Abstract
The aim of this report is two-fold. First it analyses the precision of a modification of the parallel technique that can be used in those cases with anatomical limitations. Second, it checks the influence of the reference points’ definition of objects to be measured by using both the original and the modified radiographic techniques. 2 intraoral radiographs were taken of 28 implants with 2 different methods: a standard paralleling technique and a modified technique that used a smaller film and a silicone spacer to ensure parallelism. Measurements of peri-implant bone levels and implant width were made in triplicate on digitized film radiographs. The results of the peri-implant bone levels were that with the parallel method the mean was 0.44 mm and the precision was 0.43 mm, and with the modified method the mean was 0.73 mm and the precision was 0.66 mm. In addition to the correct localization of the point of reference in this study, the precision with the parallel method was 0.08 mm and with the modified method was 0.13 mm. Although it was greater with the gold standard technique than with the modified technique, precision was very high for both methods and accurate enough for clinical use.
Keywords: dental implants, bone resorption, radiographic image interpretation, diagnostic imaging
Introduction
One of the criteria of success in the osseointegration of dental implants is the maintenance of a stable height of the marginal bone under functional loads.1 Two aspects are very important for evaluating bone height: first, the assessment of bone level changes over time requires radiographic methods with a high degree of precision, and second, the correct definition and localization on the images of the structures which were intended to be assessed.
Intraoral radiography using the parallel technique is the recommended method for visualizing minute bone changes, despite the continual improvements of extra-oral radiographic systems.2 By using this technique, high accuracy in measurements can be obtained.3 The parallel technique is defined as the parallelism between the object to be studied and the plane of the film while the central axis of the X-ray is perpendicularly adjusted to both planes. Unfortunately, it is much easier to get a perpendicular position of the X-ray central axis to the film than to the object. When the object is a dental implant, it is even more difficult because the body of the implant is situated within the alveolar bone so it cannot be seen.4 Owing to the above mentioned problems, many studies have been based on the evolution of the radiographic method made with the perpendicular technique (right-angle technique), described in the 1950s and 1960s by Benkow5 for the study of the bone crest on teeth and later improved by Larheim and Eggen.6 This shows for the first time in dental implantology history that standardized radiographs can be improved if an individualized bite record is used in combination with the bite block and the long cone technique.5,6 The use of a correctly applied X-ray positioner provides a perpendicular alignment of the X-ray cone through the film and consequently a fixed position of the focal spot. Many factors can produce inaccuracy in determining the levels of proximal bone to oral implants. The unsolved key point is the image distortion, generally magnification, owing to the oblique position of the object and this often happens in the maxilla because of the strong inclination of the palate and/or a low palate. When taking radiographs of an extremely resorbed mandible, it is often impossible to place the film intraorally because of the interference of the floor of the mouth.7,8
Another important factor to be considered is the correct definition and localization on the radiographic film of the structures which are intended to be assessed. When considering the radiographic evaluation of the marginal bone height, the distance between two reference radiographic points is measured. The most common are the neck of the implant as this is an easy point to recognize owing to its shape, its metallic structure that stands out clearly on the plate and the fact that it is the most apical contact point of the bone with the implant. One may have trouble finding this point because of scarce bone definition or superimposition of bone images corresponding to the crest on the buccal side that may coincide with crest height in the lingual or palatal side. Some authors have pointed out this important methodological limitation by stating that the main source of errors may be the correct recognition of the reference points in the interface between the alveolar bone and the implant or tooth.9
The aim of this work is two-fold: to analyse the precision of a modification of the long cone parallel technique that can be used in those cases with important anatomical limitations and to check the influence of the reference points' definition of objects to be measured by using the standard and the modified techniques.
Materials and methods
A total of 25 patients were chosen from October 2008 to July 2009 at the Dental Prosthesis Unit of the Faculty of Medicine and Dentistry of the University of Santiago de Compostela, Spain, for rehabilitation by means of implant-retained fixed prosthesis. The sample comprised a total of 18 women and 7 men with an average age of 47.8 years (range 24–74 years). The patients included in this study did not show relevant pathology and smokers were not included.
The design of this study received full approval from the Ethical Research Committee of the Faculty of Medicine and Odontology, University of Santiago de Compostela, Spain. The patients were informed of the aims and methods of the study and all gave their consent to participate.
A total of 28 Straumann implants (Institut Straumann AG, Waldenburg/BL, Switzerland) of bone level type were used measuring 4.1 mm in diameter with lengths of between 10 mm and 12 mm. Surgery and prosthetic procedures were performed according to the manufacturer's instructions and established protocols were published beforehand. Once the osseointegration period was over, implant loading began by means of using cemented prosthesis. As soon as the last cementing of the prosthesis was performed, a radiographic examination was taken for peri-implant bone level evaluation.
The radiographic examination was carried out with periapical radiographs (Kodak Ultraspeed Dental Film, Eastman Kodak, Rochester, NY) with a Siemens Heliodent MD model X1744 (Sirona Dental Systems, GmbH D-64625, Bensheim, Germany) X-ray machine set at 70 kV and 7 mA. Two methods were used to obtain the radiographs:
method 1 (paralleling standard technique): the radiograph was taken using the long cone parallel technique by employing a positioner (X-ray Holders, KerrHawe SA, CH-6934 Bioggio, Switzerland), which was placed on the 30.5 × 40.5 mm size film (Kodak Ultraspeed size II Dental Film, Eastman Kodak), parallel to the long axis of the implant and perpendicular to the X-ray central cone. A silicone bite register (Aquasil Soft Putty/Regular Set, Dentsply DeTrey GmgH 78467 Konstanz, Germany) was placed on the positioner where the patient left a print of the oclussal sides of their teeth, allowing the reposition of the control X-ray in subsequent years (Figure 1)
method 2 (modified technique): a 22 × 35 mm size pediatric X-ray (Kodak Ultraspeed size 0 Dental Film, Eastman Kodak) was used. Using silicone, the radiographic film was placed parallel to the longitudinal axis of the implant so that the implant neck was positioned in the centre of the film. The radiograph was taken by placing the X-ray cone perpendicular to the X-ray plane (Figure 2).
Figure 1.

Clinical photograph of radiographic method 1
Figure 2.

Clinical photograph of radiographic method 2
2 radiographs were obtained using methods 1 and 2 for each of the 28 implants. Then the intraoral radiographs were scanned (Hewlett-Packard ScanJet 4 C/T, Boise, ID) into a Pentium computer and digitalized. The radiographs were stored in bitmap format using 256 grey levels. The measurements were performed by means of NIH Image (Wayne Rasband, US National Institutes of Health). It was used to digitally process and manipulate the radiographic images and perform the measurements.
Measurements performed with both methods correspond to:
distance between the first point of bone-implant contact and the implant shoulder either in the mesial or distal to analyse the precision of the modified technique
measurement of the implant shoulder width to check the influence of the reference points definition.
All measurements were repeated three times. When two or more of the measurements were identical, the matching measurements were considered correct. If all three measurements varied, they were averaged to provide the accepted measurements. All measurements were rounded to the nearest 0.1 mm for presentation in this article.
Data analysis
The differences between the data of the two measurement techniques were evaluated using tests for paired data. The tests comprise the parametric Student’s t-test and the non-parametric Wilcoxon test depending on the data distributions while the contrast of normality was made with the Shapiro–Wilks test.
Firstly, a linear regression model was used to assess the principal effects. Secondly, the effect of differences in the levels of the factors on the model was analysed by analysis of variance (ANOVA). Logarithmic transformations were applied to the data for normality and homoscedasticity.
Differences were considered statistically significant for P-values < 0.05. Statistical treatment of the data was performed using software R (www.r-project.org, version 2.11.1).
The data obtained with the two methods were analysed by calculating the median difference, the range, the percentage number of differences within ±0.25 mm, ±0.50 mm and ±1.0 mm and the precision (standard deviation, SD):
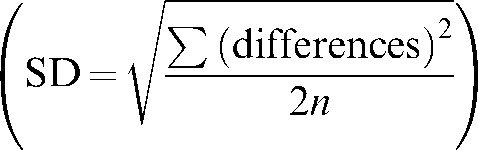 |
Results
For peri-implant bone levels related to the implant shoulder using method 1, the mean was 0.44 mm, ranging from 0.00 mm to 1.43 mm, and the precision was 0.43 mm. Using method 2, the mean was 0.73 mm, ranging from 0.00 mm to 2.92 mm, and the precision was 0.66 mm. The median difference between both methods was −0.25 mm; 41.1% were within ±0.25 mm, 69.7% were within ±0.50 mm and 92.9% were within ±1.0 mm. The bone levels using method 1 were statistically significantly different compared with method 2 (Wilcoxon matched pair sign rank test P ≤ 0.001; Table 1).
Table 1. Results of measurements of the mesial and distal peri-implant bone level related to the implant shoulder.
| Method 1 | Method 2 | |
| Mean ± SD | 0.477 ± 0.434 | 0.736 ± 0.663 |
| Median ± IR | 0.406 ± 0.846 | 0.580 ± 0.851 |
| Minimum | 0.000 | 0.000 |
| Maximum | 1.436 | 2.924 |
| Mean difference ± SD | −0.259 ± 0.388 | |
| Median difference ± IR | −0.183 ± 0.507* | |
| Minimum difference | −1.960 | |
| Maximun difference | 0.612 | |
| Differences within ±0.25 mm | 0.411 (41.1%) | |
| Differences within ±0.50 mm | 0.697 (69.7%) | |
| Differences within ±0.75 mm | 0.875 (87.5%) | |
| Differences within ±1 mm | 0.929 (92.9%) | |
*P ≤ 0.001; SD, standard deviation; IR, interquartile range
The variations of implant width measurement with both methods were:
Method 1 — the mean was 4.060 mm, the mean difference was –0.04 mm with a range of –0.30 mm to 0.13 mm. The precision was 0.08 mm. 92.9% of values were within a difference of ±0.25 mm and 100% were within ±0.5 mm.
Method 2 — the mean was 4.184 mm, the differences mean was 0.08 mm with a range of –0.25 mm to 0.63 mm and the precision was 0.13 mm. 92.9% of the values were within a difference of ±0.25 mm and 96.4% were within ±0.5 mm. The implant widths using method 1 were statistically significantly different compared with method 2 (Student’s t-test P = 0.002; Table 2).
Table 2. Measuring of implant width with methods 1 and 2.
| Method 1 | Method 2 | |
| Mean | 4.060 | 4.184 |
| Median ±IR | −0.006 ± 0.140 | 0.031 ± 0.254 |
| Minimum | −0.308 | −0.259 |
| Maximum | 0.136 | 0.633 |
| Mean difference ±SD | −0.124 ± 0.161* | |
| Median difference ± IR | −0.077 ± 0.266 | |
| Minimum difference | −0.600 | |
| Maximun difference | 0.194 | |
| Differences within ±0.25 mm | 0.929 (92.9%) | 0.929 (92.9%) |
| Differences within ±0.50 mm | 1 (100%) | 0.964 (96.4%) |
| Differences within ±0.75 mm | 1 (100%) | 1 (100%) |
| Differences within ±1 mm | 1 (100%) | 1 (100%) |
*P = 0.002; SD, standard deviation; IR, interquartile range
Discussion
Periapical radiography allows examination of crestal bone levels precisely at the mesial and distal sites of an implant only if proper projection geometry is applied.10-12 Such precision cannot be achieved if a bisecting-angle geometry technique is used. With the advent of the right-angle technique,5 the paralleling technique13 and customized occlusal records combined with a long-cone technique,9 projection errors related to rotation and angulation can be significantly decreased. When taking periapical radiographs, an attempt should be made to perfectly align the radiographic film with the long axis of the implant to evaluate crestal bone loss patterns (right-angle technique combined with paralleling technique and a customized bite record).7 Some authors have studied the signs of angulation in radiographs of implants and they have concluded that the limit at which one could misinterpret a radiograph is between 5° and 10° of angulation. It was shown that, depending on the width of the alveolar ridge and buccolingual position of a fixture, the distortion between bone margins can vary between 0.1 mm and 0.25 mm at 1° angulation and 4.8 mm at 20° angulation.10,12 The 90° periapical radiograph provided the most consistently accurate measurements with the least variation of all the techniques evaluated. Therefore, to make a correct diagnosis, it is important that radiographs with signs of angulation be rejected. These findings stress the need for using accurate methods of standardization for longitudinal control of peri-implant bone height changes. Furthermore, several authors have reported that the results of periapical radiography, with respect to the degree of crestal bone loss, underestimate the results of histometric analyses.14 One reason for this phenomenon might be that even though a right-angle technique was used, a parallel orientation of the bite block (film plane) to the long axis of the tooth/implant could not always be achieved.
Several criteria for implant success have been established by different authors. For Brägger et al,15 a mean crestal bone loss ranging from 0.9 mm to 1.6 mm during the first post-surgical year was accepted as a criterion for implant success. A mean annual crestal bone loss ranging from 0.05 mm to 0.13 mm in the maintenance period was listed as another criterion for a successful implant system. However, for a single comparison of bone height change, no method has been able to detect a difference in the range of 0.1 mm, which was described as an acceptable mean loss per year during maintenance for an implant system. When evaluating peri-implant changes, other authors have pointed out that radiographic evaluation of peri-implant bone level cannot be more than a precision of 0.5 mm when parallelism is not guaranteed and the distance focus-object is under 380 mm.4 For Moberg et al,16 the radiographic precision in measuring the distance between the crown and alveolar bone was approximately 0.2 mm, implying a random error of up to 0.4 mm for a registration with a 95% probability. In our results, the precision with method 1 was 0.08 mm and with method 2 it was 0.13 mm. Thus, the precision was higher with standard technique but with the modified technique the precision was within the reference values described in the literature.
Apart from the problems of radiographic distortion for non-parallelism, there is another important factor to be considered which is capable of giving rise to important methodological errors. This is the correct definition and localization of the structures to be evaluated on the film.9,17 The main source of error seemed to be the recognition of reference points on the interface between the alveolar bone and teeth/implant.18 In order to avoid or minimize these errors, several standardized procedures have appeared in the literature. Accessories aimed at standardizing series of radiographs are available. Levels of mesial and distal marginal changes to implants could be registered by taking the threads of fixtures as an internal reference. The accuracy in vitro of this method has been reported to be within a range of 0.3 mm.19 Another work that tested the reproducibility of peri-implant bone height measurement related to the reference points on the fixtures resulted in a measurement difference average of 0.26 ± 0.5 mm.20 In our work the average difference when implant width was measured was −0.04 mm with the standard method and 0.08 mm with the proposed modification, indicating that we have eliminated the distortion produced by an incorrect definition of the reference points. Although it was greater with the gold standard technique than with the modified technique, precision was very high for both methods and accurate enough for clinical use.
In conclusion, the modifications proposed in this work can be useful when it is difficult to use the paralleling technique. The lack of positioner use and the size 0 dental film can allow the use of a technique precise enough for the assessment of peri-implant bone level changes. The uncertainty in the assessment of alveolar bone level in the present study was mainly dependent on difficulties in the recognition of reference points in the alveolar bone.
References
- 1.Adell R. Long-term treatment results. In: Bränemark P-I, Zarb GA, Albrektsson T. (eds). Tissue-integrated prostheses: osseointegration in clinical dentistry. Chicago, London, Sao Paulo and Tokyo: Quintessence Publishing Co. Inc, 1985, pp 175–186 [Google Scholar]
- 2.De Smet E, Jacobs R, Gijbels F, Naert I. The accuracy and reliability of radiographic methods for the assessment of marginal bone level around oral implants. Dentomaxillofac Radiol 2002;31:176–181 [DOI] [PubMed] [Google Scholar]
- 3.Quirynen M, van Steenberghe D, Jacobs R, Schotte A, Darius P. The reliability of pocket probing around screw-type implants. Clin Oral Implants Res 1991;2:186–192 [DOI] [PubMed] [Google Scholar]
- 4.Schulze RK, d'Hoedt B. Mathematical analysis of projection errors in "paralleling technique" with respect to implant geometry. Clin Oral Implants Res 2001;12:362–371 [DOI] [PubMed] [Google Scholar]
- 5.Benkow HH. Periodisk-identiske og stereoskopiske intraorale røntgenopptak. Dent Norske Tannlaegetidende 1956;66:239–255 [Google Scholar]
- 6.Larheim TA, Eggen S. Measurements of alveolar bone height at tooth and implant abutments on intraoral radiographs. A comparison of reproducibility of Eggen technique utilized with and without a bite impression. J Clin Periodontol 1982;9:184–192 [DOI] [PubMed] [Google Scholar]
- 7.Hermann JS, Schoolfield JD, Nummikoski PV, Buser D, Schenk RK, Cochran DL. Crestal bone changes around titanium implants: a methodologic study comparing linear radiographic with histometric measurements. Int J Oral Maxillofac Implants 2001;16:475–485 [PubMed] [Google Scholar]
- 8.Lofthag-Hansen S, Lindh C, Petersson A. Radiographic assessment of the marginal bone level after implant treatment: a comparison of periapical and Scanora detailed narrow beam radiography. Dentomaxillofac Radiol 2003;32:97–103 [DOI] [PubMed] [Google Scholar]
- 9.Larheim TA, Wie H, Tveito L, Eggen S. Method for radiographic assessment of alveolar bone level at endosseous implants and abutment teeth. Scand J Dent Res 1979;87:146–154 [DOI] [PubMed] [Google Scholar]
- 10.Sewerin IP. Errors in radiographic assessment of marginal bone height around osseointegrated implants. Scand J Dent Res 1990;98:428–433 [DOI] [PubMed] [Google Scholar]
- 11.Gher ME, Richardson AC. The accuracy of dental radiographic techniques used for evaluation of implant fixture placement. Int J Periodontics Restorative Dent 1995;15:268–283 [PubMed] [Google Scholar]
- 12.Begoña Ormaechea M, Millstein P, Hirayama H. Tube angulation effect on radiographic analysis of the implant-abutment interface. Int J Oral Maxillofac Implants 1999;14:77–85 [PubMed] [Google Scholar]
- 13.Rosling B, Hollender L, Nyman S, Olsson G. A radiographic method for assessing changes in alveolar bone height following peiodontal therapy. J Clin Periodontol 1975;2:211–217 [DOI] [PubMed] [Google Scholar]
- 14.Gotfredsen K, Rostrup E, Hjörting-Hansen E, Stoltze K, Budtz-Jörgensen E. Histological and histomorphometrical evaluation of tissue reactions adjacent to endosteal implants in monkeys. Clin Oral Implants Res 1991;2:30–37 [DOI] [PubMed] [Google Scholar]
- 15.Brägger U. Radiographic parameters for the evaluation of peri-implant tissues. Periodontology 2000 1994;4:87–97 [DOI] [PubMed] [Google Scholar]
- 16.Moberg LE, Köndell PA, Kullman L, Heimdahl A, Gynther GW. Evaluation of single-tooth restorations on ITI dental implants. Clin Oral Impl Res 1999;10:45–53 [DOI] [PubMed] [Google Scholar]
- 17.Hausmann E, Allen K, Dunford R, Christersson L. A reliable computerized method to determine the level of the radiographic alveolar crest. J Periodontal Res 1989;24:368–369 [DOI] [PubMed] [Google Scholar]
- 18.Brägger U, Häfeli U, Huber B, Hämmerle CHF, Lang NP. Evaluation of postsurgical crestal bone levels adjacent to non-submerged dental implants. Clin Oral Implant Res 1998;9:218–224 [DOI] [PubMed] [Google Scholar]
- 19.Hollender L, Rockler B. Radiographic evaluation of osseointegrated implants of the jaws. Experimental study of the influence of radiographic techniques on the measurement of the relation between the implant and bone. Dentomaxillofac Radiol 1980;9:91–95 [DOI] [PubMed] [Google Scholar]
- 20.Adell R, Lekholm U, Gröndahl K, Bränemark PI, Lindström J, Jacobsson M. Reconstruction of severely resorbed edentulos maxillae using osseointegrated fixtures in immediate autogenous bone grafts. Int J Oral Maxillofac Implant 1990;5:233–246 [PubMed] [Google Scholar]


