Abstract
The purpose of this article is to report 20 cases of ossifying fibroma involving the jaw bone and to review the literature of this lesion. All the cases had adequate radiographs and clinical information. Varying shapes of the lesion including cystic lesion and mixed density lesion are presented, including two massive expansile lesions, which measured more than 10 cm.
Keywords: ossifying fibroma, plain X-ray, jaw bone, mandible, bone neoplasm
Introduction
Ossifying fibroma (OF) is classified as, and behaves like, a benign bone neoplasm. It is often considered to be a type of fibro-osseous lesion (FOL). It can affect both the mandible and the maxilla, particularly the mandible. This bone tumour consists of highly cellular, fibrous tissue that contains varying amounts of calcified tissue resembling bone, cementum or both.
In 1968, Hamner et al1 analysed 249 cases of fibro-osseous jaw lesions of periodontal membrane origin and classified them. In 1973, Waldron and Giansanti 2 reported 65 cases (of which 43 cases had adequate clinical histories and radiographs) and concluded that this group of lesions was best considered as a spectrum of processes arising from cells in the periodontal ligament. In 1985, Eversole et al3 described the radiographic characteristics of central ossifying fibroma, and two major patterns were noted, expansile unilocular radiolucencies and multilocular configuration.
Although some cases of OF have been reported in the published literature, massive expansile lesions measuring more than 10 cm, like the cases in this study, were rare. The adequate radiographs of the cases of OF presented can further help us to understand the variable radiographic appearances of this lesion.
Case reports
20 cases of OF were obtained from the Department of Oral Radiology, West China College of Stomatology, Sichuan University, from the years 1968 to 2002. The final diagnoses of all OF cases were confirmed by histopathological examination.
The patient clinical data are shown in Table 1. The study was based on 20 patients, 9 males and 11 females. The mean age was 27.8 years, with a range of 6–57 years. 16 cases were located in the mandible and the other 4 cases in the maxilla.
Table 1. Clinical information on 20 cases of ossifying fibroma.
| Case no. | Gender | Age (years) | Chief complaint | Oral examination |
| 1 | F | 39 | A painless swelling in the right mandible for 6 months | A painless hard mass approximately 4×5×4 cm3 in the right mandibular angle region with the expansion of the right mandible well defined |
| 2 | F | 6 | Painless expansion of the left mandible for 25 days | A hard and fixed mass with buccolingual expansion |
| 3 | F | 45 | A painless mass in the left mandible for more than 2 years | A hard and immovable mass in the left mandible |
| 4 | F | 30 | Expansion of the mandible for 6 months | A hard and fixed mass in the anterior teeth region, with buccolingual expansion of the bone |
| 5 | F | 31 | A swelling in the right mandible for several days | A painless mass in the lingual surface of the right mandible, about 6 × 3 cm2 |
| 6 | M | 38 | A painless swelling in the left mandible for more than 10 years | A raised hard mass approximately 1.5 cm in diameter in the anterior teeth region of the left mandible, the second incisor and the canine shifting because of the mass |
| 7 | F | 20 | Expansion of the left face for 1.5 months | A swelling in the left hard palate from the first premolar to the second molar |
| 8 | F | 12 | A symptomless mass for 2 weeks | A hard mass with buccolingual expansion in the left mandible |
| 9 | F | 12 | An osteal swelling at the chin for 8 years | Bulging in the anterior teeth area of the mandible |
| 10 | M | 17 | A swelling in the left face for 3 years, and recent rapid development | A hard expansion in the premolar region of the left mandible with the lingual displacement of the premolars |
| 11 | M | 30 | A painless osteal mass in the right maxilla for 7 years | A hard and fixed mass in the right maxilla, about 4×3×1.5 cm, with the absence of the maxillary right canine to the second molar |
| 12 | M | 45 | A painless swelling in the left mandible for more than 1 year, with recent pain | A hard mass in the posterior teeth region with local mucosa erosion |
| 13 | M | 15 | Right facial deformity for more than 8 years | A giant mass in the right face with the expansion of the hard palate |
| 14 | M | 12 | A painless bulge in the right mandible for more than 4 years | A fixed and well-defined mass, approximately 5 cm in diameter, with two soft and movable lymph nodes in the neck |
| 15 | M | 35 | Cellulitis of submandibular space for 5 days | A hard mass in the right mandible, 3 cm in diameter |
| 16 | M | 33 | Bulging in the mandible for more than 7 years, recurring 6 months after operation | Expansion of the whole mandible, about 10×8×7 cm3 |
| 17 | F | 20 | A swelling in the right maxilla for 10 months | A hard mass, about 2.5 cm in diameter with the absence of 7-4, first premolar to second molar |
| 18 | F | 44 | A symptomless mass in the right mandible for more than 2 months | A fixed osteal mass in the anterior region |
| 19 | F | 57 | A bulging in the right mandible for more than 10 years | Buccal expansion of the right mandible with the absence of the second and third molars |
| 20 | M | 15 | A symptomless swelling mass for more than 6 months | A round hard and smooth mass in the right mandible, about 5 cm in diameter, the first and second molars lingual displacing |
12 patients showed obvious facial asymmetry and the other 8 patients showed only the affected side plumped up. 19 patients came to the hospital with a history of gradual swelling of the jaw, 1 of whom felt a little pain; the rest had no pain. One patient was admitted to hospital with cellulitis of submandibular space, and the mass was found inadvertently during the intraoral examination. Hard texture, immovability and a clear boundary line were present in all patients.
The patient radiological data are shown in Table 2, and the radiological diagnosis in Table 3. Based on the radiographic appearances of the OF the lesions may occur at different positions on the jaw bone and present in varying shapes.
Table 2. Radiological information on 20 cases of ossifying fibroma.
| Case no. | Radiographic appearance |
| 1 | Round-like, unicystic, obvious expansion, at the molar region of the right mandible |
| 2 | Oval, unicystic, with a tooth in it, at left mandibular ascending ramus |
| 3 | Round-like, small, unicystic, between the mandibular left premolars |
| 4 | Oval radiolucent cyst, at the apex area from the mandibular right canine to left first premolar |
| 5 | Round-like, radiolucent cyst, at the root of the second premolar and the first molar of the right mandible |
| 6 | Round, unicystic, at the chin from the right canine to the left canine |
| 7 | Irregular, multicystic, well defined, at the left premolar region of the maxilla |
| 8 | Irregular, well defined, multicystic, from the left molar region of the mandible to the mandibular ascending ramus |
| 9 | Round, well defined, medium-density, at the chin |
| 10 | Round-like, mixture of radiolucent and radiopaque tissue, at the left premolar region of the mandible |
| 11 | Round-like, honeycombed septum, at the premolar and canine region of the right maxilla with the expansion of maxillary antral lumen |
| 12 | Oval, radiopaque, pushing the adjacent teeth, between the first and second molars at the left mandible |
| 13 | Round, large, medium density, occupying two-thirds of the face |
| 14 | Round, large, medium density, obvious expansion, occupying the whole right part of the mandible |
| 15 | Round, mixed density, at the molar of the right mandible |
| 16 | Round and large, obvious expansion, involving two sides of the mandible |
| 17 | Irregular, high density, at the right premolar and maxillary sinus |
| 18 | Irregular, radiopaque, relatively well defined, at the region from the right first premolar to the left second premolar |
| 19 | Irregular, relatively radiopaque, obvious expansion, at the molar region of the right mandible |
| 20 | Oval, well defined, radiolucent, at right premolar region before operation; irregular, honeycombed septum, 5 years after operation; irregular, ill defined, radiopaque, bigger 20 years after operation |
Table 3. Radiological diagnosis.
| Case no. | Radiological diagnosis |
| 1 | Calcifying epithelial odontogenic tumour |
| 2 | Ossifying fibroma |
| 3 | Calcifying odontogenic cyst |
| 4 | Ossifying fibroma |
| 5 | Ossifying fibroma |
| 6 | Odontogenic cyst or tumour |
| 7 | Odontogenic cyst |
| 8 | Ameloblastoma |
| 9 | Ameloblastoma or fibro-osseous lesion |
| 10 | Fibro-osseous lesion |
| 11 | Fibro-osseous lesion |
| 12 | Odontogenic fibroma |
| 13 | Fibro-osseous fibroma |
| 14 | Fibro-osseous lesion |
| 15 | Fibro-osseous lesion or benign cementoblastoma |
| 16 | Ossifying fibroma |
| 17 | Complex odontoma or osteochondroma |
| 18 | Ossifying fibroma |
| 19 | Odontogenic benign tumour |
| 20 | Ameloblastoma or odontogenic cyst |
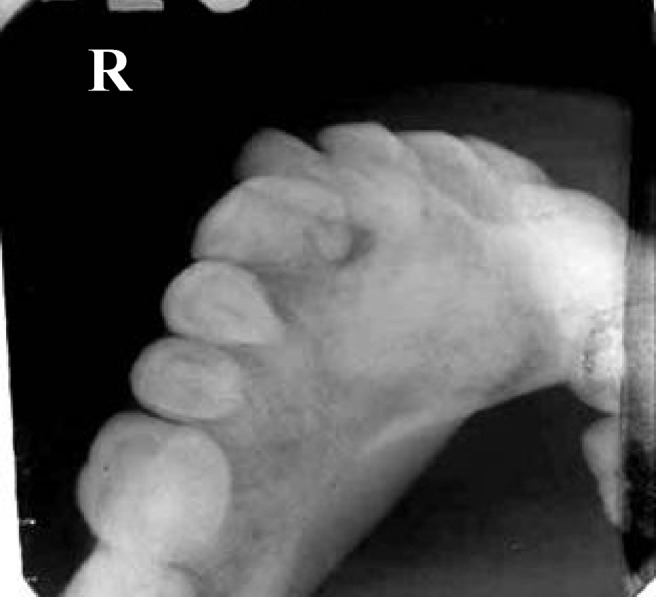
There were eight cases showing cystic lesions, of which six were unicystic (75%) and two were multicystic (25%). The radiographic appearance of case 5 demonstrated a classic unilocular cyst-like lesion with an irregular high-density mass in it. The lesion was located at the apex region from the mandibular right canine to the left first premolar. A radiopaque line at the periphery separated the internal radiolucent portion from the surrounding normal bone, so the boundary between the lesion and normal mandibular bone was easy to distinguish (Figure 1). The other five cases (cases 1–4 and case 6) which presented as unicystic lesions had similar radiographic appearances involving various ranges. The radiographic appearance of case 8 demonstrated an irregular multilocular lesion with the resorption of the affected teeth roots. Some honeycombed septa were scattered in the lesion. The lesion occupied almost the whole of the left mandibular ascending ramus and extended to the apex area of the left second premolar. The lesion was bulging and the cortex of mandibular bone was thinned (Figure 2). Case 7 also presented multicystic lesions but without obvious root resorption.
Figure 1.

Case 5. Panoramic radiograph showing a unicystic lesion at chin region. The image between the lesion and normal bone was easy to distinguish
Figure 2.

Case 8. Panoramic radiograph showing a multicystic lesion with the resorption of the affected teeth roots. Some honeycombed septa are scattered in the lesion. The lesion was bulging and the cortex of mandibular bone was thinned
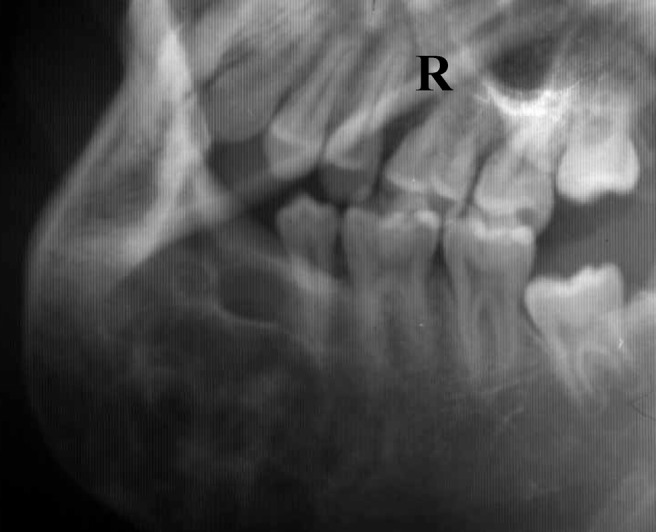
Another 11 cases of OF chiefly revealed a mixed-density mass, of which the internal structure was a mixture of radiolucent and radiopaque tissue. In four cases of this kind, a radiolucent band of capsule at the periphery separated the more mature internal radiopaque portion from the surrounding normal bone (Figure 3). However, in another seven cases, the radiographic border of the tumour appeared relatively defined and corticated (Figure 4). The tumours in two cases grew so large that the X-ray image showed a giant mass. The lesion of case 13 was located at the right side of the maxilla, occupying two-thirds of the face. The radiographic appearance revealed a round-like medium-density mass with cancellate dense lines in it (Figure 5). The tumour grew much larger and the neighbouring teeth had obviously migrated compared with 3 years previously (Figures 6 and 7). Another giant tumour, involving two sides of the mandible in case 16, was a recurrent case. The patient underwent local resection of the lesion at the left side of the mandible at the first presentation, and then underwent another resection of part of the jaw and bioceramic prosthesis implantation after 9 months because of the first recurrence. 5 years later, the tumour again recurred and involved the bilateral jaw bone. The left lateral position radiograph showed the rest of the bioceramic prosthesis (Figures 8 and 9).
Figure 3.
Case 18. Lower occlusal film showing the border between the lesion and the normal bone as a low-density area, thus it is more indistinct than the cystic lesions
Figure 4.

Case 15. An oblique lateral projection showed that there was much high-density mass as cancellate dense lines in the lesion. The border between the lesion and the normal bone was relatively defined; there was often a dense bone line surrounding the lesion. The mesial root of the right second molar was resorbed
Figure 5.
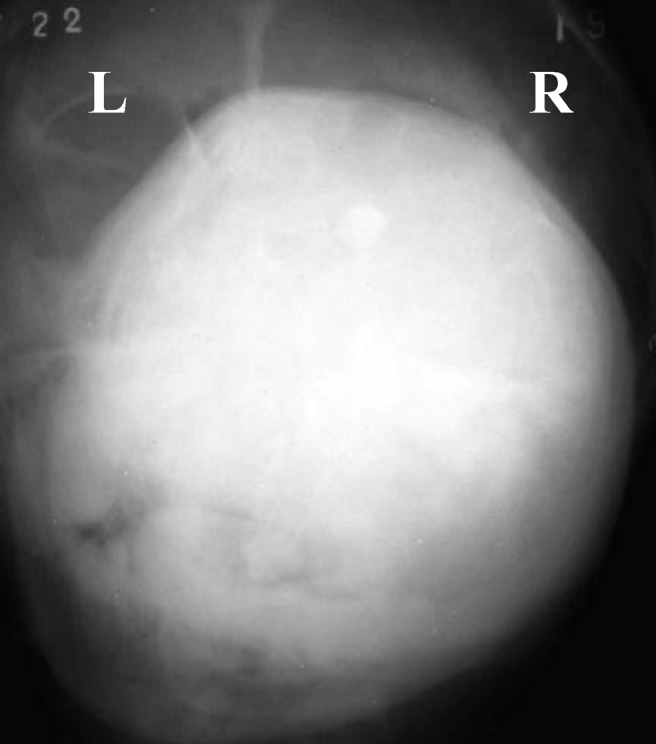
Case 13. Posteroanterior cephalometric projection showing the lesion occupying two-thirds of the patient's face, located at the right side of the maxillary bone
Figure 6.

Case 13. Lateral cephalometric projection, 1984. The maxillary lateral cephalometric projections revealed a round-like medium-density mass with cancellate dense lines in it
Figure 7.

Case 13. Lateral cephalometric projection, 1987. The tumour has grown much larger and the affected teeth have obviously migrated, compared with 3 years previously
Figure 8.
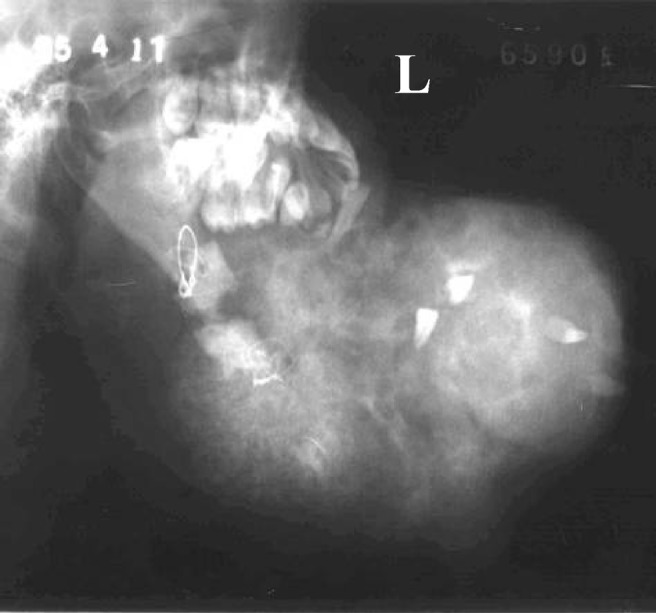
Case 16. Left lateral cephalometric projection. The radiographs in Figures 8 and 9 demonstrate that the tumour involved the bilateral jaw bone. The left mandible had been restored by bioceramic prosthesis
Figure 9.
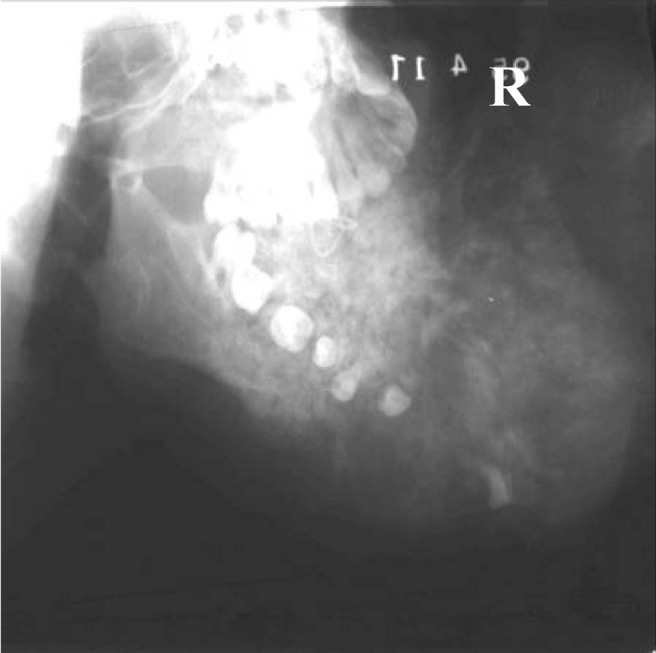
Case 16. Right lateral cephalometric projection
The last special case was located at the apex of the canine and first premolar in the right mandible, featuring both the cystic and mixed-density features in different phases. The radiographic appearance revealed a unicystic view before the patient accepted local curettage of the tumour (Figure 10). Five years after the operation, the tumour presented as an irregular multicyst when it recurrenced (Figure 11). However, the X-ray image showed a high-density mass expanded downward, with the adjacent teeth leaning to the lesion area, 19 years after the first radiological examination (Figure 12).
Figure 10.

Case 20. Right lateral oblique projection showing a single cystic view, 1981
Figure 11.
Case 20. Right lateral oblique projection showing an irregular, honeycombed cyst, 1986
Figure 12.

Case 20. Panoramic radiograph showed a high-density mass expanded downward and the affected teeth leaned toward the lesion area in 2000
In nine cases (45%), the affected teeth roots were resorbed and the lamina dura was usually missing. Four cases (20%) revealed only that the lamina dura of involved teeth was missing or obscure. Six cases (30%) showed displacement of the involved teeth and the lamina dura missing, but no root resorption. The relation between the lesions and the roots of the teeth in the last case (5%) was not clear because of the extraction of the affected teeth.
Only nine cases that were treated surgically had operation reports (Table 4). The treatments included local curettage, local resection of the lesion, excision of jaw bone and reconstructive plate internal fixation, excision of jaw bone and rib graft, and excision of jaw bone and ceramic prosthesis reconstruction. There was follow-up on 11 patients, ranging from half a month to 20 years, and recurrences were found in 3 cases.
Table 4. Operation reports and outcomes.
| Case No. | Operation | Follow-up period | Outcome |
| 1 | Local resection of the lesion | 7 months | No recurrence, pathological fracture |
| 3 | Local curettage | None | |
| 6 | Excision of jaw bone and reconstructive plate internal fixation | 5 months | No recurrence, the implanted bone was OK |
| 8 | Local resection of the lesion | None | |
| 9 | None | 7 years | The lesion became larger and the radiological appearance became more radiopaque |
| 10 | Excision of jaw bone and rib graft | 7 years | No recurrence |
| 11 | Local resection of the lesion | 7 years | Recurred, the lesion become larger, but symptomless |
| 13 | No | 3 years | The lesion became larger and the patient lost the opportunity for an operation |
| 16 | Excision of jaw bone and ceramic prosthesis | 6 months | Recurred, the tumour involved the whole of the mandible |
| 19 | Excision of jaw bone and reconstructive plate internal fixation | 2 weeks | No recurrence |
| 20 | Local curettage | 20 years | Recurred, the radiological appearance became more radiopaque |
Discussion
The term “ossifying fibroma” has been used since 1927, and since 1968 cementum-containing tumours have been grouped together.1 In 1971 the World Health Organization (WHO) classified four types of cementum-containing lesions: fibrous dysplasia, ossifying fibroma, cementifying fibroma and cemento-ossifying fibroma.4 According to the second WHO classification, benign fibro-osseous lesions in the oral and maxillofacial regions were divided into two categories, osteogenic neoplasm and non-neoplastic bone lesions; cementifying ossifying fibroma belonged to the former category.5 However, the term “cementifying ossifying fibroma” was reduced to ossifying fibroma in the new WHO classification in 2005.6
The origin of OF is thought to be the periodontal membrane.7 Some OFs do, in fact, contain prevalent cementum-like calcifications and others show only bony material, but a mixture of the two types of calcification is commonly seen in a single lesion.4, 5 It can occur at any age, however, many authors confirmed that OF of the jaw tended to occur middle-aged patients.2, 7–9 OF of the jaw bone shows a predilection for females.2, 8, 9 In the cases shown in this report, females were also affected more than males. OF predominantly affects the craniofacial bone and rarely involves the long bones. Of the craniofacial bones, the mandible is the most commonly involved site, typically inferior to the premolars and molars.10
Although MacDonald-Jankowski11 considered that radiological diagnoses was not difficult for specialist radiologists, not all radiological diagnoses in the reports were in accordance with the final histological diagnoses. However, for the early cases no CT scanning was available in the hospital and the similar radiological appearance of the tumour in the jaw bone may of confused the diagnosis of the radiologists. Here, in these reports, the radiographic characteristics of the tumour have two basic patterns: cystic lesion (unicystic or multicystic) and mixed-density lesion. The radiographic borders of the tumour appear relatively smooth, well defined and mostly corticated. The contour is regular. The lesion tends to be concentric within the medullary part of the bone with outward expansion approximately equal in all directions. This can result in the expansion of the outer cortical plate of bone. A significant point is that the outer cortical plate, although displaced and thinned, remains intact, especially in those giant tumours. The density of the lesion is mixed. The internal structure may be a mixture of radiolucent and radiopaque tissue. The expansion of the tumour can result in displacement of teeth or the inferior alveolar canal. The lamina dura of involved teeth is usually missing and the affected teeth roots may be resorbed in some cases. Some lesions exhibited aggressive growth. Those massive expansile lesions can involve the whole jaw bone. This pattern lesion often showed medium-density mass with cancellate dense lines in it.
In his review MacDonald-Jankowski,11 reported that the radiology of the OF in contrast to fibrous dysplasia is well defined and round or oval in shape. But, in fact OF may present as irregular in shape, especially if the tumour recurs or grows quickly in a short period. In these cases, the tumours always grow along the body of the jaws, even involving the whole jaw. This phenomenon suggests that OF may display aggressive local growth.
There was a case of giant OF among the current sample, which was approximately 15 cm in diameter. The tumour not only involved the right maxilla, but also affected the hard palate, the right maxillary antrum, the right zygoma and even the inferior floor of the right orbit. Its histological diagnosis was OF, but not juvenile ossifying fibroma (JOF). JOF is another kind of benign lesion, which is similar to OF but more aggressive and of earlier onset. The case suggests that OF, particularly in children (below 15-years-old), could also exhibit rapid growth and erosion or invasion of the adjacent tissue. In this special case, it is unfortunate that the tumour became too large for surgical treatment. Resection of the tumour as early as possible is necessary.
OF requires radical surgery because of the tendency for recurrence and possibility of malignant transformation.8, 12 All reported patients with partial or incomplete resection experienced recurrence.13, 14 The time of recurrence was always unpredictable, ranging from 6 months to 7 years after the operation in our reports. Therefore, there must be a long enough follow-up period of at least 10 years. In the recurrent cases in the study, the tumour often became much larger or the radiographic appearance changed extensively, especially in case 20. There were three different radiological appearances (from unicyst, multicyst to radiopaque mass) during this follow-up period. These appearances demonstrate that this group of lesions could be considered as a spectrum of processes arising from cells in the periodontal ligament.
It is known, most OFs, once completely excised, do not recur. However, although the patient in case 16 accepted a radical resection, the tumour recurred, becoming larger and occupying the whole mandible. It seems that the operation may have stimulated the growth of the tumour. Some authors report that infection and dental extractions stimulate the periodontal membrane to produce and deposit cementum.8 It is possible that trauma could serve as a factor in the proliferation of OF.15–17
Footnotes
Project supported by the National Natural Science Foundation of China (Grant 10675087 and 10574095)
References
- 1.Hamner JE, Scofied HH, Cornyn J. Benign fibro-osseous jaw lesions of periodontal membrane origin. An analysis of 249 cases. Cancer 1968;26:861–878 [DOI] [PubMed] [Google Scholar]
- 2.Waldron CA, Giansanti JS. Benign fibro-osseous lesions of the jaw: a clinical-radiologic review of sixty-five cases. Oral Surg Oral Med Oral Pathol 1973;35:340–350 [DOI] [PubMed] [Google Scholar]
- 3.Eversole LR, Merrell PW, Strub D. Radiographic characteristics of central ossifying fibroma. Oral Surg Oral Med Oral Pathol 1985;59:522–527 [DOI] [PubMed] [Google Scholar]
- 4.Pindborg JJ, Kramer IRH. Histological typing of odontogenic tumors, jaw cysts and allied lesions. In: International histological classification of tumors. Geneva: WHO, 1971, pp 31–34 [Google Scholar]
- 5.Kramer IRH, Pindborg JJ, Shear M. Neoplasm and other lesions related to bone. Histologic typing of odontogenic tumors, World Health Organization. Berlin, Springer-Verlag 1992: 28–31. [Google Scholar]
- 6.Reichart PA, Philipsen HP, Sciubba JJ. The new classification of Head and Neck Tumours (WHO) – any changes? Oral Oncol 2006;42:757–758 [DOI] [PubMed] [Google Scholar]
- 7.Krausen AS, Pullon PA, Gulmen S, Schenk NL, Ogura JH. Cementomas–aggressive or innocuous neoplasm? Arch Otolaryngol 1977;103:349–354 [DOI] [PubMed] [Google Scholar]
- 8.Hammer JE, Linghtbody PM, Ketcham AS, Swertlow H. Cemento-ossifying fibroma of the maxilla. Oral Surg Oral Med Oral Pathol 1968;26:576–587 [DOI] [PubMed] [Google Scholar]
- 9.Longdon JD, Rapidis AD, Patel MF. Ossifying fibro-osseous lesions of the jaw. Br J Oral Surg 1976;14:1–11 [DOI] [PubMed] [Google Scholar]
- 10.Eversole LR, Leider AS, Patel MF. Ossifying fibroma: a clinicopathologic study of sixty-four cases. Oral Surg Oral Med Oral Pathol 1985;60:505–511 [DOI] [PubMed] [Google Scholar]
- 11.MacDonald-Jankowski DS. Fibro-osseous lesions of the face and jaws. Clin Radiol 2004;59:11–25 [DOI] [PubMed] [Google Scholar]
- 12.Bertrand B, Eloy P, Cornelis JP, Gosseye S, Clotuche J, Gilliard C. Juvenile aggressive cemento-ossifying fibroma: case report and review of the literature. Laryngoscope 1993;103:1385–1390 [DOI] [PubMed] [Google Scholar]
- 13.Margo CE, Ragsdate BD, Perman KI, Zinnerman LE, Sweet DE. Psammomatoid (juvenile) ossifying fibroma of the orbit. Ophthalmology 1985;92:150–159 [DOI] [PubMed] [Google Scholar]
- 14.Margo CE, Weiss A, Habal MB. Psammomatoid ossifying fibroma. Arch Ophthalmol 1986;104:1347–1351 [DOI] [PubMed] [Google Scholar]
- 15.Wenig BL, Sciubba JJ, Cohen A, Goldstein MN, Abramson AL. A destructive maxillary cemento-ossifying fibroma following maxillofacial trauma. Laryngoscope 1984;94:810–815 [DOI] [PubMed] [Google Scholar]
- 16.Brademann G, Werner JA, Jänig U, Mehdorn HM, Rudert H. Cemento-ossifying fibroma of the petromastoid region: case report and review of the literature. J Laryngol Otol 1997;111:152–155 [DOI] [PubMed] [Google Scholar]
- 17.Cheng C, Takahashi H, Yao K, Nakayama M, Makoshi T, Nagai H, et al. Cemento-ossifying fibroma of maxillary and sphenoid sinuses: case report and literature review. Acta Otolaryngol 2002;547(Suppl):118–122 [DOI] [PubMed] [Google Scholar]


