Abstract
Rhabdomyolysis is rare in the head and neck. Early diagnosis and treatment is essential to prevent serious complications such as hyperkalaemia, acidosis, acute renal failure and disseminated intravascular coagulation. We present a case of rhabdomyolysis of the head and neck. CT and MRI findings supported the diagnosis of rhabdomyolysis with the patient's clinical and laboratory findings. While imaging is not crucial, it can aid in the detection of rhabdomyolysis and narrow the differential diagnosis along with laboratory findings and physical examination.
Keywords: rhabdomyolysis, head and neck, computed tomography, magnetic resonance imaging
Introduction
Rhabdomyolysis is the breakdown of muscle fibres with the release of various toxic muscle cell contents into the systemic circulation.1 It can result in renal failure, acidosis, hyperkalaemia and disseminated intravascular coagulation (DIC). Early diagnosis and treatment is essential for a better outcome. Rhabdomyolysis is rare in the head and neck. There has been description of rhabdomyolysis in the head and neck owing to drug toxicity described in the literature.2-4 We describe a case of rhabdomyolysis of the head and neck, including clinical presentation, and CT and MRI characteristics.
Case report
The patient was a 23-year-old man who was just released from a drug rehabilitation programme and went on an alcohol and cocaine binge the same day. The patient's roommate found him unconscious, lying on his right side approximately 7–12 h later. He was subsequently taken to the emergency room where a physical examination revealed marked swelling of his right face and right thigh. By this time, the patient had regained consciousness and was complaining of severe pain involving his right face and thigh. His laboratory work was remarkable owing to a potassium level of 7.6 mEq l–1 (normal range: 3.5–4.5 mEq l–1), creatine phosphokinase (CPK) level of 65505 IU l–1(normal range: 39–259 IU l–1) and creatinine level of 1.7 mg dl–1 (normal range: 0.5–1.5 mg dl–1). He also tested positive for opiates and cocaine.
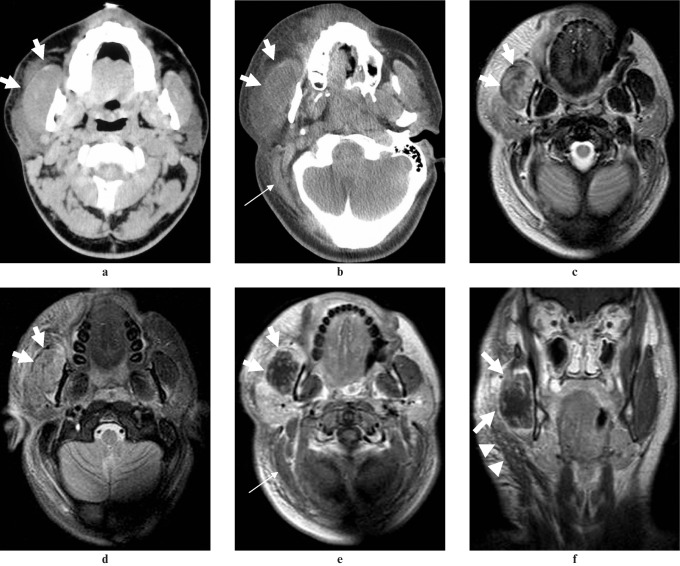
Emergency medicine physicians thought he had sustained trauma to the face and he was sent for CT of the neck. No intravenous contrast was given owing to acute renal failure. CT demonstrated swelling of the right masseter muscle and parotid gland with associated soft-tissue oedema and fat stranding in the subcutaneous tissue (Figure 1a). The follow-up CT the next day showed progression of swelling in these areas as well as swelling of the right platysma and sternocleidomastoid muscle (Figure 1b). Subsequently, MRI was performed to rule out abscesses. On MRI, those muscles showed homogeneous isointensity to slight hypointensity on T1-weighted images, heterogeneous hyperintensity on T2-weighted images and short tau inversion recovery (STIR) (Figures 1c,d) images compared with the contralateral muscles. The parotid gland and the subcutaneous fat also showed swelling and hyperintensity on T2-weighted and STIR images consistent with oedema. Post-contrast images demonstrated heterogeneous dot-like or linear enhancement in the right masseter muscle (Figures 1e,f). No abnormality was noted in the pterygoid muscles or mandible to suggest masticator space infection.
Figure 1.
23-year-old man found unconscious who presented with right-sided facial swelling and pain. (a) Axial non-contrast enhanced CT shows swelling of the right masseter muscle (arrows) and parotid gland with fat stranding in the subcutaneous tissue. (b) Follow-up CT shows progression of swelling of the right masseter muscle (arrows) and subcutaneous fatty tissue, as well as swelling of the sternocleidomastoid muscle (thin arrow). Axial T2-weighted (c) and short tau invession recovery (d) images show swelling and heterogeneously increased signal of the masseter muscle (arrows) with associated inflammatory change in the parotid gland and subcutaneous fat. Post-contrast axial (e) and coronal (f) T1-weighted image show the dot-like or linear enhancement in the swollen masseter muscle (arrows). Swelling and heterogeneous enhancement is also noted in the sternocleidomastoid muscle (thin arrow) and platysma (arrow heads)
Discussion
Rhabdomyolysis is described as the breakdown of muscle fibres with the release of various toxic muscle cell contents into the systemic circulation.
This process eventually leads to necrosis of the muscle tissue, which can lead to associated complications such as hyperkalaemia, metabolic acidosis, acute tubular necrosis, hypovolaemia, compartment syndrome and DIC.5 Common findings during the clinical workup include myalgias, weakness and fatigue with occasional swelling of the affected muscles.5 In addition, the patient reports having dark or red-coloured urine.3
Trauma is thought to be the most common cause of rhabdomyolysis owing to direct injury to muscle with associated disruption of the sarcolemma and release of cell content.6 Various types of orthopaedic trauma can cause rhabdomyolysis, including compartment syndrome, which is not only a complication but also a cause for rhabdomyolysis. Infectious aetiologies include Legionella and Group A beta haemolytic streptococcus bacteria. The most common viral causes include influenza A and B.6 In some studies, alcohol and drug abuse was thought to be the most common cause.1 This was thought to be caused by disruption of the blood supply owing to prolonged muscle compression caused by immobilization and direct toxic effects of the offending substances. Other causes include metabolic and genetic factors, thermal injury and excessive exertional activity.5 Although there are various causes for rhabdomyolysis, the common link seems to be disruption of the sarcolemma and the myocyte calcium homeostasis. There is associated release of enzymes, such as lactate dehydrogenase, CPK and aspartic aminotransferase, myoglobin and electrolytes, such as potassium and phosphates.6 The most reliable method to diagnose rhabdomyolysis, based on clinical suspicion, is by measuring the CPK. This can be more than 5 times normal values, peaks at approximately 36 h and subsequently declines with proper treatment. Other laboratory data include the complete blood count, electrolyte panel and coagulation profile. Treatment includes aggressive hydration to control hypovolaemia, monitoring of urine output and renal function, and control of acidosis and hyperkalaemia. Haemodialysis may be required if the patient develops renal failure and fasciotomies may be needed if the patient has compartment syndrome.7 While mannitol and bicarbonate have been used to treat rhabdomyolysis, some studies have suggested that there is no benefit by adding these agents in addition to aggressive hydration. Free radical scavengers (e.g. vitamin E, vitamin C, zinc, manganese etc) have been found to reduce the amount of nephrotoxic materials released from the muscles in experimental models and may have a role in the treatment of rhabdomyolysis.8
To our knowledge, three cases of rhabdomyolysis in the head and neck have been reported.2-4 Riggs et al reported swelling and a low density area in the left neck muscles on CT and hyperintensity of the muscles and adjacent soft tissues on MRI in a 22-year-old man with heroin and chronic ethanol use.2 Shah et al reported sonographic findings of rhabdomyolysis of the masseter muscle in a 33-year-old man with ingestion of an unknown quantity of alcohol and drugs.3 More recently, Jain et al reported low density of the lateral pterygoid muscles on CT with subsequent hyperintensity and contrast enhancement on MRI done several days later in a 28-year-old with psychiatric problems who was admitted to the hospital for an acetaminophen overdose.4 CT and MRI findings of rhabdomyolysis in the extremities have also been reported,9,10 and two types of rhabdomyolysis have been described.9 Type I rhabdomyolysis presents with oedema and the affected muscles reveal homogeneous isointensity to hypointensity on T1-weighted images, homogeneous hyperintensity on T2-weighted and STIR images and homogeneous enhancement. Type II rhabdomyolysis presents with myonecrosis and the affected muscles reveal heterogeneous hypodensity on the CT image, homogeneous or heterogeneous hypointensity on T1-weighted images, heterogeneous hyperintensity on T2-weighted and STIR images and rim and dot-like or linear streaky enhancement, which is called the “stipple sign”.9 In our case, the affected muscles demonstrated an MR signal pattern and enhancement similar to Type II rhabdomyolysis.
Imaging typically plays a minor role in the diagnosis of rhabdomyolysis. It is typically performed to search for orthopaedic injuries such as fractures. In our case, the initial CT was performed to evaluate for underlying traumatic injury and follow-up CT and MRI were performed to rule out possible infection because of progression of pain and soft-tissue swelling, which was confirmed on follow-up imaging since no abnormality was noted in the pterygoid muscles or mandible to suggest masticator space infection. The imaging findings supported the diagnosis of rhabdomyolysis, even though it is not common in the head and neck, and unnecessary interventions such as biopsy or drainage could be avoided. Our patient subsequently developed compartment syndrome in his thigh and required multiple fasciotomies. His facial swelling and pain had improved over the course of his hospital stay. The ultimate cause of the patient's rhabdomyolysis of the face and thigh was thought to be his intoxicated state from a combination of alcohol and drugs which led to a loss of consciousness and immobilization in the right lateral decubitus position for several hours.1,7
In conclusion, we reported CT and MRI findings of rhabdomyolysis in the head and neck. Rhabdomyolysis is rare in the head and neck; however, recognizing the imaging findings is important to avoid serious complications and unnecessary interventions. While imaging is not crucial, it can aid in establishing the diagnosis of this rare condition in the head and neck and narrow the differential diagnosis along with laboratory findings and physical exam.
References
- 1.Melli G, Chaudhry V, Cornblath D. Rhabdomyolysis: an evaluation of 475 hospitalized patients. Medicine 2005;84:377–385 [DOI] [PubMed] [Google Scholar]
- 2.Riggs JE, Schochet SS, Jr, Hogg JP. Focal rhabdomyolysis and brachial plexopathy: an association with heroin and chronic ethanol use. Mil Med 1999;164:228–229 [PubMed] [Google Scholar]
- 3.Shah HV, Irvine GH, Bradley M. Rhabdomyolysis of the masseter muscle: Case report. Br J Oral Maxillofac Surg 2008;46:138–140 [DOI] [PubMed] [Google Scholar]
- 4.Jain V, Ellingson AN, Smoker WRK. Lateral pterygoid muscle rhabdomyolysis. AJNR Am J Neuroradiol 2007;28:1876–1877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Allison RC, Bedsole DL. The other medical causes of rhabdomyolysis. Am J Med Sci 2003;326:79–88 [DOI] [PubMed] [Google Scholar]
- 6.Warren JD, Blumberg PC, Thompson PD. Rhabdomyolysis: A review. Muscle Nerve 25: 332–347 [DOI] [PubMed] [Google Scholar]
- 7.Alterman I, Sidi A, Azamfirei L, Copotoiu S, Ezri T. Rhabdomyolysis: another complication after prolonged surgery. J Clin Anesth 2007;19:64–66 [DOI] [PubMed] [Google Scholar]
- 8.Huerta-Alardin AL, Varon J, Marik PE. Bench-to-bedside review: Rhabdomyolysis—an overview for clinicians. Crit Care 2005;9:158–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lu CH, Tsang YM, Yu CW, Wu MZ, Hsu CY, Shih TT. Rhabdomyolysis: magnetic resonance imaging and computed tomography findings. J Comput Assist Tomogr 2007;31:368–374 [DOI] [PubMed] [Google Scholar]
- 10.Lamminen AE, Hekali PE, Tiula E, Suramo I, Korhola OA. Acute rhabdomyolysis: evaluation with magnetic resonance imaging compared with computed tomography and ultrasonography. Br J Radiol 1989;62:326–331 [DOI] [PubMed] [Google Scholar]