.41 | 37.85 | 0.587 * |
| Bone graft (%) | 41.77 | 31.75 | 0.168 † |
| Inserted implants number per patient(m±SD) | 2.08 ± 1.56 | 6.30 ± 4.42 | 0.015 ** |
| Post-operative paraesthesia (case) | 0 | 1 | 0.116 ‡ |
| Reimplantation rate (%) | 1.27 | 6.34 | 0.057 § |
*Significance of Pearson's χ2 test between panoramic only group and additional CT group for sinus elevation per cent, †significance of Pearson's χ2 test between panoramic radiograph only group and the additional CT group for bone graft per cent, **significance of t-test between panoramic radiograph only group and the additional CT group for inserted implant number per patient, ‡significance of Fisher's exact test between panoramic radiograph only group and the additional CT group for post-operative paraesthesia, §significance of Fisher's exact test between panoramic radiograph only group and the additional CT group for reimplantation rate; *P < 0.05
Concerning the number of implants placed per individual, Group 1 had an average of 2.08 ± 1.55 implants, and Group 2 had an average of 6.3 ± 4.2 implants. Post-surgical dysaesthesia was not shown in Group 1, but was developed in one patient in Group 2. The rate of replacement was the result obtained at the time points, average 10 months after placement and average 5 months after the completion of the prosthesis. In Group 1, the replacement was performed in 2 cases (1.27%), and in the Group 2, 4 cases of the replacement (6.34%) were performed (Table 8).
In the group imaged only by panoramic radiography and the group additionally imaged by CT, the distribution according to the clarity level of the image of anatomical structure on panoramic radiographs is shown in Table 9. In the “poor” cases that did not show anatomical structures clearly on panoramic radiographs, the rate was highest in those additionally imaged by CT — 61% (cross-tabulation analysis; P = 0.000).
Table 9. Radiographic clarity of anatomical structure.
| Clarity of anatomic structure | Panoramic radiographs only group (%) | Pre-operative CT-group (%) |
| Clearly seen | 79 | 21 |
| Moderately seen | 69 | 31 |
| Poorly seen | 39 | 61 |
Significance of cross-tabulation analysis for the additional CT group and radiographic clarity of anatomical structure; P = 0.000
Discussion
Panoramic radiography is often the first choice method for the placement of implants because it provides information on the overall shape of the jaws, the position of the maxillary sinus floor and the nasal cavity floor, and the proximal distal as well as vertical position of the mandibular canal and the mental foramen. In addition, it provides information on the presence or absence of residual dental roots or asymptomatic lesions in the dental root apex, lesions within the bone, the interval between remaining teeth, etc. CT may also be necessary to assess the buccolingual position of anatomical structures or for simulation. By using digital panoramic radiography before implant surgery we were able to explain to the patient, on the radiograph, the position, method and length of the implant to be placed, using the drawing tools. Additionally, before surgery, the volume of residual alveolar bones was measured using the tools provided by the digital panoramic radiography system and a treatment protocol, such as the length of implant to be placed, could be established.
Digital panoramic radiographs have many advantages, such as minimal storage in comparison with film radiographs, explanation can be given to the patient in front of the monitor, the radiograph appears on the monitor immediately after imaging, the data can be copied readily, it can be easily measured and magnified using various tools, contrast can be controlled readily and the effective radiation dose is smaller in comparison with film panoramic radiography.7-9
If images are taken properly, by adjusting the position of patients, panoramic radiographs are sufficiently accurate for the measurement of vertical dimensions,5,7 and the results obtained by repeated vertical measurement of the jaws did not differ greatly.10 In a study using a metal ball, the vertical magnification rate on panoramic radiographs was shown to be a constant level of 127 ± 1%.5 In this study, the vertical enlargement ratio of placed implant fixtures was shown to be 128.22 ± 4.17%. These measurements were close to the magnification rate of 130% given by the manufacturer. In some cases there was a discrepancy between the estimated and actual implants; this may pose problems in a clinical setting.
In cases where the actual length of the implants exceeded the estimated length, maxillary autogenous bone grafting was performed simultaneously with dental implant placement in the maxillary molar region. When there was insufficient residual bone at the level of the mental foramen or inferior alveolar canal, the procedure was performed intra-operatively in a defensive manner. Accurate analysis based on a 3D imaging modality, such as CT, would reduce these errors further.
The effective radiation dose of panoramic radiography was 9 μSv; of linear cross-sectional tomography is 9 μSv; of conventional spiral cross-sectional tomography was 44–117 μSv; and of CT is 314–3324 μSv.9,11,12 Based on the effective radiation dose of standard digital panoramic radiography and the effective dose of CT, the hypothetical mortality risk was obtained. The result showed that the mortality risk of standard digital panoramic radiography was 1.05 × 10−6, while the mortality risk of CT in maxillary cases was 28.20 × 10−6 and in mandibular cases was 18.20 × 10−6; this was substantially higher than standard radiography.9
Panoramic radiography can measure the vertical dimension of the jaws relatively accurately using a lower effective dose. However, horizontal (mesiodistal) images can become distorted on panoramic radiographs.13 Such distortion can be seen abundantly in the anterior tooth area because the curvature level of the jaw is different in each individual and can be influenced by patient position during imaging.13 In this study, the diameter of the placed implant was enlarged mostly in the mandibular anterior area; however, this was not significantly different from other areas. According to the results from a study examining the enlargement ratio of implants in each area using panoramic tomography, the vertical enlargement ratio was between 1.21 and 1.29, and the horizontal enlargement ratio was between 1.12 and 1.44. In particular, the enlargement ratio for width was shown to be high in the mandibular anterior area of the coronal end of the implants.14
Occasionally, the mandibular canal may not be shown distinctly on panoramic radiographs. This is because the inferior alveolar neurovascular bundle is not surrounded by the compact cortical lining in all patients.13 The mandibular canal may also not be detected in diseases such as Gaucher's disease. Older people may show a thinning of the cortical bone wall in the mandibular canal because bone density is lower in older people than in younger people, which can be due to the menopause.15 It can also be affected by gender, as resorption of the superior border of the mandibular canal is detected more often in females (32.6%) than in males (9.8%).13 Similarly, in this study, depending on whether anatomical structures such as the superior and inferior border of the inferior alveolar nerve canal, the maxillary sinus floor and nasal cavity floor were shown clearly on panoramic radiographs, they were classified as good, moderate or poor. There were 28 poor cases and all these were female. In this study, we found no significant difference depending on age in the clarity of anatomical structures. In cases where the mandibular canal could not be detected clearly by panoramic radiography, by application of conventional tomography or by CT meant that the vertical position or the buccolingual position of the mandibular canal could be assessed. CT scans also provided information on bone volume and bone contour such as vestibular concavity, lingual undercuts and cortical defaults.
In cases that used linear tomography, it has been reported that the distance to the mandibular canal could be overevaluated by up to 219.1%.15 However, other studies have reported it to be underevaluated and thus it is still controversial. At present, CT scans are not the only way to obtain accurate information on 3D examination. Cone beam CT (CBCT) is a relatively new technique that imparts lower radiation to oral tissues, but has higher spatial resolution than conventional CT and provides a better quality image. Although it may be limited in its discrimination of soft tissue because of its low contrast resolution, it can provide detailed information about cortical thickness and contour. The advantages of CBCT have been established; however, at our medical institution, where this study was conducted, CBCT is not available16,17 and therefore the use of conventional CT was unavoidable.
In this study, cases with poor levels of clarity of anatomical structures on radiographs were also imaged by CT more frequently than cases which were good or moderate. In cases imaged only by panoramic radiography, post-surgical dysaesthesia was not developed, and temporary dysaesthesia was developed in only one patient additionally imaged by CT. In the group imaged only by panoramic radiography, replacement was performed in two cases (1.27%) and in four cases in the group imaged by CT additionally (6.34%). It is speculated that the group imaged additionally by CT did not have a sufficient volume of residual alveolar bone to major anatomical structures, and invasive surgery such as bone graft in a wide area was performed frequently, and thus more complications such as nerve injury and the failure of implants were developed.
This study examined the clinical usefulness of digital panoramic radiography, which allows general practitioners to diagnose and plan the treatment for dental implants easily. Accordingly, the advantages of CT may be underestimated; for example, CT can make a 3D assessment and can also be used to establish a guided, non-invasive surgical protocol. Obviously, CBCT has the advantage over conventional CT, resulting in less radiation exposure; however, the use of CT is not recommended in all implant cases. It may also be valuable in determining the diagnostic limitations and clinical usefulness of panoramic radiography, which can be performed easily in dental practice.
In conclusion, the digital panoramic radiography system is an effective method that is simple and inexpensive for pre-implant diagnosis and establishing treatment protocol, and it uses a relatively low radiation exposure. The vertical assessment can provide useful, accurate information, however, cross-sectional information cannot be obtained.
For cases that do not show major anatomical structures distinctly on panoramic radiographs, CT can also be used. Cases that did not show anatomical structures distinctly on panoramic radiographs were seen more frequently in females.
On panoramic radiographs, the vertical enlargement ratio of placed implants was shown to be constant in most cases. It had a tendency to be enlarged slightly more in the maxilla than the mandible, and in the horizontal enlargement ratio it showed a tendency to be enlarged more in the mandibular anterior area than in other areas.
Acknowledgements
This research was supported by the National Research Foundation of Korea (NRF), funded by the Ministry of Education, Science and Technology (R13-2008-010-00000-0).
References
- 1.de Oliveira RC, Leles CR, Normanha LM, Lindh C, Ribeiro-Rotta RF. Assessments of trabecular bone density at implant sites on CT images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:231–238 [DOI] [PubMed] [Google Scholar]
- 2.Terakado M, Hashimoto K, Arai Y, Honda M, Sekiwa T, Sato H. Diagnostic imaging with newly developed ortho cubic super-high resolution computed tomography (Ortho-CT). Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;89:509–518 [DOI] [PubMed] [Google Scholar]
- 3.Bianchi J, Goggins W, Rudolph M. In vivo, thyroid and lens surface exposure with spiral and conventional computed tomography in dental implant radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:249–253 [DOI] [PubMed] [Google Scholar]
- 4.Vazquez L, Saulacic N, Belser U, Bernard JP. Efficacy of panoramic radiographs in the pre-operative planning of posterior mandibular implants: a prospective clinical study of 1527 consecutively treated patients. Clin Oral Implants Res 2008;19:81–85 [DOI] [PubMed] [Google Scholar]
- 5.Frei C, Buser D, Dula K. Study on the necessity for cross-section imaging of the posterior mandible for treatment planning of standard cases in implant dentistry. Clin Oral Implants Res 2004;15:490–497 [DOI] [PubMed] [Google Scholar]
- 6.Cho YS. Diagnostic value of dental CT (DentaScan) in dental implant. Chungbuk Med J 1998;8:11–19 [Google Scholar]
- 7.Tal H, Moses O. A comparison of panoramic radiography with computed tomography in the planning of implant surgery. Dentomaxillofac Radiol 1991;20:40–42 [DOI] [PubMed] [Google Scholar]
- 8.Lecomber AR, Yoneyama Y, Lovelock DJ, Hosoi T, Adams AM. Comparison of patient dose from imaging protocols for dental implant planning using conventional radiography and computed tomography. Dentomaxillofac Radiol 2001;30:255–259 [DOI] [PubMed] [Google Scholar]
- 9.Dula K, Mini R, van derStelt PF, Buser D. The radiographic assessment of implant patients: decision-making criteria. Int J Oral Maxillofac Implants 2001;16:80–89 [PubMed] [Google Scholar]
- 10.Larheim TA, Svanaes DB. Reproducibility of rotational panoramic radiography: mandibular linear dimensions and angles. Am J Orthod Dentofacial Orthop 1986;90:45–51 [DOI] [PubMed] [Google Scholar]
- 11.Dula K, Mini R, van derStelt PF, Sanderink GC, Schneeberger P, Buser D. Comparative dose measurements by spiral tomography for preimplant diagnosis: the Scanora machine versus the Cranex Tome radiography unit. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;91:735–742 [DOI] [PubMed] [Google Scholar]
- 12.Scaf G, Lurie AG, Mosier KM, Kantor ML, Ramsby GR, Freedman ML. Dosimetry and cost of imaging osseointegrated implants with film-based and computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;83:41–48 [DOI] [PubMed] [Google Scholar]
- 13.BouSerhal C, Jacobs R, Quirynen M, van Steenberghe D. Imaging technique selection for the pre-operative planning of oral implants: a review of the literature. Clin Implant Dent Relat Res 2002;4:156–172 [DOI] [PubMed] [Google Scholar]
- 14.Gomez-Roman G, Lukas D, Beniashvili R, Schulte W. Area-dependent enlargement ratios of panoramic tomography on orthograde patient positioning and its significance for implant dentistry. Int J Oral Maxillofac Implants 1999;14:248–257 [PubMed] [Google Scholar]
- 15.Butterfield KJ, Dagenais M, Clokie C. Linear tomography's clinical accuracy and validity for presurgical dental implant analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;84:203–209 [DOI] [PubMed] [Google Scholar]
- 16.Schulze D, Blessman M, Pohlenz P, Wagner KW, Heiland M. Diagnostic criteria for the detection of mandibular osteomyelitis using cone-beam computed tomography. Dentomaxillofac Radiol 2006;35:232–235 [DOI] [PubMed] [Google Scholar]
- 17.Guerrero M, Jacobs R, Loubele M, Schutyser F, Suetens P, van Steenberghe D. State-of-art on cone beam CT imaging for pre-operative planning of implant placement. Clin Oral Investig 2006;10:1–7 [DOI] [PubMed] [Google Scholar]