Abstract
Objectives
This study aimed to investigate the value of ultrasound in the identification of benign and malignant parotid masses.
Methods
Data of 189 patients with parotid gland masses undergoing ultrasound-guided fine-needle aspiration (FNA), core biopsy or surgery were reviewed retrospectively and the presumed sonographic diagnoses were compared with the histopathology. The sensitivity, specificity and accuracy of sonographic diagnoses were assessed and the sonographic characteristics of those lesions, including shape, margin, echogenicity, echotexture and vascularization, were studied.
Results
Of the 189 patients, the final pathological diagnosis included 18 malignant tumours and 171 benign masses; the presumed sonographic diagnoses showed 165 cases as benign and probably benign masses (11 cases were confirmed malignant, 154 cases benign) and 24 cases were diagnosed as probably malignant and malignant masses (7 cases were confirmed malignant, 17 cases benign). The sensitivity, specificity, positive predictive value, negative predictive value and accuracy of ultrasound for the diagnosis of parotid gland masses were 38.9%, 90.1%, 29.2%, 93.3% and 85.2%, respectively, and accuracy for malignant masses was 20%. The sonographic characteristics of parotid masses between benign and malignant lesions had no significant differences. The parotid gland masses in this study included pleomorphic adenoma, Warthin's tumour, retention cyst, haemangiomas, chronic granuloma, lymphoma, fibrolipoma, abscess, basal cell adenoma, oncocytoma, lymphatic tuberculosis, myoepithelioma, neurilemmoma, mucoepidermoid carcinoma, adenoid cystic carcinoma, alveolar soft part sarcoma and retinal blastoma (metastasis).
Conclusions
It is challenging to use sonography for differentiating between benign and malignant parotid gland masses. To make a definite diagnosis, ultrasound-guided FNA or core biopsy is advocated.
Keywords: parotid gland, mass, benign, malignant, ultrasound
Introduction
Parotid gland masses include benign tumours, malignant tumours and chronic inflammatory diseases. Identification of benign or malignant lesions is linked with management. Ultrasound plays an important role in the diagnosis of space-occupying lesions. Some studies1-4 found that ultrasound was able to differentiate between benign and malignant parotid masses with high accuracy while other studies5-9 presented opposing conclusions. The aim of this study was to assess the role of ultrasound in the evaluation of benignity and malignancy of parotid gland masses.
Materials and methods
The data of 189 patients (91 males, 98 females; average age 42.3 years; range, 1.5–76 years) who had undergone ultrasound-guided fine-needle aspiration (FNA) cytology, core biopsy or surgery between January 2005 and May 2010 were retrospectively reviewed. The data were obtained from Picture Archiving and Communication Systems of the Affiliated Hospital of Hainan Medical College, China, and the presumed sonographic diagnosis and sonographic characteristics were studied. The presumed sonographic diagnosis and ultrasound-guided FNA cytology or core biopsy were made at real time ultrasound imaging and the imaging study of parotid masses was done by experienced sonologists. The ultrasound systems used were Logiq 9 and Voluson 730 Expert (GE Healthcare Systems, Waukesha, WI) and HP5500, HD11 XE (HP Medical Systems, Dalian, China), and the frequency of the transducers was 10 MHz–12 MHz.
The sonographic characteristics were reviewed in consensus by two sonologists who had 9 years and 10 years' experience of parotid ultrasound examination, respectively, and who were blinded to the presumed and final diagnosis. The interpretation was based on individual ultrasound features of parotid gland masses with reference to reports1-4, 7 and was combined with our experience, including dimensions, shape (oval, lobulated or irregular), margins (circumscribed, spiculated or ill-defined), echogenicity (anechoic, hypoechoic, isoechoic or hyperechoic), echotexture (homogeneous or heterogeneous) and vascularization. Vascularization was assessed in four grades: Grade 1 indicates no vessels visible in the mass in colour Doppler flow imaging (CDFI) low-flow mode; Grade 2 indicates a few vessel segments of no more than three blood vessels visible in the whole mass; Grade 3 indicates up to five vessels visible in the mass; and Grade 4 indicates more than five vessels visible in the mass.
The sonographic characteristics suggesting probably malignant or malignant masses were irregular shape, spiculated or ill-defined margin, heterogeneous echotexture, punctate calcification and vascularization (Grade 3–4). The sonographic characteristics suggesting probably benign or benign mass were round or ovoid shape, circumscribed margin, homogeneous echotexture and vascularization (Grade 1–2).
The presumed sonographic diagnoses were categorized in regard to the above references. The analysis of sonographic characteristics associated with benign and malignant lesions was based on pathological diagnosis and the final diagnosis was based on the pathological confirmation of parotid masses which had undergone FNA cytology, biopsy or surgical resection.
Data analysis
Comparing the presumed sonographic diagnosis of parotid gland masses with the pathological results, the sensitivity, specificity, positive predictive value, negative predictive value and accuracy were determined. χ2 tests were used for the analyses of ultrasound characteristics of benign and malignant masses and p < 0.05 was considered statistically significant. The software used was SPSS (Version 11.0, SPSS, Inc., an IBM Company, Chicago, IL).
This study was approved by our institutional review board with a waiver of informed consent.
Results
Of the 189 patients, the final pathological diagnosis included 18 malignant tumours and 171 benign masses. The presumed sonographic diagnoses showed 165 cases as benign and probably benign masses (143 cases were excised and 22 cases underwent
FNA or core biopsy; 11 cases were confirmed malignant and 154 cases benign) while 24 cases were diagnosed as probably malignant and malignant masses (20 cases were excised and 4 cases underwent FNA or core biopsy; 7 cases were confirmed malignant and 17 cases benign).
The maximum dimension of benign and malignant masses was 26.4 mm (± 7.4 mm) and 27.1 mm (± 6.5 mm), respectively. Pathological classification and the numfber of parotid masses are shown in Table 1 and the sonographic characteristics of pathologically confirmed parotid masses are shown in Table 2 and illustrated on Figures 1–5. The sensitivity, specificity, positive predictive value, negative predictive value and accuracy of ultrasound for the diagnosis of parotid gland masses were 38.9%, 90.1%, 29.2%, 93.3% and 85.2%, respectively, and accuracy for malignant masses was 20%. 17 benign masses that were misdiagnosed as malignant masses were in fact lymphatic tuberculosis (Figure 5), pleomorphic adenoma and Warthin's tumour. 11 malignant masses that were misdiagnosed as benign masses were mucoepidermoid carcinoma (7 cases; Figure 4), metastasis of retinal blastoma (1 case), alveolar soft part sarcoma (1 case) and adenoid cystic carcinoma (2 cases).
Table 1. Pathological classification and number of parotid masses.
| Pathological classification | Number |
| Pleomorphic adenoma | 63 |
| Warthin's tumour | 47 |
| Retention and simple cyst | 8 |
| Haemangioma | 10 |
| Granuloma | 18 |
| Lymphoma | 4 |
| Fibrolipoma | 5 |
| Abscess | 2 |
| Basal cell adenoma | 3 |
| Oncocytoma | 4 |
| Lymphatic tuberculosis | 3 |
| Myoepithelioma | 3 |
| Neurilemmoma | 1 |
| Mucoepidermoid carcinoma | 13 |
| Adenoid cystic carcinoma | 3 |
| Alveolar soft part sarcoma | 1 |
| Retinal blastoma (metastasis) | 1 |
Table 2. Sonographic characteristics of pathologically confirmed parotid masses.
| Parameter | Benign | Malignant | p-value | |
| Shape | Ovoid | 108 | 12 | > 0.05 |
| Lobulated | 23 | 2 | > 0.05 | |
| Irregular | 40 | 4 | > 0.05 | |
| Margin | Circumscribed | 158 | 15 | > 0.05 |
| Spiculated | 2 | 1 | > 0.05 | |
| Ill defined | 11 | 2 | > 0.05 | |
| Echogenicity | Anechoic | 16 | 0 | > 0.05 |
| Hypoechoic | 149 | 18 | > 0.05 | |
| Isoechoic | 6 | 0 | > 0.05 | |
| Echotexture | Homogeneous | 15 | 3 | > 0.05 |
| Heterogeneous | 156 | 15 | > 0.05 | |
| Calcification | 20 | 3 | > 0.05 | |
| Vascularization | 0 | 62 | 5 | > 0.05 |
| + | 75 | 7 | > 0.05 | |
| ++ | 20 | 3 | > 0.05 | |
| +++ | 14 | 3 | > 0.05 |
0, grade 1 vascularization of the parotid masses; +, grade 2 vascularization of the parotid masses; ++, grade 3 vascularization of the parotid masses; +++, grade 4 vascularization of the parotid masses.
Figure 1.

Sonographic image shows a heterogeneous hypoechoic ovoid mass in the left parotid in a 36-year-old male with well-defined margin, posterior echogenicity enhancement and mild edge refraction. The presumed diagnosis was benign lesion and the pathological diagnosis was pleomorphic adenoma
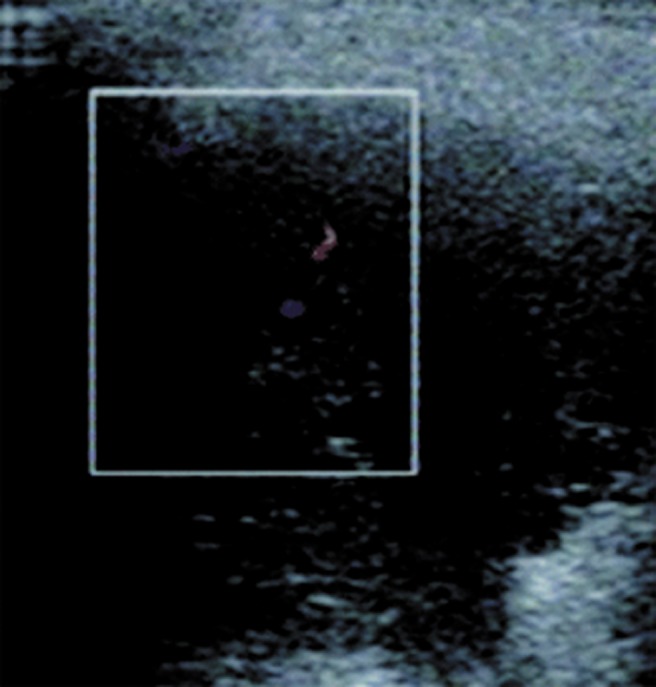
Figure 5.

Sonographic image shows a heterogeneous hypoechoic ovoid mass in the right parotid in a 27-year-old male with punctate calcifications, well-defined margin, posterior echogenicity enhancement and distinct edge refraction. The presumed diagnosis was probably malignant lesion and the pathological diagnosis was lymphatic tuberculosis
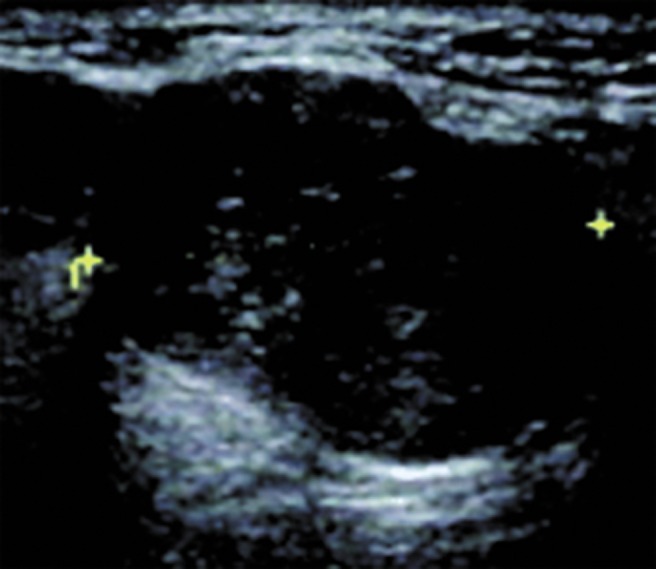
Figure 4.
Sonographic image shows a heterogeneous hypoechoic lobulated mass in the left parotid in a 52-year-old female with circumscribed margin, posterior echogenicity enhancement, distinct edge refraction and fair vascularization in colour Doppler imaging. The presumed diagnosis was probably benign lesion and the pathological diagnosis was mucoepidermoid carcinoma
Figure 2.
Sonographic image shows a heterogeneous hypoechoic ovoid mass in the left parotid in a 68-year-old female with punctate calcifications, circumscribed margin, posterior echogenicity enhancement and distinct edge refraction. The presumed diagnosis was benign lesion and the pathological diagnosis was Warthin's tumour
Figure 3.
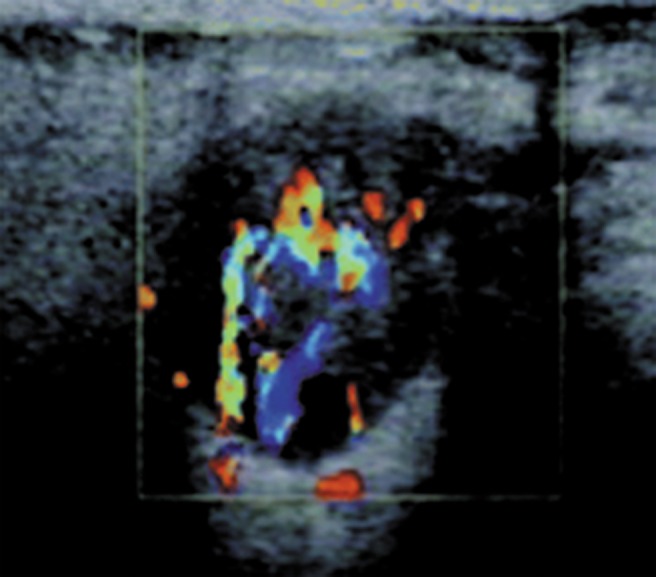
Sonographic image shows a heterogeneous hypoechoic ovoid mass in the right parotid in a 47-year-old male with circumscribed margin, posterior echogenicity enhancement, distinct edge refraction and much vascularization in colour Doppler imaging. The presumed diagnosis was probably benign lesion and the pathological diagnosis was oncocytoma
Discussion
The parotid gland masses in this study included benign tumours, malignant tumours and inflammatory or lymphatic lesions; the majority were benign lesions and only a very small amount (9.5%) were malignant, which was similar to some authors' findings.10,11 However, the proportion of malignant lesions in our study was far less than in a report by Lin et al,12 where out of 271 patients who underwent parotidectomy, 229 (85%) had benign tumours, 33 (12%) had malignant tumours and 9 had chronic inflammatory disease (3%). Our results were also lower than those of Mohammed et al11 who studied 242 patients, of whom 183 (75.6%) had benign neoplasms, 51 (21.1%) had malignant neoplasms and 8 (3.3%) had inflammatory or lymphatic lesions, suggesting that parotid malignant tumours in our region were fewer than in other regions.
In this study, the most common benign parotid tumour was pleomorphic adenoma and the most frequent malignant tumour was mucoepidermoid carcinoma, which was consistent with some studies.12-15 The results of the sensitivity, specificity, positive predictive value, negative predictive value and accuracy of ultrasound for the diagnosis of parotid gland masses and the accuracy for malignant masses indicated that the overall level of sonographic diagnosis, was low, which suggested that ultrasound examination was unable to make a sufficiently definite diagnosis, and this is in disagreement with some studies.1-4 The sonographic characteristics of parotid masses including shape, margin, echogenicity, echotexture and vascularization between benign and malignant lesions had no significant difference, which indicated that it is hard to distinguish malignant parotid masses from benign masses using sonography and that this method is unable to distinguish between different benign or malignant lesions because some tumours and lesions have similar characteristics.1-4,16-18 This was in disagreement with other studies.1-4, 6, 7 Sonographic features of infiltration of parotid malignant tumours were not found in this study and are seldom reported in other literature. CDFI may find parotid masses blood supply information, but the distribution in benign and malignant lesions had no significant difference and its value was limited, which was consistent with Bradley et al8 and Schick et al.9
The potential limitations of the study were that the sample size was not large enough, some small nodules and large size masses without FNA or pathological results were not included, a few cases did not undergo ultrasound examination and were not included, and the clinical data, including history, speed of growth, pain, facial palsy and so on, were not enrolled, which may affect the study of the parotid gland masses.
In conclusion, it is challenging to use ultrasound for the differentiation between benign and malignant parotid gland masses. To make a definite diagnosis, ultrasound-guided FNA cytology or core biopsy is advocated.
References
- 1.Białek EJ, Jakubowski W, Karpińska G. Role of ultrasonography in diagnosis and differentiation of pleomorphic adenomas. Arch Otolaryngol Head Neck Surg 2003;129:929–933 [DOI] [PubMed] [Google Scholar]
- 2.Kim J, Kim EK, Park CS, Choi YS, Kim YH, Choi EC. Characteristic sonographic findings of Warthin's tumor in the parotid gland. J Clin Ultrasound 2004;32:78–81 [DOI] [PubMed] [Google Scholar]
- 3.Howlett DC. High resolution ultrasound assessment of the parotid gland. Br J Radiol 2003;76:271–277 [DOI] [PubMed] [Google Scholar]
- 4.Yonetsu K, Ohki M, Kumazawa S, Eida S, Sumi M, Nakamura T. Parotid tumors: differentiation of benign and malignant tumors with quantitative sonographic analyses. Ultrasound Med Biol 2004;30:567–574 [DOI] [PubMed] [Google Scholar]
- 5.Bozzato A, Zenk J, Greess H, Hornung J, Gottwald F, Rabe C, et al. Potential of ultrasound diagnosis for parotid tumors: analysis of qualitative and quantitative parameters. Otolaryngol Head Neck Surg 2007;137:642–646 [DOI] [PubMed] [Google Scholar]
- 6.de Ru JA, van Leeuwen MS, van Benthem PP, Velthuis BK, Sie-Go DM, Hordijk GJ. Do magnetic resonance imaging and ultrasound add anything to the preoperative workup of parotid gland tumors? J Oral Maxillofac Surg 2007;65:945–952 [DOI] [PubMed] [Google Scholar]
- 7.Lamont JP, McCarty TM, Fisher TL, Kuhn JA. Prospective evaluation of office-based parotid ultrasound. Ann Surg Oncol 2001;8:720–722 [DOI] [PubMed] [Google Scholar]
- 8.Bradley MJ, Durham LH, Lancer JM. The role of colour flow Doppler in the investigation of the salivary gland tumour. Clin Radiol 2000;55:759–762 [DOI] [PubMed] [Google Scholar]
- 9.Schick S, Steiner E, Gahleitner A, Böhm P, Helbich T, Ba-Ssalamah A, et al. Differentiation of benign and malignant tumors of the parotid gland: value of pulsed Doppler and color Doppler sonography. Eur Radiol 1998;8:1462–1467 [DOI] [PubMed] [Google Scholar]
- 10.Li LJ, Li Y, Wen YM, Liu H, Zhao HW. Clinical analysis of salivary gland tumor cases in West China in past 50 years. Oral Oncol 2008;44:187–192 [DOI] [PubMed] [Google Scholar]
- 11.Mohammed F, Asaria J, Payne RJ, Freeman JL. Retrospective review of 242 consecutive patients treated surgically for parotid gland tumours. J Otolaryngol Head Neck Surg 2008;37:340–346 [PubMed] [Google Scholar]
- 12.Lin CC, Tsai MH, Huang CC, Hua CH, Tseng HC, Huang ST. Parotid tumors: a 10-year experience. Am J Otolaryngol 2008;29:94–100 [DOI] [PubMed] [Google Scholar]
- 13.Drivas EL, Skoulakis CE, Symvoulakism EK, Bizaki AG, Lachanas VA, Bizakis JG. Pattern of parotid gland tumors on Crete, Greece: a retrospective study of 131 cases. Med Sci Monit 2007;13:CR136–140 [PubMed] [Google Scholar]
- 14.Musani MA, Sohail Z, Zafar S, Malik S. Morphological pattern of parotid gland tumours. J Coll Physicians Surg Pak 2008;18:274–277 [PubMed] [Google Scholar]
- 15.Takahama A, Jr, Almeida OP, Kowalski LP. Parotid neoplasms: analysis of 600 patients attended at a single institution. Braz J Otorhinolaryngol 2009;75:497–501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yasumoto M, Yoshimura R, Sunaba K, Shibuya H. Sonographic appearances of malignant lymphoma of the salivary glands. J Clin Ultrasound 2001;29:491–498 [DOI] [PubMed] [Google Scholar]
- 17.Zacharia TT, Ittoop A, Perumpillichira JJ, Chavhan G. Sonographic appearance of a congenital parotid gland hemangiolymphangioma simulating malignancy in an infant. J Clin Ultrasound 2003;31:493–496 [DOI] [PubMed] [Google Scholar]
- 18.Eichhorn KW, Arapakis I, Ridder GJ. Malignant non-Hodgkin's lymphoma mimicking a benign parotid tumor: sonographic findings. J Clin Ultrasound 2002;30:42–44 [DOI] [PubMed] [Google Scholar]


