Abstract
Objective
The objective of this study was to investigate the frequency and pattern of bifid mandibular condyles (BMCs).
Methods
A retrospective study was performed using panoramic radiographs from 10 200 patients undergoing dental treatment in the Department of Oral and Maxillofacial Radiology (Erzurum, Turkey) between 1996 and 2008.
Results
Of the 10 200 patients, 32 (0.3%) had BMCs, of whom 17 were female (53.1%) and 15 were male (46.9%). The age range of the patients with BMCs was 5 to 71 years (mean age 30.0±0.40). Of these 32 patients, 24 (75.0%) had unilateral and 8 (25.0%) had bilateral BMCs, none of the patients had a history of trauma. No symptoms associated with bifid condyles were observed in any of the patients with BMCs.
Conclusions
It is possible that BMC is a more frequent condition than is commonly perceived. However, because of the minimal symptoms associated with this condition, the authors believe that it will remain an incidental finding upon routine radiographic examination, rather than a clinical observation. Nevertheless, in symptomatic cases or in cases where surgical treatment is planned, panoramic radiographs should be supplemented with CT.
Keywords: panoramic radiography, bifid condyle, duplication of condylar head, double-headed condyle
Introduction
Bifid mandibular condyle (BMC) is a rare condition characterized by a division of the mandibular condylar head. Two articulating surfaces of the bifid condyle are divided by a groove that can be oriented mediolaterally or anteroposteriorly. The condylar split can range from a shallow groove to two distinct condyles with a separate neck. Reported cases in living people and in preserved specimens are mostly unilateral and, usually, asymptomatic.1–5
When reviewing the literature regarding BMC using the PubMed Database (National Library of Medicine), the authors found that it listed only 65 cases in living people1–40 (Table 1). Although the number of reports continues to accumulate, BMC remains a relatively uncommon condition. However, because of the lack of epidemiological data, there is insufficient information about the true frequency of this malformation. It may be the case that the condition occurs more frequently than is presently supposed. Therefore, to assess the frequency of this phenomenon, a retrospective study was carried out using panoramic radiographs from 10 200 patients.
Table 1. Literature review of the bifid condyle in living subjects.
| Reported cases | Gender | Age | Side |
| Schier, 19481 | NA | NA | NA |
| Stadnicki, 19712 | F | 3 | L |
| Lysell and Oberg, 19753 | F | 21 | R |
| Farmand, 19814 | M | 45 | L |
| Forman and Smith, 19845 | M | 28 | L |
| M | 30 | L | |
| Smith, 19856 | F | 32 | L |
| Balciunas, 19867 | F | 67 | L |
| Thomason and Yusuf, 19868 | F | 5 | R |
| F | 6 | R | |
| Quayle and Adams, 19869 | F | 15 | R |
| Shaber, 198710 | F | 26 | L&R |
| Gundlach et al, 198711 | M | 23 | L |
| NA | NA | L | |
| NA | NA | L | |
| NA | NA | R | |
| Zohar and Laurian, 198712 | NA | NA | NA |
| Sahm and Witt, 198913 | NA | NA | NA |
| McCormick et al, 198914 | M | 38 | L&R |
| F | 61 | L&R | |
| M | 50 | L&R | |
| To, 198915 | M | 34 | R |
| To, 198916 | M | 53 | L |
| Loh and Yeo, 199017 | M | 24 | L |
| M | 21 | R | |
| F | 27 | R | |
| M | 59 | L | |
| M | 59 | L | |
| Philips and Delzer, 199218 | NA | NA | NA |
| Antoniades et al, 199319 | NA | NA | NA |
| Fields and Frederiksen, 199320 | NA | NA | NA |
| Wu et al, 199421 | M | 21 | L |
| M | 23 | R | |
| Kahl et al, 199522 | F | 14 | R |
| Cowan and Ferguson, 199723 | F | 24 | L |
| Stefanou et al, 199824 | F | 55 | L&R |
| M | 47 | L&R | |
| F | 39 | L&R | |
| F | 69 | L&R | |
| Garcia-Gonzalez et al, 200025 | M | 63 | L |
| Artvinli and Kansu, 200326 | F | 25 | L&R |
| Antoniades et al, 200427 | M | 15 | L&R |
| de Sales et al, 200428 | M | 4 | R |
| Hersek et al, 200429 | F | 36 | L |
| Alpaslan et al, 200430 | M | 40 | L&R |
| Shriki et al, 200531 | F | 48 | R |
| F | 17 | L&R | |
| Daniels and Ali, 200532 | M | 32 | R |
| Corchero-Martin et al, 200533 | F | 42 | R |
| Ramos et al, 200634 | F | 20 | L |
| Espinosa-Femenia, 200635 | M | 29 | L&R |
| Agarwal et al, 200636 | F | 57 | L&R |
| F | 46 | R | |
| Acikgoz, 200637 | F | 54 | L&R |
| Tunçbilek et al, 200638 | M | 8 | L |
| Sales et al, 200739 | F | 8 | L |
| Menezes et al, 200840 | F | 28 | L |
| M | 30 | L | |
| F | 74 | L&R | |
| F | 20 | L | |
| M | 43 | L&R | |
| F | 53 | R | |
| F | 72 | L | |
| F | 52 | R | |
| F | 29 | R |
F, female; L, left; M, male; R, right
Patients and methods
A retrospective cohort study was designed consisting of 10 200 panoramic radiographs from patients who presented to the Oral and Maxillofacial Radiology Service at the Ataturk University Dentistry Faculty between January 1996 and January 2008. All radiographs had been taken using an orthopantomography device (Planmeca Proline CC 2002, 60–80 kVp, 8–10 mA, 12.8 s exposure time, Helsinki, Finland) by a radiographic technician who had a minimum of 5 years experience, as of 1996. Radiographs were taken using 15 cm green-sensitive panoramic film (Medical, Konica Co., Tokyo, Japan) and an appropriate cassette-intensifying screen (15 × 30 cm, Panoramic X-Ray Film Cassette, Planmeca, Helsinki, Finland; Lanex Screen, Kodak Eastman Co., Rochester NY).
During filming, exposure adjustments were made as required for each individual and the films were developed using an automatic film-processing machine (Velopex, Extra-X, London, UK).
Researchers examined the radiographs at the same time, using standard light boxes. For those patients in whom bifid condyles were suspected, but could not be conclusively ascertained from the panoramic radiographs, and with whom contact was possible, a supplementary transcranial radiograph was taken to confirm the diagnosis. However, when examiners failed to reach a decisive opinion, the examiners discussed the particular case and either established a consensus and included it in the study, or discarded the case (n _ 2). Observations were made as to the right/left localization, symptom, aetiology and number of BMCs, as well as gender and age of patients.
Results
32 (0.3%) of 10 200 individuals had BMCs, of whom 17 (53.1%) were female and 15 (46.9%) were male. The ages of the patients ranged from 5 to 71 years (mean age 30.0±0.40). 24 cases (75.0%) were unilateral and 8 (25.0%) cases were bilateral (Figure 1). Of the 24 unilateral cases, 10 (41.7%) were on the left and 14 (58.3%) were on the right side (Figure 2). None of these patients had a history of trauma. In two of the patients, symptoms associated with temporomandibular joint (TMJ) pain dysfunction syndrome were reported; nevertheless, this pain could not be clearly related to the BMC. One patient had periodic pain in the TMJ region associated with bruxism. The patient, who was treated with interocclusal appliance therapy, was followed up. Another patient who had a clicking sound associated with subluxation was prescribed exercise therapy and followed up (Table 2). Figure 3 shows a lateral transcranio-oblique film obtained from a patient who was suspected of having BMC from panoramic radiography.
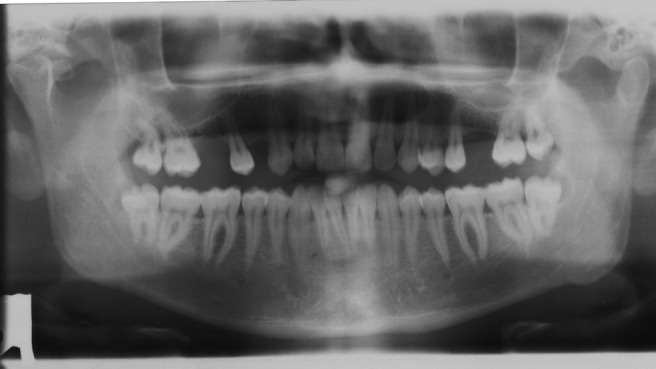
Figure 1.

Bilateral duplication of the condylar head (patient 7)
Figure 2.
View of a right bifid condyle that is divided into two parts of more or less equal size by a deep groove (patient 11)
Table 2. Bifid condyle in a Turkish patient population.
| Patient number | Gender | Age (years) | Bifid condyle, double-headed condyle and duplication of the condylar head | Aetiological factors or symptom |
| 1 | M | 19 | L&R | No |
| 2 | M | 42 | L&R | No |
| 3 | F | 30 | R | No |
| 4 | F | 8 | R | No |
| 5 | M | 5 | R | No |
| 6 | M | 71 | R | No |
| 7 | F | 22 | L&R | No |
| 8 | F | 52 | R | No |
| 9 | F | 24 | R | No |
| 10 | M | 22 | L | No |
| 11 | M | 26 | R | No |
| 12 | F | 40 | L | No |
| 13 | F | 19 | R | No |
| 14 | M | 25 | L | No |
| 15 | M | 21 | L | No |
| 16 | F | 60 | L | No |
| 17 | F | 23 | L | No |
| 18 | F | 23 | L | No |
| 19 | F | 23 | R | Clicking |
| 20 | F | 21 | L&R | No |
| 21 | M | 45 | L | No |
| 22 | M | 13 | L&R | No |
| 23 | F | 28 | R | No |
| 24 | M | 45 | L | No |
| 25 | F | 21 | L&R | Periodic pain |
| 26 | M | 43 | R | No |
| 27 | M | 30 | L&R | No |
| 28 | M | 26 | R | No |
| 29 | M | 32 | R | No |
| 30 | F | 18 | L&R | No |
| 31 | F | 30 | R | No |
| 32 | F | 20 | L | No |
F, female; M, male; L, left; R, right
Figure 3.
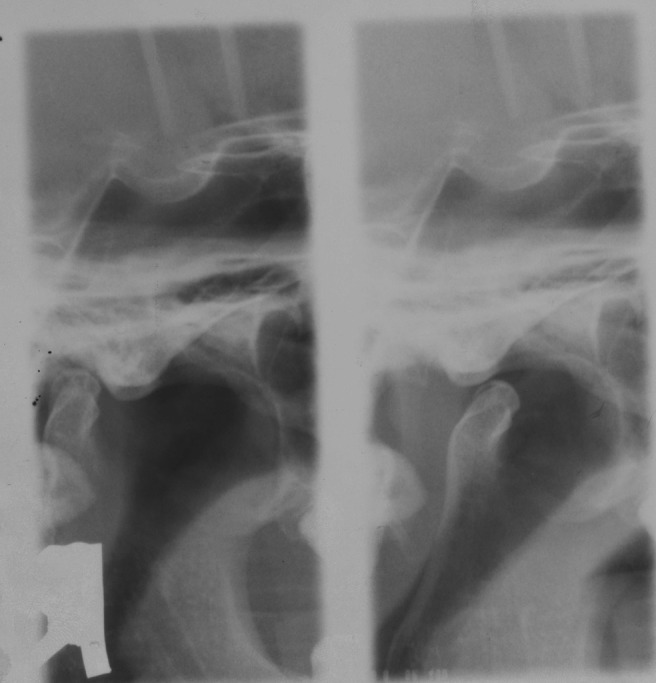
View of the right bifid condyle in a transcranio-oblique projection (patient 28)
Discussion
A review of the literature supports the conclusion that bifid condyle is usually discovered as an incidental finding on panoramic radiographs. Thus, a sudden increase from the number of cases reported can be attributed to the current widespread use of radiographs. Hrdlicka,41 in 1941, first reported this anomaly in 21 specimens from an unspecified number of dried skulls in the Smithsonian Institution Washington, DC. A subsequent survey by Szentpétery et al42 of 1882 prehistoric skulls with 2077 condyles found only 7 (0.3%) cases of bifid condyles. However, in both studies, precise determination of the frequency of the anomaly was not possible. To the authors knowledge, only five cases have been reported in Turkey.26, 29, 30, 37, 38 This retrospective study presents 32 previously unreported cases examined between 1996 and 2008. Menezes et al40 examined 50 080 panoramic radiographs between 1999 and 2006 and reported only 9 bifid condyle cases. This high frequency suggests that BMC is a more frequent condition than is presently perceived.
The aetiology of bifid condyle is largely unknown, although various factors have been suggested as possible causes: endocrine disturbances, exposure to teratogens, nutritional deficiencies and, infection and radiation.9 It is claimed that the condyle divides because of an obstructed blood supply during its development.41 Blackwood43 stated that the condylar cartilage, during the early stages of development, is divided by well-vascularized fibrous septa. He suggested that persistence of this type of septum in exaggerated form within the growing cartilage might lead to an error in development that would, in turn, give rise to the bifid condition. However, Gundlach and colleagues11 found no evidence of persistent septa in the cases of BMC that they examined. They believed that the bifid condyle is a form of embryopathy caused by a combination of a teratogenic agent and misdirection of muscle fibres, which then influences bone formation. MacAlister44 reported that there were observed downgrowths covering the histological section of an 18-week-old intrauterine fetal specimen.
Thomason and Yusuf8 described two cases of traumatic condyle fracture (bicycle accident) with subsequent unilateral formation of bifid condyles. This seems to confirm the conclusion of Walker45 and Poswillo,46 after experiments with Macaca monkeys, that bifid condyle can result from trauma.
The reported existence of two different patterns of condyle bifidism might be related to distinct causes for each type. Thus, the anteroposterior pattern might result from facial trauma during childhood, whereas the mediolateral form might be associated with persistence of the fibrous septa at the condylar cartilage.42 All of the cases investigated in the current study support this condition. However, some mediolateral bifid condyles have been reported following sagittal fracture through the condylar head.17, 21
A current literature review in living patients revealed a total of 65 cases (for 6 cases, information was insufficient). 17 cases were bilateral and 42 were unilateral: 24 on the left and 18 on the right side (left–right, 1.3:1). However, if dry skulls41, 42 and cadavers17 are included, the ratio of unilateral–bilateral cases rises to 4.6:1. In the current study, a ratio of 3.0:1 was observed, which is close to those reported in the literature. However, the left–right ratio here has been determined to be 0.7:1 on average, which is different from the ratios reported in the literature.
The occurrence of BMC does not appear to demonstrate age or gender differences, as the age of the patients ranged from 3 to 74 years. In addition, most of the reported patients, of known age, are over 20 years old.17 In this study, the sample consisted mostly of patients over 20 years (5–71 years, mean age 30.0±0.40), which is again consistent with the literature.
A review of current reports in the literature reveals an average female–male ratio of 1.3:1. Antoniades et al27 found a male–female ratio of approximately 1.5:1. Menezes et al40 found a higher BMC prevalence in women than in men. The ratio of female–male patients examined in the present study was found to be very similar (17/15).
Treatment of BMC depends on the presenting complaints of the patient. However, symptoms are not observed in the affected condyle in 67% of patients with BMC.17 Other than these asymptomatic cases, the most common and predominant symptoms are TMJ sounds.14, 17 Pain, restriction of mandibular movement, trismus, swelling, ankylosis and facial asymmetries have also been described.4, 5, 9 Bilateral condylectomy and arthroplasty have been reported to restore function in a case of ankylosis accompanied by bifid condyle.16 In the current study, two patients had complained of TMJ pain dysfunction; however, the examinations revealed that this was not associated with BMC.
Two patients were not included in the study because, they were suspected of having bifid condyles although, these could not be clearly diagnosed. Although panoramic radiography is a valid diagnostic tool for determination of BMC, it is also known to have certain disadvantages, including its inherent distortions and limitations. In contrast, CT is undoubtedly the best choice for TMJ examination because it allows bilateral visualization without osseous superpositioning. In particular, helical CT, which is based on the acquisition of multiple continuous slices of the anatomical site of interest, has several advantages, such as complete recording of the area with a single scan, short examination times, lower radiation dose and better image quality.11, 17, 19 The majority of BMC cases do not cause any TMJ dysfunction and require no treatment. However, in BMC cases with joint dysfunction or in which treatment is planned, panoramic radiography should be supplemented by CT.
In conclusion, our results suggest that the prevalence of BMC is likely to be higher than has been previously believed. There has been a marked increase in the number of reported BMC cases, in parallel with the development of new diagnostic techniques that allow earlier and easier diagnosis of the pathologies in the maxillofacial region. Nevertheless, diagnosis of this anomaly has become incidental, because it does not present any clinical symptoms and dentists are more interested in dental pathologies in the examination of radiographs.
References
- 1.Schier MB. The temporomandibular joint. A consideration of its probable functional and dysfunctional sequelae and report: condyle double head in a living person. Dent Item Interest 1948;70:889. [PubMed] [Google Scholar]
- 2.Stadnicki G. Congenital double condyle of the mandible causing temporomandibular joint ankylosis: report of case. J Oral Surg 1971;29:208–211 [PubMed] [Google Scholar]
- 3.Lysell L, Oberg T. Unilateral doubling of mandibular condyle. Dentomaxillofac Radiol 1975;4:95–98 [DOI] [PubMed] [Google Scholar]
- 4.Farmand M. Mandibular condylar head duplication. A case report. J Maxillofac Surg 1981;9:59–60 [DOI] [PubMed] [Google Scholar]
- 5.Forman GH, Smith NJ. Bifid mandibular condyle. Oral Surg Oral Med Oral Pathol 1984;57:371–373 [DOI] [PubMed] [Google Scholar]
- 6.Smith AC. Duplication of the condyle. Oral Surg Oral Med Oral Pathol 1985;60:456. [DOI] [PubMed] [Google Scholar]
- 7.Balciunas BA. Bifid mandibular condyle. J Oral Maxillofac Surg 1986;44:324–325 [DOI] [PubMed] [Google Scholar]
- 8.Thomason JM, Yusuf H. Traumatically induced bifid mandibular condyle: report of two cases. Br Dent J 1986;161:291–293 [DOI] [PubMed] [Google Scholar]
- 9.Quayle AA, Adams JE. Supplemental mandibular condyle. Br J Oral Maxillofac Surg 1986;24:349–356 [DOI] [PubMed] [Google Scholar]
- 10.Shaber EP. Bilateral bifid mandibular condyles. Cranio 1987;5:191–195 [DOI] [PubMed] [Google Scholar]
- 11.Gundlach KK, Fuhrmann A, Beckmann-Van derVen G. The double-headed mandibular condyle. Oral Surg Oral Med Oral Pathol 1987;64:249–253 [DOI] [PubMed] [Google Scholar]
- 12.Zohar Y, Laurian N. Bifid condyle of the mandible associated with polythelia and manual anomalies. J Laryngol Otol 1987;101:1315–1319 [DOI] [PubMed] [Google Scholar]
- 13.Sahm G, Witt E. Long-term results after childhood condylar fractures. A computer tomographic study. Eur J Orthod 1989;11:154–160 [DOI] [PubMed] [Google Scholar]
- 14.McCormick SU, McCormick SA, Graves RW, Pifer RG. Bilateral bifid mandibular condyles. Report of three cases. Oral Surg Oral Med Oral Pathol 1989;68:555–557 [DOI] [PubMed] [Google Scholar]
- 15.To EW. Supero-lateral dislocation of sagittaly split bifid mandibular condyle. Br J Oral Maxillofac Surg 1989;27:107–113 [DOI] [PubMed] [Google Scholar]
- 16.To EW. Mandibular ankylosis associated with a bifid condyle. J Craniomaxillofac Surg 1989;17:326–328 [DOI] [PubMed] [Google Scholar]
- 17.Loh FC, Yeo JF. Bifid mandibular condyle. Oral Surg Oral Med Oral Pathol 1990;69:24–27 [DOI] [PubMed] [Google Scholar]
- 18.Philips JD, Delzer DD. Unilateral bifid mandibular condyle. Gen Dent 1992;40:425. [PubMed] [Google Scholar]
- 19.Antoniades K, Karakasis D, Elephteriades J. Bifid mandibular condyle resulting from a sagittal fracture of the condylar head. Br J Oral Maxillofac Surg 1993;31:24–26 [DOI] [PubMed] [Google Scholar]
- 20.Fields R, Frederiksen NL. Facial trauma confusing the diagnosis of a bifid condyle. Dentomaxillofac Radiol 1993;22:216–217 [DOI] [PubMed] [Google Scholar]
- 21.Wu XG, Hong M, Sun KH. Severe osteoarthrosis after fracture of the mandibular condyle: a clinical and histologic study of seven patients. J Oral Maxillofac Surg 1994;52:138–142 [DOI] [PubMed] [Google Scholar]
- 22.Kahl B, Fischbach R, Gerlach KL. Temporomandibular joint morphology in children after treatment of condylar fractures with functional appliance therapy: a follow-up study using computed tomography. Dentomaxillofac Radiol 1995;24:37–45 [DOI] [PubMed] [Google Scholar]
- 23.Cowan DF, Ferguson MM. Bifid mandibular condyle. Dentomaxillofac Radiol 1997;26:70–73 [DOI] [PubMed] [Google Scholar]
- 24.Stefanou EP, Fanourakis IG, Vlastos K, Katerelou J. Bilateral bifid mandibular condyles. Report of four cases. Dentomaxillofac Radiol 1998;27:186–188 [DOI] [PubMed] [Google Scholar]
- 25.García-González D, Martín-Granizo R, López P. Imaging quiz case 4. Bifid mandibular condyle. Arch Otolaryngol Head Neck Surg 2000;126:798–799 [PubMed] [Google Scholar]
- 26.Artvinli LB, Kansu O. Trifid mandibular condyle: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:251–254 [DOI] [PubMed] [Google Scholar]
- 27.Antoniades K, Hadjipetrou L, Antoniades V, Paraskevopoulos K. Bilateral bifid mandibular condyle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;97:535–538 [DOI] [PubMed] [Google Scholar]
- 28.de Sales MA, Amaral JI, Amorim RF, Almeida Freitas R. Bifid mandibular condyle: case report and etiological considerations. J Can Dent Assoc 2004;70:158–162 [PubMed] [Google Scholar]
- 29.Hersek N, Özbek M, Tasar F, Akpinar E, Firat M. Bifid mandibular condyle: a case report. Dent Traumatol 2004;20:184–186 [DOI] [PubMed] [Google Scholar]
- 30.Alpaslan S, Özbek M, Hersek N, Kanli A, Avcu N, Fırat M. Bilateral bifid mandibular condyle. Dentomaxillofac Radiol 2004;33:274–277 [DOI] [PubMed] [Google Scholar]
- 31.Shriki J, Lev R, Wong BF, Sundine MJ, Hasso AN. Bifid mandibular condyle: CT and MR imaging appearance in two patients: case report and review of the literature. AJNR Am J Neuroradiol 2005;26:1865–1868 [PMC free article] [PubMed] [Google Scholar]
- 32.Daniels JSM, Ali I. Post traumatic bifid condyle associated with temporomandibular joint ankylosis: report of a case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:682–688 [DOI] [PubMed] [Google Scholar]
- 33.Corchero-Martin G, Gonzalez-Teran T, Garcia-Reija MF, Sanchez-Santolino S, Saiz-Bustillo R. Bifid condyle: case report. Med Oral Patol Oral Cir Bucal 2005;10:277–279 [PubMed] [Google Scholar]
- 34.Ramos FM, Filho JO, Manzi FR, Boscolo FN, Almeida SM. Bifid mandibular condyle: a case report. J Oral Sci 2006;48:35–37 [DOI] [PubMed] [Google Scholar]
- 35.Espinosa-Femenia M, Sartorres-Nieto M, Berini-Aytes L, Gay-Escoda C. Bilateral bifid mandibular condyle: case report and literature review. Cranio 2006;24:137–140 [DOI] [PubMed] [Google Scholar]
- 36.Agarwal V, Suhas S, Pai KM, Shetty CM, Auluck A. Bifid mandibular condyles: report of four cases. Dent Update 2006;33:368–370 [DOI] [PubMed] [Google Scholar]
- 37.Acikgoz A. Bilateral bifid mandibular condyle: a case report. J Oral Rehabil 2006;33:784–787 [DOI] [PubMed] [Google Scholar]
- 38.Tunçbilek G, Cavdar G, Mavili ME. Bifid mandibular condyle: a rare disorder. J Craniofac Surg 2006;17:1207–1209 [DOI] [PubMed] [Google Scholar]
- 39.Sales MA, Oliveira JX, Cavalcanti MG. Computed tomography imaging findings of simultaneous bifid mandibular condyle and temporomandibular joint ankylosis: case report. Braz Dent J 2007;18:74–77 [DOI] [PubMed] [Google Scholar]
- 40.Menezes AV, de MoraesRamos FM, de Vasconcelos-Filho JO, Kurita LM, de Almeida SM, Haiter-Neto F. The prevalence of bifid mandibular condyle detected in a Brazilian population. Dentomaxillofac Radiol 2008;37:220–223 [DOI] [PubMed] [Google Scholar]
- 41.Hrdlicka A. Lower jaw: double condyles. Am J Phys Anthropol 1941;28:75–89 [Google Scholar]
- 42.Szentpétery A, Kocsis G, Marcsik A. The problem of the bifid mandibular condyle. J Oral Maxillofac Surg 1990;48:1254–1257 [DOI] [PubMed] [Google Scholar]
- 43.Blackwood HJ. The double-headed mandibular condyle. Am J Phys Anthropol 1957;15:1–8 [DOI] [PubMed] [Google Scholar]
- 44.MacAlister AD. The development of the human temporomandibular joint: a microscopic study. Aust J Dent 1955;59:21–27 [Google Scholar]
- 45.Walker RV. Traumatic mandibular condylar fracture dislocations. Effect on growth in the Macaca rhesus monkey. Am J Surg 1960;100:850–863 [DOI] [PubMed] [Google Scholar]
- 46.Poswillo DE. The late effects of mandibular condylectomy. Oral Surg Oral Med Oral Pathol 1972;33:500–512 [DOI] [PubMed] [Google Scholar]


