Abstract
Objective
In general, no consensus has been reached regarding the diagnostic criteria for obstructive sleep apnoea syndrome (OSAS) in children and the criteria for selecting treatment are inconsistent. Therefore, the craniofacial and pharyngeal airway morphology of OSAS in children who had undergone drug therapy (non-op group) and OSAS in children who had undergone both drug therapy and surgical therapy (adenotonsillectomy) (op group) were compared. The purpose of this study was to examine the effectiveness of craniofacial morphology and pharyngeal airway morphology analysis in the treatment of children with OSAS.
Methods
The craniofacial and pharyngeal airway morphology of the control group, the non-op group and the op group were compared to examine the differences of each group. The comparison used Mann–Whitney's U test.
Results
A comparison between the non-op and the op groups showed significant differences in the facial axis, mandibular plane angle, ramus plane to the SN (porion and orbit) point, point Pog (pogonion) to the McNamara line, anteroposterior dysplasia indicator (APDI), D-AD1 [the distance between the posterior nasal spine (PNS) point and the nearest adenoid tissue, measured along the PNS–Ba (basion) point plane], D-AD2 (the distance between the PNS point and the nearest adenoid tissue, measured along a line from the PNS point perpendicular to the S (sella turcica)–Ba point plane), upper pharynx and soft palatal length. The op group showed significantly lower values of APDI than the non-op group, indicating that the op group showed a significant occlusion of class II, and that the mandibular bone was positioned posteriorly relative to the maxillary bone.
Conclusions
The op group showed a significant posterior position and backward rotation of the mandibular bone, stenosis of the nasopharyngeal airway and an elongated soft palate compared with the non-op group, and it was speculated that there was a high probability of the necessity of surgical therapy (adenotonsillectomy) when a morphological factor played a major role as a cause of obstructive sleep apnoea. We recommend craniofacial morphology analysis and pharyngeal airway morphology analysis in the diagnosis and treatment planning of OSAS children.
Keywords: OSAS, child, craniofacial morphology, pharyngeal airway morphology
Introduction
In obstructive sleep apnoea syndrome (OSAS) in children, enlarged adenoids and enlarged palatal tonsils are regarded as major causes of sleep apnoea. The morphological characteristics of the craniofacial part and the pharyngeal airway part of OSAS in children include the backward rotation of a mandibular bone, stenosis of the nasopharyngeal airway, etc.1-3 A diagnosis of OSAS in children is made collectively based on overnight polysomnographic examinations and conditions of daily living (somnolence, inactivity, loss of concentration). When treating OSAS children, if enlarged adenoids and enlarged palatal tonsils are the cause of sleep apnoea, drug therapy and adenotonsillectomy are performed.4 However, no consensus has been obtained regarding the diagnostic criteria in general and the criteria for the selection of treatment are inconsistent.4,5
The craniofacial and pharyngeal airway morphology are regarded as causes of influencing the treatment of OSAS in children, but it is rare to use a craniofacial and pharyngeal airway morphology analysis in treating OSAS in children.
Therefore, the craniofacial and pharyngeal airway morphology of OSAS in children who had undergone drug therapy and OSAS in children who had undergone both drug therapy and surgical therapy were compared in order to study the differences in morphology. The purpose of this study was to examine the effectiveness of craniofacial morphology analysis and pharyngeal airway morphology analysis in treatment of children with OSAS.
Materials and methods
Patients under investigation
The patients comprised 20 children with OSAS who had undergone drug therapy (non-op group) and 20 children with OSAS who had undergone both drug therapy (antibiotic, anti-allergic drug) and surgical therapy (adenotonsillectomy) (op group) among the children who visited the outpatient clinic at the Department of Otorhinolaryngology in Saitama Children's Medical Centre, Japan, with frequent respiratory arrest during sleep, fever due to tonsillitis, daytime somnolence, etc as major complaints and were diagnosed as having OSAS based on a overnight sleep examination with APNOMONITOR (Chest M.I., Inc., Tokyo, Japan). The product is a portable sleep monitoring device. The average apnoea hypopnea index (AHI) of the non-op group was 5.51 per h ( ± 6.17 per h) and the average AHI of the op group was 6.98 per h ( ± 8.07 per h). A comparison between the non-op group and the op group did not show significant differences in the AHI. The treatment of OSAS in children began with drug therapy. The effect of treatment was observed for a few months. Subsequently, surgical therapy was performed when no improvement of the symptoms was observed or it was insufficient with drug therapy. Surgical treatment is not the first choice of treatment of OSAS in children. The majority of OSAS patients in this centre are pre-school children. Patients who attended the medical centre between 2004 and 2005 were included in the patient group. After examining the results of treatment, we chose data at random from among each of the patients of drug therapy and surgical therapy. The average age of the non-op group was 5 years 0 months ( ± 9 months) and the average age of the op group was 5 years 5 months ( ± 7 months). Furthermore, the lateral cephalograms of 10 children (control group; average age 5 years 4 months ± 6 months), who had visited the Nihon University School of Dentistry Dental Hospital with mild crowding in the upper or lower anterior dental region and no abnormality in breathing during sleep or in oral function, were used as data in order to elucidate the craniofacial and pharyngeal airway morphology of the non-op group and the op group (patient group). No child in any group had coronal destruction due to caries (mandibular position might change with caries treatment). During the production of the cephalograms the patients were instructed not to swallow. Moreover, no significant difference was observed in the ages among the three groups; all three groups showed a body mass index (BMI) in the control range. The data that were used for the present research were obtained and used with the permission of the patients and their families after the purpose and details of the research were explained.
Measurements
For the analysis of craniofacial morphology, nine measurement items were selected including items in Ricketts et al's6, Miura et al's,7 Matsumoto et al's,8 McNamara's,9 Kim's10 and deBerry-Borowiecki et al's11 analysis methods. For the analysis of airway morphology, six items were selected among the measurement items in McNamara's9, Schulhof's12 and Miles et al's13 analysis methods (Figures 1–3).
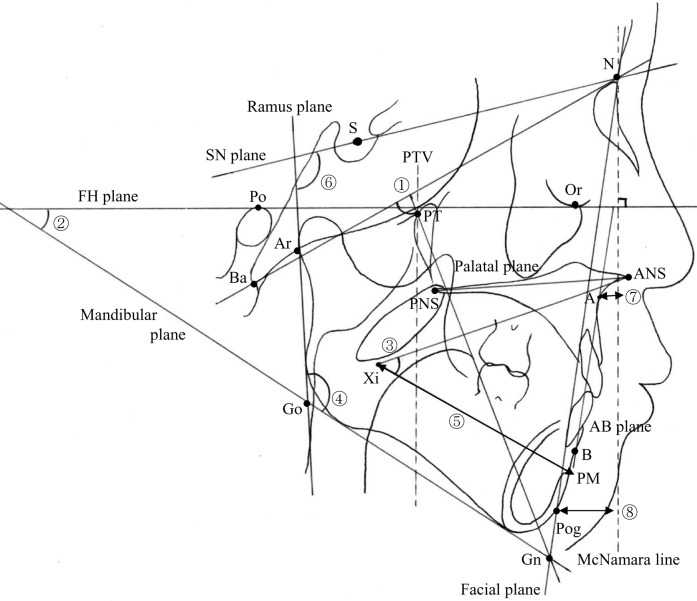
Figure 1.
Measurements of the craniofacial morphology. ◯1 Facial axis: the angle between the Pt (pterygoid point)–Gn (gnathion) point plane and the Ba (basion)–N (nasion) point plane; ◯2 mandibular plane angle: the angle between the frankfort horizontal (FH) plane and the mandibular plane; ◯3 lower facial height: the angle between the anterior nasal spine (ANS)–Xi (pterygomaxillary) point plane and the Xi–protuberance menti (PM) point plane; ◯4 gonial angle: the angle between the mandibular plane and the ramus plane; ◯5 corpus length: the distance between the Xi point and the PM point; ◯6 ramus plane to SN: the angle between the ramus plane and the SN plane [a line connecting the porion (S) and orbit (N) points]; ◯7 point A: the perpendicular distance to the McNamara line from the A point; ◯8 point Pog: the perpendicular distance to the McNamara line from the Pog point; anteroposterior dysplasia indicator (APDI): the total of the facial depth and the A–B plane angle (the angle between the FH plane and the A–B plane) and the palatal plane angle (the angle between the FH plane and the palatal plane)
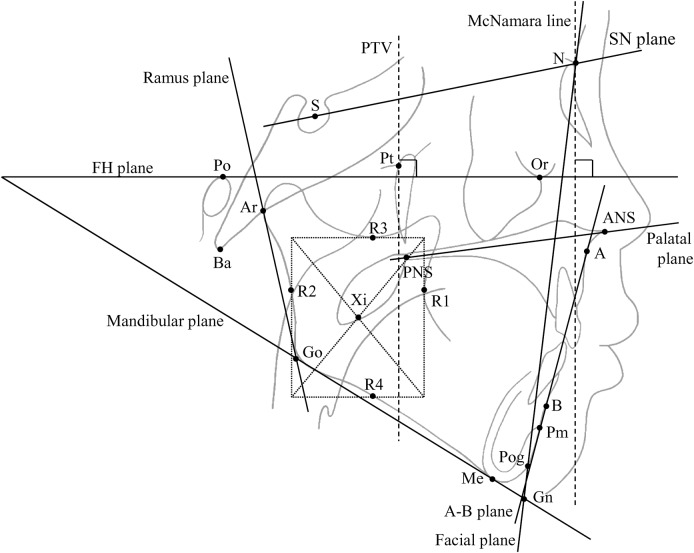
Figure 3.
Landmarks and lines. Landmarks. A point: the deepest point on the concave outline of the upper labial alveolar process; anterior nasal spine (ANS): the most anterior point at the sagittal plane on the bony hard palate; Ar (articulare): the intersection point of the ramus plane and the occipital bone bas-fond inferior margin; B point: the deepest point on the concave outline of the lower labial alveolar process; Ba (basion): the most inferior posterior point of the occipital bone at the anterior margin of the occipital foramen; Gn (gnathion): the point on the chin determined by bisecting the angle formed by the facial and the mandibular plane; Go (gonion): the intersection point of the mandibular plane and the ramus plane; H (hyoid): the most anterior superior point of the body of the hyoid bone; Me (menton): the most inferior point of the mentum section; N (nasion): the most anterior point of the frontonasal suture; Or (orbitale): the most inferior point on the lower border of the bony orbit; posterior nasal spine (PNS): the most posterior point at the sagittal plane on the bony hard palata; Po (porion): the most superior point on the radiolucency of the external and internal auditory meati, located posterior to the mandibular condyle and posterior clivus; Pog (pogonion): the most prominent point of the chin; protuberance menti (PM): the point where the curvature of the anterior border of the symphysis changes from concave to convex; Pt (pterygoid point): the intersection point of the inferior border of the foramen rotundum and the posterior wall of the pterygomaxillary fissure; S (sella turcica): the centre of the pituitary fossa of the sphenoid bone; SPB point: soft palatal back point; SPF point: soft palate front point; UT point: tip of the soft palate; Xi (pterygomaxillary) point: a point located at the centre of the ramus. The location of the Xi is keyed geometrically to the frankfort horizontal (FH) and pterygoid vertical (PTV) planes in four steps: (1) planes are constructed perpendicular to the FH and PTV planes; (2) these constructed planes are tangent to points R1, R2, R3 and R4 on the borders of the ramus; (3) the constructed planes form a rectangle enclosing the ramus; (4) Xi is located in the centre of the rectangle at the intersection of diagonals. Lines. A-B plane: a line connecting the A and B points; facial plane: a line connecting the N and Pog points; FH plane: a line connecting the Po and Or points; mandibular plane: a tangent line to the lower border of the mandible; McNamara line: the perpendicular line which goes through N for FH; palatal plane: a line connecting the ANS and PNS points; PTV plane: a line perpendicular to the FH plane through the PT point; ramus plane: a tangent line on the posterior contour of the ramus ascendens; SN plane: a line connecting the porion (S) and orbit (N) points
Measurement error
The data of cephalograms with unclear images were not used. The frankfort horizontal (FH) plane and the inferior border of the film within ± 5° were used. The first and second authors measured 50 films (the control, non-op and op group) twice with a time interval between measurements of 1 week. Each measurement value was then averaged. The difference in the measured values did not exceed the standard deviation (SD) when all three measurements were averaged. As for the error range actually measured, each length was within 0.5 mm and each angle was within 1°.
Statistical evaluation
The patient group was compared with the control group. The mean and standard deviation of the craniofacial and pharyngeal airway morphology analyses in the control group and the patient groups were calculated and the differences between the control group and the patient groups were tested using Mann–Whitney's U test. The mean and standard deviation of the craniofacial and pharyngeal airway morphology analyses in the non-op and the op groups were then calculated and the differences between the non-op group and the op group were tested using Mann–Whitney's U test. The non-op and op groups were compared to examine whether there was difference of morphology with different treatments.
Results
Comparison of the craniofacial and pharyngeal airway morphology between the control and patient groups
In the craniofacial morphology, the values for facial axis, point Pog (pogonion) to the McNamara line and anteroposterior dysplasia indicator (APDI) were significantly lower and those for mandibular plane angle and ramus plane to the SN (porion and orbit) plane were significantly higher in the patient group than in the control group (Figure 1). In the pharyngeal airway morphology, the patient group showed significantly lower values for D–AD1 [the distance between the posterior nasal spine (PNS) point and the nearest adenoid tissue, measured along the PNS–Ba (basion) point plane], D–AD2 [the distance between the PNS point and the nearest adenoid tissue, measured along a line from the PNS point perpendicular to the S (sella turcica)–Ba point plane] and upper pharynx and showed significantly higher values for soft palatal thickness and soft palatal length (Figure 2).
Figure 2.
Measurements of the pharyngeal airway morphology. ◯1 D–AD1: the distance between the posterior nasal spine (PNS) point and the nearest adenoid tissue, measured along the PNS–Ba (basion) point plane; ◯2 D–AD2: the distance between the PNS point and the nearest adenoid tissue, measured along a line from the PNS point perpendicular to the S (sella turcica)–Ba point plane; ◯3 upper pharynx: the shortest distance from the upper surface of the palatine velum to the adenoid tissue; ◯4 lower pharynx: the distance between the intersection point where the tongue base meets the lower contour, the mandible and the posterior pharyngeal wall; ◯5 soft palatal thickness: the distance between the soft palate front (SPF) point and the soft palate back (SPB) points (the maximum dimension of the soft palatal between its oral and nasal surfaces); ◯6 soft palatal length: the distance between the PNS point and the UT (tip of the soft palate) point
Comparison of the craniofacial and pharyngeal airway morphology between the non-op and op groups
Table 1 shows the mean value and standard deviation in each group in the analysis of the craniofacial and pharyngeal airway morphology and results of analysis of their differences. In the craniofacial morphology, the values for facial axis, point Pog to the McNamara line and APDI were significantly lower and those for mandibular plane angle and ramus plane to the SN were significantly higher in the op group than in the non-op group. In the pharyngeal airway morphology, the op group showed significantly lower values for D–AD1, D–AD2 and upper pharynx and showed a significantly higher value for soft palatal length.
Table 1. Mean values and standard deviations (SD) in craniofacial/pharyngeal airway morphology items in the non-op and op groups and results of analysis of their differences.
| Measurement | Non-op groupa (n = 20) |
Op groupa (n = 20) |
Differences | ||
| Mean | SD | Mean | SD | ||
| Craniofacial and airway morphology items | |||||
| Facial axis (degrees) | 86.02 | (3.27) | 82.69 | (3.99) | b |
| Mandibular plane angle (degrees) | 28.98 | (2.53) | 32.35 | (5.27) | c |
| Lower facial height (degees) | 45.78 | (3.05) | 47.77 | (3.21) | c |
| Gonial angle (degrees) | 128.07 | (4.42) | 125.05 | (24.16) | ns |
| Corpus length (mm) | 56.07 | (3.11) | 54.76 | (3.72) | ns |
| Ramus plane to SN (degrees) | 89.82 | (4.17) | 93.14 | (6.20) | c |
| Point A to McNamara line (mm) | 0.83 | (2.33) | 0.73 | (3.62) | ns |
| Point Pog to McNamara line (mm) | −9.14 | (3.82) | −12.73 | (6.40) | c |
| APDI (degrees) | 77.24 | (3.34) | 73.95 | (3.10) | b |
| Pharyngeal airway morphology items | |||||
| D-AD1 (mm) | 8.97 | (4.41) | 5.91 | (2.95) | c |
| D-AD2 (mm) | 9.50 | (1.82) | 7.75 | (1.74) | b |
| Upper pharynx (mm) | 4.49 | (2.32) | 2.98 | (2.98) | b |
| Lower pharynx (mm) | 13.34 | (3.47) | 14.56 | (3.66) | ns |
| Soft palatal thickness (mm) | 8.52 | (1.59) | 8.24 | (1.18) | ns |
| Soft palatal length (mm) | 23.16 | (3.01) | 25.76 | (3.53) | c |
AD, adenoid tissue; APDI, anteroposterior dysplasia indicator; ns, not significant; Pog, pogonion; SD, standard deviation; SN, porion and orbit.
aThe non-op group indicates the children who had undergone drug therapy. The op group indicates the children who had undergone both drug therapy and surgical therapy (adenotonsillectomy).
bp < 0.01.
cp < 0.05.
Discussion
Children with OSAS display symptoms such as night-time respiratory arrest, daytime somnolence, loss of concentration and reduced secretion of growth hormone; however, sleep apnoea cannot be overlooked in children who develop quickly. The criteria for selecting the treatment of OSAS in children are inconsistent and it is rare to analyse the craniofacial and pharyngeal airway morphology when performing treatment. Therefore, the craniofacial and pharyngeal airway morphology of OSAS in children who have undergone drug therapy and OSAS in children who have undergone both drug therapy and surgical therapy (adenotonsillectomy) were compared in order to study the differences in morphology.
Comparison of the craniofacial and pharyngeal airway morphology between the control and patient groups
A comparison of the craniofacial and pharyngeal airway morphology between the control and the patient groups resulted in the craniofacial morphology of the patient group showing a posterior position and backward rotation of the mandibular bone and the pharyngeal airway morphology showed stenosis of the nasopharyngeal airway, as well as an elongated and thickened soft palate. Therefore, the patient group showed the characteristics of craniofacial and pharyngeal airway morphology that is seen in OSAS in children.1-3
Comparison of the craniofacial and pharyngeal airway morphology between the non-op and op groups
According to the results of the present research, in the craniofacial morphology analysis the op group showed significantly lower values of facial axis and point Pog to the McNamara line, which indicate the anterior and posterior positions of the mandibular bone compared with the non-op group, so the mandibular bone was positioned posteriorly. It showed significantly higher values of mandibular plane angle and ramus plane to SN, which indicated a rotational direction of a mandibular bone, thus indicating the mandibular bone rotated posteriorly. When diagnosing the occlusion of the maxillary and mandibular dentitions, the angle classification (classes I, II and III) are used; maxillary and mandibular dentitions at control occlusal positions is diagnosed as class I, a mandibular dentition at a more posterior position than the control position relative to the maxillary dentition is class II and a mandibular dentition at a more anterior position is class III. Furthermore, when the presence of bone structural factors is investigated regarding occlusion, APDI10,14 may be used. According to Kim,10 when APDI is smaller, the tendency for class II becomes strong. According to the results of the present research, the op group showed a significantly lower value of APDI compared with the non-op group, thus indicating that the op group showed a significant occlusion of class II and the mandibular bone was positioned posteriorly relative to the maxillary bone. When researching craniofacial morphology in OSAS in children, it has been reported that a posterior position of the mandibular bone and the backward rotation of the mandibular bone are observed and because of these characteristics, sinkage of the tongue root easily occurs during sleep, causing apnoea.1-3 Accordingly, the op group more significantly showed the craniofacial morphology that was characteristic of OSAS in children compared with the non-op group. In addition, in the pharyngeal airway morphology analysis D-AD1, D-AD2 and upper pharynx showed significantly lower values, so the op group showed a significantly stenosed morphology of the nasopharyngeal airway. The soft palatal length showed a significantly higher value, illustrating morphology with a long soft palate. In the research of OSAS in children, it has been reported that stenosis of the nasopharyngeal airway morphology was observed.2,3 In research of the soft palate morphology in adults, Kitamura et al15 explained that it is effective to measure the length of the soft plate when diagnosing OSAS and Mochizuki16 explained that an elongated uvula causes a valve mechanism during sleep as a cause of apnoea. According to a report in which the soft palate morphology of OSAS in children was investigated,3 the soft palatal length showed a larger value than that in healthy children. Therefore, the op groupmore significantly showed a pharyngeal airway morphology that is more characteristic of OSAS in children compared with the non-op group.
Conclusion
In OSAS in children, it is speculated that there is a high probability that surgical therapy (adenotonsillectomy) may be required when morphological factors play a major role as a cause of obstructive sleep apnoea. We recommend craniofacial morphology analysis and pharyngeal airway morphology analysis in the diagnosis and treatment planning of OSAS children.
Footnotes
Part of this research was subsidized by grants-in-aid for scientific research (young scientists B) for 2008–2010.
References
- 1.Linder-Aronson S. Adenoids. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the denition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl 1970;265:1–132 [PubMed] [Google Scholar]
- 2.Shintani T, Asakura K, Kataura A. Adenotonsillar hypertrophy and skeletal morphology of children with obstructive sleep apnea syndrome. Acta Otolaryngol Suppl 1996;523:222–224 [PubMed] [Google Scholar]
- 3.Kawashima S, Niikuni N, Chia-hung L, Takahasi Y, Kohno M, Nakajima I, et al. Cephalometric comparisons of craniofacial and upper airway structures in young children with obstructive sleep apnea syndrome. Ear Nose Throat J 2000; 79: 499–502, 505–506 [PubMed] [Google Scholar]
- 4.Ameli F, Brocchetti F, Semino L, Fibbi A. Adenotonsillectomy in obstructive sleep apnea syndrome. Proposal of a surgical decision-taking algorithm. Int J Pediatr Otorhinolaryngol 2007;71:729–734 [DOI] [PubMed] [Google Scholar]
- 5.Sargi Z, Younis RT. Pediatric obstructive sleep apnea: current management. ORL J Otorhinolaryngol Relat Spec 2007;69:340–344 [DOI] [PubMed] [Google Scholar]
- 6.Ricketts RM, Roth RH, Chaconas SJ, Schulhof RJ, Engel GA. Orthodontic diagnosis and planning: their roles in preventive and rehabilitative dentistry. Denver, CO: Rocky Mountain;Orthodontics; 1982 [Google Scholar]
- 7.Miura F, Inoue N, Suzuki K. Cephalometric standards for Japanese according to the Steiner analysis. Am J Orthod 1965;51:288–295 [DOI] [PubMed] [Google Scholar]
- 8.Matsumoto N. Cephalometric analysis in patients with obstructive sleep apnea syndrome: effectiveness of measuring skeletal morphology and soft tissue dimensions. Nippon Jibiinkoka Gakkai Kaiho 2002;105:1147–1156 [DOI] [PubMed] [Google Scholar]
- 9.McNamara JA., Jr A method of cephalometric evaluation. Am J Orthod 1984;86:449–469 [DOI] [PubMed] [Google Scholar]
- 10.Kim YH. Overbite depth indicator with particular reference to anterior open-bite. Am J Orthod 1974;65:586–611 [DOI] [PubMed] [Google Scholar]
- 11.deBerry-Borowiecki B, Kukwa A, Blanks RH. Cephalometric analysis for diagnosis and treatment of obstructive sleep apnea. Laryngoscope 1988;98:226–234 [DOI] [PubMed] [Google Scholar]
- 12.Schulhof RJ. Consideration of airway in orthodontics. J Clin Orthod 1978;12:440–444 [PubMed] [Google Scholar]
- 13.Miles PG, O'Reilly M, Close J. The reliability of upper airway landmark identification. Aust Orthod J 1995;14:3–6 [PubMed] [Google Scholar]
- 14.Freudenthaler JW, Celar AG, Schneider B. Overbite depth and anteroposterior dysplasia indicators: the relationship between occlusal and skeletal patterns using the receiver operating characteristic (ROC) analysis. Eur J Orthod 2000;22:75–83 [DOI] [PubMed] [Google Scholar]
- 15.Kitamura T, Sakabe A, Ueda N, Shiomori T, Udaka T, Ohbuchi T, et al. Usefulness of cephalometry and pharyngeal findings in the primary diagnosis of obstructive sleep apnea syndrome. Nippon Jibiinkoka Gakkai Kaiho 2008;111:695–700 [DOI] [PubMed] [Google Scholar]
- 16.Mochizuki T. Examination of low palatal arch with long low-hanging soft palatal in obstructive sleep apnea syndrome and cephalometry. Nippon Jibiinkoka Gakkai Kaiho 1997;100:937–945 [DOI] [PubMed] [Google Scholar]