A 19-year-old female who was a known case of multiple endocrine neoplasia (MEN) type 2, presented with gradual decrease of visual acuity in her left eye and bilateral corneal opacities which had developed over a 7 month period. She had nocturnal lagophthalmos since childhood, and history of a thyroid mass with increased serum levels of calcitonin for which subtotal thyroidectomy had been performed. The histopathologic diagnosis of the thyroid mass had been medullary thyroid carcinoma. Best corrected visual acuity was 20/25 and 20/40 in her right and left eyes, respectively. Slit lamp biomicroscopic examination, photography using a photo slit lamp (Haag-Streit BQ900, Switzerland), and corneal confocal scan imaging (Confoscan 3.4, Nidek Technology, Padova, Italy) were performed. Since we suspected limbal stem cell deficiency, impression cytology was also performed on both eyes.
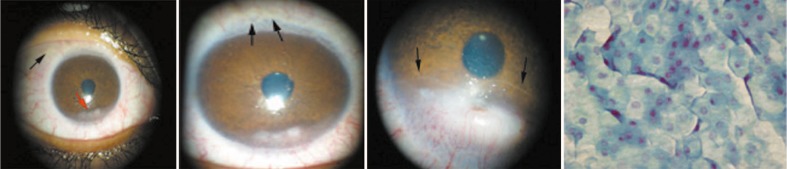
Slit lamp examination in both eyes revealed moderate thickening of the eyelid margins, meibomian gland dysfunction, gelatinous and worm-like subconjunctival masses in the perilimbal area suggestive of neuromas (Fig. 1A), nonspecific vascularized opacification of the inferior cornea which was more severe on the left side (Fig. 1B), and prominent intrastromal medullated nerves with an irregular lacy pattern across more than half of the cornea (Fig. 1C). Intraocular pressure and fundus examination were unremarkable. Although the patient had signs of meibomian gland dysfunction, she did not have dry eye symptoms. Since we were suspicious of limbal stem cell deficiency as one of the possible factors in the development of corneal opacities, impression cytology was performed bilaterally which disclosed mild epithelial squamous metaplasia of the involved areas, but no signs of limbal stem cell deficiency (Fig. 1D).
Figure 1.
(A) Slit lamp photograph of the right cornea demonstrates gelatinous vermiform lesions at the superotemporal conjunctiva (black arrow) and a vascularized corneal opacity inferiorly (red arrow); (B) The left cornea also demonstrates gelatinous worm-like conjunctival lesions in the superior limbal-conjunctival region suggestive of a neuroma (arrows) and marked vascularized corneal opacification inferiorly; (C) Note the irregular lacy pattern of visible intrastromal medullated nerves (arrows) adjacent to the corneal opacity; (D) Note lack of goblet cells in the epithelial sheet on the inferior corneal side where nuclear/cytoplasmic ratio seems to be decreased (magnification ×400).
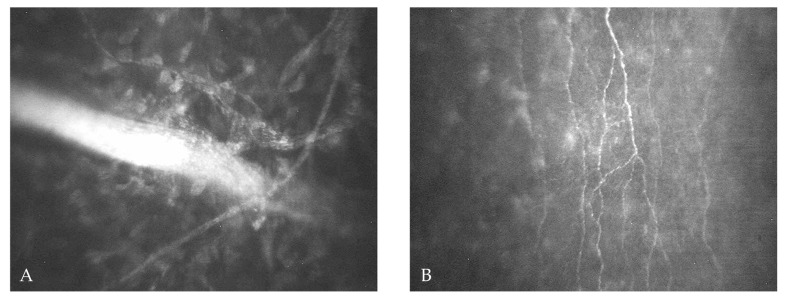
Confocal scanning of central, paracentral and inferior parts of the corneas demonstrated normal-appearing epithelium in the right eye, while the epithelium was hyper-reflective on the left side. Sub-basal epithelial nerves (Fig. 2B) were obviously thickened with maximum diameter and density of 26.7μm and 27.8μm/ mm2 respectively on the right side, and 32.4μm and 28.3μm/mm2 correspondingly in the left eye. Foci of vascularization together with areas of nonspecific hyper-reflectivity and haze were observed in the inferior peripheral corneal stroma. Adjacent to this area and towards the paracentral cornea, there was marked thickening and brightness of mid-stromal nerves (Fig. 2A) with diameter ranging from 14.5 to 66.7 (mean, 42.1±16.5) μm in the right cornea, and from 15.8 to 62.9 (mean, 39.5±17.5) μm in the left eye. A few thin and convoluted nerve fibers were also present within the mid-stroma. The endothelium was unremarkable in the right cornea but details of the endothelium were not visible on the left side.
Figure 2.
Confocal scan images of the cornea. (A) Note the presence of greatly thickened and high contrast mid-stromal nerves (magnification ×500). (B) Increased density of the sub-epithelial nerve plexus (magnification ×500).
Given the presence of possible perilimbal neuromas, the final diagnosis was consistent with MEN-2b syndrome. The patient was followed with Artelac eye drops (Pharma Global limited, Dublin, Ireland) four times a day and Liposic 0.2% ophthalmic gel (Bausch & Lomb limited, UK) applied at night-time.
DISCUSSION
MEN syndrome is an autosomal dominant disorder caused by a mutation in the RET proto-oncogene on chromosome 10 with 100% penetrance but variable expressivity; the de novo mutation rate is approximately 50%. This syndrome is categorized into type 1 and 2. Type 1 includes adenomas in the parathyroid, pancreas, thyroid and adrenal glands associated with subcutaneous lipomas. Type 2 includes pheochromocytoma, medullary thyroid carcinoma and parathyroid tumor or hyperplasia. Type 2 has two subcategories namely 2a and 2b; the former is characterized by medullary carcinoma, pheochromocytoma, and parathyroid disease, whereas type 2b is characterized by medullary thyroid carcinoma, pheochromocytoma, and multiple mucosal neuromas.1,2 Medullary thyroid carcinoma, which has a poor prognosis, develops in nearly 100% of type 2b cases early in life. Other systemic findings in this syndrome include a marfanoid habitus, thickened lips, lingual and cheek mucosal nodules, maxillofacial and orthopedic changes, café-au-lait spots and diarrhea or constipation.3,4
Due to ocular involvement, ophthalmologists may be the first physicians to diagnose this syndrome at a precancerous stage. Ocular findings typically observed in this syndrome are thickened eyelid margins, multiple small plexiform/nodular subconjunctival neuromas, and thickened corneal and ciliary nerves.1,2,5-10 Chronic ocular irritation may occur due to thickening of the eyelid margins and conjunctiva.1 Other ocular findings include heavy eyebrows and prominent orbital ridges, nasal displacement of the lacrimal puncta, keratoconjunctivitis sicca, and impaired pupillary dilation.3,4 To the best of our knowledge, there are no reports on the confocal scan and impression cytology features of corneal involvement in this syndrome. The ocular findings, confocal scan images and impression cytology features of the cornea in this case of MEN-2b syndrome are discussed herein.
Among ocular findings in MEN-2b syndrome, prominent corneal nerves with a diameter of up to 1.5mm have been reported as a hallmark of the condition7,11 and can be seen as early as 2 years of age.12 Prominent corneal nerves may also be the first manifestation of other systemic disorders such as MEN-2a syndrome, leprosy, neurofibromatosis, pheochromocytoma, primary amyloidosis, ectodermal dysplasia, Refsum’s disease and congenital ichthyosis. Keratoconus, herpes simplex and herpes zoster viruses, posterior polymorphous dystrophy and Fuchs’ endothelial dystrophy are other corneal diseases in which corneal nerves may be apparently thickened and more visible.13-17 In our patient, interlacing and thickened midstromal nerves were observed in both corneas on slit lamp biomicroscopic examination and their thickness was measured by confocal scan. The mid-stromal nerves in this case were about 5 to 6 times thicker than that observed in normal corneas (8.32+2.6μm).18 Using confocal scan, we also demonstrated an increased density of sub-basal epithelial nerves, 27.8 μm/mm2 in the right cornea and 28.3μm/mm2 in the left one, as compared to a normal density of 11.1 μm/ mm.2,19 An increase in the number of Schwann cells and axons, and in myelination of corneal nerves have been reported as causes of nerve thickening and enlargement.11,13 The mechanism underlying corneal nerve medullation in this syndrome remains unknown, but the embryological explanation may be similar to that for medullated nerve fibers in the fundus.7
Bilateral inferior corneal opacification and vascularization were the most important ocular manifestation in our patient. She presented with gradually decreased visual acuity in her left eye and bilateral corneal opacities over several months. This means that she might not have had the inferior corneal changes before developing these symptoms. The lid malfunction during night-time might have occurred following thyroidectomy, or possibly after development of thyroid-associated ophthalmopathy.20 This in turn might have had an additional effect on the severity of the corneal opacities. However, the most important cause of these corneal changes is abnormal intrastromal corneal nerves and altered sensation in MEN-2b.
Since we suspected limbal stem cell deficiency as a possible factor intensifying the corneal opacities, we performed impression cytology which revealed only mild corneal epithelial squamous metaplasia in the inferior cornea with no evidence of limbal stem cell deficiency. The results of impression cytology in this case were similar to those seen in exposure and neurotrophic keratopathies.
In summary, in this report the clinical and microstructural features of ocular involvement in MEN-2b syndrome are described. Vascularized inferior peripheral corneal opacities due to a combination of neurotrophic causes and exposure keratopathy were the most prominent ocular finding. MEN-2b must be considered in any patient with thickened and visible corneal nerves together with conjunctival neuromas.
REFERENCES
- 1.Mora ML, Smith RE. Corneal and systemic diseases. In: Tasman W. In: Tasman W, editor. Duane’s Clinical Ophthalmology. Lippincott Williams & Wilkins; 2004. [Google Scholar]
- 2.Tomida I, Rohrbach JM, Zierhut M, Dralle H. Conjunctival neuromas and prominent corneal nerve fibers as diagnostic indication of multiple endocrine disease. Klin Monbl Augenheilkd . 2001;218:463–465. doi: 10.1055/s-2001-16264. [DOI] [PubMed] [Google Scholar]
- 3.Carney JA, Bianco AJ, Sizemore GW, Hayles AB. Multiple endocrine neoplasia with skeletal manifestations. J Bone Joint Surg Am. 1981;63:405–410. [PubMed] [Google Scholar]
- 4.Schenberg ME, Zajac JD, Lim-Tio S, Collier NA, Brooks AMV, Reade PC. Multiple endocrine neoplasia type 2b. Case report and review. Int J Oral Maxillofac Surg. 1992;21:110–114. doi: 10.1016/s0901-5027(05)80545-4. [DOI] [PubMed] [Google Scholar]
- 5.Braley AE. Medullated corneal nerves and plexiform neuroma associated with pheochromocytoma. Trans Am Ophthalmol Soc. 1954;52:189–197. [PMC free article] [PubMed] [Google Scholar]
- 6.Kinoshita S, Tanaka F, Ohashi Y, Ikeda M, Takai S. Incidence of prominent corneal nerves in multiple endocrine neoplasia type 2A. Am J Ophthalmol. 1991;111:307–311. doi: 10.1016/s0002-9394(14)72314-1. [DOI] [PubMed] [Google Scholar]
- 7.Kirby BS. Clinical Eye and Vision Care. Butterworth Heinemann; 1997. [Google Scholar]
- 8.Sahin A, Yildirim N. Ocular findings in a child with multiple endocrine neoplasia type 2b. J Pediatr Ophthalmol Strabismus . 2008;45:313–315. doi: 10.3928/01913913-20080901-15. [DOI] [PubMed] [Google Scholar]
- 9.Eter N, Klingmüller D, Höppner W, Spitznas M. Typical ocular findings in a patient with multiple endocrine neoplasia type 2b syndrome. Graefes Arch Clin Exp Ophthalmol . 2001;239:391–394. doi: 10.1007/s004170000245. [DOI] [PubMed] [Google Scholar]
- 10.Takai S, Kinoshita S, Tanaka F, Ikeda M, Tanaka N, Kobayashi T. Prominent corneal nerves in patients with multiple endocrine neoplasia type 2A: diagnostic implications. World J Surg . 1992;16:620–623. doi: 10.1007/BF02067337. [DOI] [PubMed] [Google Scholar]
- 11.Riley FC, Robertson DM. Ocular histopathology in multiple endocrine neoplasia type 2b. Am J Ophthalmol . 1981;91:57–64. doi: 10.1016/0002-9394(81)90349-4. [DOI] [PubMed] [Google Scholar]
- 12.Robertson DM, Sizemore GW, Gordon H. Thickened corneal nerves as a manifestation of multiple endocrine neoplasia. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol . 1975;79:OP772–787. [PubMed] [Google Scholar]
- 13.Baum JL, Adler ME. Pheochromocytoma, medullary thyroid carcinoma, multiple mucosal neuroma. A variant of the syndrome. Arch Ophthalmol. 1972;87:574–584. doi: 10.1001/archopht.1972.01000020576016. [DOI] [PubMed] [Google Scholar]
- 14.Gorlin RJ, Sedano HO, Vickers RA, Cervenka J. Multiple mucosal neuromas, pheochromocytoma and medullary carcinoma of the thyroid: a syndrome. Cancer. 1968;22:293–299. doi: 10.1002/1097-0142(196808)22:2<293::aid-cncr2820220206>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 15.Arffa RC, Grayson M. Grayson’s Diseases of the Cornea. Mosby; St. Louis: 1991. [Google Scholar]
- 16.Kane LA, Tsai MS, Gharib H, Khosla S, Robertson DM, Schaid DJ, et al. Familial medullary thyroid cancer and prominent corneal nerves: clinical and genetic analysis. J Clin Endocrinol Metab. 1995;80:289–293. doi: 10.1210/jcem.80.1.7829628. [DOI] [PubMed] [Google Scholar]
- 17.Mensher JH. Corneal nerves. Surv Ophthalmol. 1974;19:1–18. [PubMed] [Google Scholar]
- 18.Jafarinasab MR, Zarei-Ghanavati S, Kanavi MR, Karimian F, Soroush MR, Javadi MA. Confocal microscopy in chronic and delayed mustard gas keratopathy. Cornea . 2010;29:889–894. doi: 10.1097/ICO.0b013e3181ca324c. [DOI] [PubMed] [Google Scholar]
- 19.Erie JC, McLaren JW, Patel SV. Confocal microscopy in ophthalmology. Am J Ophthalmol. 2009;148:639–646. doi: 10.1016/j.ajo.2009.06.022. [DOI] [PubMed] [Google Scholar]
- 20.Chavis PS. Thyroid and the eye. Curr Opin Ophthalmol. 2002;13:352–356. doi: 10.1097/00055735-200212000-00002. [DOI] [PubMed] [Google Scholar]