Abstract
Objective
To investigate the impact on ICD coding behaviour of a new case-mix reimbursement system based on coded patient diagnoses. The main hypothesis was that after the introduction of the new system the coding of chronic diseases like hypertension and cancer would increase and the variance in propensity for coding would decrease on both physician and health care centre (HCC) levels.
Design
Cross-sectional multilevel logistic regression analyses were performed in periods covering the time before and after the introduction of the new reimbursement system.
Setting
Skaraborg primary care, Sweden.
Subjects
All patients (n = 76 546 to 79 826) 50 years of age and older visiting 468 to 627 physicians at the 22 public HCCs in five consecutive time periods of one year each.
Main outcome measures
Registered codes for hypertension and cancer diseases in Skaraborg primary care database (SPCD).
Results
After the introduction of the new reimbursement system the adjusted prevalence of hypertension and cancer in SPCD increased from 17.4% to 32.2% and from 0.79% to 2.32%, respectively, probably partly due to an increased diagnosis coding of indirect patient contacts. The total variance in the propensity for coding declined simultaneously at the physician level for both diagnosis groups.
Conclusions
Changes in the healthcare reimbursement system may directly influence the contents of a research database that retrieves data from clinical practice. This should be taken into account when using such a database for research purposes, and the data should be validated for each diagnosis.
Key Words: Electronic health records, general practice, ICD codes, incentive, multilevel analysis, primary health care, reimbursement, Sweden
Introducing a new reimbursement system based on patient diagnoses at all consultations:
increased registration of diagnoses of chronic diseases like hypertension and cancer;
decreased the variation in diagnosis coding between physicians;
seemed to be a powerful intervention for increasing the recording of diagnosis codes.
Background
During the last decade, primary care in Sweden has been subject to considerable financial changes. In 2003 a decentralized drug budget was implemented in Skaraborg. In a previous study [1] we demonstrated that this change in economic prerequisites was associated with an increased adherence to prescribing recommendations.
In October 2009 the county authorities introduced the “Västra Götaland Primary Care” (VGPV) [2], involving a reform of the reimbursement system. In the new system resources are allocated according to a capitation formula based on the patient's age, gender, and a case-mix index inspired by the Johns Hopkins University Adjusted Clinical Groups (ACG) system [3]. This index is based on patient diagnoses coded according to the International Classification of Diseases (ICD). Codes for chronic diseases render higher reimbursement than codes for minor problems. Previous studies have shown that the method of payment affects the clinical practice behaviour of physicians [4]. The personal remuneration to the physician is not directly affected by the VGPV system. However, the general budget of the health care centres (HCCs) does depend on recorded ICD codes, and a decrease in the budget may lead to staff cuts. Consequently, the introduction of the VGPV system has introduced a strong economic incitement for coding, especially for chronic diseases.
Using the Skaraborg Primary Care Database (SPCD) [5] and multilevel regression analyses we investigated the impact of the new VGPV system on ICD coding behaviour. Our main hypothesis was that after the introduction of the new system the prevalence of coded chronic diseases like hypertension and cancer would increase in the SPCD. Furthermore, as all HCCs and physicians shared the same new incentives the variance in propensity for coding would be expected to decrease on both HCC and physician levels. We also investigated the levels of ICD code registration in the SPCD, a database that was previously used for research in primary health care [5–8].
Material and methods
Skaraborg is situated in the south-west of Sweden and populated by 250 000 inhabitants. Since 1998 it has administratively been part of the Västra Götaland Region with 1.6 million inhabitants. Before the new VGPV system, primary care in Skaraborg was supplied by 24 public HCCs and a few private general practitioners and after VGPV by 22 public and 11 private HCCs. Since 2000, all public HCCs in Skaraborg have shared the same computerized medical record system (Profdoc Journal III 1.82), allowing the construction of the SPCD containing information extracted from these records [5].
Population
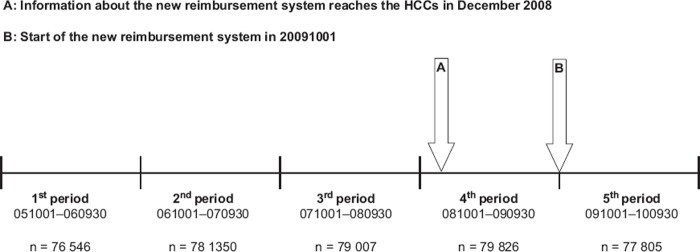
Datasets from five consecutive one-year time periods were extracted from the SPCD. The datasets contained all patients 50 years of age or older who had visited any of the 22 public HCCs. The first three periods represent the baseline (Figure 1). During the fourth period the forthcoming change in the reimbursement system became known (see Figure 1, A) but it was not officially introduced until the start of the last period, 1 October 2009 (see Figure 1, B).
Figure 1.
Relationship between the five consecutive data periods and the change in reimbursement system with numbers of patients included in each analysis. The first three periods represent the baseline, and were defined as 1 October 2005–30 September 2006 (1st period), 1 October 2006–30 September 2007 (2nd period) and 1 October 2007–30 September 2008 (3rd period). During the 4th period from 1 October 2008 the forthcoming change in reimbursement system became known but was not officially introduced until the start of the 5th period on 1 October 2009.
Assessment of variables
All diagnoses are coded using the Swedish primary care version of ICD-10 [9]. We chose to study hypertension (ICD I10-, I13-P, I15-) since it is a well-defined chronic disease, and cancer (C00-C96-P) since it represents a group of diagnoses with low registration rates in primary care. The outcome was a dichotomous variable indicating whether a patient had a hypertension or cancer code registration in the diagnosis register or not, during each time period. Patients’ sex (with women as reference) and age (centred at the mean of 68 years) were also included. For each patient and time period we identified the physician with the majority of patient contacts. Contacts were defined as direct (visits) or indirect (telephone consultations, prescription renewals, or administrative journal recordings). For comparison, the total number of registered tonsillitis (J03-) diagnoses was also determined in order to estimate potential changes in the registration of an acute diagnosis with low reimbursement value.
Multilevel logistic regression analysis
Because of the hierarchical structure of the data we performed multilevel logistic regression analysis (MLA) [10,11] with patients nested within physicians who in turn were nested within HCCs. Like any regression analysis, MLA produces regression coefficients. However, because MLA also recognizes to which level the included variables belong, the total variance is partitioned to the relevant level. Thus, the relative importance of each level for ICD coding [12] could be quantified.
For cancer and hypertension diagnoses separate analyses were performed for each time period in order to observe changes in prevalence and variance over time. To study associations in the fixed effects part of the MLA we calculated prevalences and ORs (odds ratios) and their 95% credible intervals (95% CIs).
In the random part of the model we used the variances to calculate the intra-class correlation (ICC) [11,13]. The ICC estimates the proportion of the total variance that can be attributed to a specific level. We calculated ICC as follows:
ICCPHY = (VARHCC+VARPHY)/(VARHCC+VARPHY+ VARP)
ICCHCC = (VARHCC)/(VARHCC+VARPHY+ VARP)
Where
VARPHY = Physician level variance
VARHCC = HCC level variance
VARP = Patient level variance
ICCPHY = Physician level ICC
ICCHCC = HCC level ICC
In the hypertension datasets the variances were calculated with the logit Link where the VARP = 3.29. However, because of the low prevalence in the Cancer datasets we used the probit link to calculate the variances, and the VARP = 1 [11].
Parameters were estimated using the MLwiN software [14].
Results
Descriptive analysis
The numbers of patients in each dataset from the five time periods were similar (between 76 546 and 79 826) with an overall mean age of 68 years (Table I). When comparing the mean of the first three time periods with the last time period, the prevalence of hypertension in SPCD increased from 17% to 33%, equally distributed between sexes. Prevalence of cancer diagnoses increased from 1.5% to 3.9% but with higher rates for men. Simultaneous rises in the total number of registered diagnoses (183 052 to 327 781) and in the proportion of coded indirect (13% to 24%) and direct contacts (81% to 93%) were also shown. The number of registered tonsillitis diagnoses remained approximately the same in all five time periods (data not shown).
Table I.
Characteristics of patients 50 years of age and older with hypertension and/or cancer diagnoses, contacts and HCCs in the Skaraborg Primary Care Database (SPCD) for the different time periods.1
| Time period | 051001–060930 | 061001–070930 | 071001–080930 | 081001–090930 | 091001–100930 |
|---|---|---|---|---|---|
| Characteristics of the 22 HCCs: | |||||
| Patients (n) | 76 546 | 78 350 | 79 007 | 79 826 | 77 805 |
| Median | 3186 | 3456 | 3535 | 3470 | 3310 |
| Range | 1226–7699 | 1241–7687 | 1207–7789 | 1242–7962 | 1276–7319 |
| Physicians (n) | 554 | 489 | 589 | 627 | 468 |
| Median | 19 | 17 | 23 | 23 | 20 |
| Range | 3–77 | 4–71 | 5–87 | 5–81 | 8–42 |
| Characteristics of patients: | |||||
| Age (years) | |||||
| Mean | 68.0 | 68.0 | 68.1 | 68.1 | 68.3 |
| Range | 50–106 | 50–107 | 50–108 | 50–108 | 50–109 |
| Sex | |||||
| Female | 42 266 (55%) | 43 181 (55%) | 43 327 (55%) | 43 632 (55%) | 42 436 (55%) |
| Male | 34 264 (45%) | 35 156 (45%) | 35 664 (45%) | 36 182 (45%) | 35 355 (45%) |
| Hypertension | 12 752 (17%) | 12 876 (16%) | 14 290 (18%) | 20 387 (26%) | 25 478 (33%) |
| Age (years) | |||||
| Mean | 70.6 | 70.6 | 70.8 | 71.1 | 71.6 |
| Range | 50–102 | 50–99 | 50–101 | 50–102 | 50–104 |
| Sex | |||||
| Female | 7256 (17%) | 7293 (17%) | 7975 (18%) | 11 318 (26%) | 13 975 (33%) |
| Male | 5496 (16%) | 5583 (16%) | 6313 (18%) | 9067 (25%) | 11 502 (33%) |
| Cancer | 1082 (1.4%) | 1007 (1.3%) | 1203 (1.5%) | 2030 (2.5%) | 3061 (3.9%) |
| Age (years) | |||||
| Mean | 74.8 | 74.9 | 75.5 | 75.6 | 75.5 |
| Range | 50–100 | 50–101 | 50–101 | 50–103 | 50–101 |
| Sex | |||||
| Female | 490 (1.2%) | 451 (1.0%) | 556 (1.3%) | 917 (2.1%) | 1346 (3.2%) |
| Male | 592 (1.7%) | 556 (1.6%) | 647 (1.8%) | 1113 (3.1%) | 1715 (4.9%) |
| Characteristics of contacts: | |||||
| Direct (n) | 125 346 | 121 802 | 125 196 | 126 066 | 123 900 |
| Diagnosed (%) | 77% | 80% | 86% | 89% | 93% |
| Indirect (n) | 276 740 | 293 661 | 316 462 | 319 891 | 313 162 |
| Diagnosed (%) | 13% | 13% | 13% | 17% | 24% |
| Diagnoses (n) | 173 783 | 178 608 | 196 764 | 246 341 | 327 781 |
1Values are number of patients/physicians/contacts (percentage) if not otherwise indicated.
Multilevel analysis
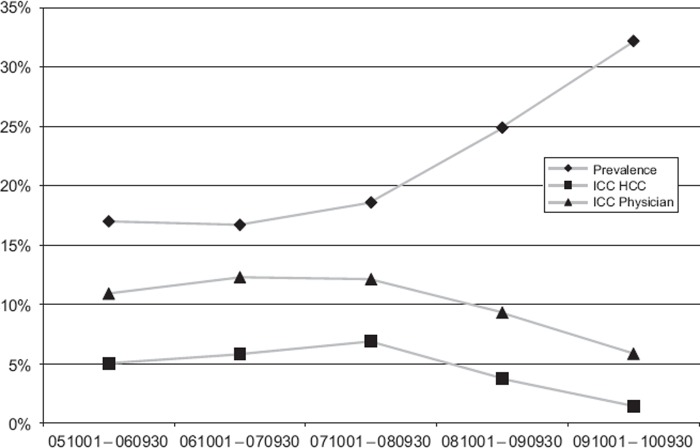
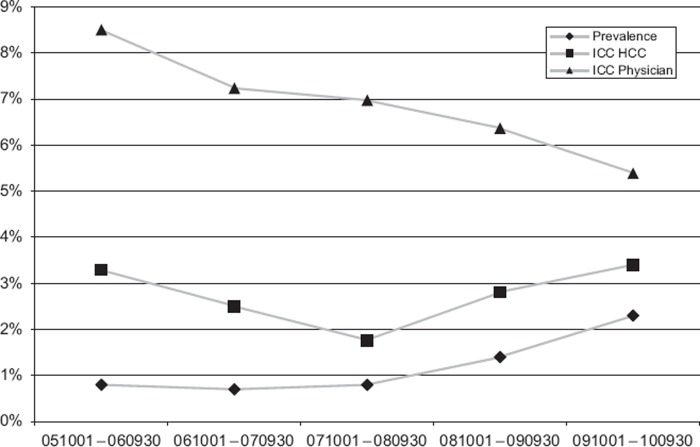
Table II shows that the adjusted prevalence of hypertension diagnoses increased from 17.4% to 32.2% between the mean of the first three and the last time period with no evident difference between sexes. In the same way, adjusted prevalence for cancer diagnoses increased from 0.79% to 2.32%. Here we can observe a clear and stable difference over time between sexes with ORs around 1.6 for men. Figure 2 shows the rise in age-adjusted prevalence of hypertension in the SPCD, and also the simultaneous decline in ICC on both HCC and physician level in the last two periods. For cancer diagnoses (Figure 3) there was a rise in prevalence and a decline in ICC at the physician level, but not at the HCC level.
Table II.
Adjusted prevalences of hypertension and cancer diagnoses, association between patient sex and these diagnoses as well as analysis of variances obtained from the multilevel regression analysis in the Skaraborg Primary care database for the five time periods.
| Time period | 051001–060930 | 061001–070930 | 071001–080930 | 081001–090930 | 091001–100930 |
|---|---|---|---|---|---|
| Diagnosis: | |||||
| Cancer | |||||
| Fixed effects: | |||||
| Adjusted prevalence,% (95% CI) | 0.79 (0.6–1.02) | 0.74 (0.58–0.93) | 0.84 (0.67–1.03) | 1.43 (1.18–1.78) | 2.32 (1.92–2.74) |
| Patient sex, OR (95% CI) | |||||
| Female | REF | REF | REF | REF | REF |
| Male | 1.6 (1.46–1.81) | 1.63 (1.43–1.85) | 1.56 (1.38–1.74) | 1.64 (1.5–1.79) | 1.71 (1.59–1.84) |
| Random effects: | |||||
| HCC variance (95% CI) | 0.036 (0.014–0.088) | 0.027 (0.011–0.064) | 0.019 (0.06–0.049) | 0.03 (0.014–0.065) | 0.036 (0.019–0.076) |
| ICC | 3.3 | 2.5 | 1.8 | 2.8 | 3.4 |
| Physician variance (95% CI) | 0.057 (0.039–0.081) | 0.051 (0.034–0.074) | 0.056 (0.038–0.08) | 0.038 (0.027–0.054) | 0.021 (0.014–0.03) |
| ICC | 8.5 | 7.2 | 7.0 | 6.4 | 5.4 |
| Hypertension | |||||
| Fixed effects: | |||||
| Adjusted prevalence,% (95%CI) | 17.0 (14.8–19.7) | 16.7 (14.4–19.2) | 18.6 (16.1–22.0) | 24.9 (21.6–28.9) | 32.2 (29.8–35.4) |
| Patient sex, OR (95% CI) | |||||
| Female | REF | REF | REF | REF | REF |
| Male | 0.91 (0.88–0.95) | 0.93 (0.89–0.96) | 0.96 (0.92–0.99) | 0.97 (0.93–1.0) | 1.01 (0.98–1.05) |
| Random effects: | |||||
| HCC variance (95% CI) | 0.19 (0.1–0.4) | 0.22 (0.11–0.46) | 0.26 (0.14–0.52) | 0.14 (0.07–0.28) | 0.05 (0.02–0.12) |
| ICC | 5.0 | 5.8 | 6.9 | 3.7 | 1.4 |
| Physician variance (95% CI) | 0.22 (0.17–0.28) | 0.24 (0.19–0.31) | 0.20 (0.16–0.25) | 0.20 (0.16–0.25) | 0.15 (0.12–0.20) |
| ICC | 10.9 | 12.3 | 12.1 | 9.3 | 5.8 |
Notes: OR = odds ratio; CI = credible interval; HCC = health care centre; ICC = intra-class correlation.
Figure 2.
Adjusted prevalences and intra-class correlations (ICC) for patients 50 years of age and older with registered hypertension diagnosis in SPCD during the five time periods.
Figure 3.
Adjusted prevalences and intra-class correlations (ICC) for patients 50 years of age and older with registered cancer diagnosis in SPCD during the five time periods.
Discussion
The main finding is that following the change of reimbursement system a clear rise in diagnosis prevalence of hypertension and cancer was observed, together with a simultaneous decline in the variation in diagnosis coding, especially at the physician level. The new practice behaviour was rather general since the clustering of possible practices habits (expressed by the ICC) were less important at the end of the study period. This study also shows that the change in diagnosis coding started when the forthcoming new reimbursement system became known, and accelerated after the implementation.
Even though we have previously shown a rather good registration rate of hypertension in the SPCD database [5], the current study demonstrates a nearly twofold rise in yearly hypertension diagnosis prevalence. This is probably due to the increased coding of indirect patient contacts. Similarly, the observed rise in cancer registration is probably also due to a shift in registration practice. Cancer diagnoses, usually established in hospital care, are most likely registered in the HCC records to a higher degree than before.
A plausible explanation for the observed increase in hypertension and cancer diagnoses in SPCD is that the increase is largely driven by the new reimbursement system, which introduced an increased economic incentive for the coding of chronic diseases. The observation that tonsillitis, which represents a diagnosis with low reimbursement value, remained constant supports this notion. Diagnoses with low reimbursement values may be less likely to increase as a consequence of the new system, simply because of the lack of an economic incentive. Furthermore, an acute diagnosis like tonsillitis may not be likely to increase over time, while chronic diseases, like hypertension and cancer, may also be coded when the reason for the visit was an acute disease.
The rise in diagnosis prevalence could also potentially be explained by upcoding, i.e. deliberate miscoding to receive higher reimbursement. Upcoding is a well-known phenomenon in other case-mix reimbursement systems, especially the US Medicare system [15,16] where 7.5% of the fees were estimated to depend on upcoding in 2009 [17]. In a comparison of three case-mix systems Steinbusch et al. [18] conclude that fewer opportunities for upcoding occur in systems where, similar to the VGPV system, the coder's salary does not directly depend on the coding. Furthermore, the observed adjusted prevalence of hypertension (33%) in the last period in our study is similar to that found in previous prevalence studies [19], indicating that the observed prevalence reflects the real burden of hypertension in the population. However, in order to exclude possible upcoding, validation of the registered ICD codes is required. The risk of upcoding will probably differ between diagnoses, with lower risks for diagnoses with more clear diagnostic criteria [18].
Even though several new private HCCs were established, the number of patients visiting the public HCCs did not change much between the time periods. An explanation for this may be that patients were automatically listed with their previous HCC unless they actively selected another HCC. Furthermore, high age and comorbidity level has previously been shown to be associated with choosing a public HCC [20].
Another potential explanation for the observed increase in hypertension and cancer diagnoses could be that incidence rates in fact increased. Unfortunately we were not able to compare the observed changes in prevalence rates with those from other health care areas. However, the observed simultaneous rise in the total number of registered diagnoses further strengthens our belief that this reflects the changing incentives for coding rather than a true change in morbidity.
A drawback of the SPCD is that patient and physician identity are not available. Therefore, it is not possible to follow physicians and patients across different HCCs. This is a minor problem when studying patients since the number of patients changing HCC is rather low (e.g. only 3.4% of patients with hypertension in Skaraborg visited more than one HCC during a 10-year period, personal communication). However, it might lead to an underestimation of the physician-level variance when studying practice variation.
A strength of our study is that it is population based and includes all patients, physicians, and HCCs in the public primary care of Skaraborg, thus minimizing the risk of selection bias. The combined study of prevalence and variance allowed us to study not only overall changes in coding prevalence but also how the coding behaviour changed at different levels.
Conclusions
This study indicates that the change of reimbursement system has had a substantial effect on the coding of chronic diseases. Part of the observed increase is probably due to an increased coding of indirect patient contacts. Thus, changes in the healthcare reimbursement system may directly influence the contents of a research database that retrieves data from clinical practice. This should be taken into account when using such a database for research purposes, and the data should be validated for each diagnosis.
Ethical approval
The study was approved by The Regional Ethical Review Board in Gothenburg
Declaration of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper
This research was funded by the Skaraborg Research and Development Councils, an ALF governmental grant (Dnr M 2008/1593, PI: JM), the Swedish Council for Working Life and Social Research [Dnr: 2010-0402, PI: JM] and the Swedish Research Council [Dnr K2011-69X-15377-07-6, PI: JM].
References
- 1.Hjerpe P, Ohlsson H, Lindblad U, Bostrom KB, Merlo J. Understanding adherence to therapeutic guidelines: A multilevel analysis of statin prescription in the Skaraborg Primary Care Database. Eur J Clin Pharmacol. 2011;67:415–23. doi: 10.1007/s00228-010-0973-4. [DOI] [PubMed] [Google Scholar]
- 2.Krav och Kvalitetsboken, Förfrågningsunderlag med förutsättningar för att bedriva vårdverksamhet inom VG Primärvård 2011. [Demands and quality, tender request documentation with requirements for running health care in Västra Götaland primary care] Vänersborg: Västra Götalandsregionen; 2011. [Google Scholar]
- 3.Johns Hopkins University ACG Case-Mix system. Available at: www.acg.jhsph.edu/html/AboutACGs.htm (accessed May 19, 2011)
- 4.Gosden T, Forland F, Kristiansen IS, Sutton M, Leese B, Giuffrida A, et al. Impact of payment method on behaviour of primary care physicians: A systematic review. J Health Serv Res Policy. 2001;6:44–55. doi: 10.1258/1355819011927198. [DOI] [PubMed] [Google Scholar]
- 5.Hjerpe P, Merlo J, Ohlsson H, Bengtsson Bostrom K, Lindblad U. Validity of registration of ICD codes and prescriptions in a research database in Swedish primary care: A cross-sectional study in Skaraborg primary care database. BMC Med Inform Decis Mak. 2010;10:23. doi: 10.1186/1472-6947-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dalemo S, Hjerpe P, Bostrom Bengtsson K. Diagnosis of patients with raised serum calcium level in primary care, Sweden. Scand J Prim Health Care. 2006;24:160–5. doi: 10.1080/02813430600784443. [DOI] [PubMed] [Google Scholar]
- 7.Dalemo S, Hjerpe P, Ohlsson H, Eggertsen R, Merlo J, Bostrom KB. Variation in plasma calcium analysis in primary care in Sweden: A multilevel analysis. BMC Fam Pract. 2010;11:43. doi: 10.1186/1471-2296-11-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weidinger P, Nilsson JL, Lindblad U. Adherence to diagnostic guidelines and quality indicators in asthma and COPD in Swedish primary care. Pharmacoepidemiol Drug Saf. 2009;18:393–400. doi: 10.1002/pds.1734. [DOI] [PubMed] [Google Scholar]
- 9.Socialstyrelsen [The National Board of Health and Welfare] Klassifikation av sjukdomar och hälsoproblem 1997 – PRIMÄRVÅRD [Classification of diseases and related health problems 1997 – PRIMARY CARE] Stockholm: Socialstyrelsen; 1997 [Google Scholar]
- 10.Rasbash J, Steele F, Browne W, Goldstein H. A User´s guide to MLwiN – Version 2.10. Bristol: Centre for Multilevel Modelling, University of Bristol; 2009. [Google Scholar]
- 11.Snijders T, Bosker R. Multilevel analysis: An introduction to basic and advanced multilevel modeling. London: Sage Publications; 1999. [Google Scholar]
- 12.Merlo J, Chaix B, Yang M, Lynch J, Rastam L. A brief conceptual tutorial on multilevel analysis in social epidemiology: Interpreting neighbourhood differences and the effect of neighbourhood characteristics on individual health. J Epidemiol Community Health. 2005;59:1022–8. doi: 10.1136/jech.2004.028035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Merlo J, Chaix B, Ohlsson H, Beckman A, Johnell K, Hjerpe P, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60:290–7. doi: 10.1136/jech.2004.029454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Browne W. MCMC estimation in MLwiN, v2.13. Bristol: Centre for Multilevel Modelling, University of Bristol; 2009. [Google Scholar]
- 15.Brunt CS. CPT fee differentials and visit upcoding under Medicare Part B. Health Econ. 2011;20:831–41. doi: 10.1002/hec.1649. [DOI] [PubMed] [Google Scholar]
- 16.Silverman E, Skinner J. Medicare upcoding and hospital ownership. J Health Econ. 2004;23:369–89. doi: 10.1016/j.jhealeco.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 17.Improper Medicare Fee-For-Service Payments Report – November 2009 Long Report. Baltimore: Centers for Medicare and Medicaid Services; 2009. [Google Scholar]
- 18.Steinbusch PJ, Oostenbrink JB, Zuurbier JJ, Schaepkens FJ. The risk of upcoding in casemix systems: A comparative study. Health Policy. 2007;81:289–99. doi: 10.1016/j.healthpol.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 19.Måttligt förhöjt blodtryck uppdatering 2007 – En systematisk litteraturöversikt [Moderately elevated blood pressure update 2007 – A systematic literature review] Stockholm: SBU [Swedish Council on Health Technology Assessment]; 2007. [Google Scholar]
- 20.Zielinski A, Håkansson A, Beckman A, Halling A. Impact of comorbidity on the individual's choice of primary health care provider. Scand J Prim Health Care. 2011;29:104–9. doi: 10.3109/02813432.2011.562363. [DOI] [PMC free article] [PubMed] [Google Scholar]