Abstract
Objective
The aim of this study was to characterize mandibular fracture locations using 64-slice multidetector CT (MDCT).
Methods
CT scans of 138 patients with mandibular fractures who underwent 64-slice MDCT were studied. Mandibular fractures were classified into five types: median, paramedian, angle, condylar and coronoid process. Statistical analysis for the relationship between multiple fractures and type of mandibular fractures was performed using χ2 test with Fisher's exact test.
Results
The percentage of multiple mandibular fractures was 80.9% median type, 74.3% paramedian type, 52.9% angle type and 60.9% condylar type. The resultant data showed a significant relationship between multiple fractures and the median type (p = 0.000), paramedian type (p = 0.002) and condylar type (p = 0.003).
Conclusion
The results suggest that multiple fractures are related to the type of mandibular fractures.
Keywords: multidetector computed tomography, mandibular trauma, multiple fractures
Introduction
CT is being increasingly applied to define the fracture location and the degree of dislocation in fractures accompanying craniomaxillofacial trauma.1 Multidetector CT (MDCT) allows high-quality multiplanar reformation (MPR) and isotropic viewing, all of which improve the diagnostic power of this imaging modality, thus benefiting facial trauma patients.2-4 The application of 64-slice MDCT technology to multitrauma imaging affords important advantages in injury detection and characterization.5 Decreasing slice thickness and the ability to routinely acquire whole body imaging using isotropic data sets have resulted in true multiplanar CT imaging.
Maxillofacial trauma has been investigated worldwide because it affects a significant percentage of trauma patients.6-11 The mandible is one of the most commonly fractured maxillofacial bones.6,8-11 Knowledge of the fracture pattern and the aetiology of the injury is important for the management of maxillofacial fractures.12 Characteristic features of the mandible have been observed in age and gender distributions and the site and severity of fractures according to the cause of trauma.13-18 However, few studies have been concerned with the evaluation of the craniomaxillofacial trauma using 64-slice MDCT.
The surgical team needs to have an accurate understanding of the facial injuries pre-operatively.19 The aim of this study was the characterization of mandibular fracture locations using 64-slice MDCT.
Materials and methods
CT scans of 138 patients (101 males, 37 females; age 4–87 years, mean age 35.7 years) with mandibular fractures who underwent 64-slice MDCT in the Department of Radiology at the Nihon University School of Dentistry at Matsudo, Chiba, Japan, from April 2006 to May 2010 were studied. All participants read and signed an informed consent form. This study was approved by the Ethics Committee of the University School of Dentistry (No. EC10–039).
CT imaging was performed with a 64-slice MDCT system (Aquilion 64; Toshiba Medical Systems, Tokyo, Japan). All patients were scanned using the clinically routine protocol for craniomaxillofacial examination at our hospital as follows: tube voltage, 120 kV; tube current, 100 mA; field of view, 240×240 mm; and helical pitch, 41. Imaging included axial (0.50 mm), MPR (3.00 mm) and three-dimensional (3D) images. The MDCT images were interpreted using a medical liquid crystal display monitor (RadiForce G31; Eizo Nanami, Ishikawa, Japan). All images were independently evaluated by two oral radiologists and any differences were resolved by forced consensus.
The relationship between multiple fractures and type of mandibular fractures was analysed. Mandibular fractures were classified according to the distribution described by Lieger et al20 into five types: median, paramedian, angle, condylar and coronoid process. Statistical analysis for the relationship between number of fractures, such as single and multiple fractures, and type of mandibular fractures was performed using χ2 test with Fisher's exact test. These analyses were performed with the statistical package SPSS version 14.0 (SPSS Japan, Tokyo, Japan). p-values <0.05 were considered to indicate statistical significance.
Results
Table 1 shows the number of mandibular fractures in 138 patients. The condylar type was most frequent (47.1%), followed by the median (20.9%) and the paramedian types (16.0%).
Table 1. Number of mandibular fractures in 138 patients.
| Type of fracture | Number | Percentage (%) |
| Condylar | 106 (R 55, L 51) | 47.1 |
| Median | 47 (M 47) | 20.9 |
| Paramedian | 36 (R 19, L 17) | 16.0 |
| Angle | 35 (R 16, L 19) | 15.6 |
| Coronoid process | 1 (R 1, L 0) | 0.4 |
| Total | 225 (R 91, M 47, L 87) | 100 |
L, left; M, median; R, right.
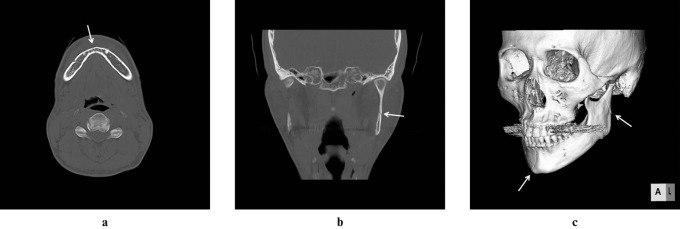
The percentage of multiple fractures was 50.7% of all mandibular fracture patients (Table 2). In all multiple fractures patients, the median and condylar types were the most frequent, followed by the paramedian and condylar and median and bilateral condylar types. Figure 1 shows MDCT images of median and condylar type.
Table 2. Patient distribution according to type of mandibular fractures in 138 patients.
| Single fractures |
Multiple fractures |
||
| Type of fracture | Patients (%) | Type of fracture | Patients (%) |
| Condylar | 34 (24.6) | Median and condylar | 17 (12.3) |
| Angle | 16 (11.6) | Paramedian and condylar | 14 (10.1) |
| Median | 9 (6.5) | Median and bi-condylar | 13 (9.4) |
| Paramedian | 9 (6.5) | Paramedian and angle | 9 (6.5) |
| Median and angle | 5 (3.6) | ||
| Bi-condylar | 5 (3.6) | ||
| Angle and condylar | 2 (1.4) | ||
| Median and paramedian | 1 (0.7) | ||
| Bi-paramedian | 1 (0.7) | ||
| Median and bi-angle | 1 (0.7) | ||
| Angle, condylar and coronoid process | 1 (0.7) | ||
| Median, paramedian and bi-condylar | 1 (0.7) | ||
| Total | 68 (49.3) | 70 (50.7) | |
Bi-, bilateral.
Figure 1.
A 40-year-old male after a fall on the chin at home. (a) Axial image demonstrates a median fracture (arrow). (b) Coronal image demonstrates a condylar fracture (arrow). (c) Three-dimensional image to better advantage depicts median and condylar fractures (arrows)
Table 3 shows the relationship between multiple fractures and type of mandibular fractures in 138 patients. The percentage of multiple fractures was 80.9% of the median type, 74.3% of the paramedian type, 52.9% of the angle type and 60.9% of the condylar type. The resultant data showed a significant relationship between multiple fractures and the median type (p = 0.000), the paramedian type (p = 0.002) and the condylar type (p = 0.003).
Table 3. Relationship between multiple fractures and type of mandibular fractures in 138 patients.
| Number of fractures | ||||
| Type of fracture | Single | Multiple | Total | p-valuea |
| Median | 9 (19.1%) | 38 (80.9%) | 47 (100%) | 0.000 |
| Paramedian | 9 (25.7%) | 26 (74.3%) | 3s (100%) | 0.002 |
| Angle | 16 (47.1%) | 18 (52.9%) | 34 (100%) | 0.844 |
| Condylar | 34 (39.1%) | 53 (60.9%) | 87 (100%) | 0.003 |
aSingle vs multiple.
Discussion
MDCT can easily detect and characterize injuries not only of the body and spine, but also of intracranial and maxillofacial injuries.21,22 Salonen et al2-4 showed that MDCT can detect the non-displaced fractures and also provides valuable 3D morphology of the more complex injuries in facial trauma using 4-slice MDCT. However, few studies have been concerned with the evaluation of craniomaxillofacial trauma using 64-slice MDCT. In our experience, 64-slice MDCT with reformatted images and 3D reconstructions helps to interpret mandibular fractures, especially the fracture location, the degree of dislocation and the relationship between multiple fractures and type of mandibular fractures.
Iida et al6 reported that the most common mandibular fracture site was the condyle (33.6%), followed by the angle (21.7%). Ahmed et al9 indicated that regarding the distribution of mandibular fractures, the majority (25.0%) occurred in the condyle and 23.0% in the angle. On the other hand, Yamamoto et al12 showed that the condyle (38.2%) and median (27.0%) were most frequently involved in the mandible. This study demonstrated that the condylar type was most common (47.1%), followed by the median type (20.9%). The results were in line with previous studies given that these parts of the face are prone to injury for anatomical reasons.
In this study, the percentage of multiple fractures was 50.7% of all mandibular fracture patients. Iida et al6 reported that multiple fractures of the mandible were present in 48.6% of patients. Yamamoto et al18 showed that fracture lines were multiple in 44.4% of all mandibular fracture patients. These reports suggest no difference of percentage in mandibular fractures between single and multiple fractures.
Sawazaki et al17 indicated that median fractures were significantly associated with both unilateral and bilateral fractures of the mandibular condyle. This study showed that the median and condylar types were most frequent, followed by the paramedian and condylar types and the median and bilateral condylar types in multiple mandibular fractures. Our resultant data also indicated a significant relationship between multiple fractures and type of mandibular fractures, such as median, paramedian and condylar. These results suggest that the mandible distributes the force of impact and fractures frequently occur in the condylar region. We consider that if a force applied to the mandible is distributed, it affects the weakest point in the mandibular arch and causes extreme bending and tensile failure at that point. Therefore, condylar fractures may be tension failures in response to bending of the mandibular neck.
Regarding radiation dose of CT, Mah et al23 showed that the effective dose for the imaging of the maxillomandibular volume with cone beam CT (CBCT) is significantly lower than that with CT imaging methods. Ilguy et al24 reported that more detailed information was obtained about dentoalveolar fractures with CBCT compared with CT and conventional radiography. However, we consider that 64-slice MDCT is an effective tool to assess craniomaxillofacial trauma, especially the fracture location and the degree of dislocation, oedema and haemorrhage.
In conclusion, this study suggests that multiple fractures are related to the type of mandibular fractures.
References
- 1.Schuknecht B, Graetz K. Radiologic assessment of maxillofacial, mandibular, and skull base trauma. Eur Radiol 2005;15:560–568 [DOI] [PubMed] [Google Scholar]
- 2.Salonen EM, Koivikko MP, Koskinen SK. Multidetector computed tomography imaging of facial trauma in accidental falls from heights. Acta Radiol 2007;48:449–455 [DOI] [PubMed] [Google Scholar]
- 3.Salonen EM, Koivikko MP, Koskinen SK. Acute facial trauma in falling accidents: MDCT analysis of 500 patients. Emerg Radiol 2008;15:241–247 [DOI] [PubMed] [Google Scholar]
- 4.Salonen EM, Koivikko MP, Koskinen SK. Violence-related facial trauma: analysis of multidetector computed tomography findings of 727 patients. Dentomaxillofac Radiol 2010;39:107–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson SW, Lucey BC, Rhea JT, Soto JA. 64 MDCT in multiple trauma patients: imaging manifestations and clinical implications of active extravasation. Emerg Radiol 2007;14:151–159 [DOI] [PubMed] [Google Scholar]
- 6.Iida S, Kogo M, Sugiura T, Mima T, Matsuya T. Retrospective analysis of 1502 patients with facial fractures. Int J Oral Maxillofac Surg 2001;30:286–290 [DOI] [PubMed] [Google Scholar]
- 7.Gassner R, Tuli T, Hachl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9543 cases with 21067 injuries. J Craniomaxillofac Surg 2003;31:51–61 [DOI] [PubMed] [Google Scholar]
- 8.Fasola AO, Nyako EA, Obiechina AE, Arotiba JT. Trends in the characteristics of maxillofacial fractures in Nigeria. J Oral Maxillofac Surg 2003;61:1140–1143 [DOI] [PubMed] [Google Scholar]
- 9.Al Ahmed HE, Jaber MA, Fanas SHA, Karas M. The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: a review of 230 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;98:166–170 [DOI] [PubMed] [Google Scholar]
- 10.Brasileiro BF, Passeri LA. Epidemiological analysis of maxillofacial fractures in Brazil: a 5-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:28–34 [DOI] [PubMed] [Google Scholar]
- 11.Bakardjiev A, Pechalova P. Maxillofacial fractures in Southern Bulgaria: a retrospective study of 1706 cases. J Craniomaxillofac Surg 2007;35:147–150 [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto K, Matsusue Y, Murakami K, Horita S, Matsubara Y, Sugiura T, et al. Maxillofacial fractures due to work-related accidents. J Craniomaxillofac Surg 2011;39:182–186 [DOI] [PubMed] [Google Scholar]
- 13.Ogundare BO, Bonnick A, Bayley N. Pattern of mandibular fractures in an urban major trauma center. J Oral Maxillofac Surg 2003;61:713–718 [DOI] [PubMed] [Google Scholar]
- 14.Iida S, Hassfeld S, Reuther T, Nomura K, Muhling J. Relationship between the risk of mandibular angle fractures and the status of incompletely erupted mandibular third molar. J Craniomaxillofac Surg 2005;33:158–163 [DOI] [PubMed] [Google Scholar]
- 15.Zachariades N, Mezitis M, Mourouzis C, Papadakis D, Spanou A. Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections on treatment and proposals. J Craniomaxillofac Surg 2006;34:421–432 [DOI] [PubMed] [Google Scholar]
- 16.Atilgan S, Erol B, Yaman F, Yilmaz N, Ucan MC. Mandibular fractures: a comparative analysis between young and adult patients in the southeast region of Turkey. J Appl Oral Sci 2010;18:17–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sawazaki R, Lima SM, Jr, Asprino L, Moreira RWF, de Moraes M. Incidence and patterns of mandibular condyle fractures. J Oral Maxillofac Surg 2010;68:1252–1259 [DOI] [PubMed] [Google Scholar]
- 18.Yamamoto K, Kuraki M, Kurihara M, Matsusue Y, Murakami K, Horita S, et al. Maxillofacial fractures resulting from falls. J Oral Maxillofac Surg 2010;68:1602–1607 [DOI] [PubMed] [Google Scholar]
- 19.Hopper RA, Salemy S, Sze RW. Diagnosis of midface fractures with CT: what the surgeon needs to know. Radiographics 2006;26:783–793 [DOI] [PubMed] [Google Scholar]
- 20.Lieger O, Zix J, Kruse A, Iizuka T. Dental injuries in association with facial fractures. J Oral Maxillofac Surg 2009;67:1680–1684 [DOI] [PubMed] [Google Scholar]
- 21.Bensch FV, Kiuru MJ, Koivikko MP, Koskinen SK. Spine fractures in falling accidents: analysis of multidetector CT findings. Eur Radiol 2004;14:618–624 [DOI] [PubMed] [Google Scholar]
- 22.Turner BG, Rhea JT, Thrall JH, Small AB, Novelline RA. Trends in the use of CT and radiography in the evaluation of facial trauma, 1992–2002: implications for current costs. Am J Roentgenol 2004;183:751–754 [DOI] [PubMed] [Google Scholar]
- 23.Mah JK, Danforth RA, Bumann A, Hatcher D. Radiation absorbed in maxillofacial imaging with a new dental computed tomography device. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;96:508–513 [DOI] [PubMed] [Google Scholar]
- 24.Ilguy D, Ilguy M, Fisekcioglu E, Bayirli G. Detection of jaw and root fractures using cone beam computed tomography: a case report. Dentomaxillofac Radiol 2009;38:169–173 [DOI] [PubMed] [Google Scholar]