Abstract
The imaging appearance of neurofibromas is well described; however, macroscopic fat in a neurofibroma has been sparsely reported and intralesional ossification has only been documented twice in the literature. We describe a diffuse neurofibroma presenting as a hemifacial mass, atypical for the presence of extensive intralesional ossification and fat; the diagnosis was suggested on identification of other associated radiological features of neurofibromatosis.
Keywords: neurofibroma, diffuse neurofibroma, ossification, fat, ossified neurofibroma
Introduction
In comparison with the localized and plexiform variants, diffuse neurofibromas are infrequently encountered in clinical practice. Also, the radiological characteristics of diffuse neurofibromas are sparsely studied. This, in conjunction with the presence of atypical features, can make it difficult to distinguish between diffuse neurofibromas and other angiomatous or fat-containing lesions. We discuss the imaging appearance of a diffuse neurofibroma of the face, which was extremely unusual for the presence of abundant intralesional fat and extensive ossification. Incidental detection of other attributes of neurofibromatosis helped in suggesting the diagnosis, which was confirmed on histopathology.
Case report
A 20-year-old man presented with a bulging right-sided hemifacial mass. The mass had been present for about 10 years and had gradually increased in size over the last 2 years. Clinical examination was remarkable owing to the presence of a large, firm, non-tender, non-fluctuant mass in the right cheek extending into the submandibular and parotid regions. There was no local warmth or bruit over the mass. The personal and occupational history was non-contributory. He was referred for CT to delineate the extent of involvement. CT revealed a large heterogeneous mass in the right buccal, masticator and parapharyngeal space. The mass was seen extending into the floor of the mouth with compression and displacement of the submandibular gland and the horizontal ramus of the mandible. The surrounding structures were merely displaced and no obvious infiltration was seen. Notable, however, was the presence of intralesional fat and extensive ossification (Figure 1a). These findings were also corroborated with an MR study (Figure 1b). In keeping with this unusual appearance, a differential diagnosis of a teratoma, osteolipoma and osteochondroma was considered. However, inspection of the scan in the bone window revealed a dysplastic ipsilateral sphenoid wing (Figure 2a) with widening of the foramen ovale (Figure 2b). Probing into the patient’s history also revealed that his brother had multiple cutaneous nodules all over the body. In keeping with the associated findings, a provisional diagnosis of a diffuse neurofibroma on a background of neurofibromatosis was offered. Other radiographic signs that may be seen in the head and neck in neurofibromatosis include macrocephaly, absence of greater and lesser wings of the sphenoid, and enlarged orbits. However, none of these was seen in our patient. Subsequently, he underwent a biopsy of the mass and histopathological examination revealed spindle-shaped cells with serpentine nuclei in a collagenous matrix. Also seen was mineralized osteoid. Overall features were in keeping with the diagnosis of diffuse neurofibroma (Figure 3). The infiltrative nature of the lesion precluded a surgical excision and close clinical and imaging follow-up to monitor for lesion size stability and possible malignant transformation was advised.
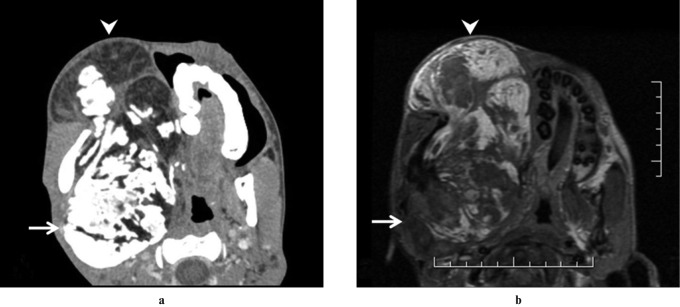
Figure 1.
Axial contrast-enhanced CT image in soft-tissue window (a) shows macroscopic fat (arrowhead) and dense bone (arrow) in the right sided hemifacial mass. Concurrence is noted on the axial unenhanced T1 weighted (time of repetition 540 ms, time of echo 12 ms) MR image (b), with areas of macroscopic fat appearing hyperintense (arrowhead) and bone appearing hypointense (arrow) relative to skeletal muscle
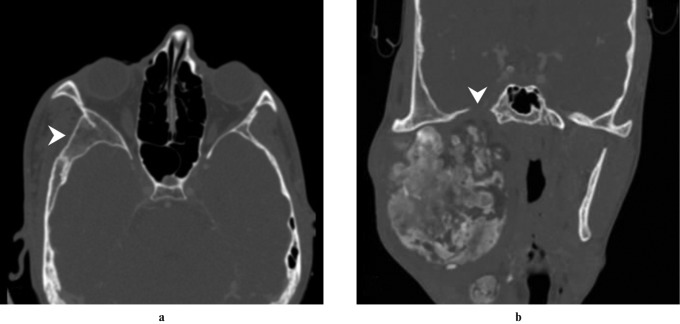
Figure 2.
Axial CT image in bone window (a) shows dysplastic right sphenoid wing (arrowhead). Coronal multiplanar reformatted CT image in bone window (b) shows widening of the right-sided foramen ovale (arrowhead)
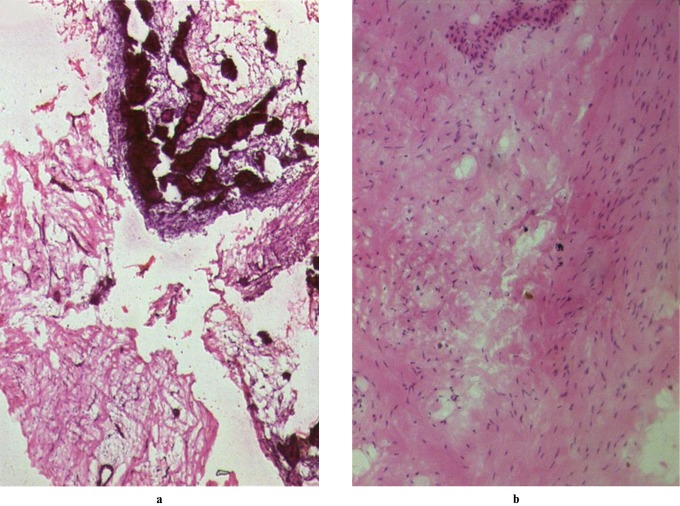
Figure 3.
(a) Histological section reveals ossified bone and fragments of spindle cell lesion (haematoxylin and eosin ×20). (b) Diffuse proliferation of spindle cells with wavy nuclei illustrate the neurogenic nature of the tumour (haematoxylin and eosin ×100)
Discussion
Neurofibromas are benign peripheral nerve sheath tumours characterized by the proliferation of Schwann cells, perineural cells and fibroblasts.1 On the basis of growth pattern, these tumours have been classified into three subtypes: localized, diffuse and plexiform, diffuse being the least common.2 Conventionally, diffuse neurofibromas are believed to involve head and neck regions in young adults and children.3 Neurofibromatosis-1 reportedly occurs in approximately 10% of patients with diffuse neurofibroma.4 However, Hassell et al2 recently documented contradictory findings in patients with a mean age of 41 years and predominant involvement of the trunk and extremities with an increased incidence of neurofibromatosis. This indicates the need for further studies with larger numbers of patients for the evolution of our understanding of diffuse neurofibromas and its associates.
Clinically, a diffuse neurofibroma is a poorly marginated, plaque-like infiltrative lesion involving the skin and subcutaneous tissues, present generally for a long duration of time. There may or may not be other associated stigmata of neurofibromatosis.2 Only a few studies are centred on the imaging appearance of diffuse neurofibroma.2,5 On ultrasound, these appear as subcutaneous hyperechoic masses with interspersed hypoechoic interconnecting tubular strands.5 On MRI, typically diffuse neurofibromas are plaque-like infiltrating masses involving the skin and subcutaneous tissue characterized by the presence of linear or reticular strands. These strands are of intermediate signal intensity on T1 weighted images and appear hyperintense on T2 weighted images in comparison with muscle. On contrast-enhanced sequences, diffuse neurofibromas enhance intensely, owing to prominent internal vascularity.2 This reticular infiltrative pattern is characteristic and distinguishes diffuse neurofibromas from the localized and plexiform variants, which appear as a well-defined nodule and a serpiginous lesion, respectively. The description of the CT appearance of diffuse neurofibromas is restricted to anecdotes and has not previously been studied. Diffuse neurofibromas can show variable density relative to skeletal muscle depending on the macroscopic composition of the tumour. The enhancement characteristics are not well established.2
Intratumoral macroscopic fat in a neurofibroma has been documented, albeit in a few cases. The precise cause of fat accumulation within a neurofibroma is unknown. Ahn et al6 postulated that it may be because of senescent change or chronic injury, whereas Van-Bernal and González-Vela7 suggested that fat cells are intrinsic to the tumour and originate from mesenchymal differentiation of neuroectodermal cells. Calcification in a neurofibroma of uncertain origin has also been documented only twice in the literature.8,9 In both these cases, the diagnosis was of localized neurofibroma. Abundant intratumoral fat with extensive ossification in a diffuse neurofibroma as seen in our case has never previously been reported. This made the diagnosis challenging, although the dysplastic ipsilateral sphenoid wing and widened foramen ovale provided clues. We believe that ossification, although exceedingly unusual, could also be a manifestation of the aging process akin to fat accumulation, as suggested by Ahn et al.6 Furthermore, the neurofibroma reported by Kapoor et al8 was in the foot, whereas our patient had a neurofibroma on the face. These sites are prone to repetitive manipulation and minor injuries which could theoretically play a role in ossification.
On histopathology, typical diffuse neurofibromas localize to the dermis and subcutaneous tissues. These tend to envelop rather than destroy adjacent structures. The tumour is composed of spindle-shaped cells with round nuclei with eosinophilic cytoplasm in a fine fibrillary collagen background. Wagner–Meissner bodies may be seen and the tumour cells show diffuse staining with antibodies against S-100 protein.10
Surgical excision is the mainstay in the treatment of diffuse neurofibromas. The aim of surgery is to restore cosmesis and address occasional symptoms associated with the size of the tumour. Owing to the infiltrative nature, complete surgical excision of diffuse neurofibromas is often not feasible. It is recommended that these patients be followed up to monitor for recurrence, possible malignant transformation and development of overt neurofibromatosis.3
Thus, in addition to delineating the extent of the tumour, which is often the purpose of referrals for imaging of head and neck masses, a meticulous scrutiny of the associated radiological features can help in providing invaluable inputs to the diagnosis, even in the face of the most unusual imaging appearances, as shown in our case.
References
- 1.Scheithauer BW, Woodruff JM, Erlandson RA. Tumors of the peripheral nervous system. Atlas of tumor pathology. Washington, DC: Armed Forces Institute of Pathology; 1997 [Google Scholar]
- 2.Hassell DS, Bancroft LW, Kransdorf JW, Peterson JJ, Berquist TH, Murphey MD, et al. Imaging appearance of diffuse neurofibroma. AJR Am J Roentgenol 2008;190:582–588 [DOI] [PubMed] [Google Scholar]
- 3.van Zuuren EJ, Posma AN. Diffuse neurofibroma of the lower back. J Am Acad Dermatol 2003;48:938–940 [DOI] [PubMed] [Google Scholar]
- 4.Peh WCG, Shek TWH, Yip DKH. Magnetic resonance imaging of subcutaneous diffuse neurofibroma. Br J Radiol 1997;70:1180–1183 [DOI] [PubMed] [Google Scholar]
- 5.Chen W, Jia JW, Wang JR. Soft tissue diffuse neurofibromas: sonographic findings. J Ultrasound Med 2007;26:513–518 [DOI] [PubMed] [Google Scholar]
- 6.Ahn SK, Ahn HJ, Kim TH, Hwang SM, Choi EH, Lee SH. Intratumoral fat in neurofibroma. Am J Dermatopathol 2002;24:326–329 [DOI] [PubMed] [Google Scholar]
- 7.Van-Bernal JF, González-Vela MC. Cutaneous lipomatous neurofibroma: characterization and frequency. J Cutan Pathol 2005;32:274–279 [DOI] [PubMed] [Google Scholar]
- 8.Kapoor R, Mittal KP, Jayaram G. Solitary neurofibroma of the foot—an unusual case with extensive calcification and ossification. Australas Radiol 1986;30:150–152 [DOI] [PubMed] [Google Scholar]
- 9.Sarma DP, Robichaux J, Fondak A. Ossified neurofibroma. J La State Med Soc 1983;135:22–23 [PubMed] [Google Scholar]
- 10.Ito H, Akagi O, Nomura N, Tahara E. Giant pigmented tumor of the scalp—a diffuse neurofibroma or congenital naevus showing neurofibromatous changes? Immunohistochemical and electron microscopic studies. Histopathology 1988;13:181–189 [DOI] [PubMed] [Google Scholar]