Abstract
Objective
The aim of this study was to evaluate the efficacy of ultrasonography in the diagnosis of swellings in the head and neck regions.
Methods
For this study, 70 cases with clinically obvious swellings in head and neck regions were selected randomly. The ultrasonographic features considered were shape, boundary, echo intensity, ultrasound architecture of lesion, posterior echoes and ultrasound characteristic of tissues. Intergroup comparisons were made between four different types of swellings: inflammatory; cystic; benign; and malignant.
Results
A comparison was made between benign and malignant neoplasms, and the criteria of boundary, echo intensity and ultrasound architecture of lesions are statistically significant as the P-value is <0.05. The comparison of inflammatory swellings and malignant neoplasms shows that criteria of boundary and ultrasound architecture of lesions are statistically significant. The comparison of cystic swellings and benign neoplasms concluded that only the criterion of ultrasound characteristics of tissues is statistically significant. The comparison of inflammatory swellings and benign neoplasms shows that the criteria of boundary and echo intensity are statistically significant. The comparison of inflammatory swellings and cystic swellings concluded that the criteria of boundary, shape, echo intensity, posterior echoes and ultrasound characteristics of tissues are statistically significant. The comparison of cystic swellings and malignant neoplasms concluded that the criteria of ultrasonography, boundary, shape, echo intensity, ultrasound architecture of lesion, posterior echoes and ultrasound characteristics of tissues are statistically significant as the P-value is <0.05.
Conclusion
It can be concluded that clinical diagnosis had a sensitivity and accuracy of 85.7% and ultrasonographic diagnosis had a sensitivity and accuracy of 98.5%.
Keywords: ultrasonography, swelling, echo intensity, posterior echoes
Introduction
“Sonography” means imaging with ultrasound; “ultra” means beyond or in excess; “sound” means audible sound energy. The term ultrasound means the form of sound energy beyond audible range. Ultrasound used for diagnostic purposes has a frequency of 2 MHz–20 MHz while ultrasound used for ophthalmology has a range of 2 MHz–50 MHz.1,2
Ultrasound wave is a form of longitudinal mechanical wave that needs a medium to transmit from one place to another. Ultrasound is produced by vibrating piezoelectric crystals using a high-frequency electrical pulse which causes mechanical oscillation and produces ultrasound waves. Therefore, electrical energy is converted into mechanical energy. Diagnostic ultrasound utilizes a transducer which generates a narrow focus beam. This beam is reflected from the tissue and sent back to the same transducer, which assembles these echoes into an image that can be visualized and recorded.1,2
Ultrasonography has several advantages over other modalities as it is harmless, uses no ionizing radiation, is widely available, easy-to-use, non-invasive, inexpensive and unaffected by metal artefacts such as dental restorations. It can be performed without heavy sedation. Ultrasound causes no health problems and may be repeated as often as necessary.
In ultrasonography, there is the facility of on-screen nodal measurement.3 Ultrasound is capable of differentiating cystic from solid lesions and is also helpful in diagnosing malignant vs benign masses. It is helpful in delineating the presence of multiple lymph nodes and the course of resolution of infectious diseases. It is used to visualize the presence and extent of facial abscesses. It can be used in cases of oral carcinoma to observe the presence of regional lymph node metastasis. Ultrasound is helpful in detecting sialoliths and in the diagnosis of conditions involving the salivary gland. CT is used for parapharyngeal space.4
Various disease processes may affect head and neck regions, which present clinically as swellings. The disease processes which lead to such types of swellings can be broadly classified as inflammatory, cystic, benign or malignant in nature.
In evaluation of such swellings, detailed case history and clinical examination are the most important and mandatory steps. But in some cases, such as chronic inflammation, abscess formation, deep-seated or infected cystic lesion and neoplasms, clinical examination and palpation do not provide complete assessment of the exact origin and nature of swellings; such cases require radiological imaging. Therefore, to get a final diagnosis, clinical examination must be joined with various investigative procedures.
In the present study, an attempt has been made to evaluate the efficacy of ultrasonography in the process of arriving at the diagnosis of swelling in the head and neck region. In this research study, sensitivity, specificity, positive predictive value, negative predictive value and accuracy of the test were calculated in inflammatory, cystic, benign and malignant swellings.
The aim of this study was to compare the ultrasonographic differentiation of inflammatory swellings, cystic swellings, benign neoplasms and malignant neoplasms with each other in head and neck regions. Intergroup comparison was also carried out in the study.
Material and methods
The protocol of this study was approved by the institutional ethical committee. The study was conducted during 2006–2008.
Inclusion criteria: for this single blind cross-sectional study, 70 cases with clinically obvious swellings in head and neck regions were selected randomly, with the age range of 8–70 years. Age limitation was not considered and male-to-female ratio was 3:2.
Exclusion criteria: swellings owing to trauma or fracture were not included because clinical diagnosis of haematoma is not a problem as there is history of trauma and changes in skin colour and mucous membrane.
Swellings obscured by an overlying jaw bone were not included, e.g. any pathology present in the deep lobe of the parotid gland not seen on the ultrasound as it is obscured by the ramus of the mandible.
Patients were informed about the procedures and written consent forms were obtained.
The patients’ detailed case history was recorded and clinical examinations were carried out on the basis of criteria given by Das.5 Criteria include inspection of swellings and palpation of swellings. In inspection, situation, colour, shape, size, border, surface and overlying skin over the swelling were noted; in palpation, consistency, tenderness, temperature, fluctuance, compressibility and fixity of skin over the swelling were recorded.
The data obtained were recorded in the structured proforma for recording clinical findings and a provisional diagnosis was made.
Based on clinical diagnosis, swellings were divided into four groups:
inflammatory swelling;
cystic swellings;
benign neoplasms; and
malignant neoplasms.
After provisional diagnosis, patients were subjected to radiological imaging. An ultrasonographic investigation of each swelling was carried out in the Department of Radiodiagnosis using Philips Envisors C Series (Sarrone, Italy) of ultrasonogram. When the lesion was less than 3.5 cm in diameter, a linear transducer probe with a frequency of 15 MHz and a depth of 3 cm was used. A transcavitary probe with a frequency of 7.5 MHz and a depth of 8 cm was used when the lesion was larger than 3.5 cm in diameter. In this study, different values of frequency were used because as frequency of ultrasound increases, depth of penetration of ultrasound decreases (thereby reducing the visibility range of ultrasounds). At the same time as frequency increases, resolution increases. For better resolution, 15 MHz was used.
The following features were considered in describing the ultrasonographic images of swelling in the head and neck in accordance with Shimizu et al:6
shape: oval, lobular, round, polygonal, irregular;
boundary: very clear, relatively clear, partially unclear, ill defined;
echo intensity: anechoic, isoechoic, hypoechoic, hyperechoic, mixed;
ultrasound architecture of lesion: homogeneous, heterogeneous;
presence of necrosis: eccentric, central;
presence of calcification: macrocalcification, microcalcification;
posterior echoes: enhanced, unchanged, attenuated; and
ultrasound characteristic of tissues: cystic, solid, mixed.
All the sonographic images obtained were interpreted by three qualified sonologists in the Department of Radiodiagnosis. After unanimous agreement, a report was given by the senior sonologist.
Following clinical and ultrasonographic diagnosis, surgical intervention was carried out by incision and drainage or excision/incisional biopsy/fine-needle aspiration cytology as indicated. The obtained biopsy specimens were submitted for histopathological examination and a final diagnosis was made. In cases of inflammatory swellings, a blood picture was carried out and final diagnosis was established on the basis of response of either surgical intervention, i.e. incision and drainage, or successful non-surgical treatment.
The obtained results were tabulated and statistically analysed. Sensitivity, specificity, positive predictive value, negative predictive value and accuracy of the test were calculated to evaluate the reliability and diagnostic efficacy of ultrasonography as an investigative tool.
Results
A total of 70 patients with clinically obvious swellings in head and neck regions were included in the study (Table 1).
Table 1. Distribution of types of swellings (70 patients) in head and neck regions.
| Diseases | No. of patients | Percentage |
| Inflammatory swelling | 35 | 50 |
| Cystic swelling | 8 | 11.4 |
| Benign neoplasms | 9 | 12.8 |
| Malignant neoplasms | 18 | 25.7 |
| Total | 70 | 100 |
Out of 35 cases, 30 swellings were finally diagnosed as inflammatory swellings by carrying out ultrasonography and surgical intervention investigations.
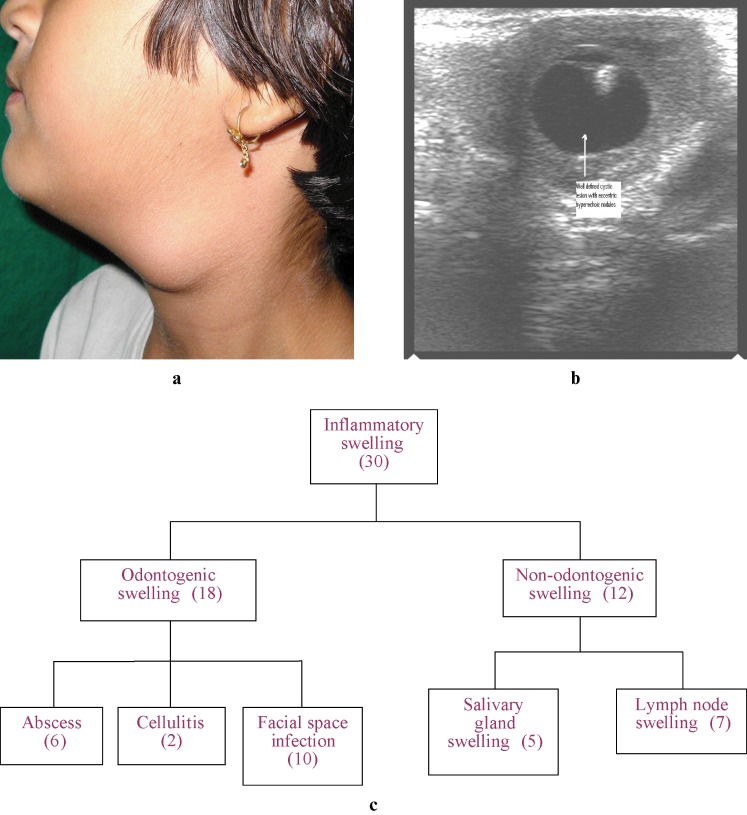
Inflammatory swellings
Inflammatory swellings that showed signs of inflammation from odontogenic origin (18 out of 30) were diagnosed as cellulites or abscesses. The remaining inflammatory swellings were from non-odontogenic origin (12 out of 30). Out of these 12 inflammatory swellings of non-odontogenic origin, 5 were diagnosed as sialadenitis as they originated from salivary glands and the remaining 7 were diagnosed as lymphadenitis as they originated from lymph nodes. In five patients, clinical diagnosis did not match with final diagnosis, and in one case sonographic diagnosis did not match with final diagnosis.
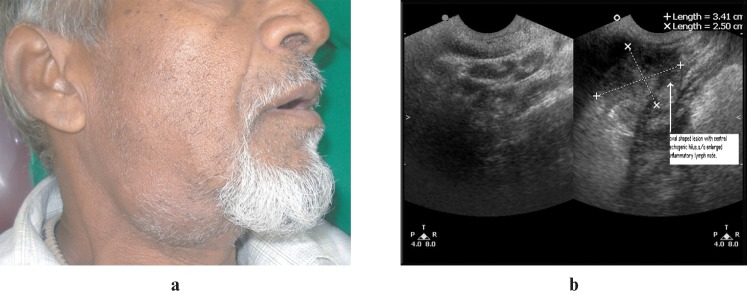
By considering ultrasonographic features given by Shimizu et al,6 in this study most of the inflammatory swellings had relatively clear boundaries, irregular shapes, hypoechoic echo intensity and homogeneous ultrasound architecture of lesion. The posterior echoes appeared enhanced and ultrasound characteristics of tissues were cystic or solid in nature (Table 2, Figures 1 and 2).
Table 2. Ultrasonographic features of inflammatory swellings—total (35).
| Greyscale sonographic features | Inflammatory swellings | No. | Percentage |
| Boundary | Very clear | 12 | 34.2 |
| Relatively clear | 18 | 51.4 | |
| Partially unclear | – | – | |
| Ill defined | 5 | 14.2 | |
| Shape | Oval | 13 | 37.1 |
| Lobular | 3 | 8.5 | |
| Polygonal | – | – | |
| Irregular | 15 | 42.8 | |
| Round | 4 | 11.4 | |
| Echo intensity | Anechoic | 11 | 31.4 |
| Isoechoic | 6 | 17.1 | |
| Hypoechoic | 15 | 42.8 | |
| Hyperechoic | – | – | |
| Mixed (hypo + hyper) | 3 | 8.5 | |
| Ultrasound architecture of lesion | Homogeneous | 23 | 65.7 |
| Heterogeneous | 12 | 34.2 | |
| Posterior echoes | Enhanced | 17 | 48.5 |
| Unchanged | 12 | 34.2 | |
| Attenuated | 5 | 14.2 | |
| Unenhancement | 1 | 2.8 | |
| Ultrasound characteristic of tissues | Cystic | 15 | 42.8 |
| Solid | 16 | 45.7 | |
| Mixed | 4 | 11.4 |
Figure 1.
(a) Inflammatory swelling—submandibular lymphadenitis (clinical photograph). (b) Inflammatory swelling—submandibular lymphadenitis (ultrasonographic image)
Figure 2.
(a) Inflammatory swelling—cysticercosis cellulosae (clinical photograph). (b) Inflammatory swelling—cysticercosis cellulosae (ultrasonographic image). (c) Flow chart of inflammatory swelling
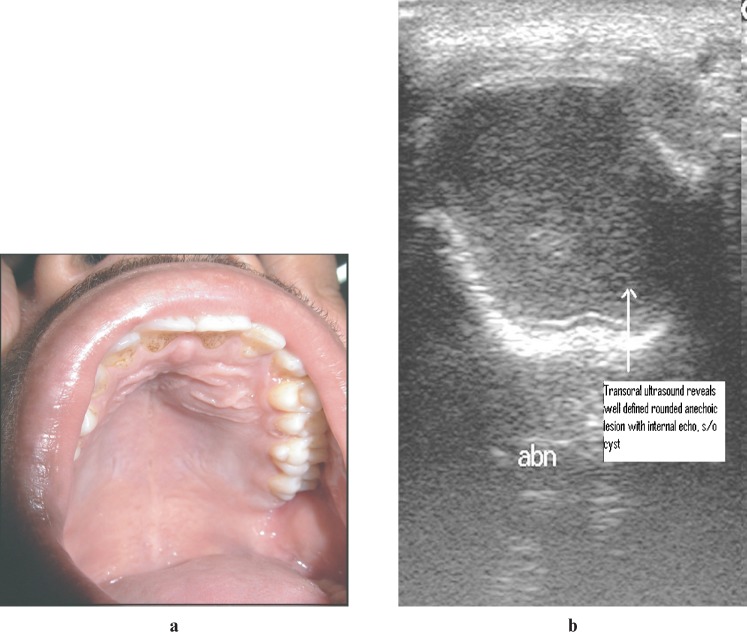
Cystic swelling
Out of the total eight cases of cystic swellings, six swellings were diagnosed as odontogenic cysts and two as non-odontogenic cysts by carrying out ultrasonography and surgical intervention investigations.
In two out of eight cases, clinical diagnosis did not match with final diagnosis, whereas all the sonographic diagnoses matched with final diagnosis.
In the present study, most of cystic swellings had very clear boundaries, round shapes and anechoic echo intensity. The ultrasound architecture of lesions of cystic swellings was homogeneous, posterior echoes appeared enhanced and ultrasound characteristic of tissues of cystic swellings were cystic in nature. Fine-needle aspiration was done in cystic cases (Table 3, Figure 3).
Table 3. Ultrasonographic features of cystic swellings—total (8).
| Greyscale sonographic features | Cystic swellings | No. | Percentage |
| Boundary | Very clear | 8 | 100 |
| Relatively clear | |||
| Partially unclear | |||
| Ill defined | |||
| Shape | Oval | 3 | 37.5 |
| Lobular | |||
| Polygonal | |||
| Irregular | |||
| Round | 4 | 50 | |
| Tubular | 1 | 12.5 | |
| Echo intensity | Anechoic | 7 | 87.5 |
| Isoechoic | |||
| Hypo + anechoic | 1 | 12.5 | |
| Hyperechoic | |||
| Ultrasound architecture of lesions | Homogeneous | 7 | 87.5 |
| Heterogeneous | 1 | 12.5 | |
| Posterior echoes | Enhanced | 8 | 100 |
| Unchanged | |||
| Attenuated | |||
| Ultrasound characteristic of tissues | Cystic | 8 | 100 |
| Solid | |||
| Mixed |
Figure 3.
(a) Cystic swelling—infected dental cyst (clinical photograph). (b) Cystic swelling—infected dental cyst (ultrasonographic image)
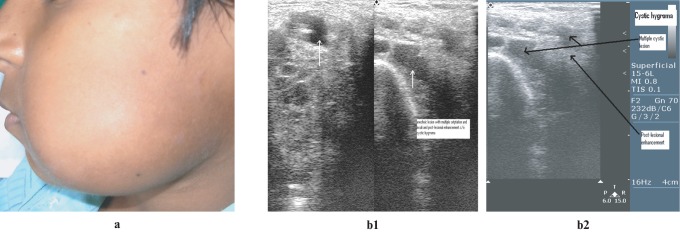
Benign neoplasm
Out of the total nine cases of benign neoplasms, seven swellings were finally diagnosed as benign neoplasms by carrying out ultrasonography and surgical intervention investigations.
Out of these seven cases of benign neoplasms, one case was of cavernous haemangioma, two cases were of capillary haemangioma, two cases were of lymphangioma, one case was of lipoma and one case was of fibroma. In two out of nine patients, clinical diagnoses did not match with final diagnosis, whereas all the sonographic diagnoses matched with final diagnosis.
Most benign neoplasms had very clear boundaries, irregular shapes and hypoechoic echo intensity. The ultrasound architecture of lesions of benign neoplasms was homogeneous, posterior echoes appeared enhanced and ultrasound characteristics of tissues were solid in nature (Table 4, Figure 4).
Table 4. Ultrasonographic features of benign neoplasms—total (9).
| Greyscale sonographic features | Benign neoplasms | No. | Percentage |
| Boundary | Very clear | 7 | 77.7 |
| Relatively clear | |||
| Partially unclear | |||
| Ill defined | 2 | 22.2 | |
| Shape | Oval | 2 | 22.2 |
| Lobular | 1 | 11.1 | |
| Polygonal | |||
| Irregular | 5 | 55.5 | |
| Round | 1 | 11.1 | |
| Echo intensity | Anechoic | 2 | 22.2 |
| Isoechoic | |||
| Hypoechoic | 3 | 33.3 | |
| Hypo + anechoic | 1 | 11.1 | |
| Hyperechoic | 3 | 33.3 | |
| Ultrasound architecture of lesion | Homogeneous | 6 | 66.6 |
| Heterogeneous | 3 | 33.3 | |
| Posterior echoes | Enhanced | 7 | 77.7 |
| Unchanged | 1 | 11.1 | |
| Attenuated | 1 | 11.1 | |
| Ultrasound characteristic of tissues | Cystic | 2 | 22.2 |
| Solid | 6 | 66.6 | |
| Mixed | 1 | 11.1 |
Figure 4.
(a) Benign neoplasm—cystic hygroma (clinical photograph). (b1) Benign neoplasm—cystic hygroma (ultrasonographic image). (b2) Benign neoplasm—cystic hygroma (ultrasonographic image)
Malignant neoplasm
Out of the total 18 cases of malignant neoplasms, 17 swellings were finally diagnosed as malignant neoplasms by performing ultrasonography and surgical intervention investigations.
Out of 17 cases of malignant neoplasms, 7 cases were of moderately differentiated squamous cell carcinomas, 5 cases were of well-differentiated squamous cell carcinomas, 2 cases were of poorly differentiated squamous cell carcinomas, 1 case was of malignant melanoma, 1 case was of fibrosarcoma and 1 case was of pleomorphic adenoma undergoing carcinomatous changes. In 1 out of 18 patients, clinical diagnosis did not match with final diagnosis, whereas all the sonographic diagnoses matched with final diagnosis.
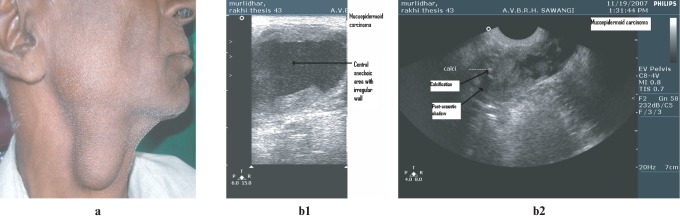
From this study, it can be concluded that most malignant neoplasms had ill-defined boundaries, irregular shapes and hypoechoic echo intensity. The ultrasound architecture of lesions of malignant neoplasms was heterogeneous, posterior echoes appeared unchanged and ultrasound characteristic of tissues of malignant neoplasms were solid in nature. If there was no enhancement or attenuation posterior to the lesion, posterior echoes were considered to be unchanged (Table 5, Figure 5).
Table 5. Ultrasonographic features of malignant neoplasms—total (18).
| Greyscale sonographic features | Malignant neoplasms | No. | Percentage |
| Boundary | Very clear | 1 | 5.5 |
| Relatively clear | |||
| Partially unclear | 6 | 33.3 | |
| Ill defined | 11 | 61.1 | |
| Shape | Oval | ||
| Lobular | 4 | 22.2 | |
| Polygonal | |||
| Irregular | 10 | 55.5 | |
| Round | 4 | 22.2 | |
| Echo intensity | Anechoic | ||
| Isoechoic | 4 | 22.2 | |
| Hypoechoic | 14 | 77.7 | |
| Iso + hypoechoic | 1 | 5.5 | |
| Hyperechoic | |||
| Ultrasound architecture of lesion | Homogeneous | 4 | 22.2 |
| Heterogeneous | 14 | 77.7 | |
| Posterior echoes | Enhanced | 6 | 33.3 |
| Unchanged | 7 | 38.8 | |
| Attenuated | 5 | 27.7 | |
| Ultrasound characteristic of tissues | Cystic | ||
| Solid | 14 | 77.7 | |
| Mixed | 4 | 22.2 |
Figure 5.
(a) Malignant neoplasm—high-grade mucoepidermoid carcinoma (clinical photograph). (b1) Malignant neoplasm—high-grade mucoepidermoid carcinoma (ultrasonographic image). (b2) Malignant neoplasm—high-grade mucoepidermoid carcinoma (ultrasonographic image)
For the intergroup comparison amongst the four groups of swellings, six groups for the comparisons were made, including benign neoplasms from malignant neoplasms; inflammatory swellings from malignant neoplasms; benign neoplasms from cystic swellings; inflammatory swellings from benign neoplasms; inflammatory swellings from cystic swellings; and cystic swellings from malignant neoplasms.
A comparison was made between benign and malignant neoplasms in head and neck swellings according to greyscale sonographic features. In these comparisons, the χ2 value and P-value were calculated. From these values, it can be concluded that in greyscale ultrasonography, criteria of boundary, echo intensity and ultrasound architecture of lesions are statistically significant to differentiate benign from malignant neoplasms in the head and neck as the P-value is <0.05.
A comparison was made between inflammatory swellings and malignant neoplasms in head and neck swellings according to greyscale sonographic features. In these comparisons, the χ2 value and P-value were calculated. From these values it can be concluded that in greyscale ultrasonography, the criteria of boundary and ultrasound architecture of lesion are statistically significant to differentiate inflammatory swellings from malignant neoplasms in the head and neck as the P-value is <0.05.
A comparison was made between cystic swellings and benign neoplasms in head and neck swellings according to greyscale sonographic features. In these comparisons, the χ2 value and P-value were calculated. From these values, it can be concluded that in greyscale ultrasonography, only the criteria of ultrasound characteristics of tissues is statistically significant to differentiate cystic swellings from benign neoplasms in the head and neck as the P-value is <0.05.
A comparison was made between inflammatory swellings and benign neoplasms in head and neck swellings according to greyscale sonographic features. In these comparisons, the χ2 value and P-value were calculated. From these values, it can be concluded that in greyscale ultrasonography, the criteria of boundary and echo intensity are statistically significant to differentiate inflammatory swellings from benign neoplasms in the head and neck as the P-value is <0.05.
A comparison was made between inflammatory swellings and cystic swellings in head and neck swellings according to greyscale sonographic features. In these comparisons, the χ2 value and P-value were calculated. From these values, it can be concluded that in greyscale ultrasonography, the criteria of boundary, shape, echo intensity, posterior echoes and ultrasound characteristics of tissues are statistically significant to differentiate inflammatory swellings from cystic swellings in the head and neck as the P-value is <0.05.
A comparison was made between cystic swellings and malignant neoplasms in the head and neck according to greyscale sonographic features. In these comparisons, the χ2 value and P-value were calculated. From these values it can be concluded that all the criteria of ultrasonography, such as boundary, shape, echo intensity, ultrasound architecture of lesion, posterior echoes and ultrasound characteristic of tissues, are statistically significant to differentiate cystic swellings from malignant neoplasms in the head and neck as the P-value is <0.05 and the criteria of boundary, echo intensity and ultrasound characteristics of tissues are also statistically highly significant.
After considering the results of all 70 cases of the present study (Tables 6–9), it can be concluded that clinical diagnosis had a sensitivity and accuracy of 85.7% whereas ultrasonographic diagnosis had a sensitivity and accuracy of 98.5%.
Table 6. Comparison of clinical and ultrasonographic diagnosis of inflammatory swellings.
| Sensitivity analysis | Clinical diagnosis (%) | Ultrasonographic diagnosis (%) |
| Sensitivity | 85.7 | 97.1 |
| Specificity | 85.7 | 100 |
| Positive predictive value | 85.7 | 100 |
| Negative predictive value | 85.7 | 97.2 |
| Likelihood ratio | 6.0 | – |
| Accuracy of the test | 85.7 | 98.5 |
Table 9. Comparison of clinical and ultrasonographic diagnosis of malignant neoplasms.
| Sensitivity analysis | Clinical diagnosis (%) | Ultrasonographic diagnosis (%) |
| Sensitivity | 94.4 | 100 |
| Specificity | 82.6 | 98.0 |
| Positive predictive value | 65.3 | 94.7 |
| Negative predictive value | 97.7 | 100 |
| Likelihood ratio | 5.4 | 52 |
| accuracy | 85.7 | 98.5 |
Discussion
The differential diagnosis of swelling in the head and neck is broad and extensive and includes both serious and benign aetiologies. Accurate diagnosis of a head and neck swelling is of paramount importance.
In this study, most of the inflammatory swellings had relatively clear boundaries, irregular shapes, hypoechoic echo intensity and homogeneous ultrasound architecture of lesion. The posterior echoes appeared enhanced and ultrasound characteristics of tissues were cystic or solid in nature. Our findings were consistent with findings given by Sivarajasingam et al7 and Baurmash et al8 who stated that in cases of abscesses, ultrasonography showed reduction of echo intensity and deep “underlying cystic change”. In this study, there were five cases of inflammatory swellings from non-odontogenic origin, such as sialadenitis, which included three cases of parotitis and two cases of submandibular sialadenitis. Three cases had coarsening of glandular parenchyma, hypoechoic areas and heterogeneous echo texture of the gland as seen in parotitis and submandibular sialadenitis. Our findings were consistent with findings given by Howlett9,11 and Alyas et al.10
In this study, in one case which was diagnosed clinically as submandibular lymphadenopathy but the ultrasound showed hyperechoic foci casting posterior acoustic shadowing and enlargement of the gland, duct dilation proximal to obstruction was seen. It was diagnosed as obstructive submandibular sialadenitis.12-14
In this study, in the group of inflammatory swellings, clinical diagnosis had a sensitivity and specificity of 85.7% whereas sonographic diagnosis had a sensitivity of 97.1% and specificity of 100% (Table 6).
Cysts on the sonogram appear as anechoic with a very clear boundary and homogeneous echo texture. If the cysts become infected then the content of the lesion can produce some echoes, producing hypoechoic structures.15,16
In this study, four cases of periapical cyst were studied. All four cases showed very clear boundaries, posterior echoes appeared enhanced and homogeneous internal echoes were suggestive of periapical cyst. In these four cases, sonography had been performed intraorally with a transcavitary probe.17
In this study, in the group of cystic swellings, clinical diagnosis had a sensitivity of 75% and a specificity of 87.1%, whereas sonographic diagnosis had a sensitivity of 100% and a specificity 98.3% (Table 7).
Table 7. Comparison of clinical and ultrasonographic diagnosis of cystic swellings.
| Sensitivity analysis | Clinical diagnosis (%) | Ultrasonographic diagnosis (%) |
| Sensitivity | 75 | 100 |
| Specificity | 87.1 | 98.3 |
| Positive predictive value | 42.8 | 88.8 |
| Negative predictive value | 96.4 | 100 |
| Likelihood ratio | 5.8 | 62 |
| Accuracy | 85.7 | 98.5 |
In this study, one pleomorphic adenoma had a very clear boundary, was rounded in shape and had hypoechoic echo intensity associated with heterogeneous internal architecture. Our findings were comparable with findings given by Howlett9,11 and Alyas et al.10
In the present study, there were four cases of haemangioma, of which two cases had hypoechoic echo intensity with heterogeneous internal architecture and a posterior echo that appeared enhanced. In one case there was an anechoic area and the heterogeneous internal architecture with posterior echo was enhanced, whereas in another case there were hyperechoic areas with homogeneous internal architecture and enhanced posterior echo. Two cases of cavernous haemangioma had compressible vascular spaces on colour Doppler examination. Our findings were consistent with findings given by Kalinowska et al,18 Turkington et al19 and Howlett et al.11
Lipoma appeared on ultrasound as a solid homogeneous mass of similar echogenicity to that of subcutaneous fat.19
In this study, clinical diagnosis of benign neoplasms had a sensitivity of 77.7% and specificity of 86.8%, whereas sonographic diagnosis had a sensitivity of 100% and a specificity 98.3%, and the accuracy of the test was 98.5% (Table 8). Our findings were consistent with findings given by Ahuja et al,20 Turkington et al19 and Howlett et al.11
Table 8. Comparison of clinical and ultrasonographic diagnosis of benign neoplasms.
| Sensitivity analysis | Clinical diagnosis (%) | Ultrasonographic diagnosis (%) |
| Sensitivity | 77.7 | 100 |
| Specificity | 86.8 | 98.3 |
| Positive predictive value | 46.6 | 90 |
| Negative predictive value | 96.3 | 100 |
| Likelihood ratio | 5.9 | 61 |
| Accuracy | 85.7 | 98.5 |
Ultrasound can predict malignancy in 89% of cases but various forms of malignancy cannot be differentiated. On ultrasounds of lower grade tumours, smaller lesions may appear as well defined and similar to a benign tumour. Larger lesions developed more overtly with malignant features, including irregular and poorly defined margins with heterogeneous internal architecture.9-11
In the present study, in the group of malignant neoplasms, clinical diagnosis had a sensitivity of 94.4% and specificity of 82.6%, whereas sonographic diagnosis had a sensitivity of 100.0% and specificity of 98.0% (Table 9).
Conclusion
The intergroup comparison amongst the four groups of swellings was made and from this it can be concluded that:
There are six criteria of ultrasonography of which three criteria (boundaries, echo intensity and ultrasound architecture of lesions) are statistically significant to differentiate benign neoplasms from malignant neoplasms in the head and neck as the P-value is <0.05.
To differentiate inflammatory swellings from malignant neoplasms in the head and neck, two criteria (boundaries and ultrasound architecture of lesion) are statistically significant as the P-value is <0.05.
Only one criterion of ultrasonography (ultrasound characteristics of tissues) is statistically significant to differentiate benign neoplasms from cystic swellings as the P-value is <0.05.
Two criteria of ultrasonography (boundaries and echo intensity) are statistically significant to differentiate inflammatory swellings from benign neoplasms in the head and neck as the P-value is <0.05.
Five criteria of ultrasonography (boundaries, shape, echo intensity, posterior echos and ultrasound characteristic of tissue) are statistically significant and differentiate inflammatory swellings from cystic swellings as the P-value is <0.05.
All six criteria of ultrasonography (boundaries, shape, echo intensity, ultrasound architecture of lesion, posterior echoes and ultrasound characteristic of tissue) are statistically significant and differentiate cystic swellings from malignant neoplasms as the P-value is <0.05.
The use of real-time ultrasonography with high-frequency transducers can significantly improve the evaluation of patients with various types of head and neck swellings. Therefore, ultrasonographic examinations, which have relatively high sensitivity and specificity, should be used to supplement clinical examination in patients with head and neck swellings to arrive at a final diagnosis.
From the present study and in accordance with Howlett et al,11 Silimy et al,15 Ishikawa et al,16 Turkington et al19 and Sajeeda et al,21 it can be summarised that after clinical examination, ultrasound should be the first modality used for the investigation as it is readily available and does not involve ionizing radiation, after which CT and MRI can be used to determine the extent of the mass and to better define tissue characteristics.
One of the goals of this study was to differentiate between various types of head and neck swellings using an ultrasonographic investigative procedure, and this study appreciates the important role of ultrasonography in diagnostic approach. Therefore, it should be routinely performed as a part of evaluation of all patients with head and neck swellings.
References
- 1.Rammohan C. Ultrasound technology. In: Rammohan C. Ultrasound unlimited. The A to Z ultrasound (1st edn) Hyderabad, India: Paras Medical Publisher, 2005, pp 2–8 [Google Scholar]
- 2.Palmer PES. Basics of ultrasound. In: Palmer PES. Manual of diagnostic (New millennium edition) AITBS. Publishers and Distributors (Regd), Delhi, 2004, pp 3–5 [Google Scholar]
- 3.Correa PD, Arya S, Laskar SG, Shrivastava SK, Dinshaw KA, Gupta T, et al. Ultrasonographic changes in malignant neck nodes during radiotherapy in head & neck squamous carcinoma. Australas Radiol 2005;49:113–118 [DOI] [PubMed] [Google Scholar]
- 4.Chodosh L, Silbey R, Oen KT. Diagnostic use of ultrasound in diseases of head & neck. Laryngoscope 1980;90:814–820 [PubMed] [Google Scholar]
- 5.Das S. Examination of lump or swelling. Das S.In: A manual on clinical surgery (3rd edn) Dr S Das: Calcutta, India, 1988, pp 8–16 [Google Scholar]
- 6.Shimizu M, Ussmuller J, Hartwein J, Donath K. A comparative study of sonographic and histopathologic findings of tumours lesions in the parotid gland. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:723–737. [DOI] [PubMed] [Google Scholar]
- 7.Sivarajasingam V, Sharma V, Crean SJ, Shepherd JP. Ultrasound-guided needle aspiration of lateral masticator space abscess. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:616–619 [DOI] [PubMed] [Google Scholar]
- 8.Baurmash HD. Ultrasonography in the diagnosis and treatment of facial abscesses. J Oral Maxillofac Surg 1999;57:635–636 [DOI] [PubMed] [Google Scholar]
- 9.Howlett DC. Pictorial review—High resolution ultrasound assessment of parotid grand. Br J Radiol 2003;76:271–277 [DOI] [PubMed] [Google Scholar]
- 10.Alyas F, Lewis K, Williams M, Moody AB, Wong KT, Ahuja AT, et al. Diseases of submandibular gland as demonstrated using high resolution ultrasound. Br J Radiol 2005;78:362–369 [DOI] [PubMed] [Google Scholar]
- 11.Howlett DC, Alyas F, Wong KT, Lewis K, Williams M, Moody AB, et al. Sonographic assessment of submandibular space. Clin Radiol 2004;59:1070–1078 [DOI] [PubMed] [Google Scholar]
- 12.Traxler M, Schurawitzki H, Ulm C, Solar P, Blahout R, Piehslinger E, et al. Sonography of non-neoplastic disorders of salivary glands. Int J Oral Maxillofac Surg 1992;21:360–363 [DOI] [PubMed] [Google Scholar]
- 13.Schmelzeisen R, Milbradt H, Reimer P, Gratz P, Wittekind C. Sonography and scintigraphy in the diagnosis of disease of major salivary glands. J Oral Maxillofac Surg 1991;49:798–803 [DOI] [PubMed] [Google Scholar]
- 14.Yoshimura Y, Inoue Y, Odagawa T. Sonographic examination of sialolithiasis. J Oral Maxillofac Surg 1989;47:907–912 [DOI] [PubMed] [Google Scholar]
- 15.El-Silimy O, Corney C. Radiology in focus: The value of sonography in management of cystic neck lesions. J Laryangol Otol 1993;107:245–251 [DOI] [PubMed] [Google Scholar]
- 16.Ishikawa H, Ishii Y, Ono T, Makimot K, Yamamoto K, Torizuka K. Evaluation of gray–scale ultrasonography in the investigation of oral & neck mass lesions. J Oral Maxillofac Surg 1983;41:775–781 [DOI] [PubMed] [Google Scholar]
- 17.Cotti E, Campisi G, Ambu R, Dettori C. Ultrasound real-time imaging in the differential diagnosis of periapical lesions. Int Endod J 2003;36:556–563 [DOI] [PubMed] [Google Scholar]
- 18.Rozylo-Kalinowska I, Brodzisz A, Galkowska E, Rozylo TK, Wieczorek AP. Application of doppler ultrasonography in congenital vascular lesions of head and neck. Dentomaxillofac Radiol 2002;31:2–6 [DOI] [PubMed] [Google Scholar]
- 19.Turkington JR, Paterson A, Sweeney LE, Thornbury GD. Pictorial review—neck masses in children. Br J Radiol 2005;78:75–85 [DOI] [PubMed] [Google Scholar]
- 20.Ahuja AT, King AD, Kew J, King W, Metreweli C. Head and neck lipomas: sonographic appearance. AJNR Am J Neuroradiol 1998;19:505–508 [PMC free article] [PubMed] [Google Scholar]
- 21.Sajeeda S, Panda N, Mann SB, Kataria S, Kalagara S. The role of ultrasonography in the management of tumors of the neck. Ear Nose Throat J 2000;79:586–589 [PubMed] [Google Scholar]